Introduction
Angiosarcoma is a rare malignant tumor with an
extremely poor prognosis, and metastasis occurs in ~50% cases,
always ending with mortality within a year (1). Although it has been detected in all
regions of the body, lung involvement is the most common site of
metastasis (2,3). Diffuse alveolar hemorrhage (DAH) is a
clinicopathological syndrome that results from a variety of
conditions and is considered as a life-threatening event, however,
it is rare as the presentation of pulmonary angiosarcoma (4). The current study presents a case of
angiosarcoma that originated from the subcutaneous soft tissue of
the mastoid process, but was subject to a delayed diagnosis and
rapid invasion into the brain and lung. The metastatic angiosarcoma
of the lung presented with DAH as the initial manifestation. The
pathological examination of a biopsy of the subcutaneous mass and
pulmonary lesions confirmed the diagnosis of angiosarcoma.
Written informed consent for the present report was
obtained from the patient's family.
Case report
In March 2012, a 66-year-old man was referred to the
Inpatient Respiratory Department of the First Affiliated Hospital,
School of Medicine, Zhejiang University, with coughing and
hemoptysis that had persisted for 20 days. The patient also
complained of dyspnea on exertion and a mild headache. In February
2012, the patient had been diagnosed with a pulmonary infection and
had been treated with antibiotics and hemostatic agents in a local
clinic for 1 week, but the symptoms were unimproved. No fever,
night sweats or weight loss were noted. The patient was a heavy
smoker who had smoked 2 packs of cigarettes daily for 40 years. In
addition, a head trauma had been suffered 2 years previously and a
protuberance in the left mastoid process had been diagnosed as a
hematoma. The protuberance had been slowly growing for 1 year. The
patient had no history of chronic lymphedema, no known
environmental exposure, including radiation, thorium dioxide, vinyl
chloride and arsenic exposure, and no exposure to tuberculosis.
A physical examination revealed moist rales in the
lung bases, and a large (almost 4×3-cm), hard lump with fixation in
the subcutaneous soft tissue below the left mastoid process was
noticed. The neurological examination was negative. Upon
hemocytological examination, mild anemia was detected, with a
hemoglobin level of 9.5 g/dl (normal range, 11.3–15.1 g/dl). Other
blood tests, including liver and kidney function, antinuclear
antibodies, thyroid hormone, immunoglobulin and complement, tumor
markers, bleeding and clotting time, were all within the normal
ranges. Anti-glomerular basement membrane and antineutrophil
cytoplasmic antibodies, and a galactomannan test for
Aspergillus were negative. No tubercle bacillus or fungi
were found in the sputum. Electrocardiogram and abdominal
ultrasonography results were normal. The patient also underwent
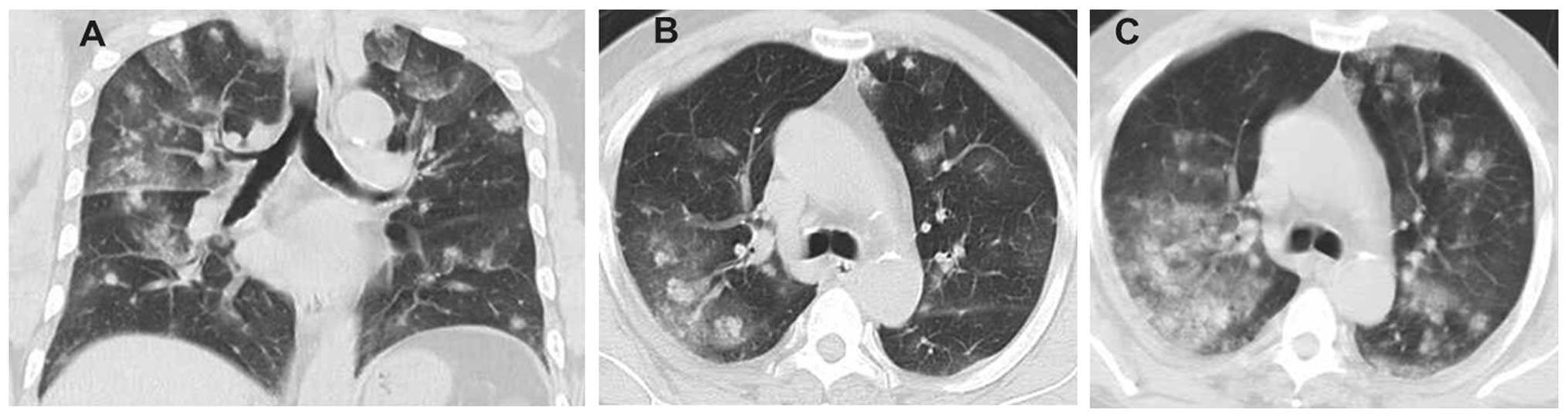
chest and brain computed tomography (CT). Multiple low-density
nodules surrounded by a wide range of ground-glass-like effusion
were identified in the bilateral lungs (Fig. 1A and B). Multifocal invasion and
cystic lesions with perilesional edema were detected in the brain
(Fig. 2); however, the brain CT was
negative 1 year previously, in January 2011. Single photon emission
CT of the bone was negative.
Based on the symptoms and imaging findings, a
possible diagnosis of intracranial and pulmonary metastasis was
suspected. To form a definitive diagnosis and determine nature of
the primary lesion, a lung biopsy was performed using CT-guided
percutaneous fine-needle aspiration. A biopsy of the subcutaneous
soft tissue below the left mastoid process was also performed by
ultrasound-guided puncture. Histological examination of both biopsy
samples revealed atypical round or spindle-shaped cells arranged
with a fascicular pattern, and consisting of focal luminal
differentiation, necrosis and hemosiderin pigmentation.
Immunohistochemical staining revealed that the tumor cells were
positive for vascular antigens, including cluster of
differentiation (CD) 31 and CD34, while being negative for
cytokeratin and thyroid transcription factor-1. The definitive
diagnosis was confirmed as a primary epithelioid angiosarcoma of
the subcutaneous soft tissue, with pulmonary and intracranial
metastases.
Due to poor general fitness, the patient was not a
candidate for chemotherapy and was therefore prescribed with
methylprednisolone (40 mg daily for 2 weeks) and aminomethylbenzoic
acid (400 mg daily for 1 week) for hemostasis, and
glycerol-fructose (500 ml daily for 2 weeks) for brain edema. The
patient rapidly deteriorated, with dyspnea and hemoptysis. A
reexamination of the hemoglobin level showed a decrease to 4 g/dl
and a repeat chest CT scan showed more nodules with
ground-glass-like shadows had appeared in extensive lung fields
(Fig. 1C). Based on the
characteristic progress of the manifestations, the patient was
diagnosed with DAH. The patient finally succumbed to respiratory
failure 1 month after the definitive diagnosis.
Discussion
Angiosarcoma is a rare and aggressive malignant
vascular tumor that originates from endothelial cells, accounting
for only 1–2% of all soft-tissue sarcomas (2,5). The tumor
can occur in any region of the body, and a wide variety of
anatomical locations have been described for this malignancy
(6). In the clinic, angiosarcoma
tends to exhibit local recurrence and distant metastasis, and the
overall prognosis is poor (5,6).
Angiosarcoma is associated with aggressive clinical
behavior, and its manifestations vary depending on the anatomical
location (7). Patients with
angiosarcoma usually present with metastatic disease at the time of
diagnosis, and the lung is the most common site of metastatic
involvement, followed by the liver, cervical lymph nodes, spleen,
and rarely by the heart and brain (3). The patient in the present study
presented with coughing and hemoptysis as the first symptom, but
rapidly deteriorated, exhibiting progressive anemia and dyspnea. On
the follow-up examination chest CT scan, spotted or patchy shadows
with obscure margins were observed in the peripheral sides of the
bilateral lung fields, which were rapidly aggravated over a course
of 2 weeks. All the presenting symptoms of this case are included
in the known characteristics of DAH. DAH is a clinicopathological
syndrome describing the accumulation of intra-alveolar red blood
cells originating from the alveolar capillaries, and it is
recognized by the clinical constellation of symptoms consisting of
hemoptysis, anemia, diffuse radiographic pulmonary infiltrates and
hypoxemic respiratory failure (4). A
number of diseases can cause DAH, including Wegener's
granulomatosis, Goodpasture's syndrome, microscopic polyangiitis,
antiphospholipid antibody syndrome, connective tissue disorders,
infectious or toxic disorders, and neoplastic diseases (8). Neoplastic diseases are not generally
considered in the differential diagnosis of DAH and it is rare as
the manifestation of angiosarcoma (9). In the present study, the diverse
etiologies were ruled out through auxiliary examinations. The chest
CT scan revealed nodules surrounded by ground-glass opacity,
indicating lung metastasis with peripheral hemorrhage, and the
pathological examination confirmed angiosarcoma. As DAH is a
catastrophic clinical syndrome causing respiratory failure,
vigilance should be maintained with regard to noting the possible
etiology of DAH due to metastatic angiosarcoma of the lung, and a
differential diagnosis of DAH should be established.
Angiosarcoma of the scalp has a predilection for
pulmonary metastasis (10), and it
appears to be a naturally privileged barrier that hinders local
spread and resultant seeding in the cranial cavity, thus
angiosarcoma metastasizing to the brain is relatively rare
(11,12). In the present study, metastases of the
lung and brain occurred at the time of diagnosis. The lesions of
the lung developed progressively and led to respiratory failure.
However the brain metastasis was only slowly aggravated, which
caused a mild headache, and was detected with multiple mass lesions
on brain CT.
Although angiosarcoma has a number of unknown
etiological sources, trauma, and exposure to polyvinyl chloride,
thorium dioxide and radiation have been suggested in its etiology
(13). The most common sites of
involvement are cutaneous, and the malignancy occurs most
frequently in the scalp and facial skin of elderly men (3). Angiosarcoma arising in the skin or
subcutaneous soft tissues may typically appear as multinodular
hemorrhagic masses, which tend to be overlooked and delay the
diagnosis of angiosarcoma (14). In
the present study, the patient had experienced a previous head
trauma and presented with a hematoma of the left mastoid process.
After a delay, the pathological analysis confirmed the diagnosis of
a primary angiosarcoma. As early diagnosis is the key for a better
clinical outcome in angiosarcoma, it is suggested that the site of
trauma in the skin should be followed up by observing the changes
to the lesion in elderly individuals, and that a biopsy is
necessary to establish a definitive diagnosis.
In conclusion, the present case demonstrates that
angiosarcoma has aggressive characteristics, with a marked tendency
for distant metastasis, and that pulmonary metastasis may present
with DAH as the initial manifestation. Pulmonary angiosarcoma
should be considered as an important differential diagnosis of DAH
and the requirement for a systematic approach for the early
recognition of angiosarcoma should be emphasized.
Acknowledgements
This study was supported by grants from Zhejiang
Medical Science Research Fund in China (nos. 2009B057 and
2010KYB045).
References
|
1
|
Saitoh J, Sakurai H, Suzuki Y, Katoh H,
Takahashi T and Nakano T: Metastatic angiosarcoma of the lung with
alveolar hemorrhage. Jpn J Radiol. 27:381–384. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Patel AM and Ryu JH: Angiosarcoma in the
lung. Chest. 103:1531–1535. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen W, Shih CS, Wang YT, Tseng GC and Hsu
WH: Angiosarcoma with pulmonary metastasis presenting with
spontaneous bilateral pneumothorax in an elderly man. J Formos Med
Assoc. 105:238–241. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lara AR and Schwarz MI: Diffuse alveolar
hemorrhage. Chest. 137:1164–1171. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Carillo GA, Carretero MA, Vazquez JE,
Fontan EG, Ramos MB, Ventura JA, Rodriguez AP, Salmon AS and
Tejedor JL: Epithelioid angiosarcoma of the lung with pleural
metastasis: a rare cause of haemoptysis clinicopathological
conference. Heart Lung Circ. 19:624–628. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fayette J, Martin E, Piperno-Neumann S, Le
Cesne A, Robert C, Bonvalot S, Ranchère D, Pouillart P, Coindre JM
and Blay JY: Angiosarcomas, a heterogeneous group of sarcomas with
specific behavior depending on primary site: A retrospective study
of 161 cases. Ann Oncol. 18:2030–2036. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liu H, Huang X, Chen H, Wang X and Chen L:
Epithelioid angiosarcoma of the kidney: A case report and
literature review. Oncol Lett. 8:1155–1158. 2014.PubMed/NCBI
|
|
8
|
Ioachimescu OC and Stoller JK: Diffuse
alveolar hemorrhage: Diagnosing it and finding the cause. Cleve
Clin J Med. 75:258, 260, 264–265. 2008.
|
|
9
|
Adem C, Aubry MC, Tazelaar HD and Myers
JL: Metastatic angiosarcoma masquerading as diffuse pulmonary
hemorrhage: Clinicopathologic analysis of 7 new patients. Arch
Pathol Lab Med. 125:1562–1565. 2001.PubMed/NCBI
|
|
10
|
Lanese DM and Pacht ER: Unusual
presentation of metastatic scalp angiosarcoma: diagnosis by
transbronchial lung biopsy. J Natl Med Assoc. 79:565–568.
1987.PubMed/NCBI
|
|
11
|
Choi KS, Chun HJ, Yi HJ and Kim JT:
Intracranial invasion from recurrent angiosarcoma of the scalp. J
Korean Neurosurg Soc. 43:201–204. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ellegala DB, Kligori C, Vandenberg S,
Dumont A and Shaffrey ME: Intracranial metastasis of a primary
scalp angiosarcoma. Case illustration. J Neurosurg. 97:7252002.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nair Somasekharan KK, Zabell AS, Vo KL and
Shaikh MA: Pneumothorax: A classical presentation of metastatic
scalp angiosarcoma. Ann Thorac Surg. 94:e77–e78. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Holden CA, Spittle MF and Jones EW:
Angiosarcoma of the face and scalp, prognosis and treatment.
Cancer. 59:1046–1057. 1987. View Article : Google Scholar : PubMed/NCBI
|