Introduction
Microcystic adnexal carcinoma (MAC) was originally
defined in 1982 (1), and is now also
termed sclerosing sweat duct carcinoma (2). MAC is a rare, slow-growing, locally
aggressive tumor of the eccrine sweat glands, and is characterized
by pilar and eccrine differentiation (3). Sweat gland malignancies, combining all
types, are particularly rare, accounting for 0.005% of all
malignant epithelial neoplasms (4),
with a total of ~350 cases currently described in the English
literature. It has been reported that the preferential location for
the development of this neoplasm is the head and neck region
(5).
When referring to the English literature, it is
evident that MAC primarily affects the Caucasian population, with
only two cases occurring in non-Caucasian patients (6,7). Fang
et al (8) described two cases
involving Chinese individuals in the Chinese literature; however,
to the best of our knowledge, there are no cases of Chinese
patients with MAC currently reported in the English literature. The
present study reviewed all patients that were referred to the
Hainan Province People's Hospital (Haikou, China) between January
1994 and January 2014, and identified only one patient with a MAC
diagnosis. This case is described herein along with a review of the
relevant literature.
Case report
A 38-year-old woman was referred to the Department
of Oral and Maxillofacial Surgery at the Hainan Province People's
Hospital with a mass on the left upper-lip that had been present
for >10 years (Fig. 1). During
physical examination, it was noted that the tumor was positioned in
the left-upper lip and subnasal region. The lesion was a firm,
solitary mass, and measured 2×1 cm in size. No submandibular or
cervical lymph nodes were palpable during the physical examination.
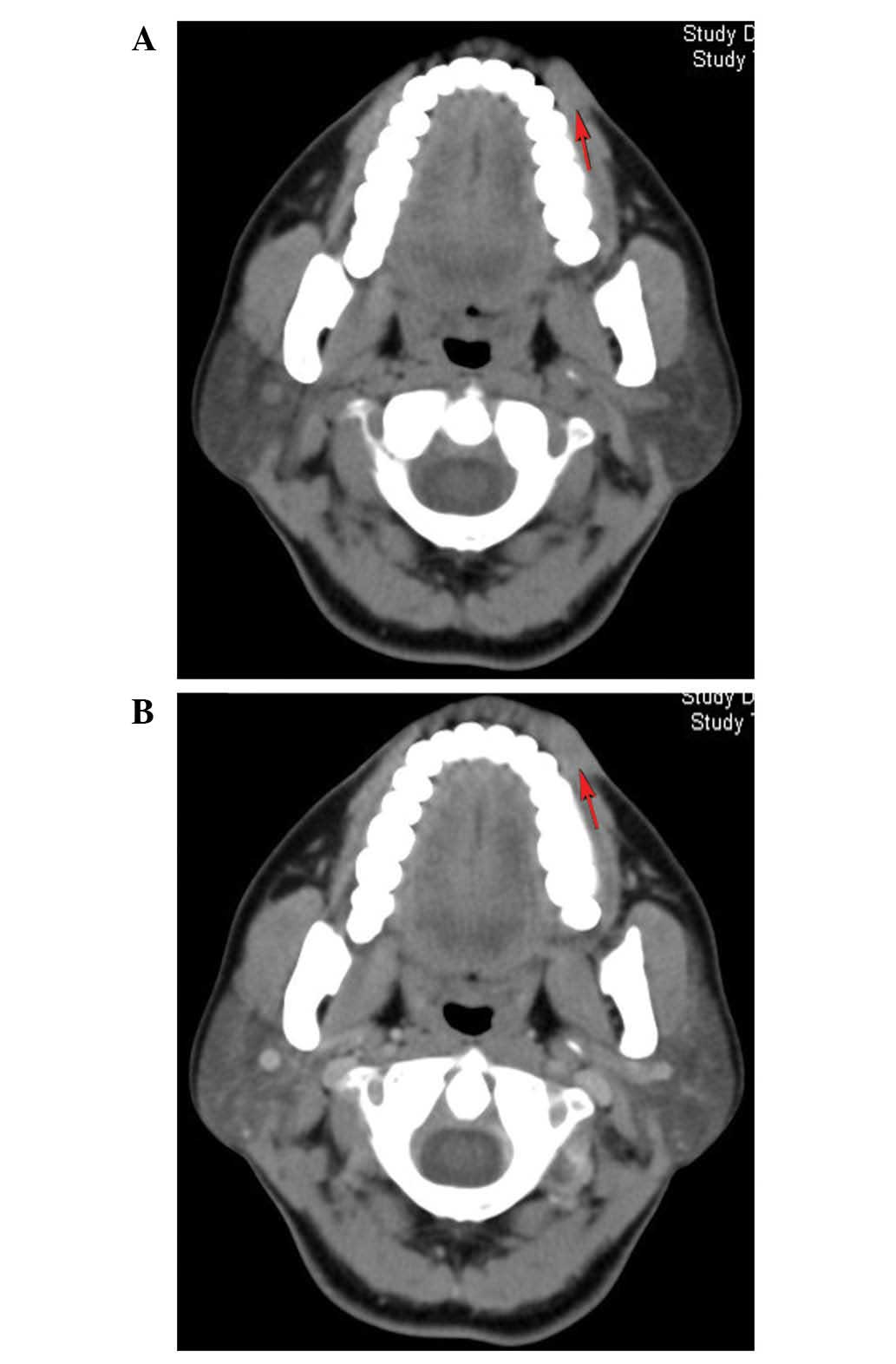
Abdominal ultrasonography and computed tomography (CT; Brilliance
iCT; Philips Medical Systems, Amsterdam, Holland) of the head, neck
and thorax demonstrated no evidence of systemic or local
metastasis. As presented in Fig. 2,
the head and neck CT scans revealed the lesion located in the
subcutaneous tissue of the left-upper lip, with a wide base
inseparable from overlying skin.
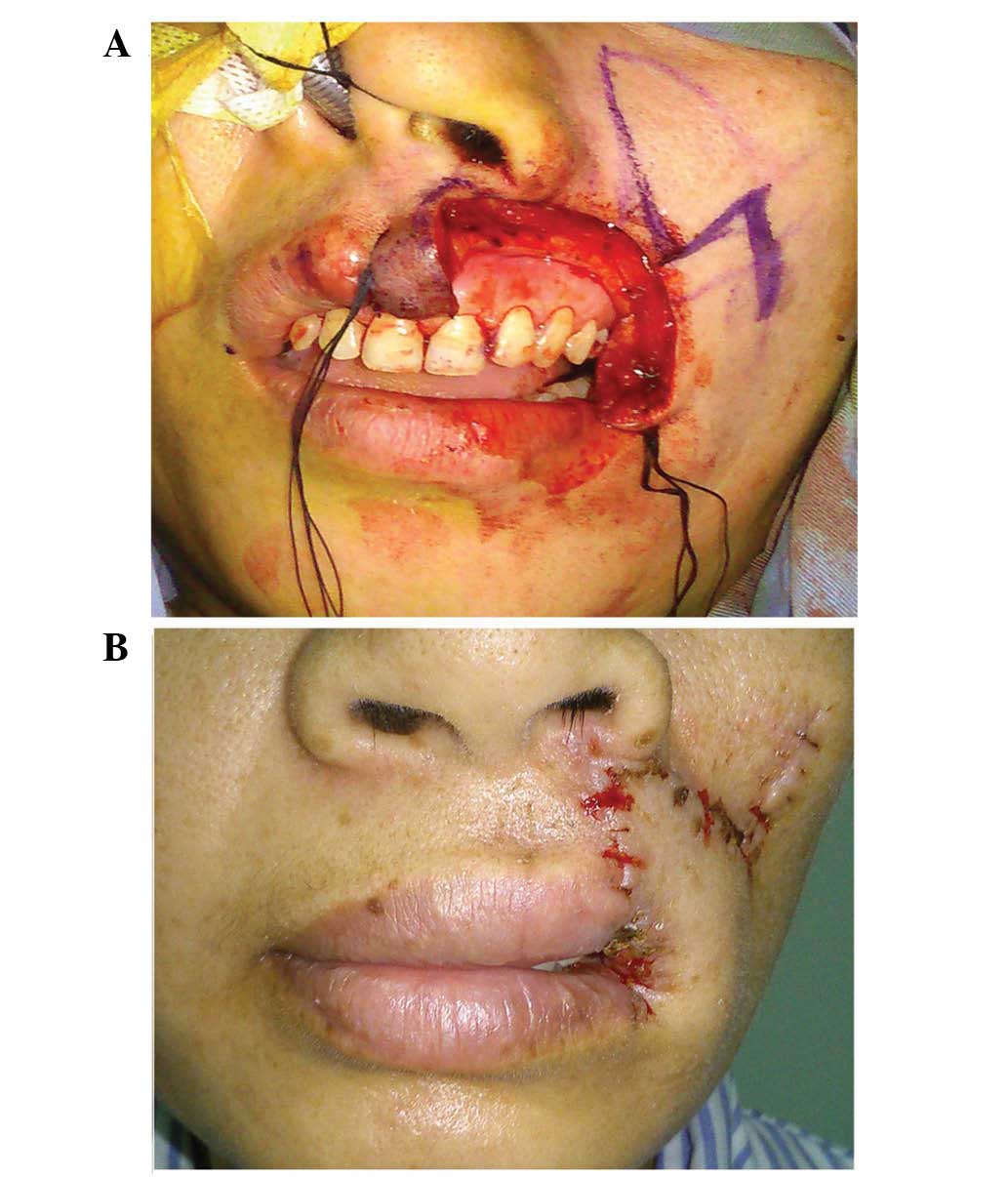
An incisional biopsy was performed with the patient
under local anesthesia. The diagnosis of the specimen was confirmed
as carcinoma. The patient underwent complete surgical resection of
the lesion, with 10 mm tumor-free margins, which resulted in a
subtotal defect of the philtrum and left-upper lip. Reconstruction
of the tissue defects was performed immediately, utilizing an
adjacent tissue flap of skin and mucous membranes from the cheek
(Fig. 3).
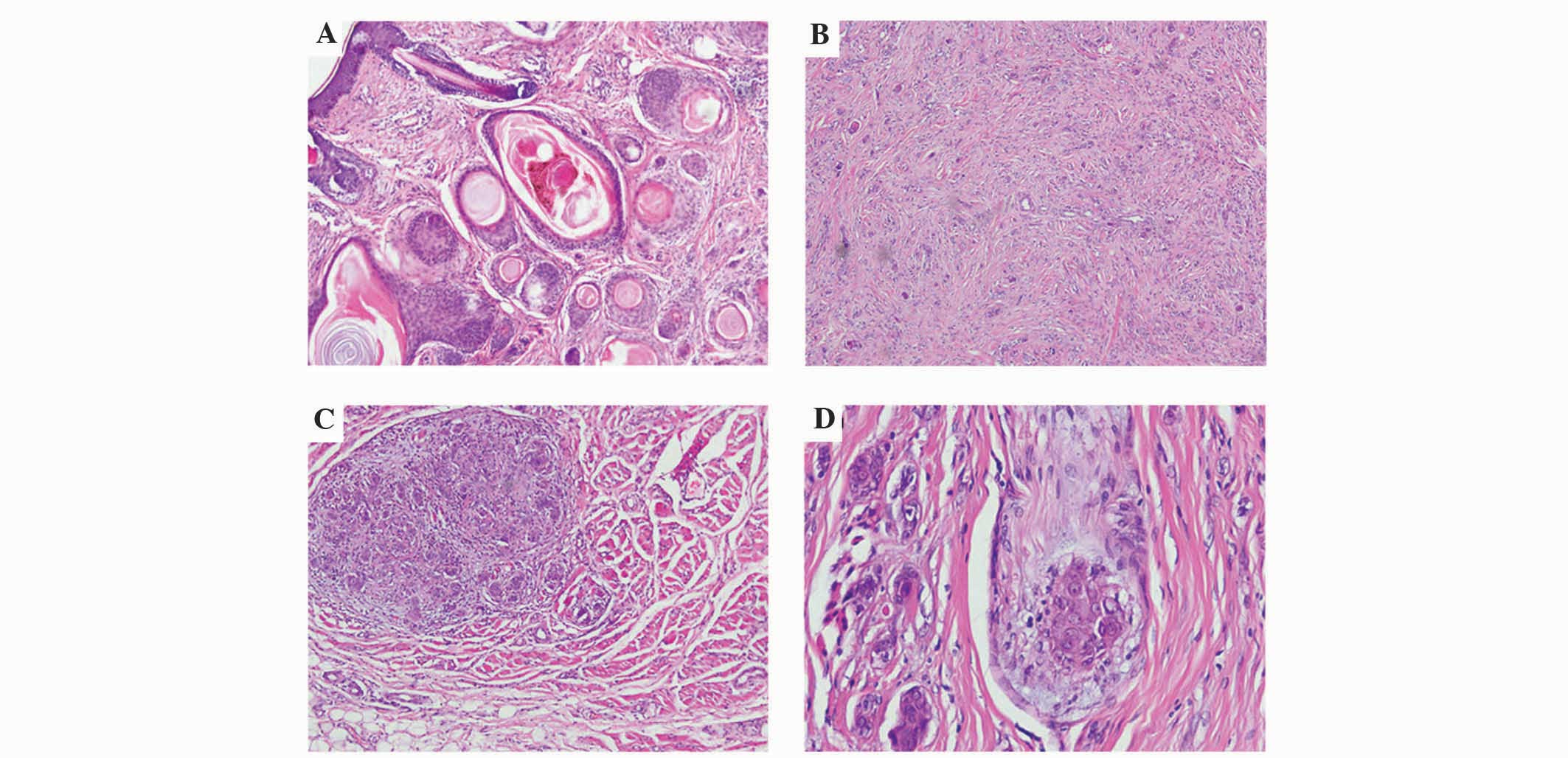
Hematoxylin and eosin staining (ZSGB-BIO, Beijing,
China) was performed on 4-µm thick formalin-fixed and
paraffin-embedded resected tumor tissue. Staining was visualized
using a BX53 microscope (Olympus Corporation, Tokyo, Japan).
Histopathological analysis demonstrated that MAC had infiltrated a
number of muscle tissues and peripheral nerve fibers (Fig. 4). Surgical margins were negative. No
chemotherapy or radiotherapy regimens were administered, and no
recurrence was observed during 6 months of follow-up. Written
informed consent was obtained from the patient for the publication
of this study.
Discussion
The clinical presentation of MAC is
characteristically a smooth-surfaced, slow-growing, firm,
non-ulcerated, asymptomatic papule, plaque or nodule (9). Nonetheless, a small number of patients
are symptomatic at presentation, experiencing burning, paresthesia
and numbness as a result of recurrent perineural invasion (9).
It has been reported in the literature that certain
MAC cases have presented with tumor histories as long as 17 and 27
years (3,10). Notably, due to the asymptomatic
presentation and extremely slow-growth of the tumors, all reported
patients have been diagnosed at least 1 year after the initial
appearance of the lesions. In the present case, the lesion was
present for >10 years prior to diagnosis.
Despite the pathogenesis of MAC not yet being fully
understood, it is believed to originate from pluripotent
keratinocytes, which are capable of differentiation into hair
follicles or sweat glands (11).
Clinically, the disease presents in the fourth to seventh decades
of life, with no evident gender predilection (11,12). In
85% of cases, the tumors develop in the head and neck area
(13), demonstrating a preference for
the periorbital skin and the centrofacial region.
MAC is commonly misdiagnosed clinically and
histologically, primarily due to its inconspicuous features
(14). Rustemeyer et al
(15) described a case of the disease
that was misdiagnosed as desmoplastic trichoepithelioma for a
period of 4 years.
The large majority of reported MAC cases have
occurred in Caucasians; however, a small number of reports in the
literature have described disease occurrence in non-Caucasians
(6,7).
To the best of our knowledge, there are currently no reports in the
English literature regarding Chinese patients with MAC. However,
due to the high prevalence of misdiagnosis and possible
under-recognition of the disease within this population, a
diagnosis of MAC may be significantly overlooked in non-Caucasian
individuals as it most commonly occurs in Caucasians. The present
case demonstrates the requirement to include MAC in the
differential diagnosis in non-Caucasian patients.
The disease presents histologically as a
deeply-infiltrative and poorly-circumscribed tumor, consisting of
solid aggregates of tumor cells in the mid dermis, superficial
keratinous cysts and elongated tubular structures in the deep
aspect of the lesion. These cell nests are enveloped by dense,
fibrous stroma (16).
MAC is resistant to radiotherapy and chemotherapy,
which may be predicted from its slow biological activity (9). The preferred treatment option is
complete surgical excision; however, the true tumor-free margins
are typically far beyond the intraoperative macroscopically
established margins (17,18). Mohs micrographic surgery may be
regarded as the gold standard treatment option, with adjuvant
radiotherapy and wide local excision offering comparable efficacy
(19). When performing adjuvant
radiotherapy, a dose of >50 Gy should be administered with wide
margins (3–5 cm), owing to the tendency of the lesion for
perineural and deep invasion (20).
The current patient was not administered any chemotherapy or
radiotherapy.
The aggressive and locally invasive nature of the
disease results in high recurrence rates, ranging from 15–60%
depending on the treatment modality, with lower rates of recurrence
observed following Mohs micrographic surgery (21–24).
However, such data may be an overestimate, with misdiagnosis often
occurring at the time of excision, and positive margins can
occasionally be misread.
It has been reported that tumor recurrence may occur
up to 30 years after the initial surgical excision (12), highlighting the importance of regular,
long-term follow-up.
Regional and distant metastasis have been described
in the literature; however, such cases are particularly rare, with
only five cases of local recurrence and three cases of distant
metastasis reported (25,26). According to the relevant literature,
only one mortality has occurred as a result of the disease
(27).
MAC is extremely rare among non-Caucasians, with the
majority of cases presenting in Caucasian individuals. The present
case describes the occurrence of MAC of the lip in a Chinese woman.
To the best of our knowledge, the current case is the first of its
kind to be reported in the English literature. The case highlights
the importance of the inclusion of MAC within the differential
diagnosis in non-Caucasian individuals, and additionally aims to
increase the awareness and aid the management of MAC in
non-Caucasian populations.
References
|
1
|
Goldstein DJ, Barr RJ and Cruz Santa DJ:
Microcystic adnexal carcinoma: A distinct clinicopathologic entity.
Cancer. 50:566–572. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cooper PH, Mills SE and Leonard DD:
Sclerosing sweat duct (syringomatous) carcinoma. Am J Surg Pathol.
9:422–433. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nickoloff BJ, Fleischmann HE, Carmel J,
Wood CC and Roth RJ: Microcystic adnexal carcinoma:
Immunohistologic observations suggesting dual (pilar and eccrine)
differentiation. Arch Dermatol. 122:290–294. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wick MR, Goellner JR, Wolfe JT III and Su
WP: Adnexal carcinomas of the skin. I. Eccrine carcinomas. Cancer.
56:1147–1162. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yu JB, Blitzblau RC, Patel SC, Decker RH
and Wilson LD: Surveillance, Epidemiology, and End Results (SEER)
database analysis of microcystic adnexal carcinoma (sclerosing
sweat duct carcinoma) of the skin. Am J Clin Oncol. 33:125–127.
2010.PubMed/NCBI
|
|
6
|
Gardner ES and Goldberg LH: Neglected
microcystic adnexal carcinoma: The second reported case in a black
patient. Dermatol Surg. 27:678–680. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Park JY and Parry EL: Microcystic adnexal
carcinoma. First reported case in a black patient. Dermatol Surg.
24:905–907. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fang W, Chen D, Shang JF, Wang F and Xiao
L: Microcystic adnexal carcinoma: Report of two cases. Zhonghua
Bing Li Xue Za Zhi. 38:59–60. 2009.(In Chinese). PubMed/NCBI
|
|
9
|
Wetter R and Goldstein GD: Microcystic
adnexal carcinoma: A diagnostic and therapeutic challenge. Dermatol
Ther. 21:452–458. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Miyamoto T, Kambe N, Nishiura S, Mihara M
and Shimao S: Microcystic adnexal carcinoma. Electron microscopic
and immunohistochemical study. Dermatologica. 180:40–43. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
LeBoit PE and Sexton M: Microcystic
adnexal carcinoma of the skin. A reappraisal of the differentiation
and differential diagnosis of an underrecognized neoplasm. J Am
Acad Dermatol. 29:609–618. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Burns MK, Chen SP and Goldberg LH:
Microcystic adnexal carcinoma: Ten cases treated by Mohs
micrographic surgery. J Dermatol Surg Oncol. 20:429–433. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Thomas CJ, Wood GC and Marks VJ: Mohs
micrographic surgery in the treatment of rare aggressive cutaneous
tumors: The Geisinger experience. Dermatol Surg. 33:333–339. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wu-Chen WY, Weng CY, Rajan KD, Eberhart C
and Miller NR: Unusual presentation of primary orbital microcystic
adnexal carcinoma. J Neuroophthalmol. 31:147–150. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Rustemeyer J, Zwerger S, Pörksen M and
Junker K: Microcystic adnexal carcinoma of the upper lip
misdiagnosed benign desmoplastic trichoepithelioma. Oral Maxillofac
Surg. 17:141–144. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Klein W, Chan E and Seykora JT: Tumors of
the epidermal appendages. Lever's Histopathology of the Skin. Elder
DE: (9th). Lippincott Williams & Wilkins. (Edinburgh). 897–898.
2005.
|
|
17
|
Lober CW and Larbig GG: Microcystic
adnexal carcinoma (sclerosing sweat duct carcinoma). South Med J.
87:259–262. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mayer MH, Winton GB, Smith AC, Lupton GP,
Parry EL and Shagets FW: Microcystic adnexal carcinoma (sclerosing
sweat duct carcinoma). Plast Reconstr Surg. 84:970–975. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chaudhari SP, Mortazie MB, Blattner CM,
Garelik J, Wolff M, Daulat J and Chaudhari PJ: Treatments for
microcystic adnexal carcinoma - A review. J Dermatolog Treat.
11:1–7. 2015.(Epub ahead of print).
|
|
20
|
Baxi S, Deb S, Weedon D, Baumann K and
Poulsen M: Microcystic adnexal carcinoma of the skin: The role of
adjuvant radiotherapy. J Med Imaging Radiat Oncol. 54:477–482.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chiller K, Passaro D, Scheuller M, Singer
M, McCalmont T and Grekin RC: Microcystic adnexal carcinoma:
Forty-eight cases, their treatment and their outcome. Arch
Dermatol. 136:1355–1359. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nelson PS, Bourgeois KM, Nicotri T Jr,
Chiu ES and Poole JC: Sclerosing sweat duct carcinoma in a
6-year-old African American child. Pediatr Dermatol. 25:38–42.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cooper PH: Sclerosing carcinomas of sweat
ducts (microcystic adnexal carcinoma). Arch Dermatol. 122:261–264.
1986. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Leibovitch I, Huilgol SC, Selva D, Lun K,
Richards S and Paver R: Microcystic adnexal carcinoma: Treatment
with Mohs micrographic surgery. J Am Acad Dermatol. 52:295–300.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gabillot-Carré M, Weill F, Mamelle G, Kolb
F, Boitier F, Petrow P, Ortoli JC, Margulis A, Souteyrand P,
Mercier S, et al: Microcystic adnexal carcinoma: Report of seven
cases including one with lung metastasis. Dermatology. 212:221–228.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ohta M, Hiramoto M and Ohtsuka H:
Metastatic microcystic adnexal carcinoma: An autopsy case. Dermatol
Surg. 30:957–960. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Peterson CM, Ratz JL and Sangueza OP:
Microcystic adnexal carcinoma: First reported case in an African
American man. J Am Acad Dermatol. 45:283–285. 2001. View Article : Google Scholar : PubMed/NCBI
|