Introduction
Kartagener's syndrome (KS) was initially described
in 1933 as the classical triad of situs inversus viscerum, chronic
sinusitis and bronchiectasis, in a series of four cases reported by
Katargener (1,2). Camner et al (3) was the first to suggest primary ciliary
dyskinesia (PCD) as the cause of KS in a report of two patients
with KS who presented ciliary dysfunction and immotile spermatozoa.
Afzelius and Eliasson (4) observed
ciliary ultrastructural changes resulting from this disease and the
absence of dynein arms in the respiratory ciliary axoneme and sperm
tail axoneme. According to various studies, KS is included in the
group of diseases arising from PCD, an autosomal recessive
disorder, and harmful factors in fetal period are etiological
factors of PCD and KS (4–7). The prevalence of PCD is estimated to be
1 in 10,000–20,000 and, as 50% of patients with PCD exhibit situs
inversus, the prevalence of KS is estimated to be 1 in
20,000–40,000. Around 95% of KS patients are diagnosed before the
age of 15 years. There is no significant difference with regard to
gender, however, evidence suggests the disease is associated with
familial factors and has a tendency towards heredity (8,9).
The present study reports the case of an adrenal
adenocarcinoma complicated by KS. To the best of our knowledge, KS
has not been previously described in a patient with adrenal
adenocarcinoma. The present study discusses the characteristics of
KS in the context of adrenal adenocarcinoma, and reports the
comprehensive treatment of the disease in the present case, with
the aim of increasing knowledge with regard to the diagnosis and
treatment of similar patients.
Case report
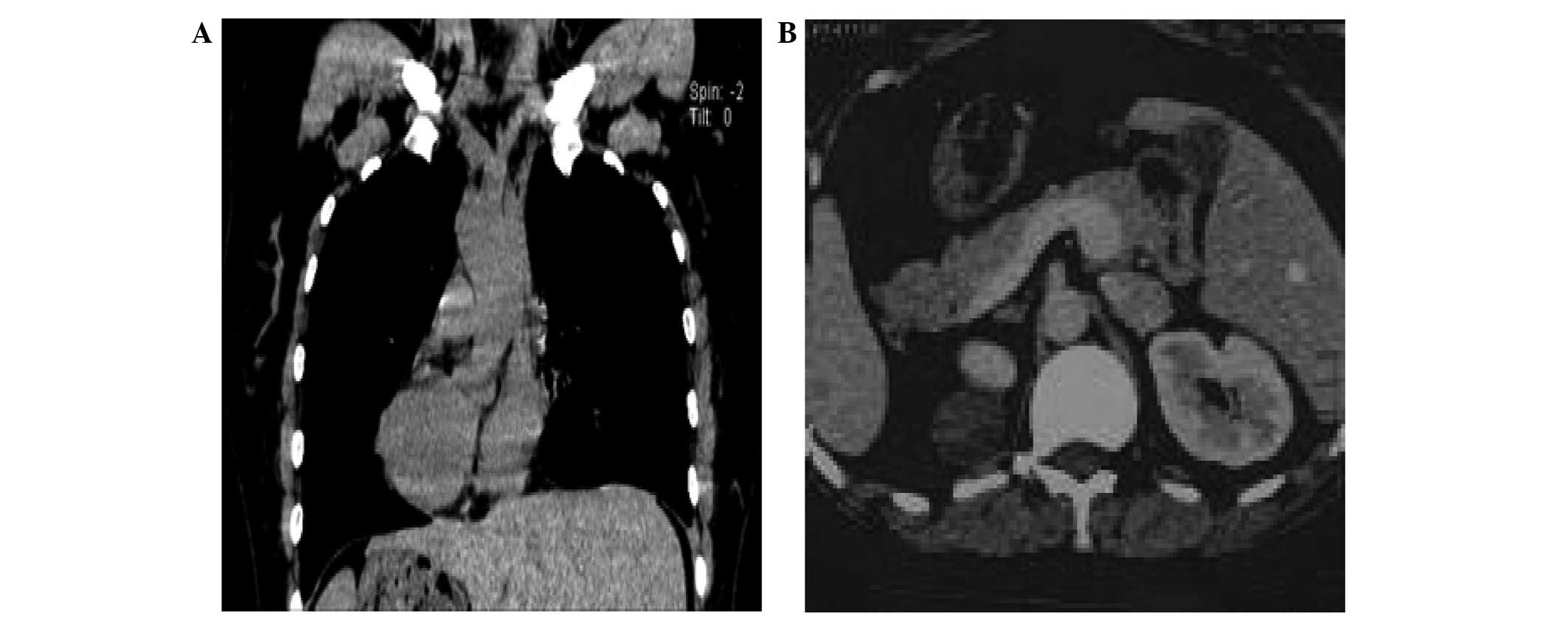
In October 2014, a 44-year-old woman was admitted to
Zhongnan Hospital (Wuhan, China) with an 8-week history of vertigo
and a recurrent cough, accompanied by sputum and a congested nose.
Hypertension (systolic, 140–160 mmHg) was detected by physical
examination, and a computed tomography (CT) scan of the abdomen 1
week prior to admission revealed an incidental 5.0×4.0 cm right
adrenal mass, as well as situs inversus. Chest roentgenography and
CT scan identified dextrocardia and chronic bronchitis of the lung,
with no bronchiectasis (Fig. 1). The
patient's blood aldosterone when standing was markedly increased
(308.50 pg/ml), while blood concentrations of potassium,
catecholamines and cortisol, as well as urinary excretion of
vanilmandelic acid were normal.
The patient exhibited the classical triad of KS
(situs inversus, chronic nasosinusitis and bronchiectasia), as well
as an underlying adrenal adenocarcinoma. The patient elected to
undergo laparoscopic right adrenal tumor resection and was
administered phenoxybenzamine [10 mg, three times/day (tid)] and
spironolactone (60 mg, tid) orally for one week, to control blood
pressure within the range of 120–130/80–90 mmHg prior to surgery.
Gentamicin (80,000 U), ambroxol hydrochloride (30 mg) and
dexamethasone (5 mg) were combined and administered as a spray
(once daily) to treat the cough and lung infection whilst the
patient remained on the waiting list for surgery.
A total of 12 days following admission to hospital,
preanesthetic evaluation with all tests had been performed in order
to prepare for safe anesthesia and surgery, and the operation was
performed using a retroperitoneal laparoscopic approach. Following
a preoperative intravenous dose of prophylactic antibiotics (2.5 g,
piperacillin-tazobactam), induction of general anesthesia was
achieved via administration of intravenous anesthetics (2.5 mg
midazolam; 80 mg propofol), followed by routine dosage of
vecuronium (6 mg) to facilitate endotracheal intubation. Routine
monitoring was established, including continuous
electrocardiography with mirror image placement of electrodes,
pulse oximetry, noninvasive blood pressure monitoring and
capnography.
Whilst under general anesthesia, the patient was
positioned in a left lateral decubitus. The skin was incised
longitudinally, below the twelfth costal arch, in the posterior
axillary line. Following blunt dissection of the subcutaneous
tissue, the lumbar muscle and fascia were identified and retracted.
The retroperitoneum was reached, and an initial digital dissection
was performed. Trocars were placed, and visualization of the
retroperitoneal space was achieved with the use of CO2
gas. Dissection was performed along the psoas muscle.
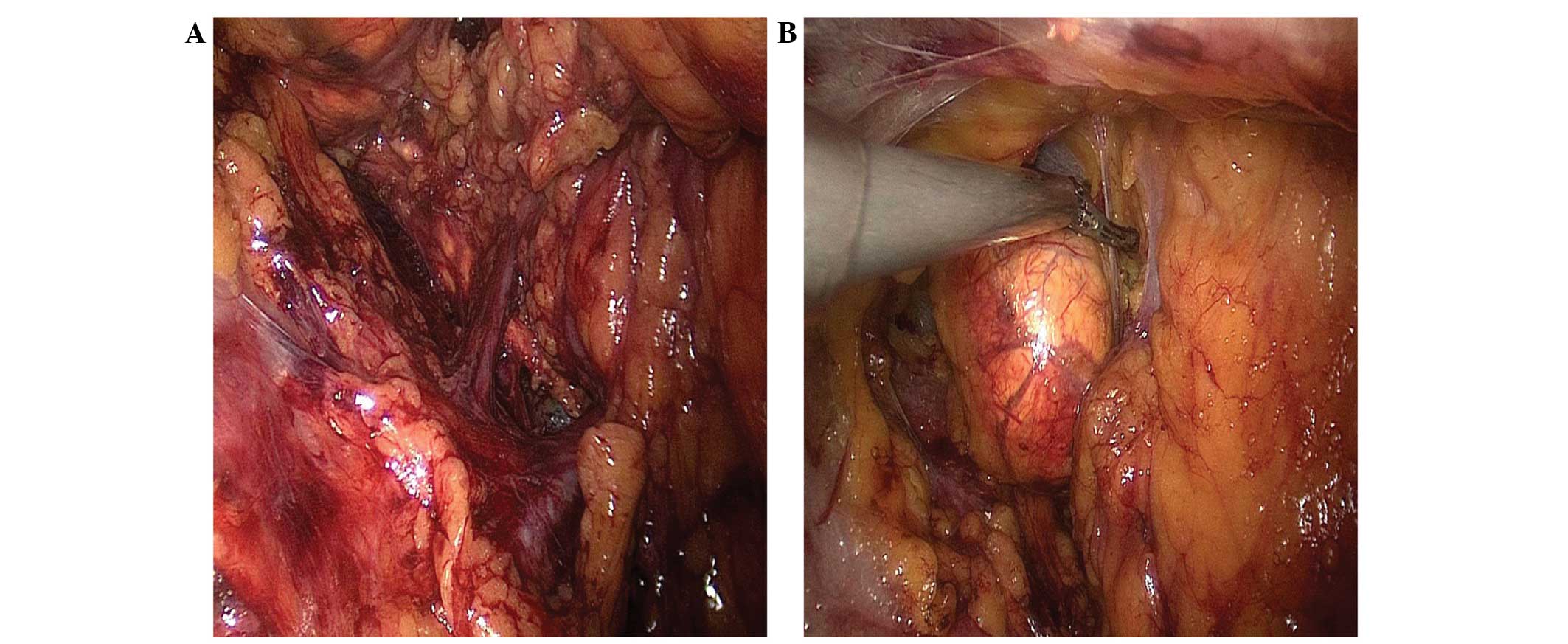
During the surgery, the renal hilum vessels were not
separated in order to avoid potential injury due to anatomic
variations. Anatomical abnormalities were identified in relation to
the right adrenal gland in the retroperitoneal space. The right
adrenal central vein was markedly longer than that of a healthy
individual, and was flowing into the right renal vein rather than
the inferior vena cava. A harmonic scalpel was used in order to
free the superior, lateral, posterior and medial attachments of the
adrenal mass (Fig. 2). Following
release, the tumor was placed into a bag and held by a grasper. The
surgical procedure was performed successfully in 15 min, and the
patient's estimated blood loss was <20 ml. Each intraoperative
step was accomplished with confidence and no intraoperative
complications occurred.
At the conclusion of surgery, the neostigmine (1
mg)-induced neuromuscular blockade was reversed. The patient was
extubated and remained in the post-anesthesia care unit for 24 h,
where standard care, including electrocardiogram monitoring,
O2 inhalation and sputum suction, was administered, and
respiratory physiotherapy and exercises were applied in order to
clear bronchial secretions and prevent the occurrence of
bronchitis. The patient was discharged ten days later and underwent
pulmonological and laryngological postoperative follow-up.
Pathological analysis of the tumor specimen identified it as an
adrenal adenocarcinoma.
Discussion
KS is a rare disease, induced as a result of ciliary
dysfunction, which occurs due to a defect in the ultrastructure of
the cilia (10). The absence of the
inner or outer dynein arms impairs the typically coordinated
ciliary motion, which leads to mucus retention and subsequently,
chronic infections (11). Treatments
for KS include the application of antibiotics, cortical hormone or
DNase to prevent the progression of complications, including
bronchiectasia and chronic nasosinusitis (12,13). Gupta
et al (14) emphasized the
potential benefits of inoculating patients with flu or pneumococcus
vaccines, in order to prevent respiratory tract infections, whilst
also performing grommet insertion and endoscopic sinus surgery
simultaneously. However, a number of studies have recommended more
conservative management of KS, due to the potentially negative
effects of surgery (13,15). Overall, the therapeutic goal for KS is
the avoidance of infection and controlling the progression of heart
and lung diseases (16).
Particular attention should be paid to imaging
studies when patients are diagnosed with adrenal tumors combined
with KS, in order to define the size, shape, position and, of
particular importance, the surrounding vessels of the tumor. The
risks during the perioperative period include: Airway obstruction
due to chronic nasosinusitis and bronchiectasia, which may lead to
serious respiratory failure; and the difficulty in the elimination
of mucopurulent discharge may result in the development of
pulmonary edema (17). An appropriate
dose of antibiotics, and pulmonary physical therapy, should be
administered prior to surgery. Avoiding the use of respiratory
inhibitors and center-left trachea cannulas may also reduce the
risk of infection (18). In the
present study, comprehensive surgical risk assessments were
performed and two antibiotics were administered to treat any
respiratory symptoms. Laparoscopic retroperitoneal tumor excision
was selected as an appropriate surgical strategy, as it generated
less trauma, reduced postoperative pain and patient recovery time
and presented a reduced risk of pulmonary complications (19). Surgical interventions in KS patients
are more difficult due to potentiality complex anatomical
variations (20). Oms et al
(21) reported the advantages of
using left-handed surgeons to perform cholecystectomy for patients
exhibiting KS, indicating that it may be useful to alter standard
operating procedures to meet the demands of such anatomical
variations. Laparoscopic adrenal adenocarcinoma excisions are
typically performed by a transabdominal pre-peritoneal approach for
removal of abdominal organs and to allow sufficient operating
space, however this type of surgery affects the internal
environment of the abdominal cavity (22) Therefore, in the present study, the
retroperitoneal route was selected in order to reach the right
adrenal gland in the shortest feasible distance, and thus improve
the safety of the surgery.
In conclusion, in the present study, the feasibility
of adrenal tumor resection via a retroperitoneal approach, using
laparoscopic instruments, was confirmed. Prevention and treatment
of respiratory infection, as well as carefully observing anatomical
variations during surgery is of particular importance for patients
exhibiting adrenal tumors combined with KS. In this manner, an
ideal balance between safety and effectiveness is achievable.
References
|
1
|
Berdon WE and Willi U: Situs inversus,
bronchiectasis, and sinusitis and its relation to immotile cilia:
History of the diseases and their discoverers - Manes Kartagener
and Bjorn Afzelius. Pediatr Radiol. 34:38–42. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kartagener M: Zur Pathogenese der
Bronchiektasien. Bronchiektasien bei Situs inversus viscerum. Beitr
Klin Tuberk. 83:489–501. 1933.(In German). doi: 10.1007/BF02141468.
View Article : Google Scholar
|
|
3
|
Camner P, Mossberg B and Afzelius BA:
Evidence of congenitally nonfunctioning cilia in the
tracheobronchial tract in two subjects. Am Rev Respir Dis.
112:807–809. 1975.PubMed/NCBI
|
|
4
|
Afzelius BA and Eliasson R: Male and
female infertility problems in the immotile-cilia syndrome. Eur J
Respir Dis Suppl. 127:144–147. 1983.PubMed/NCBI
|
|
5
|
Eliasson R, Mossberg B, Camner P and
Afzelius BA: The immotile-cilia syndrome. A congenital ciliary
abnormality as an etiologic factor in chronic airway infections and
male sterility. N Engl J Med. 297:1–6. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Carceller Armengot M, Batalla Carda C,
Escribano A and Samper GJ: Study of mucociliary transport and nasal
ciliary ultrastructure in patients with Kartagener's syndrome. Arch
Bronconeumol. 4:11–15. 2005.(In Spanish). View Article : Google Scholar
|
|
7
|
Geremek M and Witt M: Primary ciliary
dyskinesia: Genes, candidate genes and chromosomal regions. J Appl
Genet. 45:347–361. 2004.PubMed/NCBI
|
|
8
|
Afzelius BA and Stenram U: Prevalence and
genetics of immotile-cilia syndrome and left-handedness. Int J Dev
Biol. 50:571–573. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cowan MJ, Gladwin MT and Shelhamer JH:
Disorders of ciliary motility. Am J Med Sci. 321:3–10. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ceccaldi PF, Carré-Pigeon F, Youinou Y, et
al: Kartagener's syndrome and infertility: Observation, diagnosis
and treatment. J Gynecol Obstet Biol Reprod (Paris). 33:192–194.
2004.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dhar DK, Ganguly KC, Alam S, Hossain A,
Sarker UK, Das BK and Haque MJ: Kartagener's Syndrome. Mymensingh
Med J. 18:75–79. 2009.PubMed/NCBI
|
|
12
|
Flume PA, O'Sullivan BP, Robinson KA, et
al: Cystic Fibrosis Foundation, Pulmonary Therapies Committee:
Cystic fibrosis pulmonary guidelines: Chronic medications for
maintenance of lung health. Am J Respir Crit Care Med. 176:957–969.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Desai M, Weller PH and Spencer DA:
Clinical benefit from nebulized human recombinant DNase in
Kartagener's syndrome. Pediatr Pulmonol. 20:307–308. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gupta S, Handa KK, Kasliwal RR and Bajpai
P: A case of Kartagener's syndrome: Importance of early diagnosis
and treatment. Indian J Hum Genet. 18:263–267. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
McManus IC, Mitchison HM, Chung EM,
Stubbings GF and Martin N: Primary ciliary dyskinesia
(Siewert's/Kartagener's syndrome): Respiratory symptoms and
psycho-social impact. BMC Pulm Med. 3:42003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
D'Auria E, Palazzo S, Argirò S, El OS and
Riva E: Primary ciliary dyskinesia: Clinical and genetic aspects.
Pediatr Med Chir. 34:117–122. 2012.(In Italian). PubMed/NCBI
|
|
17
|
Savitha KS, Sunanda S and Vijayan R:
Kartagener's syndrome - Anaesthetic implications. Indian J Anaesth.
50:469–471. 2006.
|
|
18
|
Kashif A, Masud M, Manzoor SM and Haneef
S: Kartagener's syndrome and acute appendicitis. J Ayub Med Coll.
22:176–177. 2010.
|
|
19
|
Hazzan D, Shiloni E, Golijanin D, et al:
Laparoscopic vs open adrenalectomy for benign adrenal neoplasm.
Surg Endosc. 15:1356–1358. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Biere SS, van Berge Henegouwen MI, Maas
KW, Bonavina L, Rosman C, Garcia JR, Gisbertz SS, Klinkenbijl JH,
Hollmann MW, de Lange ES, et al: Minimally invasive versus open
oesophagectomy for patients with oesophageal cancer: A multicentre,
open-label, randomised controlled trial. Lancet. 379:1887–1892.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Oms LM and Badia JM: Laparoscopic
cholecystectomy in situs inversus totalis: The importance of being
left-handed. Surg Endosc. 17:1859–1861. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Buell JF, Abreu SC, Hanaway MJ, et al:
Right donor nephrectomy: A comparison of hand-assisted
transperitoneal and retroperitoneal laparoscopic approaches.
Transplantation. 77:521–525. 2004. View Article : Google Scholar : PubMed/NCBI
|