Introduction
Breast hamartoma is an uncommonly reported benign
breast lesion of uncertain cause and pathogenesis. The majority of
affected patients are >35 years old, with a mean age of ~45, and
the tumor exhibits a female predominance. Of all the benign breast
tumors in women (1–3), only 0.1–0.7% are diagnosed as breast
harmartomas. The diagnosis of breast hamartoma by a single method
such as mammography, magnetic resonance imaging or sonography is
inadequate. The tumor is often misdiagnosed as fibroadenoma, even
upon fine-needle aspiration (FNA). Therefore, the actual incidence
could be higher than that reported (4). This benign lesion grows slowly and could
become bigger if no intervention is given, which results in greater
trauma for the patient (5). In the
majority of cases, the breast hamartoma is excised a few years
after it has occurred, when it is not too big. In the present
study, however, a particularly large lesion with a long history is
described. Such a case has rarely been reported and shows the
necessity of early surgery. The study also presents a literature
review on breast hamartoma. Written informed consent was provided
by the patient for the publication of this case report and the
accompanying images.
Case report
A 41-year-old female with a 10-year-history of a
painless lump in the right breast presented to the First Affiliated
Hospital of Xi'an Jiaotong University (Shaanxi, China) in March
2014. The mass had been gradually increasing in size over this
period. The patient complained of significant pain in the right
breast during menstruation, which was relieved at its conclusion.
The risk of breast cancer was not increased, and the patient did
not have any of the familial factors. No history of ipsilateral
breast trauma, surgery or radiation exposure was reported. No
nipple discharge was apparent and no pyrexia was found in the
patient's case history.
Upon physical examination, an oval, palpable but
painless, smooth, rubbery mass of ~12×10 cm in size was found in
the upper outer quadrant of the right breast. The mass had neither
skin fixation nor fixation to adjacent structures in the breast,
and its most posterior margin could be defined. No skin ulceration
was found. The results of routine laboratory investigations were
within normal limits.
Mammograms showed a well-circumscribed mass lesion
of mixed density in the right breast. No ipsilateral axillary nodes
were detected. The serum level of cancer antigen 15-3 remained
normal. Ultrasound of the right breast revealed a solid
heterogeneous mass of 10×11 cm. The patient refused to undergo FNA
cytology examination.
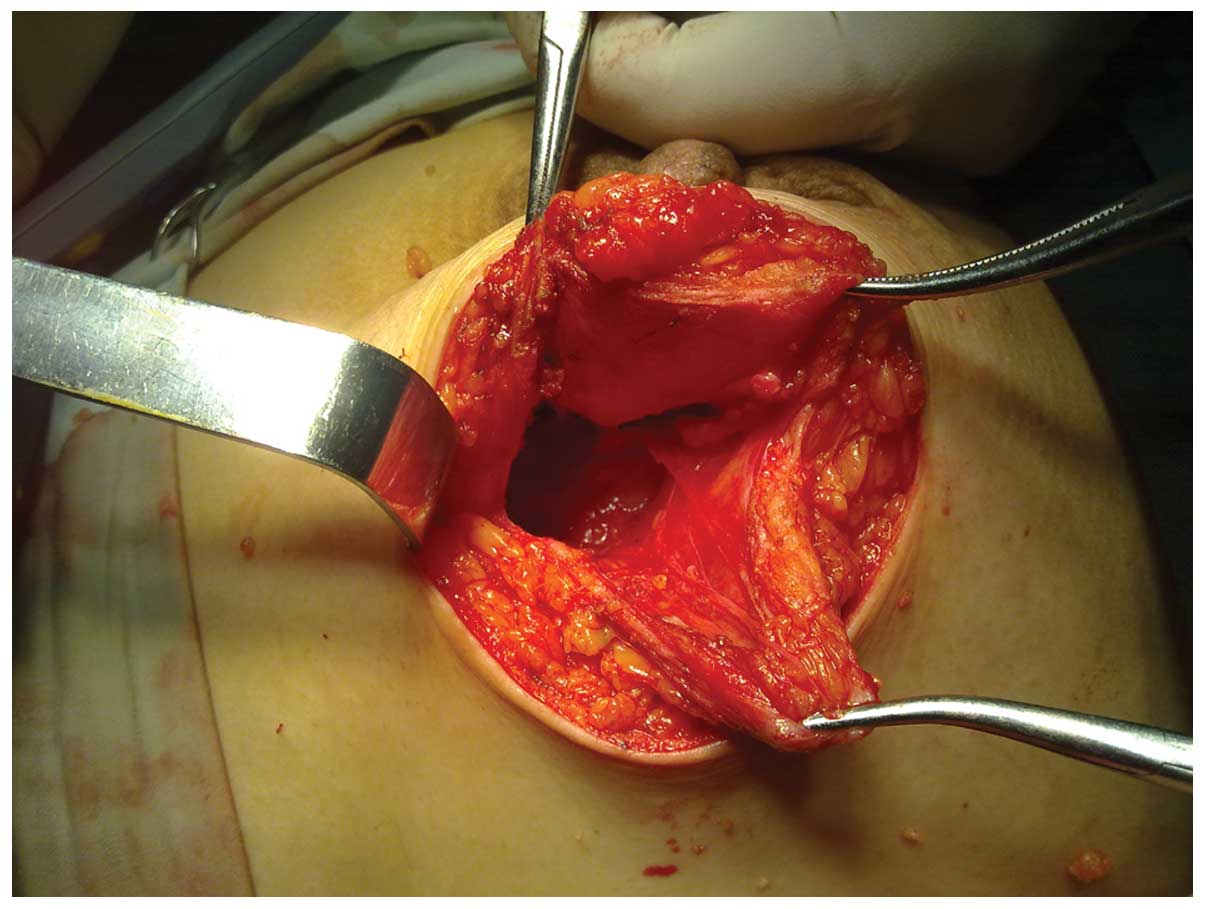
In order to achieve diagnostic and therapeutic
goals, a surgical treatment was planned. Excision of hamartoma was
successfully performed and a tumor of 11×9×3.5 cm was completely
excised (Fig. 1). Gross examination
revealed an oval, white-reddish, well-defined, encapsulated nodule
with a smooth margin. The nodule was soft and possessed a fibrotic
envelope at the time of surgery (Fig.
2). The cut surface was smooth and exhibited a grey-reddish
color. Adipocytic areas within a fibrotic stroma could be
observed.
The diagnosis of a hamartoma was confirmed by the
histological examination. Microscopically, no cells with atypia
were found. Fibroblastic-like and epithelioid-like cells admixed
with thin collagen fibers could be observed. After 3 months of
follow-up, no recurrence was reported.
Discussion
Breast hamartoma is defined as a well-circumscribed
benign lesion composed of glandular tissue, epithelial elements,
fibrous tissue and fat, which may be in normal or varying
proportions. The term ‘breast hamartoma’ was first coined by
Arrigoni et al in 1971 (1).
Affected patients are of all ages, but are mainly adults. A higher
predominance of tumors exists in females compared with males. The
histological structure of breast hamartoma indicates that the tumor
probably results from a dysgenetic factor rather than a tumorous
process, as recognized in the World Health Organization in 1981
(6). Although it is histologically
benign, in situ and infiltrating carcinomas may arise within
hamartomas (7–9). The pathology of hamartoma requires
elucidation. The definitive criteria also require identification by
pathologists, therefore, the true incidence of this tumor may be
underestimated. Fibroadenolipoma, myoid hamartoma and chondrolipoma
are histological variations of hamartomas, depending on the
proportion of normal breast tissue elements (2). Adipose tissue is commonly reported in
the majority of hamartoma cases. The presence of adipose tissue
suggests a diagnosis of a hamartoma, but its proportion varies
sharply from 5 to 90% of the lesion volume according to the
literature (10,11). Other histological characteristics,
including a pseudoangiomatous stroma and epithelial changes, have
been described in the literature (12). Although growing slowly, the tumor can
develop to a larger size and induce breast asymmetry if excision is
not performed in time. Small hamartomas are usually painless and
only present as slow-growing breast masses that do not attach to
the underlying structure of the breasts. However, large hamartomas
may be painful due to compression of the normal breast tissue.
The clinical diagnosis of hamartoma is based on the
findings from mammography, sonography and histology examinations.
The combination of these methods for the diagnosis is much better
than the use of a single method, which may lead to a misdiagnosis.
Mammographically, a breast hamartoma is a well-circumscribed mass
containing fat and soft tissue. The classic appearance of hamartoma
is, at least in part, a mass surrounded by a thin radiopaque line
(pseudocapsule), which can often be observed (13). A mammographical diagnosis is made
through such findings.
Sonographically, a well-defined mass with an
echogenic rim and internal heterogeneity is shown displacing the
adjacent normal breast tissue. The presence of a well-circumscribed
breast lesion with intact lobular units admixed with various
amounts of adipose tissue and a relative paucity of stroma in
aspirate form may support the diagnosis of hamartoma pathologically
(14). This feature is also useful to
differentiate the tumor from a fibroadenoma, with which it may
share a clinical and histological resemblance (15).
Lumpectomy is a curative method for hamartoma for
which only occasional recurrence has been reported. As a carcinoma
may arise within a hamartoma, excision is recommended when the
diagnosis is certified.
In conclusion, a hamartoma is a slow-growing,
uncommon breast lesion that possesses certain distinguishing
characteristics when mammography, sonography and histology are
combined. A definite diagnosis is hard to achieve through a single
examination technique. The correlation of imaging and histology
findings with the clinical impression is necessary. Although the
tumor is histologically benign and often painless, a hamartoma
could develop to quite a large size if local excision is not
performed in time. It should also be realized that although
hamartoma are benign, coincidental malignancy may occur. The
potential for recurrence is low, but has not been resolved.
References
|
1
|
Arrigoni MG, Dockerty MB and Judd ES: The
identification and treatment of mammary hamartomas. Surg Gynecol
Obstet. 133:577–582. 1971.PubMed/NCBI
|
|
2
|
Fisher CJ, Hanby AM, Robinson L and Millis
RR: Mammary hamartoma - a review of 35 cases. Histopathology.
20:99–106. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Daya D, Trus T, D'Souza TJ, Minuk T and
Yemen B: Hamartoma of the breast, an underrecognized breast lesion.
A clinicopathologic and radiographic study of 25 cases. Am J Clin
Pathol. 103:685–689. 1995.PubMed/NCBI
|
|
4
|
Fechner RE: Fibrodenoma and related
lesions. Diagnostic Histopathology of the Breast. Page DL and
Anderson TJ: (Edinburgh). Churchill Livingstone. 72–85. 1987.
|
|
5
|
Weinzweig N, Botts J and Marcus E: Giant
hamartoma of the breast. Plast Reconstr Surg. 107:1216–1220. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
World Health Organization: Histologic
typing of breast tumor. International histological classification
of tumors (2nd). (Washington, DC). Armed Forces Institute of
Pathology. 1991.
|
|
7
|
Scally N, Campbell W, Hall S, McCusker G
and Stirling WJ: Invasive ductal carcinoma arising within a breast
hamartoma. Ir J Med Sci. 180:767–768. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kai M, Tada K, Tamura M, Gomi N, Horii R,
Akiyama F and Iwase T: Breast cancer associated with mammary
hamartoma. Breast Cancer. 19:183–186. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mester J, Simmons RM, Vazquez MF and
Rosenblatt R: In situ and infiltrating ductal carcinoma arising in
a breast hamartoma. AJR Am J Roentgenol. 175:64–66. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jones MW, Norris HJ and Wargotz ES:
Hamartomas of the breast. Surg Gynecol Obstet. 173:54–56.
1991.PubMed/NCBI
|
|
11
|
Charpin C, Mathoulin MP, Andrac L,
Barberis J, Boulat J, Sarradour B, Bonnier P and Piana L:
Reappraisal of breast hamartomas. A morphological study of 41
cases. Pathol Res Pract. 190:362–371. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Herbert M, Schvimer M, Zehavi S, Mendlovic
S, Karni T, Pappo I and Sandbank J: Breast hamartoma: Fine-needle
aspiration cytologic finding. Cancer. 99:255–258. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Helvie MA, Adler DD, Rebner M and Oberman
HA: Breast hamartomas: Variable mammographic appearance. Radiology.
170:417–421. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Herbert M, Mendlovic S, Liokumovich P,
Segal M, Zahavi S, Rath-Wolfson L and Sandbank J: Can hamartoma of
the breast be distinguished from fibroadenoma using fine-needle
aspiration cytology? Diagn Cytopathol. 34:326–329. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Anani PA and Hessler C: Breast hamartoma
with invasive ductcarcinoma. Report of two cases and review of the
literature. Pathol Res Pract. 192:1187–1194. 1996. View Article : Google Scholar : PubMed/NCBI
|