Introduction
Olfactory neuroblastoma (ON) is an uncommon
malignant nasal tumor which is originated from neuroectoderm. It
comprises ~2% of all sinonasal tract tumors. Its incidence is ~0.4
per million in population (1,2). The most common symptoms of ON are
unilateral nasal obstruction (70%), and epistaxis (50%). Other
symptoms include headaches, pain, excessive lacrimation,
rhinorrhea, anosmia and changes in vision. ON originates from
olfactory epithelium; however, ON rarely causes anosmia (5%)
(3,4).
ON may histologically mimic a number of types of tumor within the
sinonasal tract, making it more difficult to diagnosis. The
management of ON requires bicranial-facial surgical approach,
trephination procedure, which is technically challenging and
achieving good results are difficult. Treatment modalities for ON
are en bloc resection, extra cranial resection or surgery combined
with radiotherapy (RT) and/or chemotherapy. The present study
reports the case of a patient with a mass in the nasal cavity who
was treated by combined surgical excision and RT.
Case report
A 69-year-old male patient presented to the Kanuni
Research and Education Hospital (Trabzon, Turkey) with a mass in
the nose in October 2012. Endoscopy showed the presence of a mass
within the nasal cavities, causing destruction of the nasal dorsum.
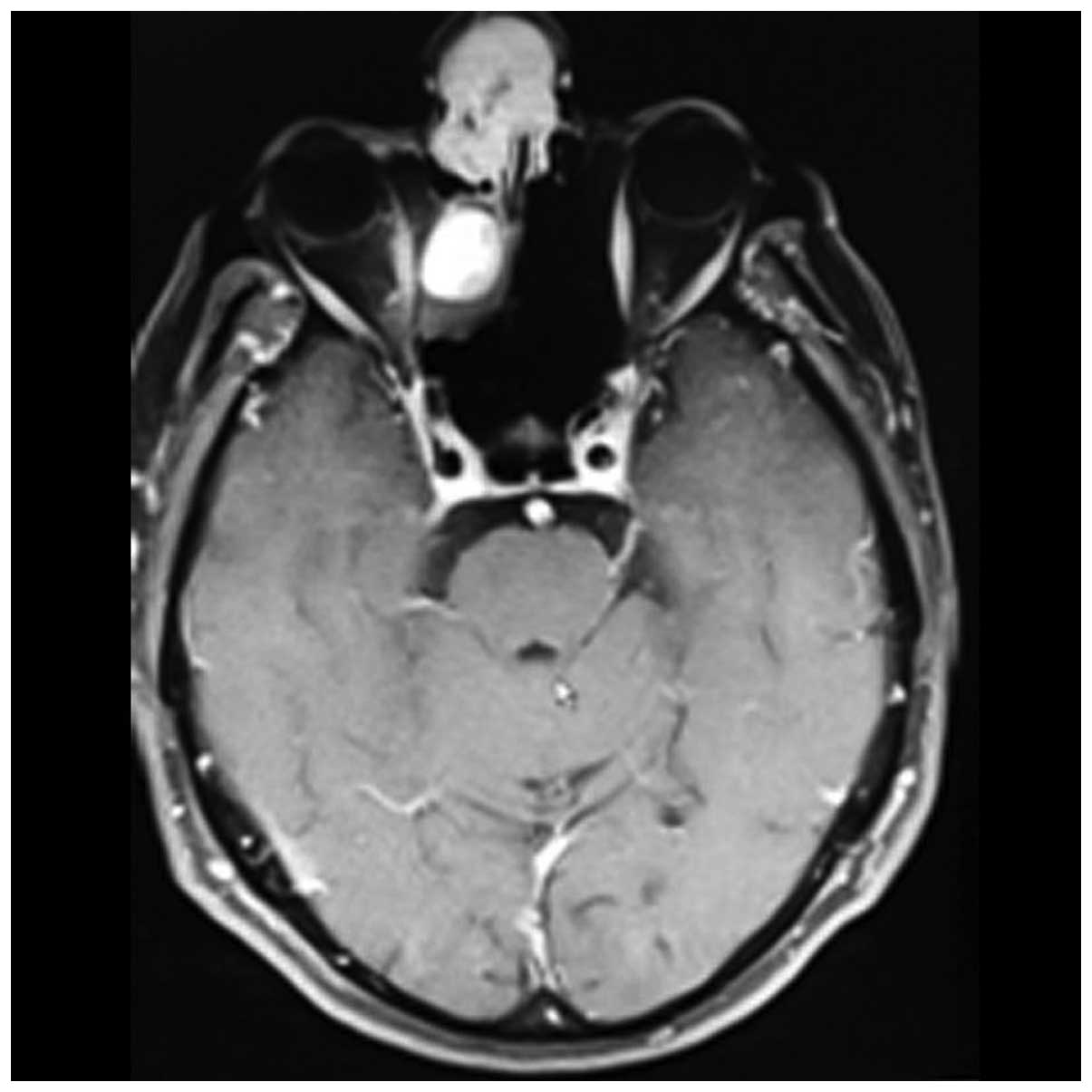
Upon cranial magnetic resonance imaging (MRI) a homogenous
contrast-enhanced mass, 24×33 mm in size, was observed (Fig. 1). The mass was isointense on
T1-weighted imaging, and hyperintense on T2-weighted imaging and
fluid attenuated inversion recovery. The mass infiltrated the nasal
septum in the anterior region. A second mass was also observed
posterior to the first mass. This second mass was 2 cm in diameter
and was an intensely contrast-enhanced well-circumscribed lesion.
At the superior border, the mass reached the frontal bone causing
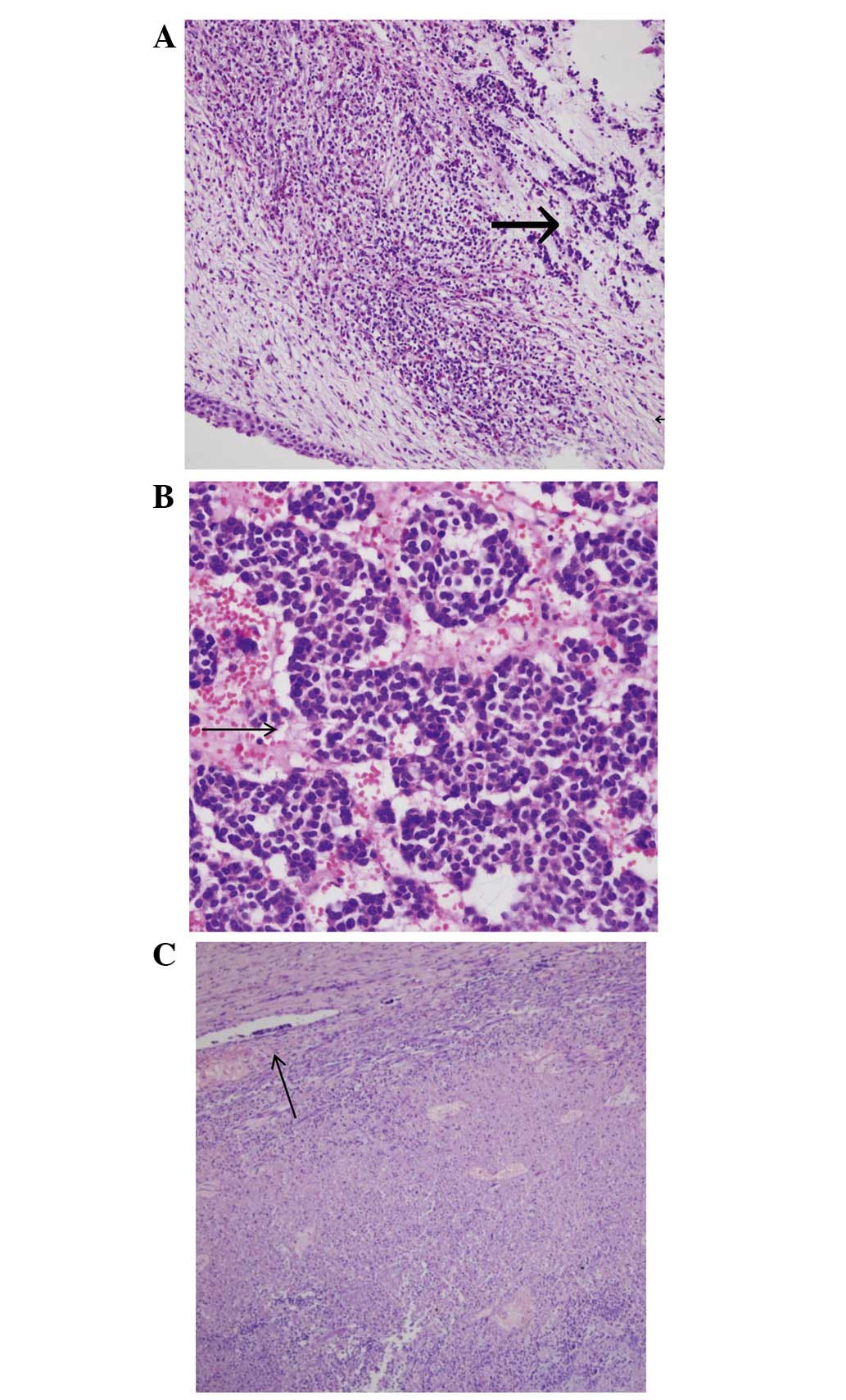
bony destruction. A biopsy from the lesion reported a diagnosis of
ON (Fig. 2A and B). The patient was
treated with a wide tumor excision by nasal endoscopic surgery. The
post-operative pathology both lesions showed a grade II ON.
Surgical margins were positive on medial canthus and negative in
the base of the cranium. Immunohistochemistry results were reported
as positive for neuron-specific enolase (NSE), weakly positive for
chromogranin, and negative for vimentin and S-100 protein.
Follwing surgery, the patient was treated with the
TomoTherapy Hi-Art System® using an intensity-modulated
radiotherapy (IMRT) technique, and 66 Gy external RT with 220
cGy/fraction was applied to the pre-operative tumor bed. The
patient was followed up without using chemotherapy.
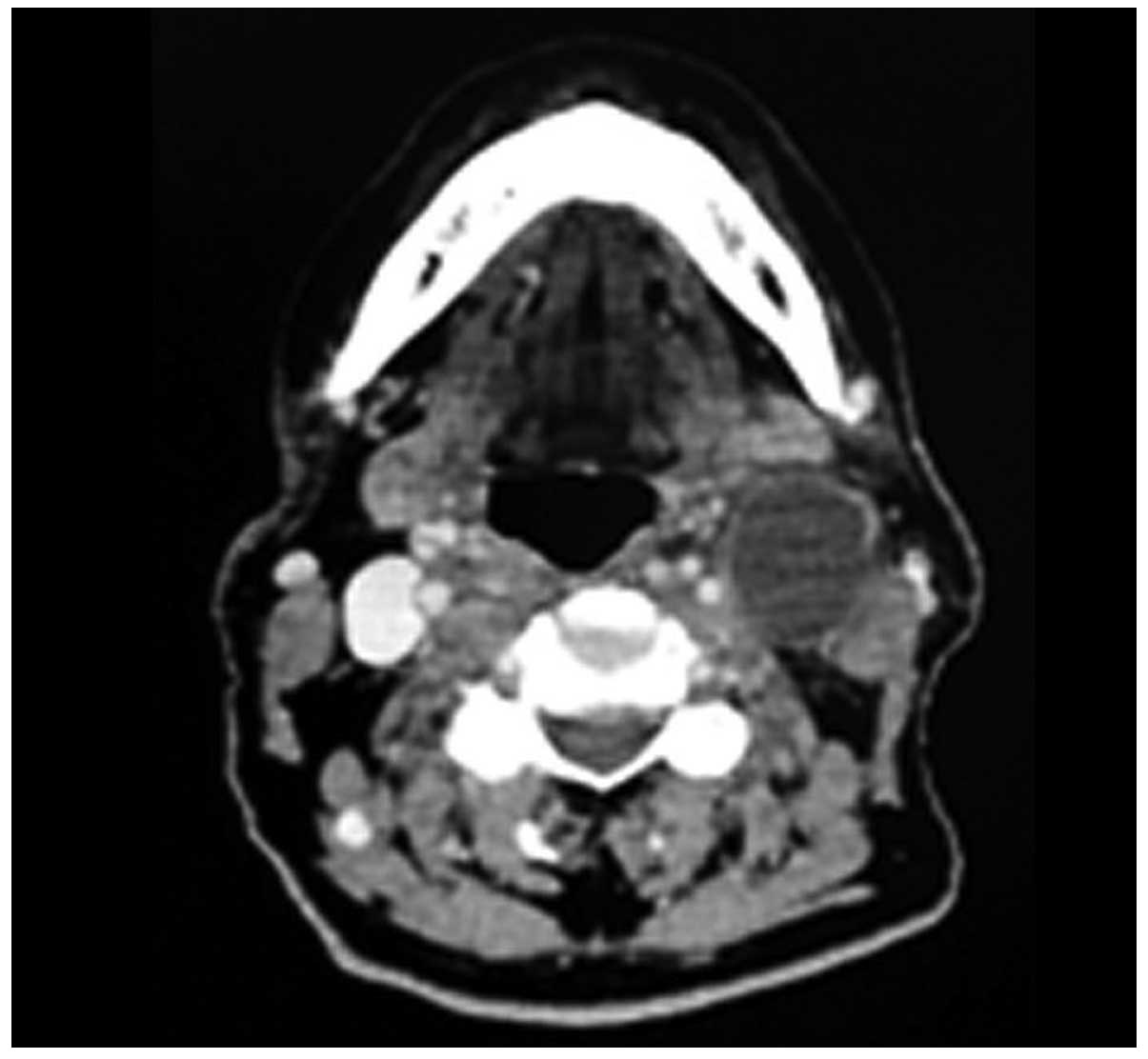
After 2 years of follow-up, a mass was palpable on
the left side of the neck upon physical examination. Computed
tomography revealed a hyperdense metastatic lymphadenopathy, 29×25
mm in size, in the left submandibular region (Fig. 3). Lymph nodes of <1 cm in diameter
were also present in the 5 cervical neck region and they were
non-malignant. The patient was treated with a radical neck
dissection. The pathology report recorded 16 reactive lymph nodes,
and 1 lymph node that was 4 cm in diameter was diagnosed as an ON
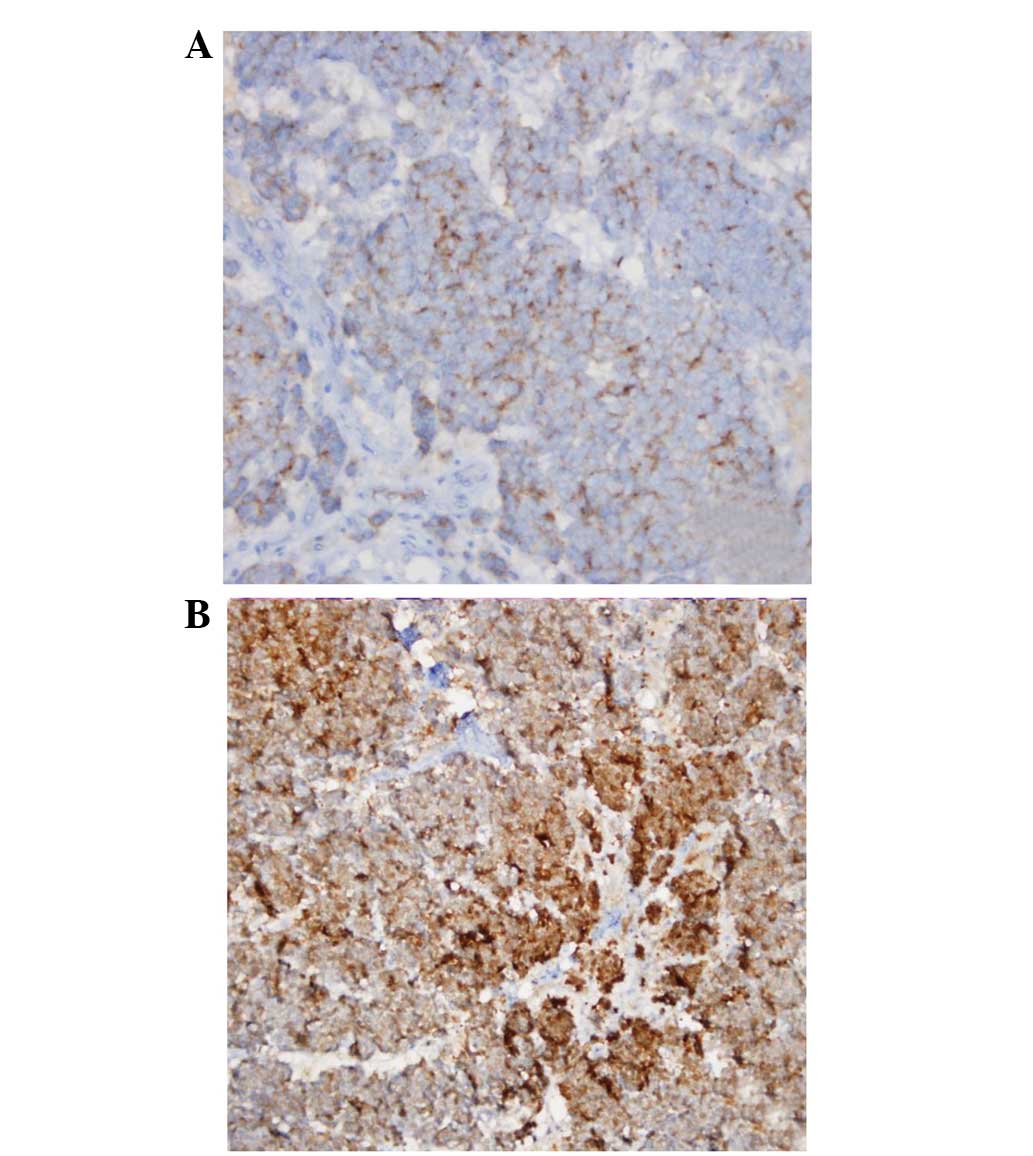
metastasis in the sub-capsular region (Fig. 2C). The immunohistochemistry results
were reported as positive for NSE and chromogranin (Fig. 4), and negative for synaptophysin.
No distant organ metastasis or recurrence in the
primary tumor region was detected. The patient was treated with the
Hi-Art Tomotherapy IMRT technique after taking consideration of the
prior treatment doses for regions and organs at risk. A total of 54
Gy external RT, with 200 cGy/fraction, was administered to the
right neck region (levels I–V), while a total of 60 Gy external RT,
with 200 cGy/fraction, was administered to the left neck region
(level I–V). Subsequently, 100 mg etoposide was administered for 7
consecutive, every 21 days, for 6 months. The patient is in the 3rd
year after diagnosis and a complete response has been observed
after post-operative treatment.
Discussion
ON is a rare locally aggressive tumor (5). Although it can be found in all age
groups, it occurs more commonly in the 3rd and 6th decades of life,
and is present equally in each gender. The most common symptoms are
one-sided nose obstruction and epistaxis, while rhinorrhea and
anosmia may also occasionally accompany these symptoms. Extensive
lesions may cause frontal headaches and diplopia. As earlier
symptoms are not specific, 70% of patients consult their doctors
with advanced-stage disease (6,7). ON can
spread quickly and easily into the intracranial structures via the
cribriform plate. Cribriform plate and orbit involvement in ON are
important prognostic factors (8). It
has been reported that the cervical lymph node involvement rate is
nearly 20%, that the local recurrence rate is 20–30% and that the
6-month distant metastasis rate is 50% (9,10). In the
present case, distant metastasis was observed 2 years after the
completion of treatment. Studies have been conducted in order to
evaluate treatment and prognosis of ON staging. Computed tomography
and MRI are important in staging. Kadish et al (11) performed the first staging of ON using
clinical evaluation and neuroradiological findings. According to
this staging, stage A is a tumor limited to the nasal cavity, stage
B is a tumor is limited to the nasal cavity and one or more of the
paranasal sinuses, and stage C is a tumor extending from the nasal
cavity and paranasal sinuses. Orbit, skull base and intracranial
cavity involvement or cervical lymph node and distant metastasis is
present. When patients are diagnosed, the majority are at stages C
(56%) and B (40%), while only a small portion of patients are at
stage A (4%) (12). The present case
was diagnosed as stage C following radiological assessment.
Subsequent to the staging of ON, multidisciplinary
approaches have been used for treatment, and no standard treatment
approach has yet been established. The aim of the treatment should
prevent local and regional recurrences, and distant metastasis.
Treatment options consist of surgery or RT only, surgery and RT,
surgery and chemotherapy combined with RT, or only chemotherapy
(13,14). A craniofacial resection has been
suggested for all patients with frontal cranial base involvement
(4,14). It has been reported that, in selected
patients, endoscopic sinus surgery and stereotactic radiosurgery
lead to good results (15). Walch
et al (10) obtained tumor
control without any patient mortality by combining stereotactic
radiosurgery and endoscopic sinus surgery in individuals with stage
B and C disease according to the Kadish classification (11).
In the present patient, endoscopic sinus surgery
with a wide local excision was performed post-diagnosis, and RT was
subsequently applied. ON may metastasize and reoccur following its
removal (12,15), so post-operative therapy should be
added to the treatment. In a study of 29 patients treated with a
craniofacial resection, Aboziada and Eisbruch (16) suggested that the addition of RT to a
craniofacial resection leads to recurrence in 2/13 patients, while
no additional RT leads to recurrence in 11/16 patients. Even though
chemotherapy and RT treatments are routine for stage C disease, the
study by Benfari et al (17)
indicated that RT should be applied to all patients, with the
exception of cases with tumors limited to the cribriform plate
without bony destruction. The most important deductions from the
aforementioned studies are summarized as follows: i) RT alone is
effective in 36.3% of patients. ii) Survival rates have a tendency
to decrease as tumor stage increases (stage A, 100%; stage B,
58.3%; and stage C, 18.9%). iii) There is no correlation between
survival and radiation dose. The majority of patients who succumbed
to the disease received RT doses of 50–65 Gy, as recommended in the
literature. iv) The presence of palpable neck nodes and/or distant
metastasis, at presentation, is a significant prognostic factor for
survival. Regional lymph node metastasis was present in 6 patients
at presentation, and of these, 4 patients succumbed to the disease,
with a median survival time of 5.2 months; an identical outcome was
noted in 2/2 patients with distant metastasis. v) A variable and
often prolonged natural history is characteristic of ON. This
prerogative is highlighted by the 1 patient who remained alive with
the disease at 120 months (17).
In another study, the 5-year local relapse-free
survival rate was significantly higher for those patients who
received post-operative RT (100%) compared with surgery alone
(29%). The 5-year disease-free survival rate was 87.5% in the RT
group and 31% in the group that underwent surgery alone. Regional
failure was observed in 7 patients (27%); 6 with stage B and 1 with
stage C disease according to the Kadish classification. Nodal
failure most commonly occurred at level II of the neck, with 3
patients experiencing nodal failure in the contralateral neck. Only
3 of the cases with regional failure were salvaged successfully.
Due to the high rate of regional failure following a lack of
elective treatment on the neck, elective nodal RT is justified in
patients with Kadish stage B and C disease. These results confirmed
the beneficial effect of adjuvant RT to the tumor bed on local
control (18). However, in a
retrospective analysis, Montava et al (19) emphasized that the gold-standard
treatment for ON is craniofacial resection and that mortality is
associated with RT.
In conclusion, a standard treatment for ON is not
yet clear as the number of ON cases is limited. However, due to the
20% risk of neck metastasis in stage B and C, treatment should
include a wide surgical excision and prophylactic neck irradiation
should be added to the RT region. Prospective studies with a large
number of patients are required in order to establish a
gold-standard treatment.
References
|
1
|
Berger L, Luc R and Richard D: Olfactory
esthesioneuroblastoma. Bull Assoc Fr Etude Cancer. 13:410–21.
1924.(In French).
|
|
2
|
Bhattacharyya N, Thornton AF, Joseph MP,
Goodman ML and Amrein PC: Successful treatment of
esthesioneuroblastoma and neuroendocrine carcinoma with combined
chemotherapy and proton radiation. Results in 9 cases. Arch
Otolaryngol Head Neck Surg. 123:34–40. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rakes SM, Yeatts RP and Campbell RJ:
Ophthalmic manifestations of esthesioneuroblastoma. Ophthalmology.
92:1749–53. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kutluhan A, Yilmaz N, Yakut F, Yurttaş V
and Uğraş S: Treatment of olfactory neuroblastoma via subfrontal
and midfacial degloving approaches: A case report. Kulak Burun
Bogaz Ihtis Derg. 18:56–8. 2008.(In Turkish). PubMed/NCBI
|
|
5
|
Fitzek MM, Thornton AF, Varvares M,
Ancukiewicz M, Mcintyre J, Adams J, Rosenthal S, Joseph M and
Amrein P: Neuroendocrine tumors of the sinonasal tract. Results of
a prospective study incorporating chemotherapy, surgery, and
combined proton-photon radiotherapy. Cancer. 94:2623–34. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kleihues P and Cavenee WK: WHO
Classification of Tumours of Pathology and Genetics Tumours of the
Nervous System. Lyon, France: IARC Press. 150–152. 2000.
|
|
7
|
Weiss SW and Goldblum JR Enzinger:
Primitive neuroectodermal tumors and related lesions. Enzinger and
Weiss's Soft Tissue Tumors (4th). (Philadelphia, PA). Mosby
Elsevier. 1308–1311. 2001.
|
|
8
|
Pickuth D, Heywang-Kobrunner SH and
Spielmann RP: Computed tomography and magnetic resonance imaging
features of olfactory neuroblastoma: an analysis of 22 cases. Clin
Otolaryngol Allied Sci. 24:457–461. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lund VJ, Howard D, Wei W and Spittle M:
Olfactory neuroblastoma: Past, present, and future? Laryngoscope.
113:502–507. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Walch C, Stammberger H, Anderhuber W,
Unger F, Kole W and Feichtinger K: The minimally invasive approach
to olfactory neuroblastoma: combined endoscopic and stereotactic
treatment. Laryngoscope. 110:635–640. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kadish S, Goodman M and Wang CC: Olfactory
neuroblastoma. A clinical analysis of 17 cases. Cancer.
37:1571–1576. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
de Gabory L, Abdulkhaleq HM, Darrouzet V,
Bébéar JP and Stoll D: Long-term results of 28
esthesioneuroblastomas managed over 35 years. Head Neck. 33:82–86.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bhattacharyya N, Thornton AF, Joseph MP,
Goodman ML and Amrein PC: Successful treatment of
esthesioneuroblastoma and neuroendocrine carcinoma with combined
chemotherapy and proton radiation. Results in 9 cases. Arch
Otolaryngol Head Neck Surg. 123:34–40. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Howard DJ, Lund VJ and Wei WI:
Craniofacial resection for tumors of the nasal cavity and paranasal
sinuses: A 25-year experience. Head Neck. 28:867–873. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Morita A, Ebersold MJ, Olsen KD, Foote RL,
Lewis JE and Quast LM: Esthesioneuroblastoma: prognosis and
management. Neurosurgery. 32:706–714. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Aboziada MA and Eisbruch A:
Esthesioneuroblastoma: the role of postoperative irradiation after
complete surgical resection. J Egypt Natl Canc Inst. 22:143–148.
2010.PubMed/NCBI
|
|
17
|
Benfari G, Fusconi M, Ciofalo A, Gallo A,
Altissimi G, Celani T and De Vincentiis M: Radiotherapy alone for
local tumour control in esthesioneuroblastoma. Acta
Otorhinolaryngol Ital. 28:292–297. 2008.PubMed/NCBI
|
|
18
|
Demiroz C, Gutfeld O, Aboziada M, Brown D,
Marentette LJ and Eisbruch A: Esthesioneuroblastoma: is there a
need for elective neck treatment? Int J Radiat Oncol Biol Phys.
15:255–261. 2011. View Article : Google Scholar
|
|
19
|
Montava M, Verillaud B, Kania R, Sauvaget
E, Bresson D, Mancini J, Froelich S and Herman P: Critical analysis
of recurrences of esthesioneuroblastomas: can we prevent them? Eur
Arch Otorhinolaryngol. 271:3215–3222. 2014. View Article : Google Scholar : PubMed/NCBI
|