Introduction
Approximately 200,000 patients are diagnosed with
cutaneous melanoma (CM) annually worldwide, and 46,000 succumb to
the disease (1). The incidence of CM
has steadily increased over the last 50 years in the majority of
fair-skinned populations (2–5), even though the great majority of the
increase in melanoma incidence has been suggested to be due to an
increase in the diagnosis of thin lesions that possess an excellent
prognosis (6,7), and a previous study demonstrated a
change in the trend suggesting that the most recent generation are
at a lower risk of developing melanoma (8).
Mortality rates have not been observed to parallel
incidence rates. In Australia, mortality rates peaked in 1985 and
then stopped rising (9), while in the
USA, between 1992 and 2006, mortality rates increased only in
patients >65 years old (10). In
Europe, melanoma mortality doubled in men, but remained unchanged
in women (11).
The discrepancy between incidence and mortality
trends has been discussed and certain studies attribute this trend
to the detection of melanoma at earlier stages in women compared
with men (12), or in general to the
over-diagnosis of thin slow melanoma. Other studies have suggested
that part of the melanoma epidemic is comprised of
non-life-threatening melanomas that may be promoted by sun exposure
(13).
Solar radiation is an established skin carcinogen
(14,15), however, sun exposure is additionally
the primary source of vitamin D, and it has been demonstrated that
vitamin D is associated with a reduced risk of cancer and overall
mortality (16–19). Thus, the main cause of melanoma may be
intentional ultraviolet (UV) exposure, as a continuous pattern of
sun exposure may not be significant risk factor, as it has been
shown in a previous meta-analysis (14). However, intermittent sun exposure and
sunbed use are consistently associated with an increased risk of
melanoma (20).
In a cohort of Swedish women, overall mortality was
significantly reduced by 30% among those who had taken vacations
featuring exposure to sun more than once a year over 3 decades.
Conversely, solarium use one or more times per month for at least a
decade significantly increased the risk of all causes of mortality
and cancer-associated mortality compared with those who never used
solaria (21). Consistently, in a
previous study of an Italian patient cohort, holidays with exposure
to the sun prior to diagnosis were associated with thinner
melanomas in women and reduced rates of relapse in the two genders
(22).
The present study aimed to confirm previously
observed results in a larger patient cohort, investigating the
primary prognostic factors of melanoma in association with sun and
artificial light exposure, and adjusting for possible confounders,
including socioeconomic factors, history of non-melanoma skin
cancer, body site, specialization of diagnosing doctors and season
of diagnosis.
Materials and methods
Patients and data collection
Since December 2010, the present hospital-based
multicenter study of melanoma cases has been ongoing in Italy.
Patients exhibiting a histologically confirmed diagnosis of primary
CM were recruited from Italian institutions (hospitals and
university settings, including dermatological, surgical and
oncological units) between December 2010 and December 2013.
Following the provision of written informed consent, patients were
enrolled in the study and all data expected from the study plan was
collected via an electronic Case Report Form (eCRF), which was
developed by Clinical Research Technology S.r.l. (Salerno, Italy)
on its clinical platform ‘eClinical’. ‘eClinical’ assigned an
identification (ID) number to all screened patients.
The acquisition and collection of clinical data were
achieved through utilizing central web based systems (http://imi.cr-technology.com/cnmr/). eClinical
software was compliant with Computer System Validation (US Food and
Drug Administration-21 CFR Part 11: Electronic Records; Electronic
Signatures; http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=11)
(23). The eCRF layout was designed
to collect the data specified by the study protocol. Among other
features, eClinical assigned a unique and secure User ID/password
combination for each clinical research team member, managed queries
and developed descriptive statistics. The quality of the electronic
data was verified against the source documents via onsite
monitoring visits periodically undertaken during the study.
Patients interviewed at the initial diagnosis of melanoma were
considered as incident cases.
Study variables
A self-administered questionnaire, which collected
information on sociodemographic variables (age at melanoma
diagnosis, gender and level of education), body mass index (BMI),
host factors (phenotype), UV exposure (holidays with sun exposure
in the previous 5 years), sun exposure during peak hours of
sunlight (11:00 a.m. to 1:00 p.m.) in the previous 2 years, sunbed
use (prior to the age of 30), geographical residence, season of
diagnosis and site of melanoma (head and neck, trunk, upper limb
and lower limb). Skin sensitivity to UV was measured using the
Fitzpatrick classification, with a six-level scale ranging from
subjects who always tan and never burn to subjects who always burn
when exposed to sun (24).
Statistical analysis
Associations between categorical variables at
baseline and Breslow thickness were evaluated using non-parametric
median two-sample tests that evaluated differences in median
Breslow thickness. Associations between categorical variables and
frequencies of patients with holidays with sun exposure were
evaluated using the χ2 test or Fisher's exact test, as
appropriate.
Multivariate analyses were performed with Breslow
thickness as the response variable, and also to investigate
variables associated with sunbed use and holidays with sun
exposure. Information on lesion thickness was investigated and
patients were grouped into two categories, thin and thick melanoma
(Breslow thickness, ≤1.00 and >1.00 mm, respectively),
considering very thick melanoma (Breslow thickness, >2.00 mm)
and additionally evaluating Breslow thickness as a continuous
measure. Multivariate logistic models were utilized to evaluate the
associations for thick and very thick melanoma. Multivariate random
effects models, with center considered as a random factor, were
introduced, transforming Breslow thickness in order to achieve a
normal distribution of residuals. All possible confounding factors,
including age, gender, educational and professional level,
phenotype, residence, season of diagnosis and speciality of
diagnosing doctor were evaluated in the multivariate models.
All analyses were performed with SAS software
version 9.2 (SAS Institute, Cary, NC, USA) and R software, version
2.12.2 (http://www.r-project.org). All reported
P-values were two-sided (P<0.05).
Results
Characteristics of the patient
cohort
Patients from 38 centers were included in the
present study: 50% from the north, 11% from the center and 40% from
the south of Italy and its islands. A total of 33% of the centers
were dermatology units. For the present analysis, patients
exhibiting CM with information on melanoma thickness were selected.
From 3,111 patients, the following cases were excluded: Acral
lentiginous melanoma (n=12; 0.4%), mucosal lentiginous melanoma
(n=14; 0.5%), vulvar and anorectal melanoma (n=18; 0.6%), in
situ melanoma (n=41; 1%) and retrospective melanoma (n=288;
9%). Following exclusion, a final cohort of 2,738 patients
diagnosed between December 2010 and December 2013 remained, and 99%
of these patients exhibited first primary melanoma.
The median patient age was 55 years (interquartile
range, 43–68 years). In total, 51% (n=1,398) of patients were men
and 57% (n=1,553) had a high level of education (at least high
school). Furthermore, 9% (n=234) of the patients had melanoma
familiarity and 56% (n=1,527) exhibited a fair phenotype
(Fitzpatrick skin type I or II). A total of 50% (n=1,375) of
patients exhibited a thin melanoma (Breslow thickness, ≤1 mm), and
29% percent (n=806) had a very thick melanoma (Breslow thickness,
>2 mm). Additionally, 25% (n=694) of patients had ulcerated
melanoma, and 1% (n=34) exhibited distant metastases, with lymph
node involvement in 13% (n=357) of patients. A total of 28% (n=774)
of patients were diagnosed by a dermatologist and significantly
(P<0.001) higher numbers of thin melanoma cases were diagnosed
by dermatologists (53%) compared with other types of medical doctor
(46%).
A number of factors are associated
with sunbed use and holidays with sun exposure
Sunbed use was significantly associated with age
(P<0.0001), gender (P<0.0001), BMI (P=0.004), social economic
status (SES; P=0.0003) and holidays with sun exposure
(P<0.0001), with an increased prevalence among younger women
(<55 years) with low BMI (<25) (Table I). However, holidays with sun exposure
were associated with SES (P<0.0001) and residence (P<0.0001),
but not with gender or BMI (Table
I).
 | Table I.Odds ratio and 95% confidence
interval for use of sunbeds and holidays with sun exposure from the
multivariate model. |
Table I.
Odds ratio and 95% confidence
interval for use of sunbeds and holidays with sun exposure from the
multivariate model.
| A, Odds ratio and
95% confidence interval for use of sunbeds from the multivariate
model |
|---|
|
|---|
| Variable | Category | Odds ratio | 95% confidence
interval |
P-valuea |
|---|
| Age, years | ≥55 vs. <55 | 0.29 | 0.22–0.38 | <0.0001 |
| Gender | Men vs. women | 0.44 | 0.34–0.57 | <0.0001 |
| Body mass
index | ≥25 vs. <25 | 0.64 | 0.50–0.82 | 0.0004 |
| SESb | High vs. low | 1.20 | 1.01–1.32 | 0.0003 |
| Sun exposure | Yes vs. no | 2.19 | 1.64–2.93 | <0.0001 |
|
| B, Odds ratio and
95% confidence interval for holidays with sun exposure from the
multivariate model |
|
| Variable | Category | Odds ratio | 95% confidence
interval |
P-valuec |
|
| Age, years | ≥55 vs. <55 | 0.45 | 0.37–0.53 | <0.0001 |
| SESb | High vs. low | 1.36 | 1.27–1.46 | <0.0001 |
| Residence | North vs.
south | 0.75 | 0.62–0.89 | <0.0001 |
|
| Centre vs.
south | 1.54 | 1.13–2.10 | <0.0001 |
| Sunbed use | Yes vs. no | 2.25 | 1.69–2.99 | <0.0001 |
Table II presents the
associations between patient characteristics and holidays with sun
exposure. Thick melanoma was less frequent among patients taking
holidays with sun exposure compared with those who did not take
holidays with sun exposure (57 vs. 46%; P<0.0001). Patients with
a history of holidays with sun exposure in the 5 years prior to
diagnosis were younger (patients ≥55 years old demonstrated 39 vs.
66%, for holidays with sun exposure vs. holidays with no sun
exposure; P<0.0001), had a higher educational and professional
level (P<0.0001), and possessed a fair phenotype (54 vs. 61%,
for holidays with sun exposure vs. holidays with no sun exposure;
P=0.004) and low BMI (49 vs. 59% BMI ≥25, for holidays with sun
exposure vs. holidays with no sun exposure; P<0.0001).
 | Table II.Association between patient
characteristics and holidays with sun exposure. |
Table II.
Association between patient
characteristics and holidays with sun exposure.
| Variable | Total | Holidays with sun
exposure | Holidays with no
sun exposure |
P-valuea |
|---|
| Total patients,
n | 2673b | 1678 | 995 |
|
| Breslow thickness,
n (%) |
|
|
| <0.0001 |
| <1
mm | 1329 (50) | 902 (54) | 427 (43) |
|
| ≥1
mm | 1344 (50) | 776 (46) | 568 (57) |
|
|
Missing | 0 | 0 | 0 |
|
| Gender, n (%) |
|
|
| 0.29 |
|
Men | 1391 (52) | 860 (51) | 531 (53) |
|
|
Women | 1282 (48) | 818 (49) | 464 (47) |
|
|
Missing | 0 | 0 | 0 |
|
| Age, years, n
(%) |
|
|
| <0.0001 |
|
<55 | 1351 (51) | 1018 (61) | 333 (33) |
|
|
≥55 | 1318 (49) | 658 (39) | 660 (66) |
|
|
Missing | 4 | 2 | 2 |
|
| Education level, n
(%) |
|
|
| <0.0001 |
|
Low | 1046 (39) | 501 (30) | 545 (55) |
|
|
High | 1550 (58) | 1140 (68) | 410 (41) |
|
|
Missing | 77 | 37 | 40 |
|
| Profession level, n
(%) |
|
|
| <0.0001 |
|
Low | 1507 (56) | 848 (51) | 659 (66) |
|
|
High | 1166 (44) | 830 (49) | 336 (34) |
|
|
Missing | 0 | 0 | 0 |
|
| Skin
typec, n (%) |
|
|
| 0.004 |
|
Dark | 1149 (43) | 765 (46) | 384 (39) |
|
|
Fair | 1523 (57) | 913 (54) | 610 (61) |
|
|
Missing | 1 | 0 | 1 |
|
| Season of
diagnosis, n (%) |
|
|
| 0.217 |
|
Winter | 1269 (47) | 818 (49) | 451 (45) |
|
|
Summer | 694 (26) | 422 (25) | 272 (27) |
|
|
Autumn | 710 (27) | 438 (26) | 272 (27) |
|
|
Missing | 0 | 0 | 0 |
|
| Residence, n
(%) |
|
|
| 0.0004 |
|
North | 1298 (49) | 775 (46) | 523 (53) |
|
|
Center | 296 (11) | 218 (13) | 78 (8) |
|
|
South | 1058 (40) | 672 (40) | 386 (39) |
|
|
Missing | 21 | 13 | 8 |
|
| Doctor specialty, n
(%) |
|
|
| 0.0174 |
|
Oncologist | 1484 (56) | 904 (54) | 580 (58) |
|
|
Dermatologist | 774 (29) | 503 (30) | 271 (27) |
|
|
Other | 378 (14) | 257 (15) | 121 (12) |
|
|
Missing | 37 | 14 | 23 |
|
| Sunbed use, n
(%) |
|
|
| <0.0001 |
|
None | 2253 (84) | 1329 (79) | 924 (93) |
|
|
Few | 338 (13) | 280 (17) | 58 (6) |
|
|
Often | 72 (3) | 61 (4) | 11 (1) |
|
|
Missing | 10 | 8 | 2 |
|
| Body mass index, n
(%) |
|
|
| <0.0001 |
|
<25 | 1262 (47) | 853 (51) | 409 (41) |
|
|
≥25 | 1406 (53) | 823 (49) | 583 (59) |
|
|
Missing | 5 | 2 | 3 |
|
A number of factors are associated
with Breslow thickness and ulceration
Table III presents
sociodemographic characteristics that were identified to be
significantly associated with Breslow thickness in a multivariate
random effects model. As expected, men, patients >55 years old
and patients with a low education had a significantly greater
Breslow thickness compared with women, younger patients and more
educated patients (Table III). BMI
was also independently identified to be significantly associated
with Breslow thickness.
 | Table III.Median Breslow thickness with patient
features and results from multivariate random effects model. |
Table III.
Median Breslow thickness with patient
features and results from multivariate random effects model.
| Variable | n | Median | Lower quartile | Upper quartile |
P-valuea |
|---|
| Overall | 2738 | 1.1 | 0.5 | 2.4 |
|
| Gender |
|
|
|
| 0.0002 |
|
Men | 1398 | 1.2 | 0.6 | 2.7 |
|
|
Women | 1284 | 0.9 | 0.5 | 2.1 |
|
| Educational
levelb |
|
|
|
| 0.005 |
|
Low | 1048 | 1.3 | 0.6 | 3.3 |
|
|
High | 1553 | 0.9 | 0.5 | 1.9 |
|
| Professional
levelc |
|
|
|
| 0.012 |
| No | 1572 | 1.2 | 0.6 | 2.8 |
|
|
Yes | 1166 | 0.9 | 0.5 | 1.8 |
|
| Body mass
index |
|
|
|
| 0.0008 |
|
<25 | 1265 | 0.8 | 0.5 | 2.0 |
|
|
≥25 | 1412 | 1.2 | 0.6 | 3.0 |
|
| Age, years |
|
|
|
| <0.0001 |
|
<55 | 1360 | 0.8 | 0.5 | 1.7 |
|
|
≥55 | 1327 | 1.3 | 0.6 | 3.4 |
|
| Season of
diagnosisd |
|
|
|
| 0.002 |
| Winter
and spring | 1307 | 1.1 | 0.5 | 2.6 |
|
|
Summer |
712 | 1.1 | 0.6 | 2.4 |
|
|
Autumn |
719 | 0.9 | 0.5 | 2.0 |
In a multivariate logistics model, evaluating the
association with >1 mm Breslow thickness, and adjusting for age,
gender, residence, socioeconomic factors (education and
profession), skin awareness/screening indicators (specialization of
medical doctor performing the diagnosis and season of diagnosis)
and BMI, holidays with sun exposure remained significantly
associated with Breslow thickness (P=0.01) (Table IV; Fig.
1), whereas sunbed use and exposure during peak hours of
sunlight were not significantly associated with Breslow thickness.
Similar results were obtained considering ulceration as a response
variable; holidays with sun exposure remained significantly
inversely associated with ulceration (P=0.009; Table IV), as well as number of weeks of
holidays with sun exposure (P=0.011; data not shown).
 | Table IV.Results from multivariate logistic
model for thick and ulcerated melanomas. |
Table IV.
Results from multivariate logistic
model for thick and ulcerated melanomas.
| A, Results from
multivariate logistic model for thick melanoma |
|---|
|
|---|
| Variable | Category | Odds ratio | 95% confidence
interval | P-value |
|---|
| Holidays with sun
exposure | Yes vs. no | 0.79 | 0.65–0.95 | 0.014 |
| Gender | Men vs. women | 1.26 | 1.06–1.50 | 0.010 |
| Age, years | ≥55 vs. <55 | 1.58 | 1.31–1.90 | <0.0001 |
| Educational
level | High vs. low | 0.74 | 0.61–0.89 | 0.002 |
| Professional
level | High vs. low | 0.83 | 0.69–1.00 | 0.048 |
| Body mass
index | ≥25 vs. <25 | 1.34 | 1.12–1.59 | 0.001 |
| Area of residence
in Italy | North vs.
south | 0.52 | 0.43–0.62 | 0.005 |
|
| Center vs.
south | 0.45 | 0.33–0.62 | 0.002 |
| Season of
diagnosis | Winter vs.
autumn | 1.31 | 1.07–1.61 | 0.054 |
|
| Summer vs.
autumn | 1.25 | 0.99–1.56 | 0.388 |
| Specialty of
diagnosing doctor | Oncologist vs.
other | 0.91 | 0.71–1.17 | 0.360 |
|
| Dermatologist vs.
other | 0.70 | 0.53–0.93 | 0.005 |
| Sunbed use | Yes vs. no | 0.83 | 0.64–1.06 | 0.132 |
| Exposure during
peak sunlight hours | Yes vs. no | 1.00 | 0.83–1.21 | 0.979 |
|
| B, Results from
multivariate logistic model for ulcerated melanoma |
|
| Variable | Category | Odds ratio | 95% confidence
interval | P-value |
|
| Holidays with sun
exposure | Yes vs. no | 0.76 | 0.61–0.93 | 0.009 |
| Gender | Men vs. women | 1.41 | 1.17–1.71 | 0.0004 |
| Age, years | ≥55 vs. <55 | 1.47 | 1.19–1.81 | 0.0003 |
| Educational
level | High vs. low | 0.70 | 0.57–0.85 | 0.0004 |
| Area of residence
in Italy | North vs.
south | 0.57 | 0.47–0.70 | 0.157 |
|
| Center vs.
south | 0.45 | 0.31–0.66 | 0.004 |
| Specialty of
diagnosing doctor | Oncologist vs.
other | 0.78 | 0.59–1.02 | 0.413 |
|
| Dermatologist vs.
other | 0.72 | 0.52–0.98 | 0.093 |
| Sunbed use | Yes vs. no | 0.77 | 0.56–1.06 | 0.108 |
| Exposure during
peak sunlight hours | Yes vs. no | 0.97 | 0.78–1.19 | 0.739 |
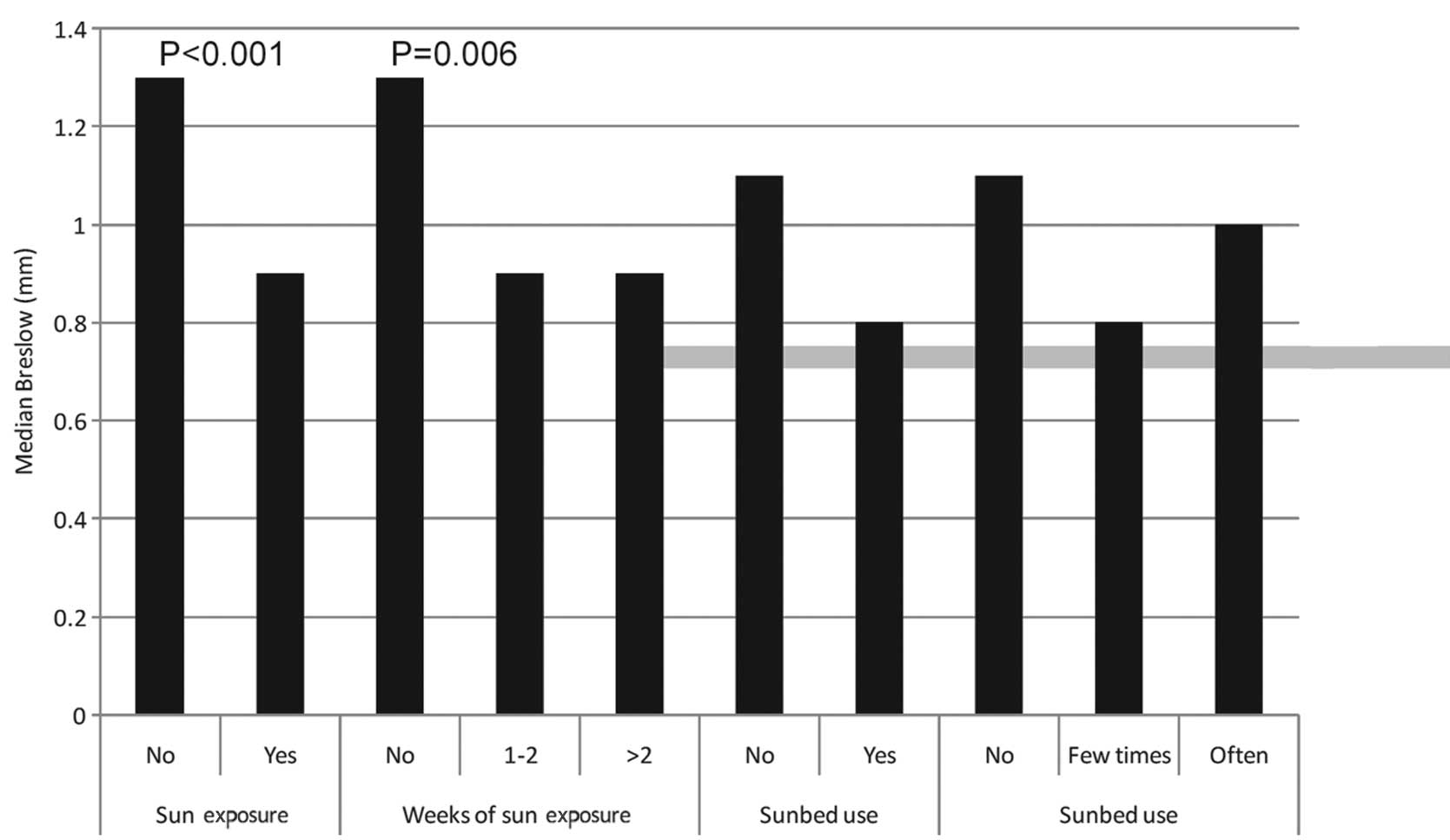
Median Breslow thickness values are presented in
Fig. 2 for a number of categorical
variables that may be potentially associated with sun (or UV)
exposure [holidays with sun exposure in the previous 5 years, sun
exposure during peak hours of sunlight (11:00 a.m. to 1:00 p.m.),
sunbed use and frequency of sunbed use]. Median thickness values
were identified to be significantly lower among patients who took
holidays with sun exposure. Random effects model analysis revealed
that this difference remained significant following adjustment for
confounding factors (including age, gender, education, profession,
BMI and season of diagnosis; P<0.001 and P=0.006 for holidays
with sun exposure and weeks of holiday with sun exposure,
respectively).
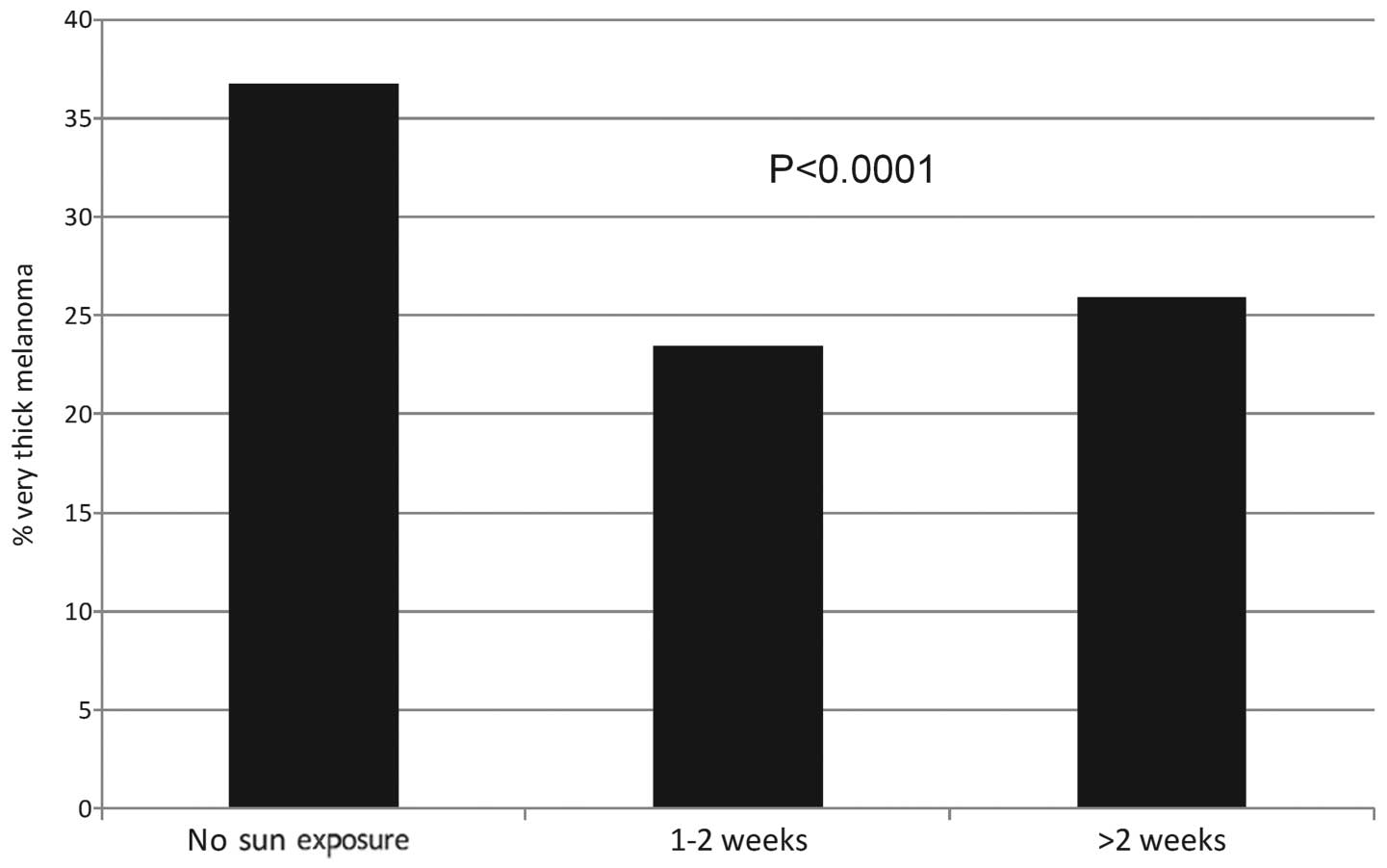
In Fig. 3, frequencies
of very thick melanoma (Breslow thickness, >2.0 mm) are
presented with the number of weeks of holiday with sun exposure.
Frequencies of very thick melanoma were significantly lower in
patients with a history of 1–2 weeks and >2 weeks of holiday
with sun exposure compared with patients with no history of
holidays with sun exposure in the 5 years prior to diagnosis
(P<0.0001, from multivariate logistic model adjusting for
confounding variables).
Discussion
The present study of 2,738 melanoma patients
suggested that holidays with sun exposure prior to diagnosis and
number of weeks of holiday with sun exposure were significantly
inversely associated with Breslow thickness and ulceration, whereas
sunbed use and sun exposure during peak hours of sunlight were not
identified to be associated with CM prognostic factors.
The analysis of skin awareness indicators (CM family
history, visit to a dermatologist rather than a general medical
doctor, diagnosis during summer and phenotype) was taken into
account and results were confirmed. The present study additionally
evaluated socioeconomic factors, as certain previous studies have
demonstrated that low socioeconomic status may be significantly
associated with the survival of melanoma patients (25). Previous holidays with sun exposure and
number of weeks of holiday with sun exposure appear to be
associated with a beneficial effect on disease status, in the form
of less aggressive melanoma.
Solar radiation is a well-established skin
carcinogen (14,15), however, sun exposure is additionally
the primary source of vitamin D. In a previous meta-analysis it was
demonstrated that a continuous pattern of sun exposure was not a
significant risk factor for melanoma, whereas intentional sun
exposure and sunbed use were consistently associated with an
increased risk (14). Furthermore,
the results of the present study are in line with previous studies,
suggesting a beneficial effect of sun exposure on melanoma patient
survival (26) and overall survival
(21). In an Italian population-based
case-control study, multivariate models suggested an inverse
association between holidays with sun exposure prior to diagnosis
and melanoma-associated mortality, in a dose-dependent manner
(27). An international
population-based study of 3,578 melanoma cases revealed that a high
recent UVB dose was associated with a significant 35% reduction in
overall mortality (28).
One hypothesis is that the increased number of
primarily thin melanoma cases and the decrease in recurrence may be
associated with sun exposure, due to a potential link with vitamin
D (29). It has been hypothesized
that sun-associated vitamin D synthesis may have a beneficial
effect on total mortality (16,30–32) and
the incidence of certain types of cancer (17,33).
Additional observational studies identified an inverse association
between vitamin D serum levels and melanoma prognosis (31,32,34).
However, the hypothetical role of vitamin D in the present study
has been extrapolated by declared sun exposure, and such
extrapolation should be performed with caution, particularly as sun
exposure is a well-known risk factor for melanoma.
One novel hypothesis is that a percentage of the
increase in the incidence of melanoma is comprised of
non-life-threatening melanoma cases, which may be promoted by sun
exposure (35,36). Intense recent sun exposure may be able
to trigger melanoma with little malignant potential. If this is
true, then there is a requirement to develop an improved
understanding of what triggers aggressive melanoma.
Population-based registries with clinical data on
melanoma are few in Italy, and the Clinical National Melanoma
Registry (CNMR) does not have the typical aim of cancer registries
to estimate incidence data. The registry is a multi-center
collection of clinical and epidemiological data, with the aim of
improving collaboration between hospitals and research centers in
order to obtain homogeneous data collection of epidemiological and
clinical data on a large data scale. Being able to increase the
statistical power and obtain homogeneous data, particularly for a
rare disease like melanoma, is important when the aim is to
evaluate associations between melanoma prognostic factors and
epidemiological and clinical data, taking into account multiple
confounding variables. CNMR is not a tumor registry and it does not
possess the aim of estimating Italian melanoma incidence rates;
however, the data are comparable with results identified in
population-based tumor registries, for example, significantly
higher Breslow thickness values were observed at an advanced age,
among men and among patients of higher socioeconomic levels
(37).
Even if the present study adjusted for educational
and professional level, it may be supposed that the association
with holidays with sun exposure may remain confounded by
socioeconomic factors that are not easily recorded. For example,
the present study did not record data on salary and economic
factors, as well as information on lifestyle factors and changes in
profession over time. Furthermore, melanoma cases in highly
educated individuals may be diagnosed at a thinner stage due to
more frequent skin screening and increased access to medical
doctors; however, thinner melanomas may additionally be occurring
at an increased rate in the more affluent population that are able
to travel and take holidays abroad. However, holidays with sun
exposure remained significantly associated with Breslow thickness
and ulceration following adjustment for level of education and skin
awareness indicators.
In conclusion, additional efforts are necessary to
improve public and medical education concerning early detection and
prompt surgical treatment, which is known to be the most effective
treatment modality for CM. Men of a lower educational level should
be the focus of future prevention campaigns, and this may be
achieved by promoting more frequent full body skin examinations for
older men. Investigation of the hypothesis of a possible role of
vitamin D in melanoma survival in a clinical trial setting has the
potential to be an interesting and useful future research area
(38,39).
Acknowledgements
The CNMR was supported by grants received from
Bristol Myers Squibb (New York, NY, USA) and GlaxoSmithKline
(Brentford, UK) and the authors would like to thank the Intergruppo
Melanoma Italiano.
References
|
1
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: Estimates of worldwide burden of cancer in
2008: GLOBOCAN 2008. Int J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tryggvadóttir L, Gislum M, Hakulinen T,
Klint A, Engholm G, Storm HH and Bray F: Trends in the survival of
patients diagnosed with malignant melanoma of the skin in the
Nordic countries 1964–2003 followed up to the end of 2006. Acta
Oncol. 49:665–672. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hollestein LM, de Vries E and Nijsten T:
Trends of cutaneous squamous cell carcinoma in the Netherlands:
Increased incidence rates, but stable relative survival and
mortality 1989–2008. Eur J Cancer. 48:2046–2053. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
de Vries E, Bray FI, Coebergh JW and
Parkin DM: Changing epidemiology of malignant cutaneous melanoma in
Europe 1953–1997: Rising trends in incidence and mortality but
recent stabilizations in western Europe and decreases in
Scandinavia. Int J Cancer. 107:119–126. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Garbe C and Leiter U: Melanoma
epidemiology and trends. Clin Dermatol. 27:3–9. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Qin J, Berwick M, Ashbolt R and Dwyer T:
Quantifying the change of melanoma incidence by Breslow thickness.
Biometrics. 58:665–670. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lipsker D, Engel F, Cribier B, Velten M
and Hedelin G: Trends in melanoma epidemiology suggest three
different types of melanoma. Br J Dermatol. 157:338–343. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Erdmann F, Lortet-Tieulent J, Schüz J,
Zeeb H, Greinert R, Breitbart EW and Bray F: International trends
in the incidence of malignant melanoma 1953–2008 - are recent
generations at higher or lower risk? Int J Cancer. 132:385–400.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Coory M, Baade P, Aitken J, Smithers M,
McLeod GR and Ring I: Trends for in situ and invasive
melanoma in Queensland, Australia, 1982–2002. Cancer Causes
Control. 17:21–27. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jemal A, Saraiya M, Patel P, Cherala SS,
Barnholtz-Sloan J, Kim J, Wiggins CL and Wingo PA: Recent trends in
cutaneous melanoma incidence and death rates in the United States,
1992–2006. J Am Acad Dermatol. 65:S17–S25. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
MacKie RM, Bray C, Vestey J, Doherty V,
Evans A, Thomson D and Nicolson M: Scottish Melanoma Group:
Melanoma incidence and mortality in Scotland 1979–2003. Br J
Cancer. 96:1772–1777. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
de Vries E, Schouten LJ, Visser O,
Eggermont AM and Coebergh JW: Working Group of Regional Cancer
Registries: Rising trends in the incidence of and mortality from
cutaneous melanoma in the Netherlands: A Northwest to Southeast
gradient? Eur J Cancer. 39:1439–1446. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Anderson WF, Pfeiffer RM, Tucker MA and
Rosenberg PS: Divergent cancer pathways for early-onset and
late-onset cutaneous malignant melanoma. Cancer. 115:4176–4185.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gandini S, Sera F, Cattaruzza MS, Pasquini
P, Picconi O, Boyle P and Melchi CF: Meta-analysis of risk factors
for cutaneous melanoma: II. Sun exposure. Eur J Cancer. 41:45–60.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
El Ghissassi F, Baan R, Straif K, Grosse
Y, Secretan B, Bouvard V, Benbrahim-Tallaa L, Guha N, Freeman C,
Galichet L and Cogliano V: WHO International Agency for Research on
Cancer Monograph Working Group: A review of human carcinogens -
part D: Radiation. Lancet Oncol. 10:751–752. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zittermann A, Iodice S, Pilz S, Grant WB,
Bagnardi V and Gandini S: Vitamin D deficiency and mortality risk
in the general population: A meta-analysis of prospective cohort
studies. Am J Clin Nutr. 95:91–100. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gandini S, Boniol M, Haukka J, Byrnes G,
Cox B, Sneyd MJ, Mullie P and Autier P: Meta-analysis of
observational studies of serum 25-hydroxyvitamin D levels and
colorectal, breast and prostate cancer and colorectal adenoma. Int
J Cancer. 128:1414–1424. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gandini S, Raimondi S, Gnagnarella P, Doré
JF, Maisonneuve P and Testori A: Vitamin D and skin cancer: A
meta-analysis. Eur J Cancer. 45:634–641. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gnagnarella P, Pasquali E, Serrano D,
Raimondi S, Disalvatore D and Gandini S: Vitamin D receptor
polymorphism FokI and cancer risk: A comprehensive meta-analysis.
Carcinogenesis. 35:1913–1919. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Boniol M, Autier P, Boyle P and Gandini S:
Cutaneous melanoma attributable to sunbed use: Systematic review
and meta-analysis. BMJ. 345:e47572012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Berwick M, Armstrong BK, Ben-Porat L, Fine
J, Kricker A, Eberle C and Barnhill R: Sun exposure and mortality
from melanoma. J Natl Cancer Inst. 97:195–199. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yang L, Lof M, Veierød MB, Sandin S, Adami
HO and Weiderpass E: Ultraviolet exposure and mortality among women
in Sweden. Cancer Epidemiol Biomarkers Prev. 20:683–690. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
US Food and Drug Administration: US Food
and Drug Administration-21 CFR Part 11: Electronic Records;
Electronic Signatures. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=11Accessed.
May 28–2008
|
|
24
|
Fitzpatrick TB: The validity and
practicality of sun-reactive skin types I through VI. Arch
Dermatol. 124:869–871. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gandini S, De Vries E, Tosti G, Botteri E,
Spadola G, Maisonneuve P, Martinoli C, Joosse A, Ferrucci PF,
Baldini F, et al: Sunny holidays before and after melanoma
diagnosis are respectively associated with lower Breslow thickness
and lower relapse rates in Italy. PLoS One. 8:e788202013.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mandalá M, Imberti GL, Piazzalunga D,
Belfiglio M, Lucisano G, Labianca R, Marchesi L, Merelli B, Robone
S, Poletti P, et al: Association of socioeconomic status with
Breslow thickness and disease-free and overall survival in stage
I–II primary cutaneous melanoma. Mayo Clin Proc. 86:113–119. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rosso S, Sera F, Segnan N and Zanetti R:
Sun exposure prior to diagnosis is associated with improved
survival in melanoma patients: Results from a long-term follow-up
study of Italian patients. Eur J Cancer. 44:1275–1281. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Berwick M, Reiner AS, Paine S, Armstrong
BK, Kricker A, Goumas C, Cust AE, Thomas NE, Groben PA, From L, et
al: Sun exposure and melanoma survival: A GEM study. Cancer
Epidemiol Biomarkers Prev. 23:2145–2152. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Egan KM, Sosman JA and Blot WJ: Sunlight
and reduced risk of cancer: Is the real story vitamin D? J Natl
Cancer Inst. 97:161–163. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Autier P and Gandini S: Vitamin D
supplementation and total mortality: A meta-analysis of randomized
controlled trials. Arch Intern Med. 167:1730–1737. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Randerson-Moor JA, Taylor JC, Elliott F,
Chang YM, Beswick S, Kukalizch K, Affleck P, Leake S, Haynes S,
Karpavicius B, et al: Vitamin D receptor gene polymorphisms, serum
25-hydroxyvitamin D levels, and melanoma: UK case-control
comparisons and a meta-analysis of published VDR data. Eur J
Cancer. 45:3271–3281. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Newton-Bishop J, Beswick S, Jackon S, Moor
Renderson J, Elliott F, Barrett J, Affleck P, Marsden J and Bishop
T: Vitamin D and survival from melanoma. Melanoma Res. 16:S26–S27.
2006. View Article : Google Scholar
|
|
33
|
Raimondi S, Johansson H, Maisonneuve P and
Gandini S: Review and meta-analysis on vitamin D receptor
polymorphisms and cancer risk. Carcinogenesis. 30:1170–1180. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Newton-Bishop JA, Beswick S,
Randerson-Moor J, Chang YM, Affleck P, Elliott F, Chan M, Leake S,
Karpavicius B, Haynes S, et al: Serum 25-hydroxyvitamin D3 levels
are associated with breslow thickness at presentation and survival
from melanoma. J Clin Oncol. 27:5439–5444. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Gilchrest BA, Eller MS, Geller AC and Yaar
M: The pathogenesis of melanoma induced by ultraviolet radiation. N
Engl J Med. 340:1341–1348. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Berwick M, Armstrong BK, Ben-Porat L, Fine
J, Kricker A, Eberle C and Barnhill R: Sun exposure and mortality
from melanoma. J Natl Cancer Inst. 97:195–199. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ambrosini-Spaltro A, Dal Cappello T,
Deluca J, Carriere C, Mazzoleni G and Eisendle K: Melanoma
incidence and Breslow tumour thickness development in the central
Alpine region of South Tyrol from 1998 to 2012: A population-based
study. J Eur Acad Dermatol Venereol. 29:243–248. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Guerrieri-Gonzaga A and Gandini S: Vitamin
D and overall mortality. Pigment Cell Melanoma Res. 26:16–28. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Gandini S, Francesco F, Johanson H,
Bonanni B and Testori A: Why vitamin D for cancer patients?
Ecancermedicalscience. 3:1602009.PubMed/NCBI
|