Introduction
Gastric adenocarcinoma is a prevalent disease that
accounts for ~10% of cancers worldwide (1). In recent decades, advances in surgical
treatment, postoperative care and multimodality therapy have
yielded modest improvements in the prognosis of the disease.
Gastric adenocarcinoma is considered a heterogeneous disease
exhibiting multiple epidemiological and histopathological
characteristics (2). However, the
uniform treatment of the disease disregards the histological
subtypes of adenocarcinoma. The molecular study of gastric cancer
may clarify the pathogenesis of tumors and facilitate the
identification of alternative forms of effective treatment.
Positive transcriptional elongation factor b
(P-TEFb) is a complex that contains the catalytic subunit,
cyclin-dependent kinase 9 (CDK9), and the regulatory subunit,
cyclin T. Cyclin T contains subunits T1, T2a and T2b. In general,
CDK9 consists of a complex of T1, T2a and T2b at ratios of ~80%,
10% and 10%, respectively (3–5). The expression pattern of cyclin T2a
almost completely overlaps the pattern described for cyclin T1
(5). The expression of cyclin T1
increases CDK9 activity and the phosphorylation of RNA polymerase
II (RNAPII). The hypophosphorylated carboxyl-terminal domain of
RNAPII instigates the elongation phase of transcription (6), thus enabling RNAPII to escape from
promoter-proximal pausing factors in pre-mRNA processing (7).
P-TEFb has been thoroughly investigated in cardiac
hypertrophy and HIV infection. Interaction with human cyclin T1 is
required for the transcriptional activation of HIV-1. The
interaction forms a complex with P-TEFb, which increases the RNAPII
number (8). In addition, the CDK
inhibitor, flavopiridol, was reported to exhibit certain
therapeutic qualities (9). However,
hypertrophic signals may activate CDK9 and the consequent
phosphorylation of RNAPII. This effect not only increases RNA
synthesis but also enlarges myocytes. This potentially results in
cardiac hypertrophy (6,7). A previous study suggests that P-TEFb and
transcriptional elongation play crucial roles in protecting normal
and cancer cells from apoptosis (10). CDK9 inhibitors are generally
considered potential therapeutic agents in chronic lymphocytic
leukemia (11) and lung
adenocarcinoma (12). Cyclin T1 and
CDK9 are also overexpressed in the cell lines of human head and
neck carcinoma (3).
Clinical studies have identified the expression of
cyclin A, B1, D1 and E in gastric adenocarcinoma. Cyclin D1 and E
are the key regulators of progression through the G1 phase of the
cell cycle (13,14). Overexpression of cyclin D1 and E is
considered an early biomarkers of gastric cancer (15). The overexpression of cyclin E has been
considered alternatively as a favorable, poor and irrelevant
prognostic factor in clinical outcome (16). Cyclin A may be activated during the
transition from the G1 to the S phase of the cell cycle (17,18).
Cyclin B1 regulates cell progression through the G2 and M phase.
Overexpression of cyclin B1 is associated with tumor progression
and poor prognosis (19). However,
there are few effective clinical predictors for gastric
adenocarcinoma. This study, therefore, assessed the clinical
significance of cyclin T1 and CDK9 expression in gastric
adenocarcinoma.
Materials and methods
Tissues and patients
Tests were conducted on 39 gastric adenocarcinoma
patients, all of whom had received either radical total or distal
gastrectomy during the period from 2008 to 2011 from the same team
at Tungs' Taichung Metro Harbor Hospital, Taiwan. Normal gastric
tissues were collected from 16 other patients. Twenty-two of the
patients received postoperative adjuvant chemotherapy. The
patients' medical charts, pathological reports and surgical notes
were retrospectively reviewed. The pathological diagnoses in these
cases were reviewed by at least two experienced pathologists. The
Tumor-Node-Metastasis (TNM) system was used according to the
seventh edition of the AJCC cancer staging manual (20). As recognized in the 2010 World Health
Organization classification, there are four major histological
patterns of gastric cancers: tubular, papillary, mucinous and
poorly differentiated signet ring cell carcinoma (21). The specimens were fixed in formalin
and embedded in paraffin wax; the fixed paraffin was then cut into
3-µm sections.
Ethics
This study was approved by the Institutional Review
Board of the Tungs' Taichung Metro Harbor Hospital (approval number
100006). All patients included in the study were informed of the
involved procedures and provided written consent prior to the
collection of all specimens and clinical information.
Immunohistochemical staining
Slides were stained with the CDK9 monoclonal
antibody and the cyclin T1 polyclonal antibody using the Bond-Max
autostainer (Leica Microsystems, Melbourne, Australia). Table I lists the details of these
immunomarkers, including methods of pretreatment for antigen
retrieval. In brief, formalin-fixed and paraffin-embedded tissue
specimens were introduced to Tris-buffered saline and Tween-20.
They were then rehydrated through serial dilutions of alcohol,
before being washed in phosphate-buffered saline (pH 7.2). Coated
slides were then stained with the aforementioned antibodies. This
procedure was performed on the fully automated Bond-Max system
using onboard heat-induced antigen retrieval and a Leica Refine
polymer detection system (Leica Microsystems). Diaminobenzidine was
used as the chromogen (Leica Microsystems) in all immunostainings.
Negative controls were obtained by excluding the primary antibody,
and appropriate positive controls were applied throughout the
study. Finally, the slides were mounted with gum for examination,
and the images of each slide were captured using the Olympus BX51
microscope/DP71 digital camera system (Ina-shi, Nagano, Japan) for
comparison.
 | Table I.Antibodies used in study. |
Table I.
Antibodies used in study.
| Antigen | Clone | Product code | Antibody class | Supplier | Dilution | Antigen
retrieval |
|---|
| Cyclin T1 | Rabbit
polyclonal | ab2098 | IgG | Abcam | 1:500 | ER1 20 min |
| CDK9 | Rabbit
monoclonal | 2454-1 | IgG | Epitomics | 1:500 | ER2 20 min |
To assess CDK9 and cyclin T1 expression, the
intensity of immunostaining was scored on a scale of 0 (no
staining) to 4 (strongest intensity). The percentage of cell
staining at each intensity level was estimated from 0 to 100. The
percentage of cells at each intensity level was then multiplied by
the corresponding intensity value, thus providing an immunostaining
score ranging from 0 to 400.
Statistical analysis
Twenty-five patients with a cyclin T1 score ≤180
were defined as having low expression. Fourteen patients with
cyclin T1 scores >180 were defined as having high expression.
Seventeen patients with a CDK9 score ≤240 were defined as having
low expression. Twenty-two patients with CDK9 scores >240 were
defined as having high expression.
The disease-free survival (DFS) rates of patients
were analyzed by applying Kaplan-Meier estimates and compared
according to the log-rank test. The DFS rate was defined as the
interval between the date of surgery and the date of tumor
recurrence or distant metastasis. Cox regression methods were used
to determine the correlation among survival, clinical parameters
and immunohistochemical variables in multivariate models.
The differences between positive and negative cyclin
T1 or CDK9 stains were analyzed using Mann-Whitney U-tests. All
statistical tests were two-sided. P<0.05 was considered to
indicate a statistically significant difference between groups.
The results of immunohistochemical staining
intensity, the percentage of tumor staining and the total score are
expressed as the mean ± standard errors of the mean. Statistical
analysis was performed using a nonparametric Chi-square test, and
P<0.05 was considered to indicate a statistically significant
difference. All analyses were performed using the SPSS 16.0
software package (SPSS, Inc., Chicago, IL, USA).
Results
In this study, 39 patients were examined. The mean
age was 67.4 years, and the group included 13 patients of 60 years
old or less and 26 patients over 60 years old. Among the patients,
25 were male and 14 were female. A total of 19 patients developed
tumor recurrence or distant metastasis during the study, and 22
received postoperative adjuvant chemotherapy. The other patients
did not receive postoperative adjuvant chemotherapy.
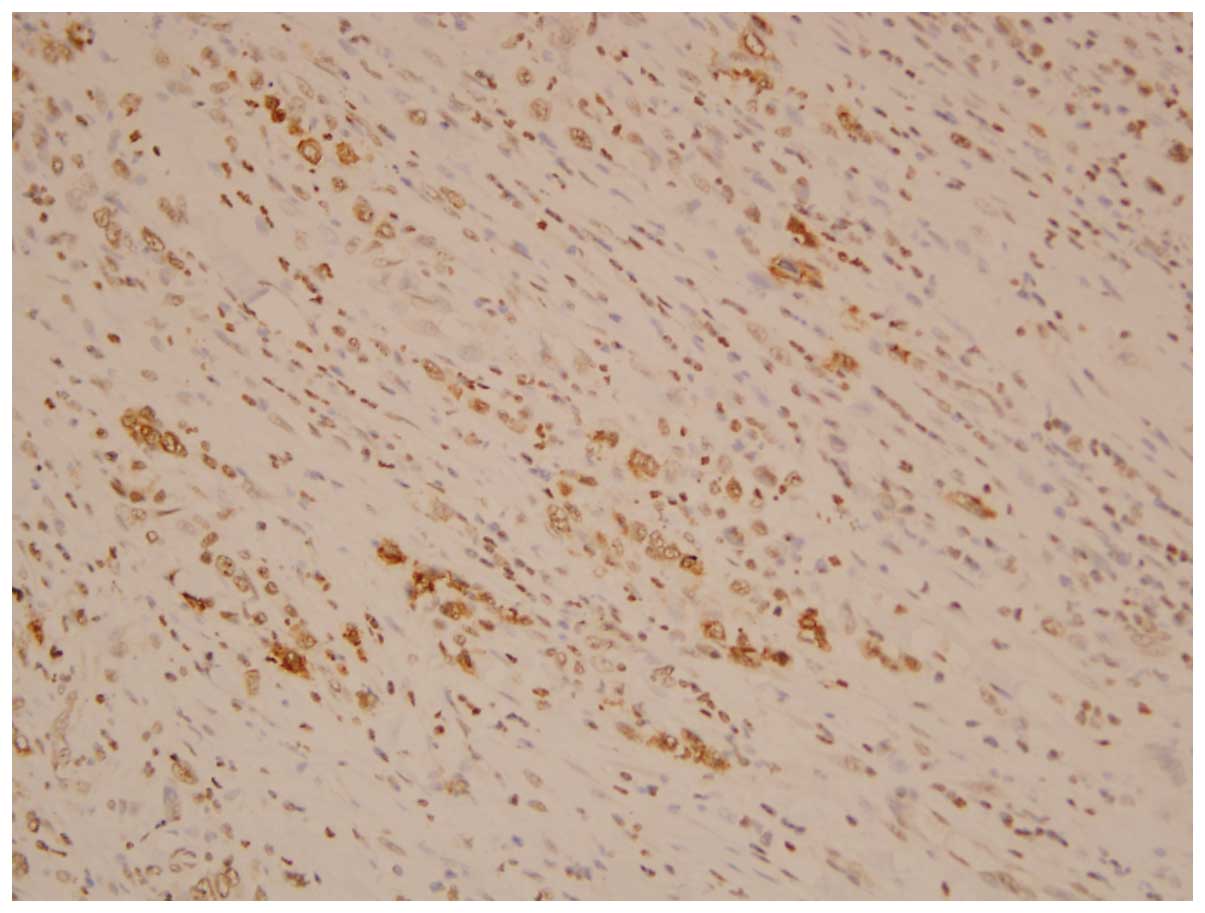
Among the 19 patients with tumor-recurrent or
distant metastasis, 16 exhibited low cyclin T1 expression (score
≤180) and only 3 exhibited high cyclin T1 expression (score
>180) (Fig. 1). The DFS rates were
analyzed using the univariate log-rank test and the multivariate
stepwise Cox-regression test. Higher T stage, higher N stage,
higher tumor grade and lower cyclin T1 scores in the univariate
analysis revealed poorer clinical outcomes. The Kaplan-Meier
survival curve demonstrated that the DFS rate of patients with low
expression of cyclin T1 was significantly lower than that of
patients with higher expression of cyclin T1 (P=0.028, Fig. 2). In addition, the differential DFS
rate among T stage, N stage, tumor grade and cyclin T1 expression
was significant, based on multivariate analysis. The
clinicopathological features of the univariate and multivariate
analyses are summarized in Table II.
The cyclin T1 score was also analyzed in association with other
clinicopathological factors. No significant difference was observed
between the two subgroups, except with regard to the histological
subtype. Tubular-type adenocarcinoma demonstrated a significantly
higher cyclin T1 expression. A summary of the correlation between
cyclin T1 staining scores and other clinicopathological factors is
shown in Table III.
 | Table II.Univariate log-rank and multivariate
Cox analyses for prognostic factors with respect to disease-free
survival. |
Table II.
Univariate log-rank and multivariate
Cox analyses for prognostic factors with respect to disease-free
survival.
|
|
|
|
| P-value |
|---|
|
|
|
|
|
|
|---|
| Parameters | Category | No. of cases | No. of events | Univariate | Multivariate |
|---|
| Gender | Male | 25 | 14 | 0.244 |
|
|
| Female | 14 | 5 |
|
|
| Age | ≤60 | 13 | 6 | 0.303 |
|
|
| >60 | 26 | 13 |
|
|
| Cell type | Tubular | 14 | 5 | 0.268 |
|
|
| Papillary | 7 | 4 |
|
|
|
| Mucinous | 3 | 1 |
|
|
|
| Signet ring | 15 | 9 |
|
|
| T stage | 1 | 1 | 0 | 0.018a | 0.581 |
|
| 2 | 14 | 5 |
|
|
|
| 3 | 16 | 8 |
|
|
|
| 4 | 8 | 6 |
|
|
| N stage | 0 | 7 | 2 | 0.040a | 0.083 |
|
| 1 | 13 | 7 |
|
|
|
| 2 | 8 | 2 |
|
|
|
| 3 | 11 | 8 |
|
|
| Grade | 1 | 0 | 0 |
<0.0001a | 0.007a |
|
| 2 | 12 | 6 |
|
|
|
| 3 | 23 | 9 |
|
|
|
| 4 | 4 | 4 |
|
|
| CDK9 score | ≤240 | 17 | 10 | 0.549 |
|
|
| >240 | 22 | 9 |
|
|
| Cyclin T1
score | ≤180 | 25 | 16 | 0.028a | 0.033a |
|
| >180 | 14 | 3 |
|
|
 | Table III.Association of cyclin T1 with various
clinicopathological parameters. |
Table III.
Association of cyclin T1 with various
clinicopathological parameters.
|
|
|
| Cyclin T1
score |
|
|---|
|
|
|
|
|
|
|---|
| Parameters | Category | No. of cases | ≤180 | >180 | P-value |
|---|
| Cell type | Tubular | 14 | 4 | 10 | 0.004a |
|
| Papillary | 7 | 6 | 1 |
|
|
| Mucinous | 3 | 2 | 1 |
|
|
| Signet ring | 15 | 13 | 2 |
|
| Age | ≤60 | 13 | 9 | 4 | 0.733 |
|
| >60 | 26 | 16 | 10 |
|
| Gender | Male | 25 | 17 | 8 | 0.741 |
|
| Female | 14 | 8 | 6 |
|
| T stage | 1 | 1 | 1 | 0 | 0.302 |
|
| 2 | 14 | 7 | 7 |
|
|
| 3 | 16 | 10 | 6 |
|
|
| 4 | 8 | 7 | 1 |
|
| N stage | 0 | 7 | 4 | 3 | 0.967 |
|
| 1 | 13 | 9 | 4 |
|
|
| 2 | 8 | 5 | 3 |
|
|
| 3 | 11 | 7 | 4 |
|
| Grade | 1 | 0 | 0 | 0 | 0.544 |
|
| 2 | 12 | 9 | 3 |
|
|
| 3 | 23 | 13 | 10 |
|
|
| 4 | 4 | 3 | 1 |
|
| CDK9 score | ≤240 | 17 | 13 | 4 | 0.281 |
|
| >240 | 22 | 12 | 10 |
|
The immunostaining scores of cyclin T1 and CDK9 in
gastric adenocarcinoma and normal gastric epithelia are shown in
Tables IV and V. The staining percentages and total scores
of cyclin T1, but not CDK9, were significantly higher in the
adenocarcinoma group than in the normal stomach epithelia group.
The immunostaining scores of cyclin T1 and CDK9 for the four
histological subtypes of gastric adenocarcinoma are shown in
Tables VI and VII. These results reveal that the
intensity of cyclin T1 and CDK9 is higher in tubular-type stomach
adenocarcinoma than in its papillary-type equivalent.
 | Table IV.Cyclin T1 immunostaining scores in
gastric adenocarcinoma and normal tissue. |
Table IV.
Cyclin T1 immunostaining scores in
gastric adenocarcinoma and normal tissue.
|
| Cyclin T1 |
|---|
|
|
|
|---|
| Tissue | Intensity | % staining | Total score |
|---|
| Adenocarcinoma
(n=39) | 2.00±1.17 | 73.72±27.57 | 158.72±114.76 |
| Normal gastric
epithelia (n=16) | 1.19±1.11 |
17.50±18.80a |
36.87±39.62a |
 | Table V.CDK9 immunostaining scores in gastric
adenocarcinoma and normal tissue. |
Table V.
CDK9 immunostaining scores in gastric
adenocarcinoma and normal tissue.
|
| CDK9 |
|---|
|
|
|
|---|
| Tissue | Intensity | % staining | Total score |
|---|
| Adenocarcinoma
(n=39) | 2.77±1.29 | 72.69±32.48 |
237.95±132.37 |
| Normal gastric
epithelia (n=16) | 3.19±0.98 | 75.00±22.51 | 255.63±88.62 |
 | Table VI.Cyclin T1 immunostaining scores in
gastric adenocarcinoma tissue. |
Table VI.
Cyclin T1 immunostaining scores in
gastric adenocarcinoma tissue.
|
| Cyclin T1 |
|---|
|
|
|
|---|
| Histological
type | Intensity | % staining | Total score |
|---|
| Tubular (n=14) | 2.57±0.94 | 83.21±24.78 |
220.00±108.63 |
| Papillary
(n=7) |
1.29±0.76a | 71.43±26.10 | 100.00±91.10 |
| Mucinous (n=3) | 1.67±0.58 | 66.67±35.12 | 123.33±86.22 |
| Signet ring
(n=15) | 1.87±1.41 | 67.33±29.63 |
136.00±117.77 |
 | Table VII.CDK9 immunostaining scores in gastric
adenocarcinoma. |
Table VII.
CDK9 immunostaining scores in gastric
adenocarcinoma.
|
| CDK9 |
|---|
|
|
|
|---|
| Histological
type | Intensity | % staining | Total score |
|---|
| Tubular (n=14) | 3.36±0.63 | 88.57±12.77 | 302.86±89.99 |
| Papillary
(n=7) |
1.57±1.62a | 50.00±47.61 |
141.43±155.40 |
| Mucinous (n=3) | 2.33±2.08 | 60.00±51.96 |
210.00±187.35 |
| Signet ring
(n=15) | 2.87±1.13 | 71.00±28.42 |
228.00±124.63 |
Discussion
In this study, T stage, N stage, tumor grade and
cyclin T1 staining score were identified as recurrent prognostic
factors of postsurgical resection in gastric adenocarcinoma.
Univariate and multivariate analysis results demonstrated a
significant difference in DFS rates between patients with high and
low expression of cyclin T1. Other than T stage, N stage and tumor
grade, alternative negative prognostic factors, including
overexpression of cyclin A, B1, D1 and E (13–16) were
also observed.
The correlation between the cyclin T1 staining score
and various other factors was also analyzed. The immunostaining
score of tubular-type adenocarcinoma was noted to be significantly
higher than that of other types of stomach adenocarcinoma.
A previous study has revealed that upregulation of
the CDK9/cyclin T1 complex contributes to T lymphocyte
differentiation and malignant transformation (22). Regulation of the CDK9/cyclin T1
complex depends on its tissue-specific signaling pathway (23) and its response to cytokines including
tumor necrosis factor and interleukin-6 (5,24).
Deregulated CDK9-related pathways were observed in several human
tumors including lymphoma (23,25,26),
neuroblastoma (27), prostate cancer
(28) and several instances of
hematopoietic malignancy (23). These
studies have suggested that cyclin T1 and CDK9 may promote the
expression of anti-apoptotic factors and induce proliferation
(11,29,30). By
contrast, an alternative study has demonstrated that cyclin T1, but
not CDK9, induces the in vitro transformation of head and
neck tumors (3). Upregulation of
cyclin T1 is the main mechanism for the activation of the complex
during T cell activation, and cyclin T1 acts as a rate-limiting
subunit (31). Furthermore, our
results reveal that cyclin T1, but not CDK9, is a potential
prognostic factor for improving the DFS rate of gastric
adenocarcinoma. However, it is possible that it may also induce
malignant transformation.
Our results confirm that cyclin T1 plays a
regulatory role in the CDK9/cyclin T complex and that the
upregulation of cyclin T1 is the main mechanism in the activation
of this complex. Our results also support that cyclin T1 acts as a
rate-limiting positive regulatory subunit (31).
In contrast to previous studies (3,17,18,31) that
have suggested that the overexpression of cyclin T1 is a poor
prognostic factor, our results indicate that low cyclin T1
expression is a poor prognostic factor in treating stomach
adenocarcinoma. Patterns of CDK9 and cyclin T1 expression were
observed to be similar in normal organ tissue, yet quite different
in other tissues (5). Cyclin T1 was
expressed in a wide variety of human tissues. The tissue of
mesenchymal organs, including connective tissue, skeletal muscle,
blood and lymphoid tissue, exhibits high levels of cyclin T1
expression (4,5). In addition, cyclin T1 is not considered
a typical cell cycle regulator as its levels do not oscillate in
any phase during the cell cycle (4).
Moreover, upregulation of cyclin T1 has not been linked directly to
cell cycle entry or progression (4).
In different tissues, the expression of cyclin T1 plays a different
role in tumor behavior. Deregulation of cyclin T1 contributes to a
poor outcome, and negative cyclin T1 expression is a potentially
less favorable factor.
There were limitations to this study. The subgroups
of patients were too small for individual subtype analysis. A study
with a larger sample size is necessary for further differentiation
of the predictors. In addition, in vitro cell molecular
studies would have enabled identification of the cyclin T1 pathway.
This was a pilot study to determine whether cyclin T1 could be
considered for further studies including more patients and cell
lines to confirm the role of the CDK9/cyclin T1 complex in gastric
adenocarcinoma.
In conclusion, the results of this study confirm the
hypothesis that high expression of cyclin T1 is a favorable
prognostic factor in stomach adenocarcinoma.
Acknowledgements
This study was supported by grant TTMHH-100R0004
from Tungs' Taichung Metro Harbor Hospital.
References
|
1
|
Ferlay J, Bray F, Pisani P and Parkin M:
GLOBOCAN 2002: cancer incidence, mortality and prevalence
worldwide. Lyon: IARC Press. 2004.
|
|
2
|
Shah MA, Khanin R, Tang L, Janjigian YY,
Klimstra DS, Gerdes H and Kelsen DP: Molecular classification of
gastric cancer: a new paradigm. Clin Cancer Res. 17:2693–2701.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Moiola C, De Luca P, Gardner K, Vazquez E
and De Siervi A: Cyclin T1 overexpression induces malignant
transformation and tumor growth. Cell Cycle. 9:3119–3126. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
De Luca A, De Falco M, Baldi A and Paggi
MG: Cyclin T: three forms for different roles in physiological and
pathological functions. J Cell Physiol. 194:101–107. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
De Luca A, Russo P, Severino A, Baldi A,
Battista T, Cavallotti I, De Luca L, Baldi F, Giordano A and Paggi
MG: Pattern of expression of cyclin T1 in human tissues. J
Histochem Cytochem. 49:685–692. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sano M and Schneider MD: Cyclin-dependent
kinase-9: an RNAPII kinase at the nexus of cardiac growth and death
cascades. Circ Res. 95:867–876. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sano M, Wang SC, Shirai M, Scaglia F, Xie
M, Sakai S, Tanaka T, Kulkarni PA, Barger PM, Youker KA, et al:
Activation of cardiac Cdk9 represses PGC-1 and confers a
predisposition to heart failure. EMBO J. 23:3559–3569. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chiu YL, Cao H, Jacque JM, Stevenson M and
Rana TM: Inhibition of human immunodeficiency virus type 1
replication by RNA interference directed against human
transcription elongation factor P-TEFb (CDK9/CyclinT1). J Virol.
78:2517–2529. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chao SH and Price DH: Flavopiridol
inactivates P-TEFb and blocks most RNA polymerase II transcription
in vivo. J Biol Chem. 276:31793–31799. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Napolitano G, Majello B and Lania L: Role
of cyclinT/Cdk9 complex in basal and regulated transcription
(review). Int J Oncol. 21:171–177. 2002.PubMed/NCBI
|
|
11
|
Chen R, Keating MJ, Gandhi V and Plunkett
W: Transcription inhibition by flavopiridol: mechanism of chronic
lymphocytic leukemia cell death. Blood. 106:2513–2519. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shan B, Zhuo Y, Chin D, Morris CA, Morris
GF and Lasky JA: Cyclin-dependent kinase 9 is required for tumor
necrosis factor-alpha-stimulated matrix metalloproteinase-9
expression in human lung adenocarcinoma cells. J Biol Chem.
280:1103–1011. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sugai T, Tsukahara M, Endoh M, Shioi Y,
Takebe N, Mue Y, Matsushita H, Toyota M and Suzuki K: Analysis of
cell cycle-related proteins in gastric intramucosal
differentiated-type cancers based on mucin phenotypes: a novel
hypothesis of early gastric carcinogenesis based on mucin
phenotype. BMC Gastroenterol. 10:552010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ioachim E: Expression patterns of cyclins
D1, E and cyclin-dependent kinase inhibitors p21waf1/cip1, p27kip1
in colorectal carcinoma: correlation with other cell cycle
regulators (pRb, p53 and Ki-67 and PCNA) and clinicopathological
features. Int J Clin Pract. 62:1736–1743. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Motohashi M, Wakui S, Muto T, Suzuki Y,
Shirai M, Takahashi H and Hano H: Cyclin D1/cdk4, estrogen
receptors α and β, in N-methyl-N'-nitro-N-nitrosoguanidine-induced
rat gastric carcinogenesis: immunohistochemical study. J Toxicol
Sci. 36:373–378. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kouraklis G, Katsoulis IE, Theocharis S,
Tsourouflis G, Xipolitas N, Glinavou A, Sioka C and Kostakis A:
Does the expression of cyclin E, pRb and p21 correlate with
prognosis in gastric adenocarcinoma? Dig Dis Sci. 54:1015–1020.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li JQ, Miki H, Wu F, Saoo K, Nishioka M,
Ohmori M and Imaida K: Cyclin A correlates with carcinogenesis and
metastasis and p27(kip1) correlates with lymphatic invasion, in
colorectal neoplasms. Hum Pathol. 33:1006–1015. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mrena J, Wiksten JP, Kokkola A, Nordling
S, Haglund C and Ristimäki A: Prognostic significance of cyclin A
in gastric cancer. Int J Cancer. 119:1897–1901. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yasuda M, Takesue F, Inutsuka S, Honda M,
Nozoe T and Korenaga D: Overexpression of cyclin B1 in gastric
cancer and its clinicopathological significance: an
immunohistological study. J Cancer Res Clin Oncol. 128:412–416.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Washington K: 7th edition of the AJCC
cancer staging manual: Stomach. Ann Surg Oncol. 17:3077–3079. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Berlth F, Bollschweiler E, Drebber U,
Hoelscher AH and Moenig S: Pathohistological classification systems
in gastric cancer: Diagnostic relevance and prognostic value. World
J Gastroenterol. 20:5679–5684. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Leucci E, De Falco G, Onnis A, Cerino G,
Cocco M, Luzzi A, Crupi D, Tigli C, Bellan C, Tosi P, et al: The
role of the Cdk9/Cyclin T1 complex in T cell differentiation. J
Cell Physiol. 212:411–415. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bellan C, De Falco G, Lazzi S, Micheli P,
Vicidomini S, Schürfeld K, Amato T, Palumbo A, Bagella L, Sabattini
E, et al: CDK9/CYCLIN T1 expression during normal lymphoid
differentiation and malignant transformation. J Pathol.
203:946–952. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
MacLachlan TK, Sang N, De Luca A, Puri PL,
Levrero M and Giordano A: Binding of CDK9 to TRAF2. J Cell Biochem.
71:467–478. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fu TJ, Peng J, Lee G, Price DH and Flores
O: Cyclin K functions as a CDK9 regulatory subunit and participates
in RNA polymerase II transcription. J Biol Chem. 274:34527–34530.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bettayeb K, Tirado OM, Marionneau-Lambot
S, Ferandin Y, Lozach O, Morris JC, Mateo-Lozano S, Drueckes P,
Schächtele C, Kubbutat MH, et al: Meriolins, a new class of cell
death inducing kinase inhibitors with enhanced selectivity for
cyclin-dependent kinases. Cancer Res. 67:8325–8334. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
De Falco G and Giordano A: CDK9: From
basal transcription to cancer and AIDS. Cancer Biol Ther.
1:342–377. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lee DK, Duan HO and Chang C: Androgen
receptor interacts with the positive elongation factor P-TEFb and
enhances the efficiency of transcriptional elongation. J Biol Chem.
276:9978–9984. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Peng J, Zhu Y, Milton JT and Price DH:
Identification of multiple cyclin subunits of human P-TEFb. Genes
Dev. 12:755–762. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Napolitano G, Majello B, Licciardo P,
Giordano A and Lania L: Transcriptional activity of positive
transcription elongation factor b kinase in vivo requires the
C-terminal domain of RNA polymerase II. Gene. 254:139–145. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Garriga J, Peng J, Parreño M, Price DH,
Henderson EE and Graña X: Upregulation of cyclin T1/CDK9 complexes
during T cell activation. Oncogene. 17:3093–3102. 1998. View Article : Google Scholar : PubMed/NCBI
|