Introduction
Prostate cancer (PCA) is one of the most common
forms of malignancy in men >50 years of age, and there are
>200,000 newly diagnosed cases worldwide per year (1). Several clinicopathological variables,
including prostate-specific antigen (PSA) level, Gleason score (GS)
and clinical stage of PCA have contributed to treatment
decision-making prior to the administration of an intervention.
However, prescribing an appropriate treatment for men with newly
diagnosed PCA remains controversial, since there are no precise
molecular biomarkers that are associated with the biological
characteristics of the tumors (2).
The identification of a biomarker that may be used in clinical
practice is therefore required to provide accurate prognostic
information.
Ribosomal L1 domain containing 1 (RSL1D1; gene no.,
26156), also termed PBK1, L12 and CSIG, is a nucleolar protein that
belongs to the L1p/L10e family, and contains a ribosomal L1 domain
in the N-terminus and a lysine-rich domain in the C-terminus
(3). RSL1D1 has been demonstrated to
delay cellular senescence through the inhibition of the translation
of phosphatase and tensin homolog protein (3). In addition, it is a novel proapoptotic
regulator that is activated in response to DNA damage (4). One of the most significant risk factors
associated with PCA is aging, a process which represents an
attenuation of antitumorigenic signals (5), such as those in cellular aging (6–9). It is
currently widely accepted that cellular aging is critical in tumor
suppression and has been associated with the presence of benign
prostate lesions (10–12). However, to the best of our knowledge,
there are no studies concerning RSL1D1 expression in prostatic
tumor tissues and its association with the clinicopathological
features of patients with PCA. Therefore, the current study
investigated whether prostate tumors may be distinguished from
benign prostatic hyperplasia (BPH) using cellular processes
associated with aging and senescence, and whether RSL1D1 may be
used as a novel biomarker for the diagnosis or risk stratification
of patients with PCA.
Materials and methods
Patient characteristics and tissue
samples
For the present study, tumor samples were obtained
from 138 patients with prostatic adenocarcinoma, who underwent a
radical prostatectomy at the Guangxi Medical University (Nanning,
China) between October 2004 and July 2008. No patients received
adjuvant androgen deprivation therapy prior to surgery. In addition
to the PCA samples, the present study obtained 50 corresponding
tissue samples, via transurethral resection performed at the same
hospital, from patients with BPH to serve as controls. The mean age
of the patients with PCA at the time of diagnosis was 68.3 years
(range, 51–85 years), and the mean pre-operative PSA level was
18.92 ng/ml (range, 2.14–121.50 ng/ml). The mean age of the 50
patients diagnosed with BPH was 68.8 years, (range, 52–89 years)
and the mean PSA was 6.05 ng/ml (range, 0.3–14.4 ng/ml). All
patients with PCA were followed-up after radical surgery.
Biochemical recurrence (BCR) was defined as PSA levels >0.2
ng/ml occurring two or more times.
The use of tissues was approved by the Institutional
Review Board of the Guangxi Medical University and written informed
consent was obtained from all patients.
Histological staining and
immunohistochemical analysis
Paraffin-embedded, 4-mm thick tissue sections from
all the obtained samples were stained with hematoxylin and eosin
for histological analysis. RSL1D1 was detected using a goat
anti-human RSL1D1 polyclonal antibody (catalog no., BS-0793R;
dilution, 1:200; Bioss Inc., Woburn, MA, USA). The antibody was
diluted according to the manufacturer's recommendations.
All the tissue sections were de-waxed, rehydrated
and incubated in 3% hydrogen peroxide for 10 min at room
temperature to halt endogenous peroxidase activity, prior to
subsequent incubation overnight with the RSL1D1 antibody at 4°C in
phosphate-buffered saline (PBS; ZSGB-BIO, Beijing, China)
containing 1% bovine serum albumin (ZSGB-BIO). RSL1D1 staining was
detected using an EnVision kit (EnVision™+HRP; Dako, Glostrup,
Denmark). The nuclei were counterstained with
4′,6′-diamidino-2-phenylindole dilactate (ZSGB-BIO), and 0.3%
hydrogen peroxide (ZSGB-BIO) in PBS was used as the chromogen.
Following staining, the tissue sections were counterstained using
hematoxylin (ZSGB-BIO), and subsequently dehydrated using ethanol
and xylene. Permount (ZSGB-BIO) was then applied to the coverslips.
Rat anti-human polyclonal immunoglobulin G (catalog no., CB3560554;
dilution, 1:200; Biomeda Corporation, Foster City, CA, USA) was
used as the primary antibody in the negative controls.
Histological analysis was performed by two
pathologists (Department of Urology, Sixth Affiliated Hospital of
Sun Yat-sen University; Department of Nuclear Medicine, Third
Affiliated Hospital of Sun Yat-sen University, Guangzhou, China)
who were blinded to the clinical information of the patients. The
staining intensity of the cells for RSL1D1 was graded according to
the percentage of cells that expressed RSL1D1, as follows: 0,
<10% of cells; grade I, 10–25% of cells; grade II, 26–50% of
cells; grade III, 51–75% of cells; and grade IV, ≥76% of cells.
Strong staining (grade III and IV) of RSL1D1 was considered as the
high expression group, whereas light staining (grade I and II) was
considered as the low expression group. Overexpression of RSL1D1
was determined as any expression in the PCA samples compared with
the BPH samples. Morphological diagnoses were conducted according
to the International Union Against Cancer 2009 staging
classification guidelines for PCA (13), and histological analyses were
performed according to the 2010 Gleason grading system (14).
Statistical analysis
The association between the expression of RSL1D1 and
the clinicopathological variables of the patients was analyzed
using Fisher's exact or the χ2 test. Variables affecting
the BCR of the patients were analyzed using logistic regression.
SPSS version 13.0 software (SPSS, Chicago, IL, USA) was used for
analysis. Two-tailed P<0.05 was considered to indicate a
statistically significant difference.
Results
RSL1D1 expression in PCA and BPH
tissue samples
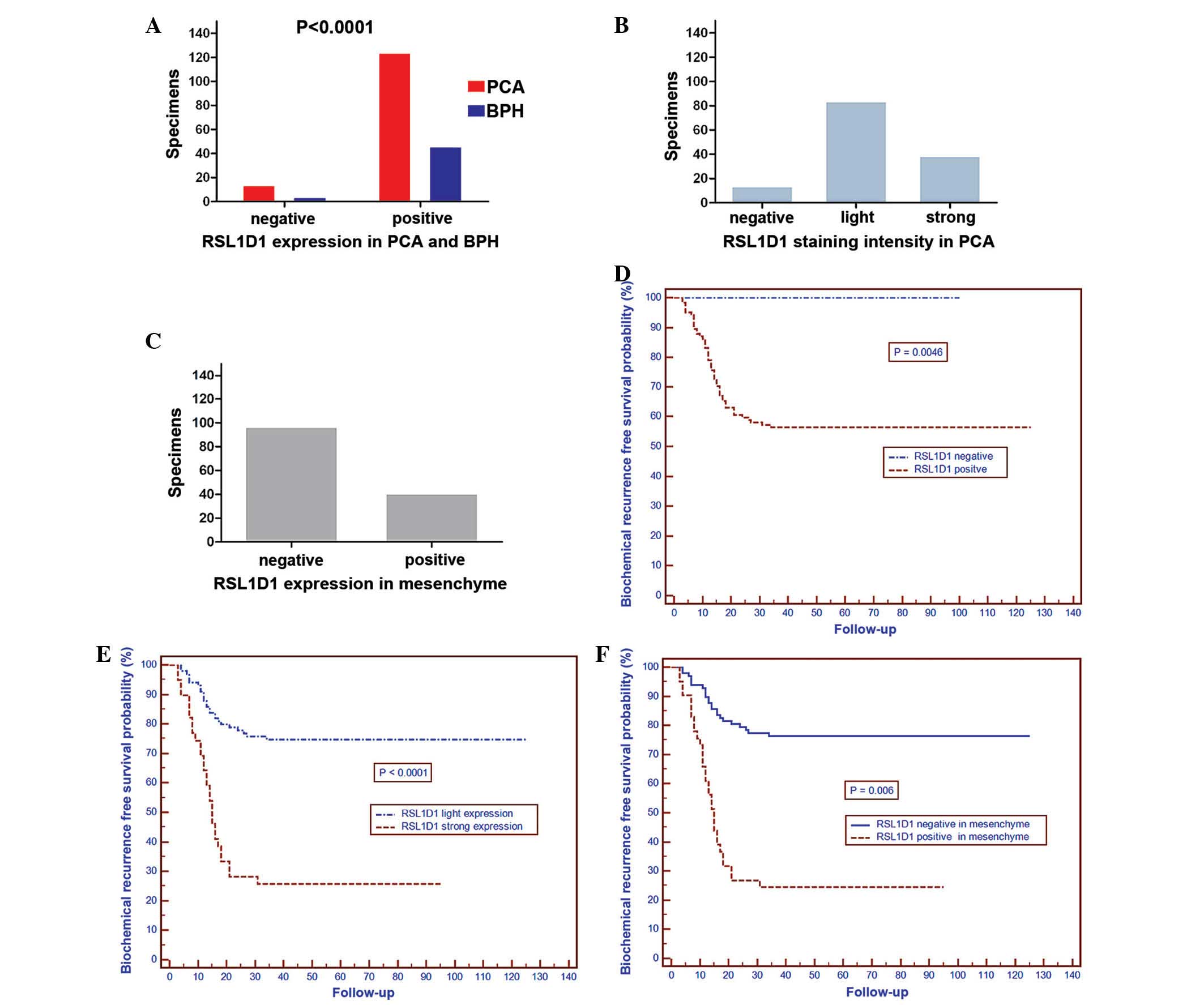
Immunohistochemical analysis demonstrated that
RSL1D1 expression was localized to the nucleoli, with low to high
expression in PCA cells. There was also expression in the
mesenchyme of PCA cells (Fig. 1A–G).
Positive expression of RSL1D1 was observed in 124 out of 138
(89.9%) patients with PCA and 4 out of 50 (8.0%) patients with BPH.
Of these 124 patients, 18 patients (13.0% of total) exhibited grade
I staining, 67 patients (48.6%) grade II staining, 25 patients
(18.1%) grade III staining and 14 patients (10.1%) grade IV
staining. Furthermore, RSL1D1 expression was more likely to be
observed in the mesenchyme of PCA cells (41 out of 138 patients;
29.7%) (Fig. 2A–C).
Association between RSL1D1
overexpression and clinicopathological variables of patients with
PCA
The present study observed that the overexpression
rate of RSL1D1 was significantly associated with the pathological
GS of the patients with PCA (<7 vs. >7; 80.3 vs. 100%;
P<0.0001). Similarly, the pathological stage of the cancer was
associated with the overexpression rate of RSL1D1 [organ-confined
(≤pT2c) vs. extraprostatic (≥pT3a); 85.7 vs. 97.8%; P=0.028]. There
was no significant association identified between age (P=0.604),
PSA level (P=0.166) and lymph node status (P=0.126) of patients
with the overexpression rate of RSL1D1. A high expression rate of
RSL1D1 was significantly associated with the GS of patients with
PCA (>7 vs. <7; 44.8 vs. 12.7%; P<0.0001). There was a
significant association between a strong expression rate of RSL1D1
and the pathological stage of the patients with PCA (≤pT2c vs.
≥pT3a; 21.9 vs. 45.7%; P=0.001). However, there was no significant
association with the PSA level (<20 vs. ≥20 ng/ml; 26.0 vs.
33.3%; P=0.381), the age of the patients (≥70 and <70 years;
31.7 vs. 25.6%, P=0.436) or the presence of lymph node metastasis
(yes vs. no; 39.1 vs. 26.1%; P=0.31) (Table I).
 | Table I.Association between
clinicopathological variables and expression of RSL1D1 in 138
patients with prostate cancer. |
Table I.
Association between
clinicopathological variables and expression of RSL1D1 in 138
patients with prostate cancer.
| Variables | Total, n | RSL1D1+
overexpression, n (%) | P-value | RSL1D1 strong
expression, n (%) | P-value |
|---|
| Age, years |
|
|
0.6040 |
| 0.4360 |
|
<70 | 78 | 71 (91.0) |
| 20 (25.6) |
|
| ≥70 | 60 | 53 (88.3) |
| 19 (31.7) |
|
| PSA, ng/ml |
|
|
0.1660 |
| 0.3810 |
|
<20 | 96 | 84 (87.5) |
| 25 (26.0) |
|
| ≥20 | 42 | 40 (95.2) |
| 14 (33.3) |
|
| Pathological
stage |
|
|
0.0280 |
| 0.0010 |
| T2c | 92 | 79 (85.7) |
| 18 (19.6) |
|
| ≥T3a | 46 | 45 (97.8) |
| 21 (45.7) |
|
| Post-operative
GS |
|
| <0.0001 |
| <0.0001 |
|
<7 | 71 | 57 (80.3) |
| 9
(12.7) |
|
| ≥7 | 67 | 67
(100.0) |
| 30
(44.8) |
|
| LN metastasis |
|
|
0.1260 |
| 0.3100 |
| No | 115 | 101 (87.8) |
| 30 (26.1) |
|
| Yes | 23 | 23
(100.0) |
| 9
(39.1) |
|
Association between RSL1D1 expression
and BCR
Cox analysis was performed to analyze whether RSL1D1
expression was significantly associated with the BCR of the
patients. The results are shown in Table
II. A GS of ≥7, PSA ≥20 ng/ml, RSL1D1 strong expression,
extraprostatic cases (≥pT3a cancer stage), lymph node metastasis
and RSL1D1-positive staining in the mesenchyme were significant
predictors of BCR using Cox univariate analysis, whereas
multivariate analysis demonstrated that GS and a strong expression
of RSL1D1 were significant predictors of BCR.
 | Table II.Prognostic factors for biochemical
recurrence of 138 patients with prostate cancer using Cox
regression analysis. |
Table II.
Prognostic factors for biochemical
recurrence of 138 patients with prostate cancer using Cox
regression analysis.
| Variables | HR | 95% CI | P-value |
|---|
| Univariate
analysis |
|
|
|
| Age,
years (<70 vs. ≥70) |
1.059 | 0.621–1.807 | 0.833 |
| PSA,
ng/ml (<20 vs. ≥20) |
5.276 | 3.041–9.155 | <0.0001 |
|
Pathological GS (<7 vs.
≥7) | 30.922 |
9.659–98.998 | <0.0001 |
|
Pathological stage (OC vs.
EPE) | 11.403 |
6.040–21.527 | <0.0001 |
| Lymph
node status (neg vs. pos) |
7.000 |
4.018–12.197 | <0.0001 |
| RSL1D1
expression (neg vs. pos) | – | – | – |
| RSL1D1
staining (light vs. strong) |
4.405 | 2.570–7.549 | <0.0001 |
| RSL1D1 in
mesenchyme (neg vs. pos) |
2.079 | 1.215–3.559 | 0.008 |
| Multivariate
analysis |
|
|
| Age,
years (<70 vs. ≥70) |
1.116 | 0.639–1.948 | 0.700 |
| PSA,
ng/ml (<20 vs. ≥20) |
1.895 | 0.950–3.780 | 0.069 |
|
Pathological GS (<7 vs.
≥7) | 11.498 |
3.155–41.910 | 0.0001 |
|
Pathological stage (OC vs.
EPE) |
1.885 | 0.798–4.452 | 0.148 |
| Lymph
node status (neg vs. pos) |
1.157 | 0.536–2.498 | 0.711 |
| RSL1D1
expression (neg vs. pos) | – | – | – |
| RSL1D1
staining (light vs. strong) |
1.915 | 1.094–3.350 | 0.023 |
| RSL1D1
in mesenchyme (neg vs. pos) |
1.193 | 0.585–2.433 | 0.628 |
The mean follow-up time of the patients was 87
months (range, 61–136 months). Of the 138 cases analyzed
immunohistochemically, 54 patients had BCR with PSA levels of ≥0.2
ng/ml ≥3 times, and 23 patients succumbed to the disease. The
present results demonstrated that 5-year BCR-free survival rate was
increased in patients that did not express RSL1D1 compared with
patients that did express RSL1D1 (P=0.0046; Fig. 2D), in patients with light RSL1D1
expression compared with patients with strong expression
(P<0.0001; Fig. 2E) and in
patients that did not have mesenchymal RSL1D1 staining compared
with patients that did have mesenchymal RSL1D1 staining (P=0.006;
Fig. 2F).
Discussion
The identification of a novel biomarker is required
for PCA, since it may be used by physicians and surgeons to
identify patients who require radical surgery or active
surveillance. Furthermore, a biomarker leads to improved screening,
diagnosis and clinical outcome prediction prior to surgery
(15). As a consequence of the high
global incidence of PCA, the demand for the identification of
dependable biomarkers is strong. PSA remains the most widely used
biomarker for PCA diagnosis and screening; however, it has a number
of limitations, including false-positive diagnoses and may lead to
excessive treatment, due to its poor sensitivity and specificity
(16–18).
The present study analyzed the association between
RSL1D1 protein expression and the pre-operative clinicopathological
characteristics of patients with PCA. It was observed that the
levels of RSL1D1 protein were significantly increased in PCA
tissues compared with the expression levels in the tissues of
patients with BPH. In addition, the expression of the RSL1D1
protein was observed to be significantly associated with the
pathological stage and increased GS of patients with PCA. In
survival analysis, the BCR-free survival rate of PCA patients with
high RSL1D1 protein expression was significantly decreased compared
with patients with low RSL1D1 expression. Similarly, this result
was also observed in patients that expressed RSL1D1 and in those
that expressed RSL1D1 in the mesenchyme compared with patients with
no expression and no mesenchymal expression, respectively.
Univariate analyses also demonstrated that high RSL1D1 protein
expression in patients with PCA was significantly associated with
the BCR-free survival rate. Furthermore, multivariate analysis
showed that a high expression level of RSL1D1 protein is an
independent risk factor in the prognosis of patients with PCA.
These results indicate that the detection of increased RSL1D1
protein may aid in identifying patients with an aggressive PCA
phenotype and a poor prognosis. Therefore, RSL1D1 may be a
promising prognostic marker for patients with PCA, although the
precise molecular mechanisms behind the high expression of RSL1D1
in patients with PCA remains unknown.
In addition, the present study demonstrated that a
GS of ≥7 was an independent predictor for the BCR of patients. It
is widely accepted that the GS of patients is one of the most
critical predictors of PCA progression and survival regardless of
the therapy used, and it is also one of the most influential
factors used to determine treatment for PCA (19). An increased GS was associated with
recurrence and metastasis in a previous study that consisted of 450
patients with PCA with ≥8 years follow-up (20). In the study, the lowest risk of BCR
and metastases at 10 years was found in patients with a GS of ≤7.
In addition, another study demonstrated that the GS may be used to
assess the risk of progression post-operatively in patients
primarily treated with radiotherapy that subsequently develop local
recurrence (21). In that study, the
patients that had the most favorable outcome had a GS of ≤7 and PSA
levels of <4 ng/ml. These findings were also confirmed by other
studies, which demonstrated that patients with a GS of ≥7 and a
higher GS of the tumor were more likely to have BCR compared with
patients with a lower GS (22–24).
RSL1D1 can be identified using a yeast two-hybrid
screen and is a cellular aging regulatory gene, whose expression is
associated with senescence; however, its role in malignant tumors
remains unknown (25). The present
pilot study has demonstrated that there was a significant
association between RSL1D1 protein overexpression and patients with
PCA, suggesting that it may be used as a novel biomarker for the
diagnosis and risk stratification of patients with PCA. The present
pilot study has certain limitations, including the small sample
size; therefore, additional studies to investigate the molecular
mechanisms of RSL1D1 expression in the tumorigenesis or progression
of PCA are essential.
In summary, the present results demonstrated that
RSL1D1 protein overexpression is an independent prognostic factor
for 5-year BCR-free survival and suggest that the RSL1D1 protein
may be a novel biomarker for the risk stratification and prognosis
of patients with PCA.
Acknowledgements
The authors would like to thank everyone from the
Department of Pathology at Guangxi Medical University.
References
|
1
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gleason DF: Histologic grading of prostate
cancer: A perspective. Hum Pathol. 23:273–279. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ma L, Chang N, Guo S, Li Q, Zhang Z, Wang
W and Tong T: CSIG inhibits PTEN translation in replicative
senescence. Mol Cell Biol. 28:6290–6301. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Li N, Zhao G, Chen T, Xue L, Ma L, Niu J
and Tong T: Nucleolar protein CSIG is required for p33ING1 function
in UV-induced apoptosis. Cell Death Dis. 3:e2832012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shen MM and Abate-Shen C: Molecular
genetics of prostate cancer: New prospects for old challenges.
Genes Dev. 24:1967–2000. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Narita M and Lowe SW: Senescence comes of
age. Nat Med. 11:920–922. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Campisi J: Senescent cells, tumor
suppression, and organismal aging: Good citizens, bad neighbors.
Cell. 120:513–522. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Campisi J: Aging, tumor suppression and
cancer: High wire-act! Mech Ageing Dev. 126:51–58. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Collado M, Blasco MA and Serrano M:
Cellular senescence in cancer and aging. Cell. 130:223–233. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Choi J, Shendrik I, Peacocke M, Peehl D,
Buttyan R, Ikeguchi EF, Katz AE and Benson MC: Expression of
senescence-associated beta-galactosidase in enlarged prostates from
men with benign prostatic hyperplasia. Urology. 56:160–166. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Castro P, Giri D, Lamb D and Ittmann M:
Cellular senescence in the pathogenesis of benign prostatic
hyperplasia. Prostate. 55:30–38. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen Z, Trotman LC, Shaffer D, Lin HK,
Dotan ZA, Niki M, Koutcher JA, Scher HI, Ludwig T, Gerald W, et al:
Crucial role of p53-dependent cellular senescence in suppression of
Pten-deficient tumorigenesis. Nature. 436:725–730. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sobin LH, Gospodarowicz MK and Wittekind
C: TNM Classification of Malignant Tumors (UICC). 1:(7th).
Wiley-Blackwell. Hoboken, NY: 2009.
|
|
14
|
Epstein JI: An update of the Gleason
grading system. J Urol. 183:433–440. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Prensner JR, Rubin MA, Wei JT and
Chinnaiyan AM: Beyond PSA: The next generation of prostate cancer
biomarkers. Sci Transl Med. 4:127rv32012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lilja H, Ulmert D and Vickers AJ:
Prostate-specific antigen and prostate cancer: Prediction,
detection and monitoring. Nat Rev Cancer. 8:268–278. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wolf AM, Wender RC, Etzioni RB, Thompson
IM, D'Amico AV, Volk RJ, Brooks DD, Dash C, Guessous I, Andrews K,
et al: American Cancer Society Prostate Cancer Advisory Committee:
American cancer society guideline for the early detection of
prostate cancer: Update 2010. CA Cancer J Clin. 60:70–98. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Balk SP, Ko YJ and Bubley GJ: Biology of
prostate-specific antigen. J Clin Oncol. 21:383–391. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gleason DF and Mellinger GT: Veterans
Administration Cooperative Urological Research Group: 1974. J Urol.
167:953–958. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Antonarakis ES, Feng Z, Trock BJ,
Humphreys EB, Carducci MA, Partin AW, Walsh PC and Eisenberger MA:
The natural history of metastatic progression in men with
prostate-specific antigen recurrence after radical prostatectomy:
Long-term follow-up. BJU Int. 109:32–39. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chade DC, Shariat SF, Cronin AM, Savage
CJ, Karnes RJ, Blute ML, Briganti A, Montorsi F, van der Poel HG,
Van Poppel H, et al: Salvage radical prostatectomy for
radiation-recurrent prostate cancer: A multi-institutional
collaboration. Eur Urol. 60:205–210. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Han M, Partin AW, Zahurak M, Piantadosi S,
Epstein JI and Walsh PC: Biochemical (prostate specific antigen)
recurrence probability following radical prostatectomy for
clinically localized prostate cancer. J Urol. 169:517–523. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Miyake M, Tanaka N, Asakawa I, Morizawa Y,
Anai S, Torimoto K, Aoki K, Yoneda T, Hasegawa M, Konishi N and
Fujimoto K: Proposed salvage treatment strategy for biochemical
failure after radical prostatectomy in patients with prostate
cancer: A retrospective study. Radiat Oncol. 9:2082014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cao D, Kibel AS, Gao F, Tao Y and Humphrey
PA: The Gleason score of tumor at the margin in radical
prostatectomy is predictive of biochemical recurrence. Am J Surg
Pathol. 34:994–1001. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Meng L, Yasumoto H and Tsai RY: Multiple
controls regulate nucleostemin partitioning between nucleolus and
nucleoplasm. J Cell Sci. 119:5124–5136. 2006. View Article : Google Scholar : PubMed/NCBI
|