Introduction
Schwannomas are tumors originating from Schwann
cells. This type of tumor may be found throughout the body along
the peripheral nerves; however schwannomas of the colon and rectum
are extremely rare (1). This rare
tumor accounts for 2–6% of all mesenchymal tumors (2). The incidence rates of schwannoma are
identical for men and women, and the age of such patients is
between 60 and 65 years (3). Due to
the small number of such cases, the characteristics of this tumor
are not fully established (4).
Immunohistochemistry of the tumor cells remains the most important
diagnostic method. When the tumor is located in the colon or in the
rectum, radical excision with wide margins is mandatory, due to its
tendency to recur locally or become malignant if left untreated.
The surgical approach depends on the size, location and
histopathological pattern of the tumor (4). The use of radiotherapy or adjuvant
chemotherapy has conflicting results and is not recommended for
routine use. The present study reports a rare case of a schwannoma
present in the ascending colon that was detected by colonoscopy and
abdominal computed tomography (CT) scanning, and required surgical
resection.
Case report
A 62-year-old female patient was admitted to The
First Affiliated Hospital of Zhejiang University School of Medicine
(Hangzhou, China), presenting with abdominal pain and a history of
intermittent, dark-red bloody stools for 1 month. The patient's
medical history included uterine fibroids and hypertension. The
patient had no other specific medical conditions, including
neurofibromatosis. There was no family history of inflammatory
bowel disease or cancer, and she had had no prior abdominal
surgeries. A physical examination revealed mild tenderness in the
right lower quadrant. The laboratory test results were normal. A
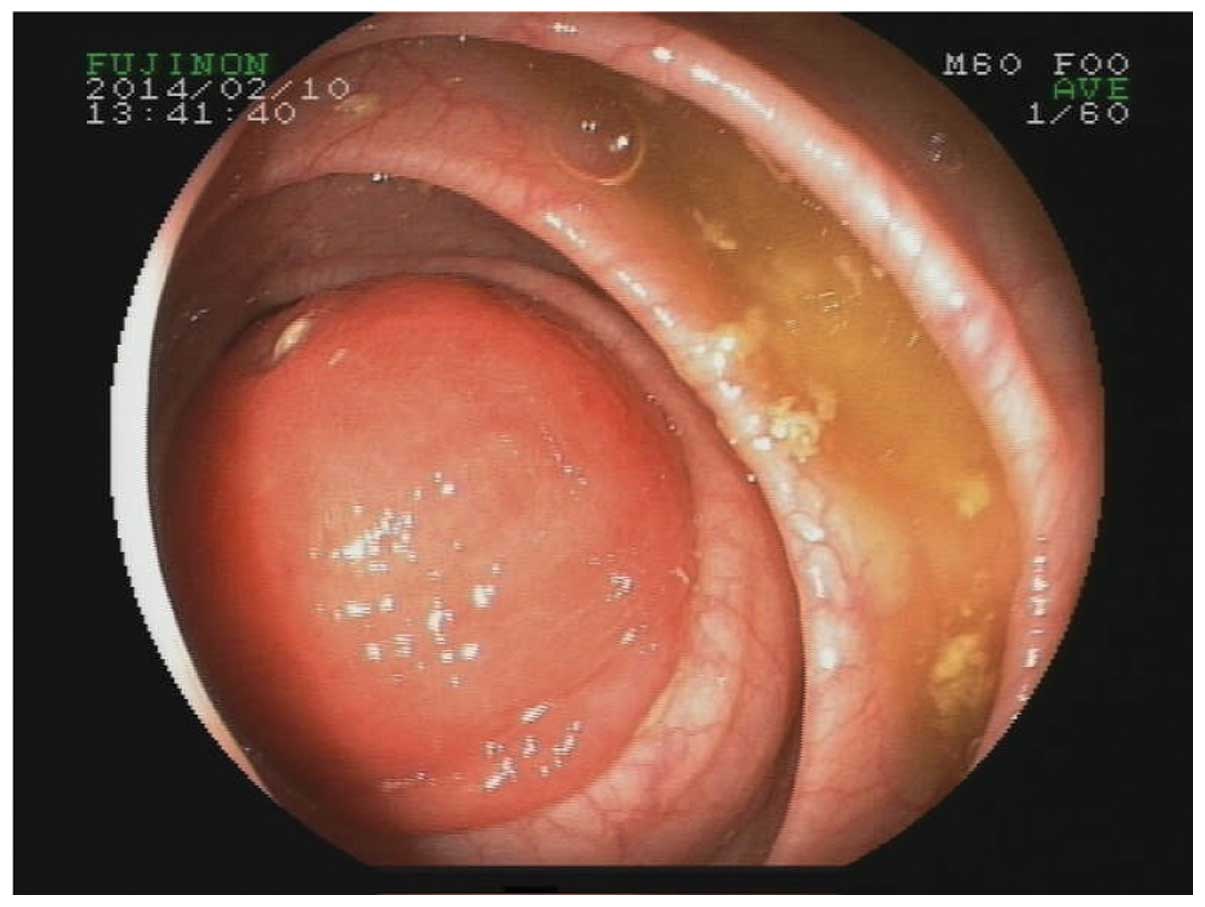
colonoscopy (Olympus Corporation, Toyko, Japan) revealed a
pedunculated mass in the proximal ascending colon measuring ~4×4 cm
(Fig. 1). No lesions were found in
the other colon segments, including the cecum. An abdominal CT scan
(Aquilion 16; Toshiba, Tokyo, Japan) revealed a round, homogeneous,
low-attenuation mass in the proximal ascending colon, without
adjacent wall thickening (Fig. 2). No
enlarged pericolic lymph nodes were observed.
The patient underwent a right hemicolectomy without
a preoperative endoscopic biopsy. The procedure involved removal of
the bowel from 4–6 cm proximal to the ileocecal valve to the
portion of the transverse colon supplied by the right branch of the
middle colic artery. An anastomosis was fashioned between the
terminal ileum and the transverse colon. No infiltration or distant
dissemination was identified. The resected specimens were fixed
with 10% formalin fixative and 95% ethanol fixative, dehydrated,
embedded in wax, sectioned and stained with hematoxylin and eosin
(Leica Microsystems, Inc., Buffalo Grove, IL, USA). Microscopic
analysis revealed that the tumor was composed of proliferating
spindle cells arranged in fascicular or vague palisading patterns,
in a loose edematous stroma with inflammatory cell infiltration
(Fig. 3; hematoxylin and eosin
stain). Immunohistochemical analysis revealed that the tumor was
positive for S-100; however, no reactivity for cluster of
differentiation (CD) 117, CD34, desmin, smooth muscle actin or
discovered on gastrointestinal stromal tumor-1 was detected. Ki-67
labeling was observed in <3% of the tumor cells. The definitive
diagnosis was schwannoma of the colon. No recurrence was observed
during the 24-month follow-up period and no additional treatment
was administered.
Discussion
Verocay first described schwannomas in 1910
(4). Despite the increasing number of
mesenchymal tumor reports with the advent of modern
immunohistochemical staining techniques, primary schwannomas of the
colon and rectum that are not associated with systemic
neurofibromatosis (von Recklinghausen disease) are extremely rare
(5,6).
Due to the small number of such cases, the incidence rates and
characteristics of schwannomas have not been fully determined.
Schwannomas are known to be benign neoplasms of ectodermal origin,
which are characterized by slow growth and the capability for
malignant degeneration if not removed (5–7). This type
of tumor typically manifests as a polyp that may ulcerate the
mucosa (8,9), leading to nonspecific symptoms,
including abdominal pain with rectal bleeding, defecation disorders
and colonic obstruction or invagination, as in the present case
(10,11). Imaging findings are nonspecific; CT
scans show well-defined, homogeneous mural masses, and can help to
distinguish schwannomas from gastrointestinal stromal tumors
(GISTs), which are heterogeneous masses (12). On most occasions, diagnosis is not
established based on a biopsy but on a surgical specimen (13).
Macroscopically, schwannomas are well-circumscribed,
yellowish-white lesions (4).
Immunohistochemical examination of the tumor cells is considered
the optimal diagnostic tool for this type of tumor (14). Schwannomas usually exhibit positive
reactivity for S-100, vimentin and glial fibrillary acidic protein,
and no reactivity for CD117, CD34, actin or cytokeratins, which
appear more typically in GISTs, gastrointestinal autonomic tumors
or muscle tumors (15,16). Following diagnosis, treatment options
include polypectomy or segmental colectomy with free margins due to
the low risk of malignancy (17,18). The
benign nature of the tumor is responsible for the good prognosis of
patients with schwannoma; recurrence and metastasis are considered
rare events. In conclusion, colonic schwannoma is a rare tumor with
a benign behavior and patients with this type of tumor have a
favorable prognosis.
Acknowledgements
This study was supported by the Natural Science
Foundation of Zhejiang Province (grant no. LY13H030004).
References
|
1
|
Zippi M, Pica R, Scialpi R, Cassieri C,
Avallone EV and Occhigrossi G: Schwannoma of the rectum: A case
report and literature review. World J Clin Cases. 1:49–51. 2010.
View Article : Google Scholar
|
|
2
|
Verdú-Fernández MÁ, Guillén-Paredes MP,
García-García ML, García-Marín JA, Pellicer-Franco E and
Aguayo-Albasini JL: Schwannoma in descending colon: Presentation of
a neoplasm in a rare location. Rev Esp Enferm Dig. 105:502–503.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Miettinen M, Sarlomo-Rikala M and Lasota
J: Gastrointestinal stromal tumours. Ann Chir Gynaecol. 87:278–281.
1998.PubMed/NCBI
|
|
4
|
Baek SJ, Hwangbo W, Kim J and Kim IS: A
case of benign schwannoma of the ascending colon treated with
laparoscopic-assisted wedge resection. Int Surg. 98:315–318. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Daimaru Y, Kido H, Hashimoto H and Enjoji
M: Benign schwannoma of the gastrointestinal tract: A
clinicopathologic and immunohistochemical study. Hum Pathol.
19:257–264. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nonose R, Lahan AY, Valenciano Santos J
and Martinez CA: Schwannoma of the colon. Case Rep Gastroenterol.
3:293–299. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lauwers GY, Erlandson RA, Casper ES,
Brennan MF and Woodruff JM: Gastrointestinal autonomic nerve
tumors: A clinicopathological, immunohistochemical and
ultrastructural study of 12 cases. Am J Surg Pathol. 17:887–897.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kwon MS, Lee SS and Ahn GH: Schwannomas of
the gastrointestinal tract: Clinicopathological features of 12
cases including a case of esophageal tumor compared with those of
gastrointestinal stromal tumors and leiomyomas of the
gastrointestinal tract. Pathol Res Pract. 198:605–613. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tanaka T, Ishihara Y, Takabayashi N,
Kobayashi R, Hiramatsu T and Kuriki K: Gastrointestinal:
Asymptomatic colonic schwannoma in an elderly woman; a rare case. J
Gastroenterol Hepatol. 26:13392011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Martínez Crespo JJ, Vicente JJ, García
Pérez B, Pérez Guillermo M and González Costea R: Atipic
manifestation of an infrequent lesion. Video- and ecoendoscopy in a
gastric schwannoma. Rev Esp Enferm Dig. 97:844–845. 2005.PubMed/NCBI
|
|
11
|
Kim HJ, Kim CH, Lim SW, Huh JW, Kim YJ and
Kim HR: Schwannoma of ascending colon treated by laparoscopic right
hemicolectomy. World J Surg Oncol. 10:812012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Levy AD, Quiles AM, Miettinen M and Sobin
LH: Gastrointestinal schwannomas: CT features with
clinicopathologic correlation. AJR Am J Roentgenol. 184:797–802.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yoon W, Paulson K, Mazzara P, Nagori S,
Barawi M and Berri R: Gastric schwannoma: A rare but important
differential diagnosis of a gastric submucosal mass. Case Rep Surg.
2012:2809822012.PubMed/NCBI
|
|
14
|
Arai T, Sugimura H, Suzuki M, Iwase T,
Sakuramachi S, Kimura T, Harada Y and Kino I: Benign schwannoma of
the esophagus: Report of two cases with immunohistochemical and
ultrastructural studies. Pathol Int. 44:460–465. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Torres Gómez FJ, Fernández Machín P, del
Álamo Juzgado C, Martínez A, Martínez Moyanol A and Moreno Corral
S: Schwannoma quístico de colon. Presentación de un caso. Rev Esp
Patol. 42:143–146. 2009.
|
|
16
|
Hou YY, Tan YS, Xu JF, Wang XN, Lu SH, Ji
Y, Wang J and Zhu XZ: Schwannoma of the gastrointestinal tract: A
clinicopathological, immunohistochemical and ultrastructural study
of 33 cases. Histopathology. 48:536–545. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Park KJ, Kim KH, Roh YH, Kim SH, Lee JH,
Rha SH and Choi H: Isolated primary schwannoma arising on the
colon: Report of two cases and review of the literature. J Korean
Surg Soc. 80:367–372. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Watanabe A, Ojima H, Suzuki S, Mochida Y,
Hirayama I, Hosouchi Y, Nishida Y, Kashiwabara K, Ohno T, Mochiki E
and Kuwano H: An individual with gastric schwannoma with
pathologically malignant potential surviving two years after
laparoscopy-assisted partial gastrectomy. Case Rep Gastroenterol.
5:502–507. 2011. View Article : Google Scholar : PubMed/NCBI
|