Introduction
Giant cell tumor of the tendon sheath (GCTTS)
predominantly occurs in the tendon sheaths of the hands (1). However, rare cases of GCTTS may occur in
larger joints, such as the knee and ankle joints (1). GCTTS usually occurs in individuals aged
between 30 and 50 years, with a female to male ratio of 2:1
(2). In Japan, the incidence rate of
GCTTS is 1 case per 50,000 individuals (3). The most common symptom of a GCTTS is a
painless swelling, and imaging studies usually reveal a
well-circumscribed soft tissue mass (2). To date, only a small number of cases of
GCTTS have been reported in the knee (4–11);
however, to the best of our knowledge, no cases of GCTTS in the
knee mimicking patellar tendinopathy have been previously reported.
The most common treatment for GCTTS is local excision, which
includes open surgery and arthroscopic excision (2,4–11). Previous case reports have suggested
that the arthroscopic excision of GCTTS in the knee has favorable
clinical outcomes (5,11). The reported rate of local recurrence
following surgery is 10–20% (4) and
the 5-year survival rate is 96% (12). However, these recurrences can usually
be controlled by surgical re-excision (2). The present study reports a case of GCTTS
in the knee mimicking patellar tendinopathy, due to the clinical
manifestation of anterior knee pain. The tumor was successfully
treated by arthroscopic excision. Written informed consent was
obtained from the patient.
Case report
In December 2012, a 36-year-old male patient
presented to the Department of Sports Medicine and Arthroscopy
Surgery of Huashan Hospital, Fudan University (Shanghai, China)
with a history of intermittent bilateral anterior knee pain for 9
months. The pain was stronger in the right knee compared with the
left, and it typically appeared following extensive walking or
during stair climbing, but disappeared at rest and during the
night. The patient often cycled but denied any history of knee
trauma. Physical examination revealed tenderness at the insertion
of the patellar tendon and proximal patellar tendon in both knees.
No effusion was observed and no mass was palpable. The range of
motion in both knees was normal (0–140°). Plain radiographs of both
knees were normal. Magnetic resonance imaging (MRI; Signa 1.5 T; GE
Healthcare, Milwaukee, WI, USA) of the right knee detected an oval
lesion located at the proximal segment of the infrapatellar fat
pad, with low signal intensity on T1-weighted images and high
signal intensity on T2-weighted images (Fig. 1). MRI of the left knee revealed no
abnormal findings and all laboratory tests were normal. Thus, a
diagnosis of GCTTS of the right knee was determined.
Under spinal anesthesia (10 mg bupivacaine
hydrochloride; Shanghai Harvest Pharmaceutical Co., Ltd., Shanghai,
China), which was administered for 75 min, right knee arthroscopy
was performed using the superolateral and anterolateral approaches,
as follows: The arthroscope was introduced through the
superolateral portal, followed by the insertion of a 4.5 mm
motorized shaver (Smith & Nephew Endoscopy, Andover, MA, USA)
through the anterolateral portal. Following removal of the synovium
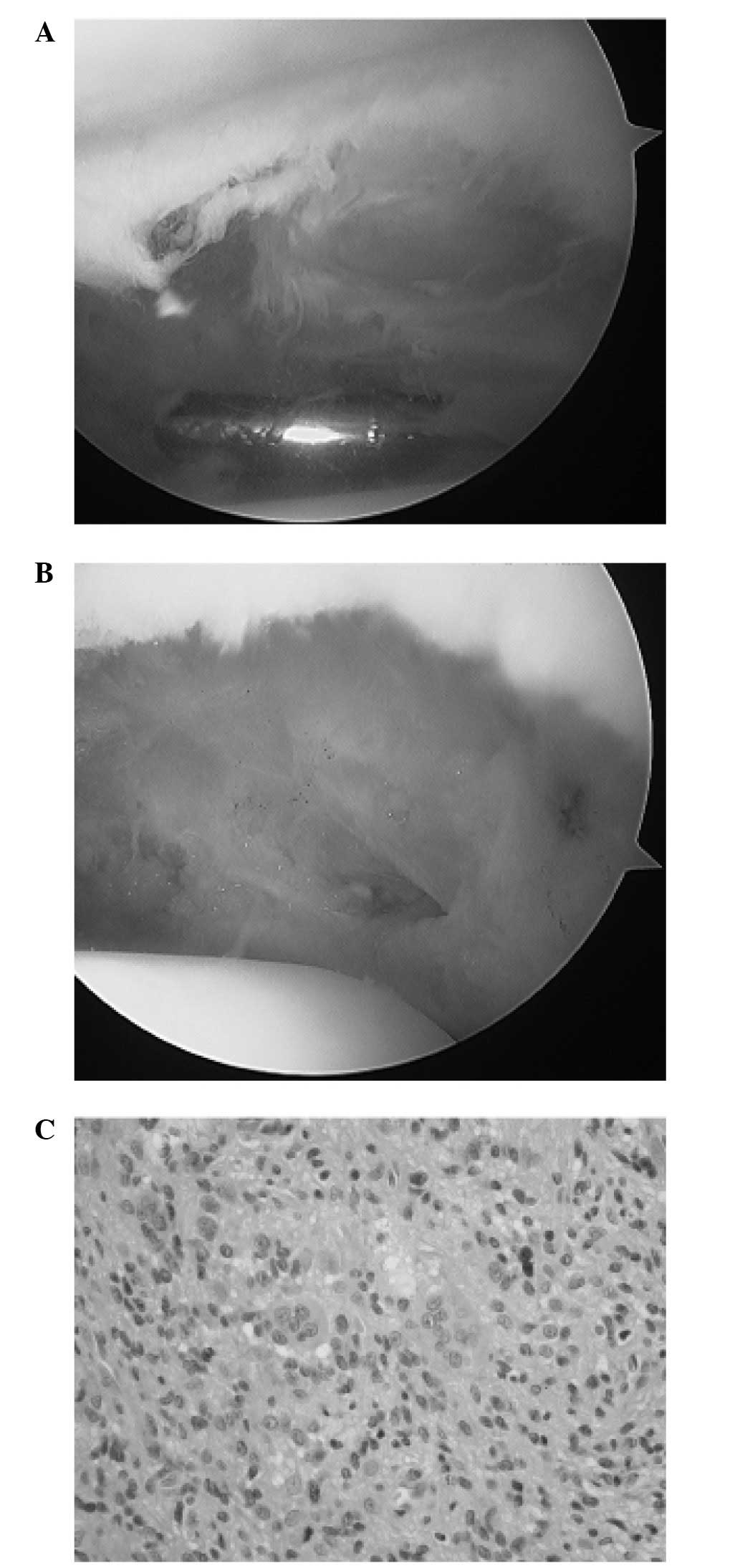
using a motorized shaver, a 2.0×1.5×1.2-cm well-defined yellow mass
covered by synovium was observed laterally adjacent to the distal
patella (Fig. 2A). The tumor was
removed using forceps (Shanghai Medical Instruments Co., Ltd.,
Shanghai, China) via the anterolateral approach, and the motorized
shaver and a radiofrequency ablation device (3.75 mm radiofrequency
ablation wand; ArthroCare Corporation, Austin, TX, USA) were
utilized to remove the peripheral synovium of the tumor, revealing
the fat underneath the tumor (Fig.
2B). The pain was relieved immediately following surgery. The
resected tissue was fixed in 10% formalin (Shanghai Ling Feng
Chemical Reagent Co., Ltd., Shanghai, China), paraffin (Leica
Biosystems Nussloch GmbH, Nussloch, Germany)-embedded and cut into
5-µm sections using a microtome (Leica RM2235; Leica Biosystems
Nussloch GmbH), prior to staining with hematoxylin and eosin (Baso
Diagnostics Inc., Zhuhai, China). Staining was visualized under a
microscope (Eclipse 55i; Nikon Corporation, Tokyo, Japan).
Pathological examination of the lesion revealed closely packed
medium-sized mononuclear cells with a variable admixture of giant
cells containing fat and hemosiderin, and evident stromal fibrosis
and hyalinosis. The mononuclear component comprised two types of
cells: small histiocyte-like cells, which represent the main
cellular component, and larger cells. A diagnosis of GCTTS was
subsequently confirmed by pathological examination (Fig. 2C), according to the World Health
Organization Classification of tumors of the soft tissue and bone
(2). No postoperative complications
occurred and the patient returned to full activity 6 weeks after
surgery. Furthermore, there was no evidence of recurrence at the
2-year follow-up examination.
Discussion
Anterior knee pain is a common symptom in
orthopaedic practice. Patellar tendinopathy is considered to be a
common cause of anterior knee pain, while the presence of tumors is
a particularly rare cause (9,13). The clinical presentation of GCTTS in
the knee is typically non-specific, thus, its clinical diagnosis is
challenging (4–11). In the present study, the GCTTS in the
knee mimicking patellar tendinopathy was located just posterior to
the proximal patellar tendon. Therefore, it was considered that the
GCTTS originated from the patellar tendon, as they were in close
proximity to one another. Thus, the present study suggests that
GCTTS should be considered in the differential diagnosis of
patellar tendinopathy. In such cases, physical examination is
insufficient to make a definitive diagnosis of the tumor. MRI scans
are required to establish the diagnosis of GCTTS (14); GCTTSs appear as well-circumscribed
lesions with a low signal intensity on T1-weighted images and a
high signal intensity on T2-weighted images (11).
Surgical treatment options for GCTTS in the knee
include arthroscopic excision and open surgery. Arthroscopy has
been applied in the diagnosis and treatment of this type of tumor
(5,11). The advantage of arthroscopic excision
is that it is minimally invasive. Furthermore, during arthroscopy,
accompanied disorders can be simultaneously diagnosed and treated
(5). However, GCTTSs most commonly
arise from patellar tendons and anterior cruciate ligaments
(4–11). If the GCTTS is covered by synovium, as
was the case with the present patient, direct arthroscopic
visualization of the tumor is not possible. In such cases, a
motorized shaver should be used to remove the synovium, thereby
exposing the underlying tumor. Open surgery allows adequate local
excision of tumors invading the surrounding tissue and thus,
exhibits a decreased risk of local recurrence when compared with
arthroscopy (4).
In conclusion, despite its rarity, GCTTS should be
considered in the differential diagnosis of patellar tendinopathy.
Furthermore, MRI is essential for the preoperative diagnosis of
this type of tumor. Regarding treatment options, the arthroscopic
excision of GCTTs of the tendon sheath in the knee can have
favorable outcomes.
References
|
1
|
Ushijima M, Hashimoto H, Tsuneyoshi M and
Enjoji M: Giant cell tumor of the tendon sheath (nodular
tenosynovitis). A study of 207 cases to compare the large joint
group with the common digit group. Cancer. 57:875–884. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
de St. Aubain Somerhausen N and Dal Cin N:
Giant cell tumour of tendon sheath. In: World Health Organization
Classification of Tumors. Pathology and Genetics of Tumors of Soft
Tissue and Bone. Fletcher CDM, Krishnan Unni K and Mertens F: IARC
Press. (Lyon). 110–111. 2002.
|
|
3
|
Monaghan H, Salter DM and Al-Nafussi A:
Giant cell tumour of tendon sheath (localised nodular
tenosynovitis): Clinicopathological features of 71 cases. J Clin
Pathol. 54:404–407. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Akahane T, Mori N and Yoshida K: Giant
cell tumor of the tendon sheath extending around the patellar
tendon and invading the knee joint and tibia: A case report. Oncol
Lett. 8:2800–2802. 2014.PubMed/NCBI
|
|
5
|
Cho HJ, Lee SH, Han SB, Lee DK, Kim CH and
Lee DH: Bilateral tenosynovial giant cell tumor of the knee
accompanied by chronic ACL tear. J Orthop Sci. 17:93–97. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chechik O, Amar E, Khashan M and Morag G:
Giant cell tumors in the patellar tendon area. J Knee Surg.
23:115–119. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sun C, Sheng W, Yu H and Han J: Giant cell
tumor of the tendon sheath: A rare case in the left knee of a
15-year-old boy. Oncol Lett. 3:718–720. 2012.PubMed/NCBI
|
|
8
|
Lüthje P and Nurmi-Lüthje I: Tenosynovial
juxta-articular giant-cell tumour of the knee-an unusual location
of the tumour. Acta Orthop Belg. 72:772–774. 2006.PubMed/NCBI
|
|
9
|
Relwani J, Factor D, Khan F and Dutta A:
Giant cell tumour of the patellar tendon sheath-an unusual cause of
anterior knee pain: A case report. Knee. 10:145–148. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Abdullah A, Abdullah S, Haflah NH and
Ibrahim S: Giant cell tumor of the tendon sheath in the knee of an
11-year-old girl. J Chin Med Assoc. 73:47–51. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Carls J, Kohn D and Maschek H: Benign
giant-cell tumor of the patellar ligament. Arthroscopy. 14:94–98.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Somerhausen NS and Fletcher CD:
Diffuse-type giant cell tumor: Clinicopathologic and
immunohistochemical analysis of 50 cases with extraarticular
disease. Am J Surg Pathol. 24:479–492. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kodali P, Islam A and Andrish J: Anterior
knee pain in the young athlete: Diagnosis and treatment. Sports Med
Arthrosc. 19:27–33. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jelinek JS, Kransdorf MJ, Shmookler BM,
Aboulafia AA and Malawer MM: Giant cell tumor of the tendon sheath:
MR findings in nine cases. AJR Am J Roentgenol. 162:919–922. 1994.
View Article : Google Scholar : PubMed/NCBI
|