Introduction
Breast cancer is the most common type of cancer
among females, with an estimated annual incidence of 1.6 million
cases, worldwide (1). The majority of
breast cancer patients are diagnosed during the early stages,
during which treatment is generally effective, with a 5-year
survival rate of almost 90%. However, breast cancer also has a high
recurrence rate, with up to 40% of patients eventually progressing
to metastatic breast cancer. Compared to early stage breast cancer,
metastatic breast cancer is associated with a much more negative
prognosis, with a 5-year survival rate of only 25% (2).
Secondary breast carcinomas are extremely rare. The
first case of metastasis to the breast was reported in an autopsy
study in 1957 (3). Alva and
Shetty-Alva (4) reported that
metastases to the breast have been identified at rates of 1.7–6.6%
based on autopsy studies of patients with any type of cancer,
1.2–2% in clinical case reports and 2.7% in cytological
reviews.
Commonly, metastatic breast cancer is an incurable
disease, and treatment aims to prolong survival and to improve or
maintain quality of life by palliating disease-associated symptoms
while minimizing the toxicity of treatment. The median survival
time of metastatic breast cancer patients is ~2 years (5). Patients with hormone-insensitive disease
and patients that do not respond to endocrine therapy are
candidates for chemotherapy (6).
Combination chemotherapy provides higher response rates and
increased time to progression. Newer taxane-containing combination
regimens, including docetaxel/capecitabine and
paclitaxel/gemcitabine, have been demonstrated to improve overall
survival compared with single-agent taxanes, and these regimens are
commonly used when a combination therapy is adopted. However, the
optimal duration of treatment to control disease with these
regimens remains to be elucidated. In a previous meta-analysis,
Gennari et al (6) reported
that increased first-line chemotherapy duration was associated with
prolonged progression-free survival and marginally longer overall
survival. Continuing chemotherapy until disease progression ceases
is additionally reported to improve quality of life measures.
Capecitabine is an oral fluoropyrimidine and has been demonstrated
to have marked activity in metastatic breast cancer (7).
Longer survival of patients with metastatic breast
cancer and the use of improved imaging techniques are associated
with an increased incidence of brain metastases. Patients who
develop brain metastases tend to have poor prognosis, with short
overall survival times. In addition, brain metastases are a
significant cause of morbidity, associated with progressive
neurological deficits that result in a reduced quality of life.
Current therapies include surgery, whole-brain radiation therapy,
stereotactic radiosurgery, chemotherapy and targeted therapies.
However, the timing and appropriate use of these therapies is
controversial and careful patient selection by using available
prognostic tools is extremely important (8).
In the current study, a retrospective analysis that
assessed cases of metastases to the breast from a gastric
carcinoma, diagnosed between January 2007 and April 2013, was
performed, and two patients were identified. The clinical and
pathological features of the aforementioned metastasis are
presented herein, in order to gain insight into the clinical
presentation and natural history of this disease. Consent for the
publication of patient data was obtained from the next of kin.
Case report
Case one
In January 2007, a 37-year-old woman presented to
the First Affiliated Hospital of Nanchang University (Nanchang,
Jiangxi, China) with upper abdominal pain that had lasted for 2
months. Computed tomography indicated a diagnosis of signet ring
cell carcinoma, and the patient underwent a radical gastrectomy.
The subsequent pathological examination revealed a level II gastric
adenocarcinoma with an ulcerative signet ring cell histology.
Metastasis was identified in 2/8 lymph nodes along the lesser
curvature of the stomach. Subsequent to surgery, the patient
received two 3-week cycles of chemotherapy with paclitaxel (210 mg,
day 1 of each cycle) and cisplatin (30 mg, days 1–3 of each
cycle).
In October 2009, a radical colectomy was performed
on the right half of the colon due to the presence of colonic
metastasis, and was followed by 1 cycle (3 weeks) of chemotherapy
with oxaliplatin (200 mg, day 1 of each cycle), calcium folinate
(0.6 g/day, day 1 of the cycle) and 5-fluorouracil (3.75 g/day, 46
h intravenous administration, day 1 of the cycle). In June 2011,
four years since the gastrectomy was performed, the patient
presented to the same hospital with a 9×5 cm left upper outer
quadrant and a 3×2 cm left lower outer quadrant breast mass. The
masses were movable, smooth with irregular margins and exhibited
slight tenderness. Two asymptomatic left axillary lymph nodes were
palpable. A mammography examination revealed dense left breast
glands with malignant changes and hyperplasia, and the breast
ultrasound demonstrated hypoechoic lesions in the left breast and
the two axillas. The right breast appeared normal.
A breast biopsy indicated the presence of a signet
ring cell carcinoma, and a modified radical mastectomy was
performed. A hard, gray mass, measuring 10×7×4 cm, had replaced the
majority of the breast tissue and invaded the nipple. The
postoperative pathological diagnosis was signet ring cell carcinoma
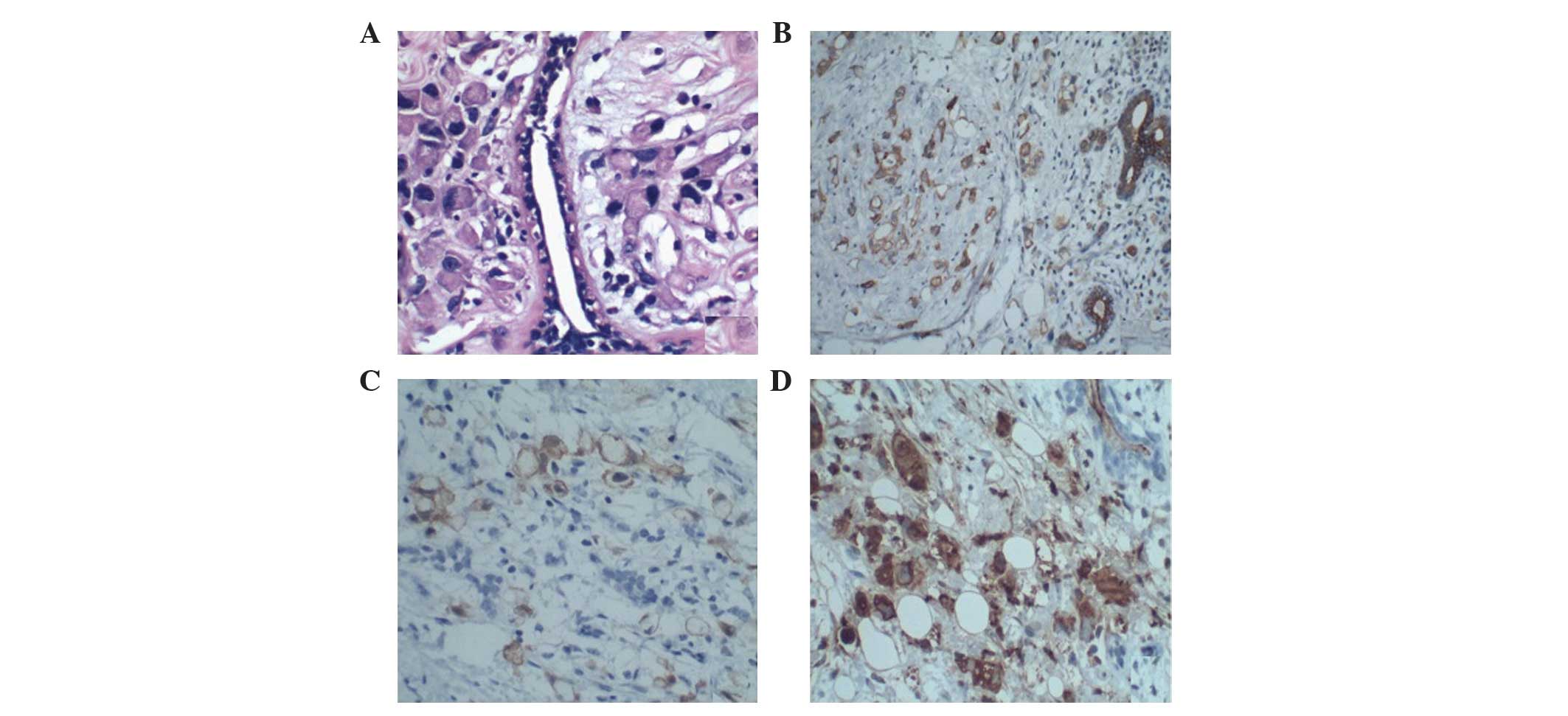
(Fig. 1A). An intravascular tumor
thrombus was present, and metastasis was identified in 17/21 of the
axillary lymph nodes. Immunohistochemical staining of the tumor
revealed the following: Cytokeratin (CK) 7(2+) (Fig. 1B), CK20(−), villin(2+) (Fig. 1C), carcinoembryonic antigen (CEA)(3+)
(Fig. 1D), caudal type homeobox 2(−),
estrogen receptor (ER)(−), progesterone receptor (PR)(−) and
receptor tyrosine-protein kinase Erb-B2 (HER2)(−). The patient
refused postoperative treatment and succumbed to the disease 18
months later, in December 2012.
Case two
In February 2013, a 31-year-old woman presented to
the First Affiliated Hospital of Nanchang University with a 6.5×6.4
cm mass in the right breast, and an ultrasound confirmed a
hypoechoic mass. The mammography revealed retraction of the right
nipple and dense glands. A biopsy of the breast revealed an
invasive carcinoma.
A modified radical mastectomy of the right breast
was performed. A subsequent pathological examination revealed a
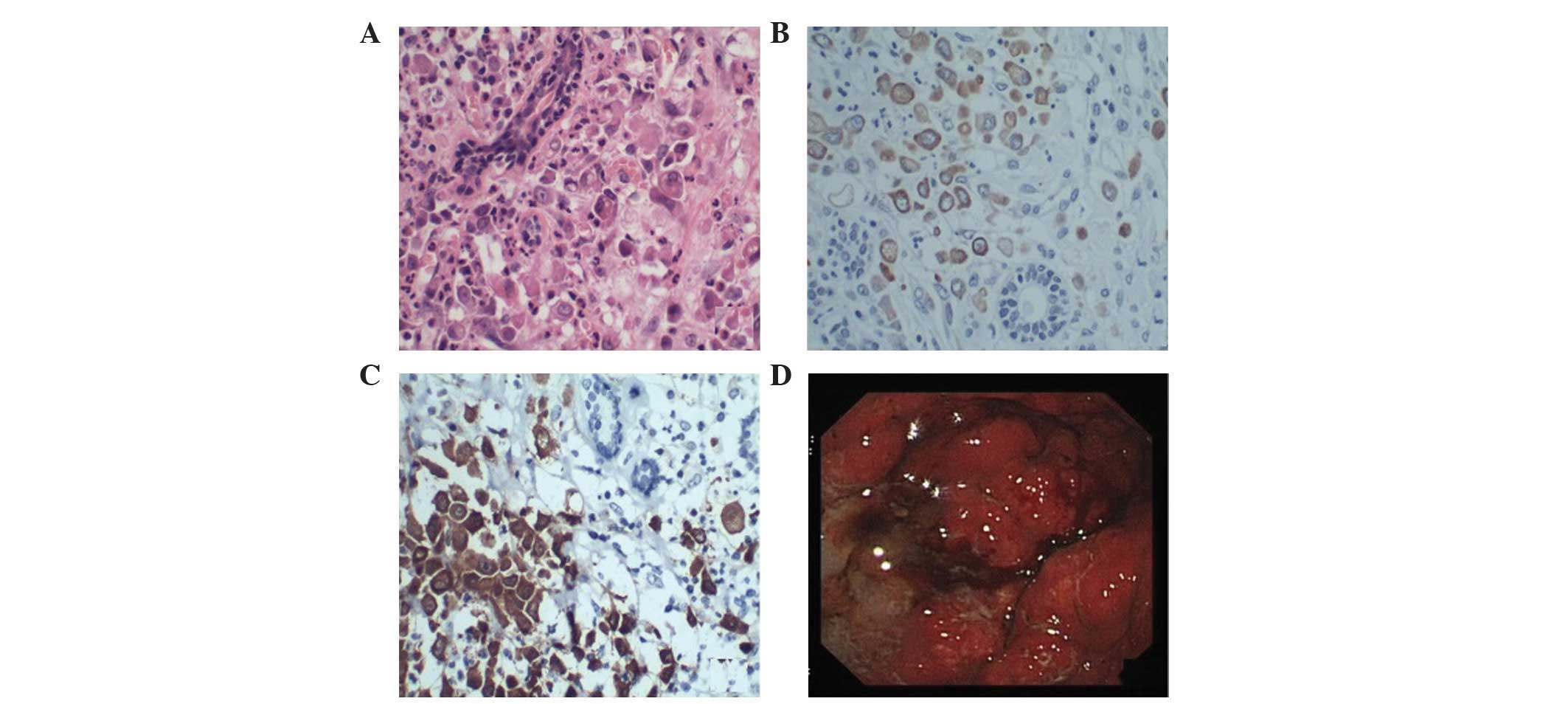
metastatic signet ring cell carcinoma (Fig. 2A), and metastasis was identified in
7/15 of the axillary lymph nodes. Immunohistochemical evaluation of
the tumor yielded the following staining results: CK7(−), CK20(3+)
(Fig. 2B), villin(3+) (Fig. 2C), S100(−), Vim(−), ER(−), PR(−),
c-Erb-B2(−), Ki-67 (80%, +), P53(−), CD34(−) and E-cadherin(2+). An
abdominal computed tomography scan was performed, the results of
which revealed a diffuse gastric wall thickening, consistent with
gastric cancer. A gastroscopy revealed the presence of linitis
plastica (Fig. 2D) and a biopsy
indicated the presence of signet ring cell carcinoma. The patient
was diagnosed with stage IV gastric cancer, and 2 cycles of
chemotherapy with paclitaxel (270 mg, day 1) and cisplatin (40 mg,
days 1–3) were administered. The patient succumbed to the disease
in November 2013.
Discussion
The most common metastatic tumor to the breast is
malignant melanoma, followed by lymphoma, neuroendocrine tumor,
thyroid, lung, cervical, ovarian, renal and liver cancers, sarcoma
and nasopharyngeal carcinoma (9).
Gastric carcinomas metastasizing to the breast are less common; to
the best of our knowledge, only 25 cases had been reported in the
English literature prior to 2006 (10). Gastric cancer tends to metastasize to
hormone-dependent organs, which is likely to be due to the rich
blood supply available to these organs. Premenopausal women are
most commonly affected by the disease, and a previously reported
average age at presentation is 47 years (11). The patients in the current study were
younger compared with this figure, with an average age of 34
years.
Gastric carcinoma metastases to the breast are
typically signet ring carcinomas, and must be differentiated from
primary breast signet ring carcinomas, which were first described
as a subtype of lobular tumors by Steinbreche and Silverberg in
1976 (12). Primary breast signet
ring cell carcinomas account for 2.0–4.5% of all breast tumors, are
more aggressive compared with other breast tumors and frequently
metastasize to the abdomen and gastrointestinal tract (12). Approximately two thirds of secondary
tumors present as a single painless mass in the upper outer
quadrant of the breast. Nipple discharge is rarer than that
observed in primary breast cancer. The disease is similar to
inflammatory breast cancer, and edema of the skin is evident.
In previous studies, ~25% of patients with breast
metastases possessed bilateral breast tumors and 5% were found to
have axillary lymph node metastases (10,11). By
contrast, the patients in the present study had solitary left and
right breast masses, respectively, with no pain, and axillary lymph
node metastases were confirmed. Toombs and Kalisher (13) reported that 66% of solitary metastases
to the breast were located in the upper outer quadrant. In a
retrospective study of 2,414 cases of primary breast cancer,
approximately two thirds of the tumors were located in the outer
quadrants, and one third were located in the inner quadrants. The
position of the breast mass was not found to be useful for the
differentiation between primary and secondary breast cancer
(14).
Immunohistochemistry is useful for the
differentiation of primary or metastatic breast signet ring cell
carcinomas. Primary breast signet ring cell carcinomas occur most
frequently in premenopausal women and have high expression levels
of ER, PR and gross cystic disease fluid protein (15). The pathological features of metastatic
carcinomas to the breast include the replacement of normal breast
tissue by malignancy and the invasion of the adjacent normal
tissue. Lobular carcinomas in situ and intraductal tumors
are not observed in metastatic disease (10). Metastatic tumors are generally similar
to their primary tumors based on immunohistochemistry, which may be
useful in discerning whether breast tumors are primary or
metastatic. Villin, for example, is a gastrointestinal cytoskeletal
protein present in brush border microvilli that is not present in
breast tissue. In addition, metastases from adenocarcinoma of the
stomach express the skin markers CEA, CK7 and CK20, while ER and PR
are not expressed (15). HER2 is
expressed in 20% of gastric cancers and is not specific to breast
cancer (16).
Microcalcifications within breast metastases are not
commonly observed on axial imaging. Only a few cases of
microcalcifications associated with breast metastases from gastric
cancer have been reported in the literature (17). In 2012, Luk et al (18) described the case of a patient who
presented with a breast mass that contained microcalcifications,
which was later confirmed to be metastasized from a gastric
carcinoma.
A breast lumpectomy is currently the recommended
treatment. Furthermore, previous evidence has indicated that
radiotherapy may not be effective in the treatment of breast
metastases (11). The systemic
treatment of the primary cancer is necessary, and a resection of
the primary tumor may prolong the survival of patients with gastric
carcinoma metastatic to the breast.
Breast metastases from gastric carcinomas are
associated with a poor prognosis, and the majority of patients
succumb within 1 year (19). The
survival of patients with breast metastases from gastric carcinomas
is significantly decreased compared with patients with primary
breast cancer (20). Breast
metastases from gastric carcinoma are rare; thus, increasing
awareness of the disease is important in order to avoid
misdiagnosis. Additional studies are required to define the best
treatment.
Acknowledgements
The present study was supported by the foundation
grant from JiangXi Province Scientific and Technological Bureau
(no. 20112BBG70051).
References
|
1
|
Cuzick J, Sestak I, Bonanni B, Constantino
JP, Cummings S, DeCensi A, Dowsett M, Forbes JF, Ford L, LaCroix
AZ, et al: SERM Chemoprevention of Breast Cancer Overview Group:
Selective oestrogen receptor modulators in prevention of breast
cancer: An updated meta-analysis of individual participant data.
Lancet. 381:1827–1834. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
National Cancer Institute. Surveillance,
Epidemiology and End Results Stat Fact Sheets: Female Breast
Cancer. National Cancer Institute. Bethesda, MD, USA: 15–16.
2014.
|
|
3
|
Kashlan RB, Powell RW and Nolting SF:
Carcinoid and other tumors metastatic to the breast. J Surg Oncol.
20:25–30. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Alva S and Shetty-Alva N: An update of
tumor metastasis to the breast data. Arch Surg. 134:4501999.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Albain KS, Nag SM, Calderillo-Ruiz G,
Jordaan JP, Llombart AC, Pluzanska A, Rolski J, Melemed AS,
Reyes-Vidal JM, Sekhon JS, et al: Gemcitabine plus paclitaxel
versus paclitaxel monotherapy in patients with metastatic breast
cancer and prior anthracycline treatment. J Clin Oncol.
26:3950–3957. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gennari A, Stockler M, Puntoni M, Sormani
M, Nanni O, Amadori D, Wilcken N, D'Amico M, DeCensi A and Bruzzi
P: Duration of chemotherapy for metastatic breast cancer: A
systematic review and meta-analysis of randomized clinical trials.
J Clin Oncol. 29:2144–2149. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
O'Shaughnessy JA, Kaufmann M, Siedentopf
F, Dalivoust P, Debled M, Robert NJ and Harbeck N: Capecitabine
monotherapy: Review of studies in first-line HER-2-negative
metastatic breast cancer. Oncologist. 17:476–484. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Arslan C, Dizdar O and Altundag K:
Systemic treatment in breast-cancer patients with brain metastasis.
Expert Opin Pharmacother. 11:1089–1100. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Domanski HA: Metastases to the breast from
extramammary neoplasms. A report of six cases with diagnosis by
fine needle aspiration cytology. Acta Cytol. 40:1293–1300. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Boutis AL, Andreadis C, Patakiouta F and
Mouratidou D: Gastric signet-ring adenocarcinoma presenting with
breast metastasis. World J Gastroenterol. 12:2958–2961. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Qureshi SS, Shrikhande SV, Tanuja S and
Shukla PJ: Breast metastases of gastric signet ring cell carcinoma:
A differential diagnosis with primary breast signet ring cell
carcinoma. J Postgrad Med. 51:125–127. 2005.PubMed/NCBI
|
|
12
|
Steinbrecher JS and Silverberg SG:
Signet-ring cell carcinoma of the breast. The mucinous variant of
infiltrating lobular carcinoma? Cancer. 37:828–840. 1976.PubMed/NCBI
|
|
13
|
Toombs BD and Kalisher L: Metastatic
disease to the breast: Clinical, pathologic, and radiographic
features. AJR Am J Roentgenol. 129:673–676. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Janni W, Rack B, Sommer H, Schmidt M,
Strobl B, Rjosk D, Klanner E, Thieleke W, Gerber B, Friese K and
Dimpfl T: Intra-mammary tumor location does not influence prognosis
but influences the prevalence of axillary lymph-node metastases. J
Cancer Res Clin Oncol. 129:503–510. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Briest S, Horn LC, Haupt R, Schneider JP,
Schneider U and Höckel M: Metastasizing signet ring cell carcinoma
of the stomach-mimicking bilateral inflammatory breast cancer.
Gynecol Oncol. 74:491–494. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gravalos C and Jimeno A: HER2 in gastric
cancer: A new prognostic factor and a novel therapeutic target. Ann
Oncol. 19:1523–1529. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lee SK, Kim WW, Kim SH, Hur SM, Kim S,
Choi JH, Cho EY, Han SY, Hahn BK, Choe JH, et al: Characteristics
of metastasis in the breast from extramammary malignancies. J Surg
Oncol. 101:137–140. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Luk YS, Ka SY, Lo SS, Chu CY and Ma MW: An
unusual case of gastric cancer presenting with breast metastasis
with pleomorphic microcalcifications. J Breast Cancer. 15:356–358.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Soler Parrell C, Palacios Marqués A, López
Saco L, De Las Heras Bermejo R and Martínez Pertusa S: Breast
metastatic localization of signet-ring cell gastric carcinoma. ISRN
Obstet Gynecol. 2011:4261502011.PubMed/NCBI
|
|
20
|
Zibari GB, Riche A, Zizzi HC, McMillan RW,
Aultman DF, Boykin KN, Gonzalez E, Nandy I, Dies DF, Gholson CF, et
al: Surgical and nonsurgical management of primary and metastatic
liver tumors. Am Surg. 64:211–220; discussion, 220–221.
1998.PubMed/NCBI
|