Introduction
Umbilical hernia is a common surgical complication,
with ~10% of all primary hernias comprised of umbilical and
epigastric hernias (1). According to
the European Hernia Society classification, abdominal wall hernias
located 3 cm above to 3 cm below the umbilicus are defined as
umbilical hernia (2). In adults,
intra-abdominal hypertension is a major cause of umbilical hernia
(3). Predisposing factors for
intra-abdominal hypertension include obesity, pregnancy or ascites.
There are two primary repair options for umbilical hernias: Suture
and mesh. Currently, due to low recurrence rates, mesh
reinforcement is recommended (4).
Mucocele of the appendix is a descriptive term that implies a
dilated appendiceal lumen caused by abnormal accumulation of mucus
(5). Mucinous cystadenoma is the most
common cause of mucoceles of the appendix (63–84%) (6), and can generate a large amount of
ascites. An appendiceal mucocele is a rare condition that is
observed in 0.2–0.6% of all appendectomy specimens (7). Mucinous cystadenoma of the appendix is a
rare clinical entity with symptoms that can vary, which poses a
diagnostic challenge (8).
Appendectomy is advised for focal or diffuse mucosal hyperplasia
and cystadenoma when the appendiceal base is intact. Cecal
resection is performed for cystadenoma with a large base and right
colectomy is recommended for cystadenocarcinoma (9). In the present case, the increased
abdominal pressure followed by the accumulation of ascites
contributed to the occurrence of an umbilical hernia.
Case report
A 66-year-old female was admitted to the Third
Central Hospital of Tianjin (Tianjin, China) on 3 September 2014,
presenting with a 6-month history of a reducible mass in the
umbilical region. A tentative diagnosis of an umbilical hernia was
formed. The patient had no history of chronic coughing or
constipation. Local examination revealed a large umbilical hernia
(3 cm in diameter) when standing. Further examination revealed a
distended and soft abdomen with no signs of tenderness or rebound
tenderness, and no palpable mass or presence of shifting dullness.
The patient was confirmed to be negative for hepatitis and
cirrhosis. Tumor marker test results were as follows: Cancer
antigen (CA)72-4, 28.98 U/ml (normal range, <8.20 U/ml); CA-125,
40.21 U/ml (normal range, <35.00 U/ml); and carcinoembryonic
antigen (CEA), 11.55 ng/ml (normal range, <5.00 ng/ml).
Ultrasonography showed massive ascites and disclosed no
abnormalities in the liver, gallbladder, pancreas and spleen.
Increased levels of CA72-4, CA-125, CEA may indicate the existence
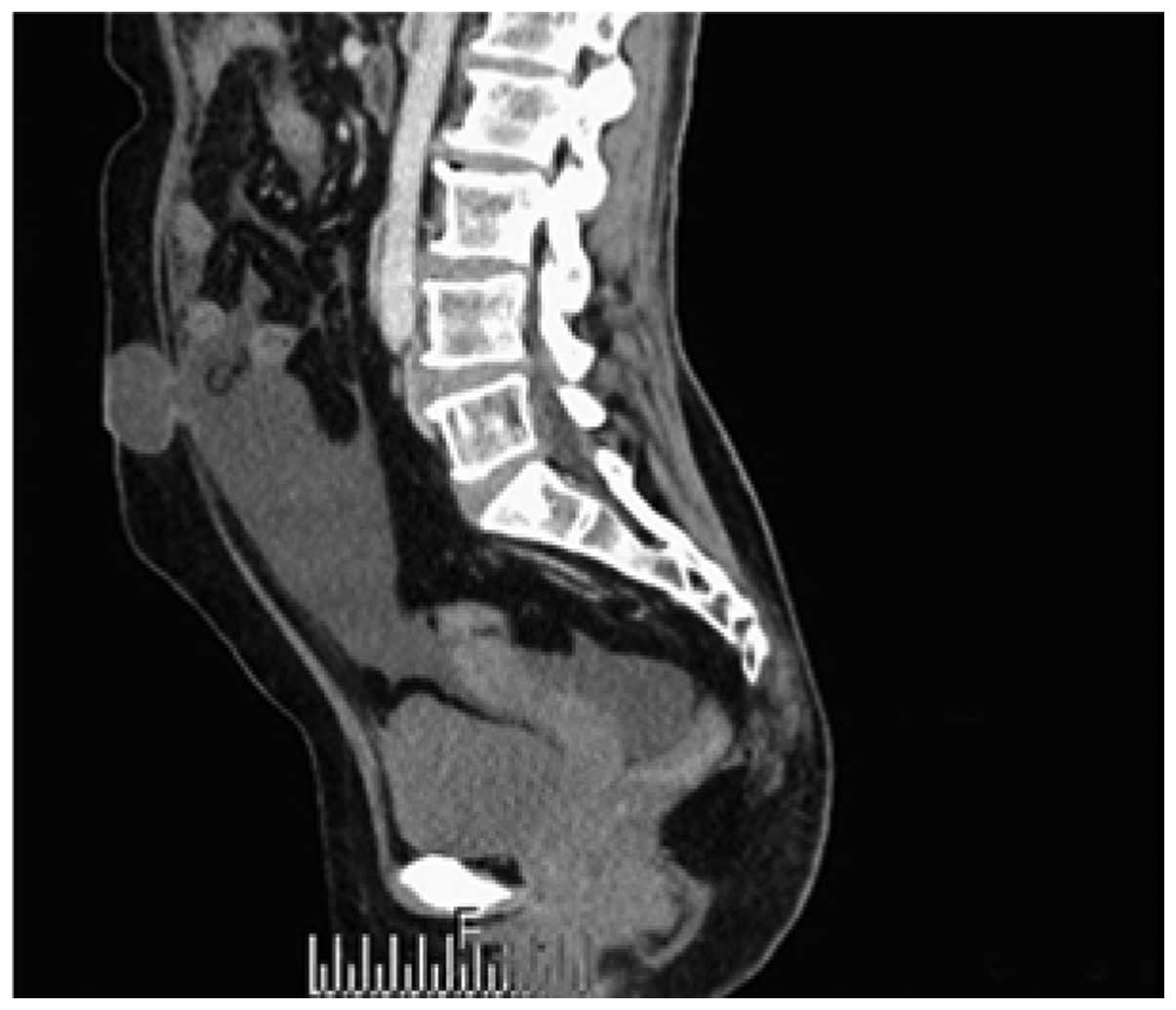
of coeliac or gynecological diseases. Computed tomography (CT) of
the abdomen using a SOMATOM Definition Flash CT scanner (Siemens
Healthcare AG, Munich, Germany) showed the following: i) An
umbilical hernia with abdominopelvic effusion (Fig. 1); ii) diffuse peritoneal and omental
thickening and calcification (Fig.
2); and iii) a cystic mass arising from the cecum, with
calcification observed on the inside (Fig. 3). Due to the increased levels of tumor
markers, abdominopelvic effusion and the imaging results, a
laparoscopic exploration was performed to identify the primary
cause of the hernia. During surgery, a yellow, jelly-like fluid
filling the abdominal cavity and a swollen appendix wrapped with
mucus and calcification were observed. Densely calcified foci were
interspersed among the omentum, mesentery and lower abdominal wall.
No uterine or ovarian abnormalities were found. Next, a
laparoscopic appendectomy was performed. The intraoperative
histopathological diagnosis was that of mucinous cystadenoma of the
appendix with malignant potential. The postoperative pathological
features included a single layer of tall mucus-secreting adenoma
cells, large amounts of mucin filling the lumen and scant mucinous
epithelium with low-grade dysplasia presented in mucinous pools.
However, no invasive lesions were observed. Therefore, the
post-operative pathology results diagnosed a borderline mucinous
appendiceal cystadenoma of low malignant potential. No
complications were observed in the post-operative period, and the
patient had no recurrent disease at 1 year follow-up. The present
study was approved by the Ethics Committee of the Third Central
Hospital of Tianjin and written informed consent was obtained from
the patient and her family.
Discussion
In adults, intra-abdominal hypertension is a major
cause of umbilical hernia (3). The
possible causes of intra-abdominal hypertension include obesity,
pregnancy or ascites. In the present case, it was believed that the
main cause of the umbilical hernia was ascites. The increased
levels of tumor markers and the CT scan findings led to the
consideration of the existence of ovarian cancer or mucinous
cystadenoma; the diagnosis of mucinous cystadenoma of the appendix
during laparoscopic exploration was unexpected.
An appendiceal mucocele is a rare condition that is
observed in 0.2–0.6% of all appendectomy specimens (7). Four histological types of appendiceal
mucocele exist: i) Retention cysts, ii) mucosal hyperplasia, iii)
mucinous cystadenoma; and iv) mucinous cystadenocarcinoma (10,11).
Mucinous cystadenoma is a rare cystic neoplasm of the vermiform
appendix, which characteristic villous adenomatous changes of the
appendiceal epithelium that are associated with marked distension
of the appendiceal lumen with mucin (12). Among these four types, mucinous
cystadenocarcinoma has the least developed etiology, and the
clinical progression of the disease has not yet been determined.
The clinical symptoms for mucinous cystadenocarcinoma may include
right lower abdominal pain, palpable abdominal masses, weight loss,
nausea, vomiting, gastrointestinal bleeding and signs of intestinal
intussusception (13); however, in
the present case, the disease presented as an umbilical hernia. In
the present study, ultrasonography did not provide useful
information, while the CT scan indicated peritoneal pseudomyxoma.
Peritoneal pseudomyxoma is a peritoneal or retroperitoneal
accumulation of a gelatinous substance secondary to the rupture of
a mucinous appendiceal lesion (14),
thus it occasionally combines mucinous ascites and peritoneal
implants, in which case the prognosis is considerably poorer,
synonymous with recurrent peritoneal involvement, which is known as
a gelatinous disease of the peritoneum (15). Pre-operatively, the high risk of an
appendiceal malignant tumor was considered in the present case;
however, the intraoperative histopathological diagnosis was of a
mucinous cystadenoma of the appendix, with malignant potential. An
appendectomy was the only surgical procedure performed, since it is
sufficient for the treatment of such cases.
In conclusion, patients with appendiceal mucoceles
present with a range of clinical symptoms. In the present case, the
patient presented with an umbilical hernia. An accurate diagnosis
is essential for the selection of the appropriate surgical
procedure. The present showed that laparoscopic exploration is a
useful procedure for the diagnosis of this intractable condition,
and an appendectomy may be performed at the same time if indicated.
Although rare, appendiceal mucoceles should be considered during
the diagnosis of an umbilical hernia.
References
|
1
|
Klinge U, Prescher A, Klosterhalfen B and
Schumpelick V: Development and pathophysiology of abdominal wall
defects. Chirurg. 68:293–303. 1997.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Muysoms F E, Miserez M, Berrevoet F,
Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi
I, Hauters P, et al: Classification of primary and incisional
abdominal wall hernias. Hernia. 13:407–414. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Muschaweck U: Umbilical and epigastric
hernia repair. Surg Clin North Am. 83:1207–1221. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kulaçoğlu H: Current options in umbilical
hernia repair in adult patients. Ulus Cerrahi Derg.
31:1572015.PubMed/NCBI
|
|
5
|
Shabeeb F, Hairol AO and Jarmin R:
Amyand's hernia with mucinous cysadenoma of the appendix. Indian J
Surg. 72:341–343. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pickhardt PJ, Levy AD, Rohrmann CA Jr and
Kende AI: Primary neoplasms of the appendix: Radiologic spectrum of
disease with pathologic correlation. Radiographics. 23:645–662.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Soueï-Mhiri MT, Tlili-Graies K, Ben
Cherifa L, Derbel F, Hmissa S, Dahmen Y and Jeddi M: Mucocele of
the appendix. Retrospective study of 10 cases. J Radiol.
82:463–468. 2001.(In French). PubMed/NCBI
|
|
8
|
Kelemouridou E, Mogrampi SA, Tsavis G,
Verroiotou M, Rallis T and Fardellas I: Mucinous cystadenoma of the
appendix. A diagnostic dilemma? Chirurgia (Bucur). 106:251–254.
2011.PubMed/NCBI
|
|
9
|
Zagrodnik DF II and Rose DM: Mucinous
cystadenoma of the appendix: Diagnosis, surgical management, and
follow-up. Curr Surg. 60:341–343. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Aho AJ, Heinonen R and Lauren P: Benign
and malignant mucocele of the appendix. Histological types and
prognosis. Acta Chir Scand. 139:392–400. 1973.PubMed/NCBI
|
|
11
|
Higa E, Rosai J, Pizzimbono CA and Wise L:
Mucosal hyperplasia, mucinous cystadenoma and mucinous
cystadenocarcinoma of the appendix. A re-evaluation of appendiceal
‘mucocele’. Cancer. 32:1525–1541. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Iswariah H, Metcalfe M, Lituri D and
Maddern GJ: Mucinous cystadenoma of the appendix. ANZ J Sur.
74:918–919. 2004. View Article : Google Scholar
|
|
13
|
Demetrashvili Z, Chkhaidze M, Khutsishvili
K, Topchishvili G, Javakhishvili T, Pipia I and Qerqadze V:
Mucocele of the appendix: Case report and review of literature. Int
Surg. 97:266–269. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fairise A, Barbary C, Derelle A, Tissier
S, Granger P, Marchal F, Laurent V and Régent D: Mucocele of the
appendix and pseudomyxoma peritonei. J. Radiol. 89:751–762.
2008.(In French). View Article : Google Scholar
|
|
15
|
Rouchaud A, Glas L, Gayet M and Bellin MF:
Appendiceal mucinous cystadenoma. Diagn Interv Imaging. 95:113–116.
2014. View Article : Google Scholar : PubMed/NCBI
|