Introduction
Non-small cell lung cancer (NSCLC) accounts for ~80%
of all lung cancer cases (1) and is
the most common cause of cancer-associated mortality worldwide
(2). Globally, the annual diagnosis
rate of new NSCLC cases is ~1.6 million, with the rate increasing
over the last decades (3). A previous
study demonstrated the importance of molecular characterization of
these tumors and the identification of potential molecular targets
for treatment (3). However, the
prognosis in these patients remains poor as the overall 5-year
survival is <15% (4). These
unsatisfactory clinical outcomes indicate the requirement for more
reliable predictors of survival and novel therapeutic targets
(3).
The tripartite motif (TRIM) family members are
involved in numerous biological processes and, when altered, are
implicated in a number of pathological conditions (5). TRIM29, which is also known as
ataxia-telangiectasia group D complementing protein (ATDC), is a
member of the TRIM family proteins (6). TRIM29 is highly expressed in gastric
cancer and is involved in the differentiation, proliferation and
progression of gastric cancer cells (7). In addition, TRIM29 was found to be
overexpressed in bladder cancer, ovarian serous papillary tumors
and endometrial neoplasms (8,9). However, the clinical significance and
prognostic value of TRIM29 expression in NSCLC patients remain
unclear. The present study aimed to investigate the association
between TRIM29 expression and the clinicopathological features of
NSCLC, as well as examine the potential role of TRIM29 as a
prognostic factor in NSCLC patients.
Materials and methods
Patients and histological
evaluation
NSCLC patients who were diagnosed, treated and
followed-up at the Department of Thoracic Surgery (Shandong
Qianfoshan Hospital, Jinan, China) between January 2000 and January
2007 were recruited in this study. The inclusion criteria were as
follows: Patients with surgically resected and pathologically
confirmed primary NSCLC, complete medical records and available
paraffin-embedded specimens were included. In total, 320 patients
with NSCLC were enrolled, including 221 patients treated with
lobectomy and 99 patients treated with pneumonectomy. Clinical
variables were retrieved from the patients' medical records,
including age, gender, and survival or disease progression
(Table I). Tumor diagnosis and
histological classification were based on a new multidisciplinary
classification of lung cancer proposed by the International
Association for the Study of Lung Cancer, American Thoracic
Society, and European Respiratory Society (10). Tumors were staged according to the 7th
edition of the TNM Classification of Malignant Tumors (11,12).
Normal bronchial epithelium obtained from noncancerous lung tissue
of the NSCLC patients was used as the control. The study was
approved by the Institutional Review Board at the Shandong
Qianfoshan Hospital. Written informed consent was obtained from all
patients.
 | Table I.Association between TRIM29 expression
and clinicopathological features. |
Table I.
Association between TRIM29 expression
and clinicopathological features.
|
| TRIM29
expression |
|
|---|
|
|
|
|
|---|
| Characteristic | High | Low | P-value |
|---|
| Patients, n (%) | 79 (24.7) | 241 (75.3) |
|
| Gender, n (%) |
|
| 0.092 |
| Male | 65 (82.3) | 214 (88.8) |
|
|
Female | 14 (17.7) | 27 (11.2) |
|
| Mean age ± SD,
years | 57.32±11.8 | 59.26±9.77 | 0.113 |
| Smoking status, n
(%) |
|
| 0.012 |
|
Smoker | 50 (63.3) | 200 (83) |
|
|
Non-smoker | 29 (36.7) | 41 (17) |
|
| Histology, n (%) |
|
| 0.821 |
| SCC | 31 (39.2) | 184 (76.3) |
|
| ADC | 48 (60.8) | 57 (23.7) |
|
| Pathological stage, n
(%) |
|
| 0.210 |
| Stage
I | 28 (35.4) | 110 (45.6) |
|
| Stage
II | 26 (32.9) | 72 (29.9) |
|
| Stage
III | 21 (26.6) | 50 (20.7) |
|
| Stage
IV | 4 (5.1) | 9 (3.7) |
|
| T stage, n (%) |
|
| 0.015 |
| T1 | 23 (29.1) | 30 (12.4) |
|
| T2 | 40 (50.6) | 163 (67.6) |
|
| T3 | 12 (15.2) | 20 (8.3) |
|
| T4 | 4 (5.1) | 28 (11.7) |
|
| N stage, n (%) |
|
| 0.920 |
| N0 | 48 (60.8) | 147 (61) |
|
| N1 | 15 (19) | 51 (21.2) |
|
| N2 | 16 (20.2) | 43 (17.8) |
|
| M stage, n (%) |
|
| 0.003 |
| M0 | 29 (36.7) | 205 (85.1) |
|
| M1 | 50 (63.3) | 36 (14.9) |
|
Follow-up
Standardized follow-up was conducted every 3 months
for the first 2 years after surgery, every 6 months for the 3rd
year and yearly thereafter. Follow-up included physical
examination, complete blood count, chest computed tomography scans,
brain magnetic resonance imaging scans and abdominal ultrasound.
The median follow-up period for surviving patients was 31.5 months
(6–72 months). Disease-free survival (DFS) was defined as the time
from the initial surgery until a documented relapse, including
locoregional recurrence and distant metastasis. The overall
survival (OS) was defined from the date of the initial surgery
until mortality or the end of follow-up.
Immunohistochemical analysis
Tissue sections (6 µm) were deparaffinized in
xylene, rehydrated and heated at 100°C in citrate buffer (pH 6.0)
for 5 min for nonenzymatic antigen retrieval. The sections were
then incubated with monoclonal mouse anti-human TRIM29 antibody
(cat. no. H00023650-B01; dilution, 1:100; Novus Biologicals, LLC,
Littleton, CO, USA) for 60 min at room temperature, followed by
incubation with a goat anti-mouse immunoglobulin G antibody (cat.
no. AI-9200; dilution, 1:1,000; Vector Laboratories, Inc.,
Burlingame, CA, USA) for 1 h at room temperature. Staining was
performed with 3,3′-diaminobenzidine chromogen for 5 min, followed
by counterstaining using hematoxylin (Beijing Solarbio Science
& Technology Co., Ltd., Beijing, China) for 5 min, as
previously described (13). Rabbit
IgG (cat. no. NP-001; Epitomics Inc., Burlingame, CA, USA) was used
as a negative control. TRIM29 expression was scored as follows: 0,
no staining; 1+, <10% of tumor cells expressing TRIM29; 2+,
10-50% of tumor cells expressing TRIM29; and 3+, >50% of tumor
cells expressing TRIM29. Scores of 0 and 1+ were classified as low
TRIM29 expression, whereas scores of 2+ and 3+ were classified as
high TRIM29 expression. The scoring is a modification of a
previously described classification (14). Two pathologists blinded to the
patients' clinical data interpreted all the slides and agreed on
the classification of the sections into the low or high TRIM29
expression groups.
Statistical analysis
In order to determine any possible associations
between qualitative clinicopathological variables and TRIM29
expression, the χ2 test or two-tailed Fisher's exact
test was applied. Survival differences among the high- and
low-expression groups were calculated using the Kaplan-Meier method
along with the log-rank test. The Cox proportional hazards model
was used for multivariate analyses of OS and DFS. SPSS version 16.0
statistical software (SPSS Inc., Chicago, IL, USA) was used for all
statistical analyses. P<0.05 was considered to indicate a
statistically significant difference.
Results
Association between TRIM29 expression
and clinicopathological features of NSCLC patients
Various patient characteristics and their
correlation with TRIM29 expression are listed in Table I. The mean age at diagnosis was
58.9±10.7 years (range, 34–82 years). A total of 138 patients
(43.1%) were diagnosed with stage I, 98 (30.6%) with stage II, 71
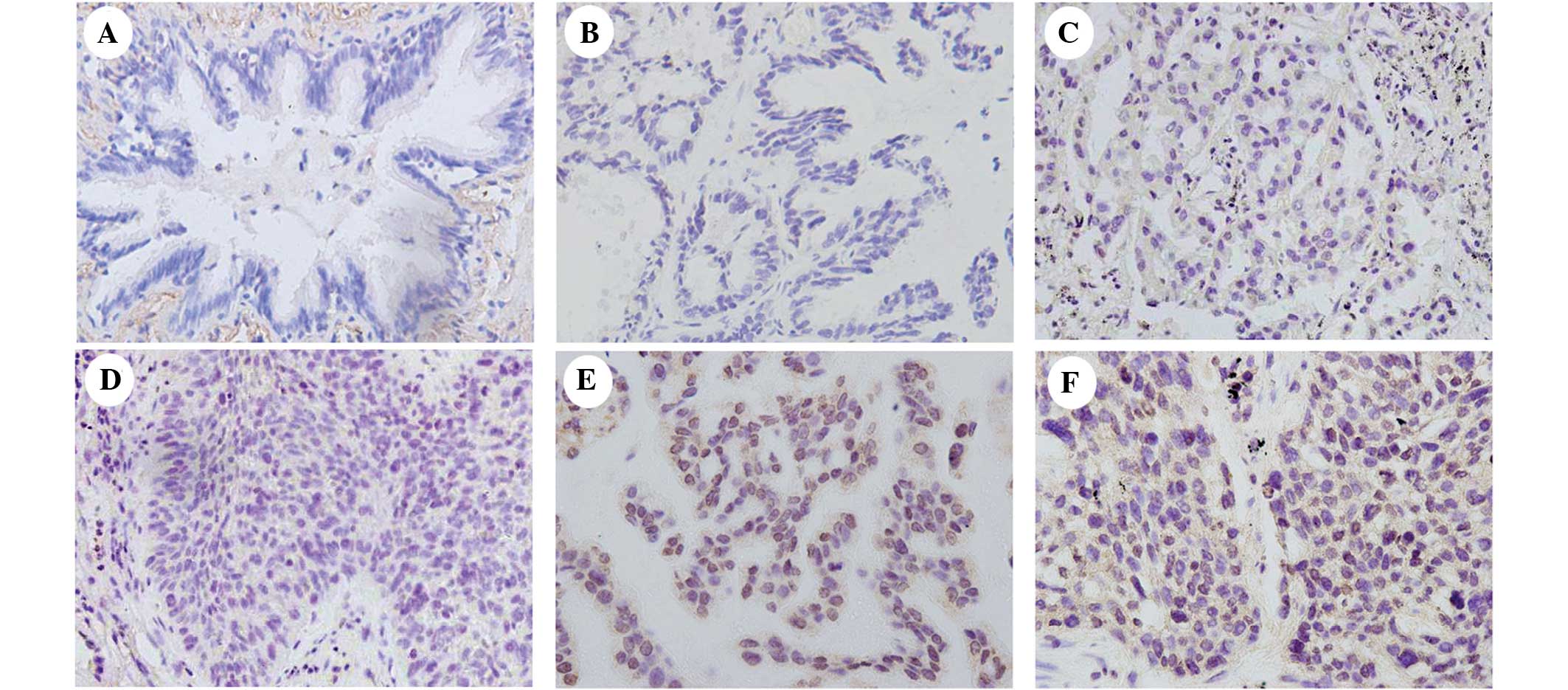
(22.2%) with stage III and 13 (4.1%) with stage IV disease. TRIM29
expression was predominantly localized in the nuclear compartments
of the tumor cells, while the normal bronchial epithelia exhibited
negative or low staining (Fig.
1).
The association between total TRIM29 expression and
various clinical parameters was investigated. As shown in Table I, a high TRIM29 expression was
significantly associated with smoking (P=0.012), a higher T stage
(P=0.015) and a higher M stage (P=0.003). However, no statistically
significant correlation was observed between TRIM29 expression and
other clinical features.
Association between TRIM29 expression
and OS or DFS
The prognostic relevance of TRIM29 expression and
other clinicopathological parameters with regard to OS and DFS in
patients with NSCLC was investigated (Table II; Fig. 2A
and B). Patients with high TRIM29 expression presented shorter
OS and DFS rates compared with patients with low TRIM29 expression
(P=0.007 and P=0.014, respectively). In addition, pathological
stage (I/II vs. III/IV) and TNM stage were demonstrated to be
independent prognostic factors affecting OS and DFS (P<0.001;
Table II). Furhtermore, high TRIM29
expression was demonstrated to be an independent prognostic factor
affecting OS (P=0.003; hazard ratio, 2.102; 95% confidence
interval, 1.069–3.193) using multivariate analyses (Table III).
 | Table II.Univariate analyses of overall
survival and disease-free survival in 320 patients with non-small
cell lung cancer. |
Table II.
Univariate analyses of overall
survival and disease-free survival in 320 patients with non-small
cell lung cancer.
|
| Overall survival |
| Disease-free
survival |
|
|---|
|
|
|
|
|
|
|---|
| Characteristic | Hazard ratio (95%
CI) | P-value | Hazard ratio (95%
CI) | P-value |
|---|
| TRIM29
expression |
| 0.007 |
|
0.014 |
| Low vs.
high | 1.52
(1.120–2.061) |
| 1.51
(1.089–2.119) |
|
| Gender |
| 0.134 |
|
0.982 |
| Female
vs. male | 0.56
(0.267–1.049) |
| 0.97
(0.670–1.427) |
|
| Smoking status |
| 0.025 |
|
0.190 |
| No vs.
yes | 1.48
(1.049–2.138) |
| 0.80
(0.570–1.121) |
|
| Age, years |
| 0.079 |
|
0.447 |
| ≤60 vs.
>60 | 1.43
(1.036–1.901) |
| 0.82
(0.642–1.213) |
|
| Histology |
| 0.814 |
|
0.625 |
| SCC vs.
ADC | 1.07
(0.766–1.403) |
| 1.34
(0.979–1.858) |
|
| Stage |
| <0.001 |
| <0.001 |
| I/II
vs. III/IV | 2.69
(1.933–3.550) |
| 1.86
(1.314–2.648) |
|
| T stage |
| <0.001 |
| <0.001 |
| T1/T2
vs. T3/T4 | 2.84
(2.082–3.995) |
| 2.35
(1.621–3.429) |
|
| N stage |
| <0.001 |
| <0.001 |
| N0 vs.
N1/N2 | 2.30
(1.725–3.120) |
| 1.96
(1.419–2.695) |
|
| M stage |
| <0.001 |
| <0.001 |
| M0 vs.
M1 | 2.54
(1.894–3.725) |
| 2.02
(1.711–3.502) |
|
 | Table III.Multivariate analyses of overall
survival and disease-free survival in 320 patients with non-small
cell lung cancer. |
Table III.
Multivariate analyses of overall
survival and disease-free survival in 320 patients with non-small
cell lung cancer.
|
| Overall
survival |
| Disease-free
survival |
|
|---|
|
|
|
|
|
|
|---|
| Characteristic | Hazard ratio (95%
CI) | P-value | Hazard ratio (95%
CI) | P-value |
|---|
| TRIM29
expression |
| 0.003 |
|
0.064 |
| Low vs.
high | 2.102
(1.069–3.193) |
| 1.384
(0.982–1.952) |
|
| Gender |
|
0.036 |
|
0.331 |
| Female
vs. male | 1.921
(1.044–3.535) |
| 1.327
(0.750–2.347) |
|
| Smoking status |
|
0.312 |
|
0.406 |
| No vs.
yes | 1.277
(0.795–2.052) |
| 0.813
(0.499–1.325) |
|
| Age, years |
|
0.001 |
|
0.692 |
| ≤60 vs.
>60 | 1.752
(1.274–2.410) |
| 1.070
(0.766–1.495) |
| Histology |
|
0.007 |
|
0.040 |
| SCC vs.
ADC | 1.611
(1.141–2.275) |
| 1.506
(1.020–2.225) |
|
| Stage |
|
0.415 |
|
0.649 |
| I/II
vs. III/IV | 1.196
(0.778–1.838) |
| 0.891
(0.543–1.463) |
|
| T stage |
|
<0.001 |
| <0.001 |
| T1/T2
vs. T3/T4 | 2.050
(1.371–3.065) |
| 2.246
(1.427–3.537) |
|
| N stage |
|
<0.001 |
| <0.001 |
| N0 vs.
N1/N2 | 2.053
(1.592–3.413) |
| 1.817
(1.100–2.713) |
|
| M stage |
|
<0.001 |
|
0.001 |
| M0 vs.
M1 | 2.316
(1.618–3.313) |
| 1.952
(1.320–2.888) |
|
Discussion
The aim of the present study was to determine the
prognostic significance of TRIM29 protein expression in NSCLC.
Based on the findings of the current study, TRIM29 overexpression
appears to be associated with aggressive tumor behavior and
ultimately influences patients' clinical outcomes. In addition, a
high TRIM29 expression was prevalent in smokers and was found to be
an unfavorable clinical factor in NSCLC.
Recent evidence has suggested that TRIM29 promotes
cancer cell proliferation via inhibiting the nuclear activities of
p53, which is a major tumor suppressor gene involved in the
determination of proliferation or growth arrest at the cellular
level (15,16). TRIM29 binds p53 and represses the
expression of p53-regulated genes, including p21 and
NOXA (15,17). In addition, TRIM29 is selectively
expressed in basal cells of the normal prostate gland. In a
previous study, immunohistochemical staining with anti-TRIM29
antibody revealed the same expression pattern as that observed for
staining with 34βE12 in prostate cancer and its benign mimics,
indicating that TRIM29 may be useful for distinguishing prostate
cancer from benign tissues (18).
Furthermore, younger females with early-stage breast cancer who
were not administered adjuvant systemic therapy had a significantly
lower risk of relapse when their tumor exhibited a high TRIM29
expression (19). This finding
suggests that loss of TRIM29 expression in normal breast luminal
cells can contribute to malignant transformation and lead to
progression of breast cancer in premenopausal women (19). The expression of TRIM29 was also
significantly associated with progression to muscle-invasive
bladder cancer and was identified as an independent prognostic
marker (20). In addition, TRIM29 has
been reported to upregulate matrix metalloproteinase 9 to promote
lung cancer cell invasion by activating the extracellular
signal-regulated kinase and c-Jun N-terminal kinase signaling
pathways (21). Previous results have
identified a DNA repair pathway leading from MAPK-activated protein
kinase-2 and ataxia telangiectasia mutated to TRIM29 (22). Therefore, as TRIM29 has been used as a
therapeutic target to radiosensitize pancreatic ductal
adenocarcinoma and improve the efficacy of DNA-damaging treatment
in pancreatic cancer (22), the use
of TRIM29 as a potential therapeutic target for the treatment of
NSCLC was investigated in the present study.
In conclusion, in the present study, TRIM29
expression was investigated by immunohistochemical analysis in
paraffin-embedded specimens obtained from 320 patients with
surgically resected NSCLC, treated between 2000 and 2007. High
TRIM29 expression was significantly associated with smoking, T
stage and M stage. Furthermore, elevated TRIM29 expression level
was correlated with reduced OS and DFS and was an independent
prognostic factor for OS in NSCLC. Therefore, TRIM29 may be a
useful prognostic marker in NSCLC patients and a potential
molecular target for NSCLC treatment.
References
|
1
|
Dempke WC, Suto T and Reck M: Targeted
therapies for non-small cell lung cancer. Lung Cancer. 67:257–274.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Greenlee RT, Hill-Harmon MB, Murray T and
Thun M: Cancer statistics. CA Cancer J Clin. 51:15–36. 2011.
View Article : Google Scholar
|
|
3
|
Gainor JF and Shaw AT: Novel targets in
non-small cell lung cancer: ROS1 and RET fusions. Oncologist.
18:865–875. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Villarreal Garza, de la Mata D, Zavala DG,
Macedo-Perez EO and Arrieta O: Aggressive treatment of primary
tumor in patients with non-small-cell lung cancer and exclusively
brain metastases. Clin Lung Cancer. 14:6–13. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Napolitano LM and Meroni G: TRIM family:
Pleiotropy and diversification through homomultimer and
heteromultimer formation. IUBMB Life. 64:64–71. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hatakeyama S: TRIM proteins and cancer.
Nat Rev Cancer. 11:792–804. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kosaka Y, Inoue H, Ohmachi T, Yokoe T,
Matsumoto T, Mimori K, Tanaka F, Watanabe M and Mori M: Tripartite
motif-containing 29 (TRIM29) is a novel marker for lymph node
metastasis in gastric cancer. Ann Surg Oncol. 14:2543–2549. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Santin AD, Zhan F, Bellone S, Palmieri M,
Cane S, Bignotti E, Anfossi S, Gokden M, Dunn D, Roman JJ, et al:
Gene expression profiles in primary ovarian serous papillary tumors
and normal ovarian epithelium: Identification of candidate
molecular markers for ovarian cancer diagnosis and therapy. Int J
Cancer. 112:14–25. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dyrskjøt L, Kruhøffer M, Thykjaer T,
Marcussen N, Jensen JL, Møller K and Ørntoft TF: Gene expression in
the urinary bladder: A common carcinoma in situ gene expression
signature exists disregarding histopathological classification.
Cancer Res. 64:4040–4048. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Travis WD, Brambilla E, Noguchi M,
Nicholson AG, Geisinger KR, Yatabe Y, Beer DG, Powell CA, Riely GJ,
Van Schil PE, et al: International association for the study of
lung cancer/american thoracic society/european respiratory society
international multidisciplinary classification of lung
adenocarcinoma. J Thorac Oncol. 6:244–285. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Goldstraw P, Crowley J, Chansky K, et al:
International Association for the Study of Lung Cancer
International Staging Committee; Participating Institutions: The
IASLC Lung Cancer Staging Project: Proposals for the revision of
the TNM stage groupings in the forthcoming (seventh) edition of the
TNM Classification of malignant tumours. J Thorac Oncol. 2:706–714.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Groome PA, Bolejack V, Crowley JJ, et al:
The IASLC Lung Cancer Staging Project: Validation of the proposals
for revision of the T, N, and M descriptors and consequent stage
groupings in the forthcoming (seventh) edition of the TNM
classification of Malignant Tumours. J Thorac Oncol. 2:694–705.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kwon MJ, Park S, Choi JY, Oh E, Kim YJ,
Park YH, Cho EY, Kwon MJ, Nam SJ, Im YH, et al: Clinical
significance of CD151 overexpression in subtypes of invasive breast
cancer. Br J Cancer. 106:923–930. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Suzuki S, Miyazaki T, Tanaka N, Sakai M,
Sano A, Inose T, Sohda M, Nakajima M, Kato H and Kuwano H:
Prognostic significance of CD151 expression in esophageal squamous
cell carcinoma with aggressive cell proliferation and invasiveness.
Ann Surg Oncol. 18:888–893. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yuan Z, Villagra A, Peng L, Coppola D,
Glozak M, Sotomayor EM, Chen J, Lane WS and Seto E: The ATDC
(TRIM29) protein binds p53 and antagonizes p53-mediated functions.
Mol Cell Biol. 30:3004–3015. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sho T, Tsukiyama T, Sato T, Kondo T, Cheng
J, Saku T, Asaka M and Hatakeyama S: TRIM29 negatively regulates
p53 via inhibition of Tip60. Biochim Biophys Acta. 1813:1245–1253.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shibata MA, Yoshidome K, Shibata E, Jorcyk
CL and Green JE: Suppression of mammary carcinoma growth in vitro
and in vivo by inducible expression of the Cdk inhibitor p21.
Cancer Gene Ther. 8:23–35. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kanno Y, Watanabe M, Kimura T, Nonomura K,
Tanaka S and Hatakeyama S: TRIM29 as a novel prostate basal cell
marker for diagnosis of prostate cancer. Acta Histochem.
116:708–712. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liu J, Welm B, Boucher KM, Ebbert MT and
Bernard PS: TRIM29 functions as a tumor suppressor in
nontumorigenic breast cells and invasive ER+breast cancer. Am J
Pathol. 180:839–847. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fristrup N, Birkenkamp-Demtröder K,
Reinert T, Sanchez-Carbayo M, Segersten U, Malmström PU, Palou J,
Alvarez-Múgica M, Pan CC, Ulhøi BP, et al: Multicenter validation
of cyclin D1, MCM7, TRIM29 and UBE2C as prognostic protein markers
in non-muscle-invasive bladder cancer. Am J Pathol. 182:339–349.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tang ZP, Cui QZ, Dong QZ, Xu K and Wang
EH: Ataxia-telangiectasia group D complementing gene (ATDC)
upregulates matrix metalloproteinase 9 (MMP-9) to promote lung
cancer cell invasion by activating ERK and JNK pathways. Tumour
Biol. 34:2835–2842. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang L, Yang H, Palmbos PL, Ney G, Detzler
TA, Coleman D, Leflein J, Davis M, Zhang M, Tang W, et al:
ATDC/TRIM29 phosphorylation by ATM/MAPKAP kinase 2 mediates
radioresistance in pancreatic cancer cells. Cancer Res.
74:1778–1788. 2014. View Article : Google Scholar : PubMed/NCBI
|