Introduction
Giant cell tumor of the tendon sheath (GCTTS), also
termed tendosynovial giant cell tumor, is a benign, slow-growing
tumor that originates from the tendon sheath or bursa (1). GCTTS is a type of tumor that mainly
occurs in the hand, and a previous study reported that only 3–5% of
GCTTS are detected in the foot and ankle (1). Microscopically, GCTTS is characterized
by a mixture of multinuclear giant cells, mononuclear cells and
histiocytes (1,2). GCTTS typically arises from the flexor
tendon sheath of the hand, but GCTTS in the foot is much less
frequently reported (3). However,
GCTTS should be considered as a differential diagnosis of soft
tissue tumors observed in the foot and ankle. Literature regarding
treatment strategies of GCTTS in the foot and ankle are limited due
to a scarcity of patients with this tumor type (Table I). Clinicians generally refer to
personal experience and preference when choosing surgical protocols
from various alternative operations for GCTTS patients. However,
the improper selection of surgical treatment may lead to
unfavorable outcomes and an unexpected burden on the patient;
hence, additional analyses of cases that have been diagnosed with
GCTTS in the foot and ankle are warranted for better postoperative
outcomes for patients. The present study describes the case of a
patient presenting with intra-articular GCTTS arising from the
right ankle capsule, which is a rare anatomical location for this
tumor.
 | Table I.Previous studies on giant cell tumor
of the tendon sheath in the ankle. |
Table I.
Previous studies on giant cell tumor
of the tendon sheath in the ankle.
| First author,
year | Age, years | Gender | Site of tumor | Clinical
manifestations | Type of lesion | Treatment | Recurrence | Ref. |
|---|
| Vasconez et
al, 2008 | 40 | F | Ankle | Slightly painful soft
tissue mass, plantar numbness, limitation of mobility | Localized | LE | No | (3) |
| Gibbons et al,
2002 | 28 | F | Ankle | NA | Localized | LEa | No | (8) |
| Gibbons et al,
2002 | 25 | M | Ankle | NA | Localized | LEa | No | (8) |
| Gibbons et al,
2002 | 22 | M | Ankle | NA | Localized | LEa | No | (8) |
| Gibbons et al,
2002 | 42 | M | Ankle | NA | Localized | LEa | No | (8) |
| Goni et al,
2012 | 36 | F | Ankle | Painless soft tissue
mass | Localized | LEb | No | (4) |
| Zhang et al,
2013 | 22 | F | Ankle | NA | Localized | LE | No | (1) |
| Zhang et al,
2013 | 33 | F | Ankle | NA | Localized | LEc | No | (1) |
| Zhang et al,
2013 | 15 | F | Ankle | NA | Localized | LE | No | (1) |
| Zhang et al,
2013 | 59 | M | Ankle | NA | Localized | LE | No | (1) |
| Zhang et al,
2013 | 51 | F | Ankle | NA | Localized | LE | No | (1) |
| Zhang et al,
2013 | 29 | F | Ankle and foot | NA | Localized | LE | Yes | (1) |
| Zhang et al,
2013 | 23 | F | Ankle | NA | Localized | LE | No | (1) |
| Zhang et al,
2013 | 31 | F | Ankle | NA | Localized | LE | No | (1) |
| Choudhury et
al, 2000 | 37 | F | Ankle | NA | Localized | LE | No | (5) |
| Pan et al,
2012 | 61 | F | Ankle | NA | Diffuse | WE∆ | Yes | (13) |
Case report
A 58-year-old female patient was referred to the
General Hospital of Jinan Military Region (Jinan, Shandong, China)
in December 2012 with a slow-growing swelling in the anterior
aspect of the right ankle that had been developing over 12 months.
The patient felt mild pain in the swelling a week prior to hospital
admission, but there was no history of trauma to the region prior
to the onset of symptoms. A clinical examination revealed the
presence of a 3.0×4.0 cm non-tender firm tumor in the anterior
aspect of the right ankle (Fig. 1).
There was no free mobility of the tumor over the underlying bone
surface, and the range of motion of the right ankle was not
compromised. A sonography revealed that the tumor possessed a
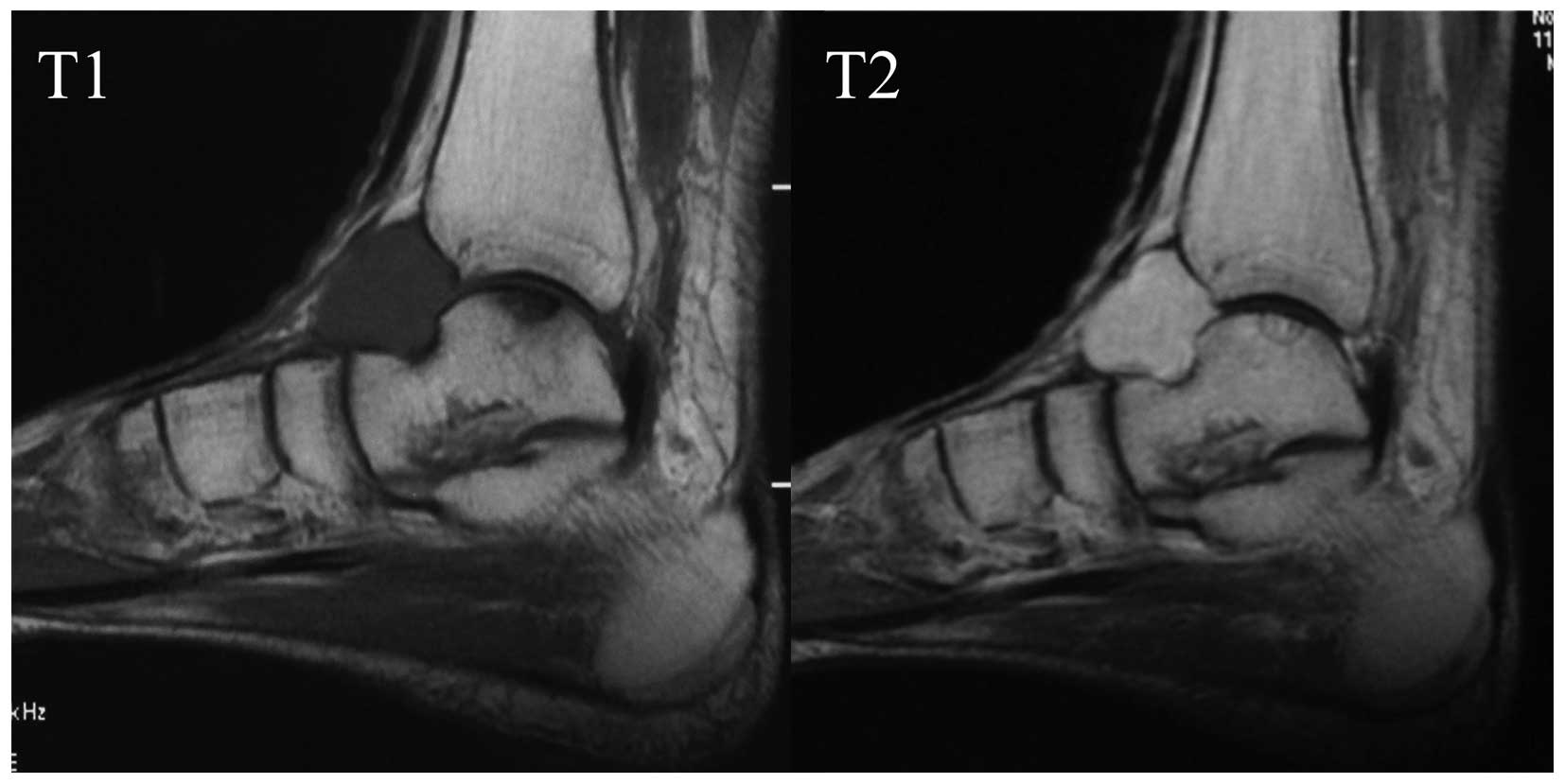
solid, homogeneous and hypoechoic nature. Magnetic resonance
imaging (MRI) indicated that the tumor was located in front of the
tibiotalar joint surface with isointensity on T1 weighted imaging
and mild hyperintensity on T2 weighted imaging. There was no
significant osseous erosion in the adjoining bone (Fig. 2). A marginal excision of the tumor was
performed under epidural anesthesia. Intra-operatively, the tumor
was well-circumscribed and gray-yellow, and was observed to
originate from the ankle capsule. Dorsalis pedis vessels and a
superficial peroneal nerve were dislocated laterally due to
compression by the tumor. The marginal resection of the tumor was
followed by a hydrogen peroxide lavage. The tumor was not malignant
and the adjacent non-tumorous structures were preserved. An imprint
in the front aspect of the underlying tibiotalar joint was
observed, due to the lasting compression by the tumor (Fig. 3). The capsule of the ankle was sutured
and the ankle was immobilized for 3 weeks post-operatively.
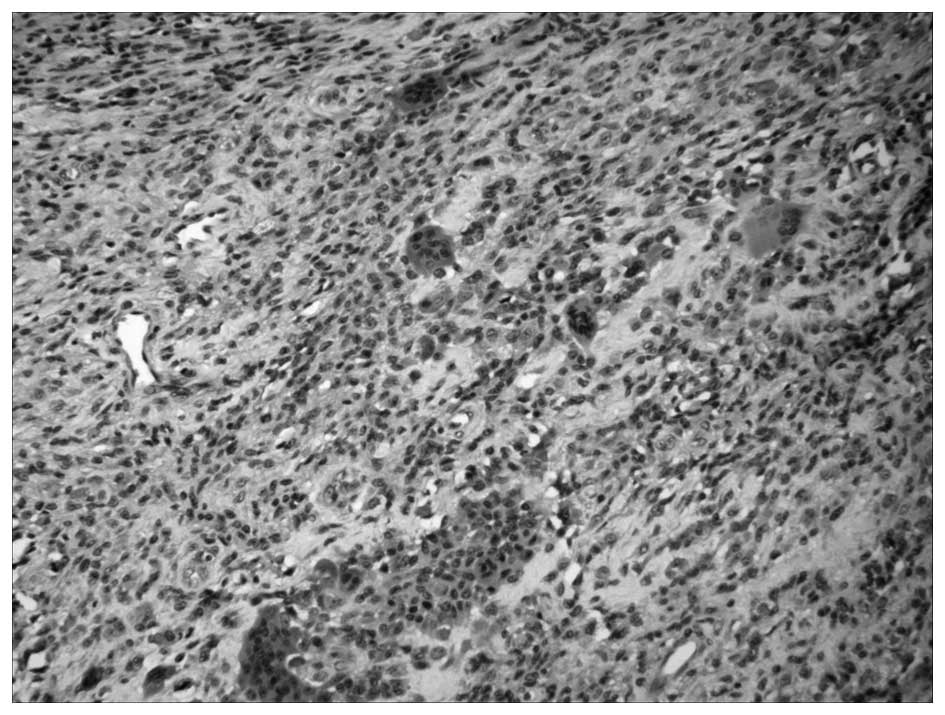
The resected tumor was sent to the Department of
Pathology, General Hospital of Jinan Military Region, for
histological analysis. Histological staining with hematoxylin and
eosin revealed a well-encapsulated tumor composed of a mixture of
mononucleated cells and multinuclear cells with thick fibrous
septae (Fig. 4). The patient was
subsequently diagnosed with GCTTS. Due to the lack of involvement
of adjacent structures, no adjuvant therapy was provided to the
patient. There was no evidence of recurrence during a follow-up
period of 12 months.
Discussion
GCTTS, also termed tendosynovial giant cell tumor,
is a benign, slow-growing solid soft-tissue tumor, with a mild
female predilection (4,5). The most common clinical observation is
the development of an asymptomatic mass, and additional symptoms,
including pain and a limited range of motion in the joints, are
suggestive of compression or involvement of structures adjacent to
the tumor (3,4). The origins of GCTTS remain to be
elucidated, including whether the tumor is neoplastic or reactive.
Karyotype analysis has identified abnormal cells in GCTTS, which is
considered to be evidence of neoplasia, whereas polymerase chain
reaction-based assays for methylation of the X-linked human
androgen receptor gene suggest GCTTS develops from polyclonal
proliferation, indicating that the disease is reactive or
hyperplastic (6). In addition, GCTTS
is considered to be due to injury, indicating a reactive nature;
however, this association has not been determined (7). Therefore, the nature of GCTTS remains to
be elucidated.
The involvement of the forefoot and hindfoot are
common locations of GCTTS of the foot and ankle, and the tumors are
primarily reported to originate from tendon sheaths surrounding the
ankle (1,8). In the present patient, the localized
tumor originated from the capsule of the ankle, and the patient
presented with an intra-articular mass, which is extremely rare for
GCTTS in this anatomical region. Although GCTTS rarely involves the
foot and ankle, it is extremely important to consider GCTTS as a
differential diagnosis for soft tissue tumors in this location. In
addition to GCTTS, differential diagnosis of soft tissue tumors in
the foot and ankle may consist of lipoma, a synovial cyst,
pigmented villondular synovitis (PVNS), fibromatosis,
undifferentiated pleomophic sarcoma, synovial sarcoma and
leiomyosarcoma (4,9). Imaging, such as ultrasonography and MRI,
has been identified as effective in differentiating GCTTS from
other soft tissue tumors in the foot and ankle (5). Ultrasonography differentiates a solid
mass from a cyst, and sonographically, GCTTS is a typically
homogeneous, solid and hypoechoic mass (10). Resonance imaging is the most valuable
modality in identifying GCTTS in the foot and ankle. MRI features
of GCTTS are associated with hemosiderin content in the tumor, and
tumors typically exhibit iso- or hypointensity on T1 weighted
images and hypointensity on T2 weighted images (11). Notably, the MRI features of GCTTS are
similar to those of PVNS, particularly when GCTTS is diffuse-type
(1). GCTTS originates from the
extra-articular synovium, and as a result, the majority of lesions
are located outside the ankle capsule, even when intra-articular
structures are involved (12). By
contrast, PVNS arises from the intra-articular synovium and
primarily involves intra-articular osseous and chondral structures
(1,13). Patients present with limited motion in
the ankle at an early-stage of disease (1,13). A
precise pre-operative diagnosis must be determined since the
surgical treatment of the two tumors is different; a local
resection with the removal of affected tissue is reported to be
effective in treating GCTTS, whereas a wide excision with ankle
fusion is recommend in PVNS, since the articular cartilage and
subchondral bone are extensively eroded (1,13).
Studies regarding treatment of GCCTS in the foot and
ankle are rare due to the scarcity of the tumor (Table I). The recurrence rate of GCTTS has
been reported to be as high as 44% and an integral removal of the
tumor is recommended as the pivotal treatment to prevent local
recurrence (12). In the present
study, the patient presented with a localized intra-articular GCTTS
of the ankle capsule, and the lesion was integrally removed
followed by a hydrogen peroxide lavage. The capsule was preserved
for the reconstruction of the ankle capsule and radical resection
was avoided due to the proximity of the tumor to the adjacent
non-tumorous structures. There was no evidence of recurrence during
follow-up. The present findings suggest that a local excision of
localized GCTTS in the ankle may be the treatment of choice, since
the removal of adjacent structures may be impossible. The optimal
treatment strategy regarding diffuse GCTTS, with involvement of
adjacent structures, including bone and cartilage, is controversial
and the recurrence rate in this type of GCTTS is increased
(1). Pan et al (13) reviewed the cases of patients with
GCTTS in the lower extremities and the authors suggested that the
articular structures should be exposed extensively in patients with
diffuse GCTTS and the affected structures require integral
excision. In addition, the authors advised that adjuvant
radiotherapy treatment is provided to patients to prevent local
recurrence. Goda et al (14)
conducted radiotherapy treatment for localized GCTTS in the thumb
with a customized device, and the outcome of this was favorable.
The present study hypothesizes that the prognosis of patients
presenting with GCTTS of the foot and ankle is dependent on a
precise pre-operative diagnosis and optimal treatment strategy
based on the biological behaviors of the tumors; however, the
efficacy of adjuvant therapy is unclear. The treatment of GCTTS,
particularly in diffuse GCTTS, remains to be determined, and
therefore additional clinical studies are required.
References
|
1
|
Zhang Y, Huang J, Ma X, Wang X, Zhang C
and Chen L: Giant cell tumor of the tendon sheath in the foot and
ankle: Case series and review of the literature. J Foot Ankle Surg.
52:24–27. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ushijima M, Hashimoto H, Tsuneyoshi M and
Enjoji M: Giant cell tumor of the tendon sheath (nodular
tenosynovitis). A study of 207 cases to compare the large joint
group with the common digit group. Cancer. 57:875–884. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vasconez HC, Nisanci M and Lee EY: Giant
cell tumour of the flexor tendon sheath of the foot. J Plast
Reconstr Aesthet Surg. 61:815–818. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Goni V, Gopinathan NR, Radotra BD,
Viswanathan VK, Logithasan RK and Balaji S: Giant cell tumour of
peroneus brevis tendon sheath - a case report and review of
literature. BMJ Case Rep. 2012:2012.PubMed/NCBI
|
|
5
|
Choudhury M, Jain R, Nangia A and Logani
KB: Localized tenosynovial giant cell tumor of tendon sheath. A
case report. Acta Cytol. 44:463–466. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vogrincic GS, O'Connell JX and Gilks CB:
Giant cell tumor of tendon sheath is a polyclonal cellular
proliferation. Hum Pathol. 28:815–819. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Monaghan H, Salter DM and Al-Nafussi A:
Giant cell tumour of tendon sheath (localised nodular
tenosynovitis): Clinicopathological features of 71 cases. J Clin
Pathol. 54:404–407. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gibbons CL, Khwaja HA, Cole AS, Cooke PH
and Athanasou NA: Giant-cell tumour of the tendon sheath in the
foot and ankle. J Bone Joint Surg Br. 84:1000–1003. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bancroft LW, Peterson JJ and Kransdorf MJ:
Imaging of soft tissue lesions of the foot and ankle. Radiol Clin
North Am. 46:1093–1103, vii. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Middleton WD, Patel V, Teefey SA and Boyer
MI: Giant cell tumors of the tendon sheath: Analysis of sonographic
findings. AJR Am J Roentgenol. 183:337–339. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
De Beuckeleer L, De Schepper A, De Belder
F, Van Goethem J, Marques MC, Broeckx J, Verstraete K and Vermaut
F: Magnetic resonance imaging of localized giant cell tumour of the
tendon sheath (MRI of localized GCTTS). Eur Radiol. 7:198–201.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Reilly KE, Stern PJ and Dale JA: Recurrent
giant cell tumors of the tendon sheath. J Hand Surg Am.
24:1298–1302. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pan GP, Zhao LJ, Fang Y and Feng RH:
Diagnosis and clinical application of MRI for giant cell tumor of
tendon sheath in lower extremity. Zhongguo Gu Shang. 25:953–956.
2012.(In Chinese). PubMed/NCBI
|
|
14
|
Goda JS, Patil P, Krishnappan C and
Elangovan D: Giant cell tumor of the tendon sheath treated by
brachytherapy (surface mold) technique-A technical illustration.
Brachytherapy. 8:79–83. 2009. View Article : Google Scholar : PubMed/NCBI
|