Introduction
Tumors developing in the patella have a considerably
rare occurrence, with the vast majority of them being giant cell
tumors (GCTs) and chondroblastomas (1). Although the diagnosis and treatment of
these histologies are typically straightforward, only a few
patellar primary tumors have been reported to date (1). GCTs account for 33% of all patellar
tumors, while aneurysmal bone cyst (ABC) accounts for 5% of all
patellar tumors (1). Knee pain and/or
swelling are the most common symptoms of these two patellar tumors
(1). To the best of our knowledge,
the occurrence of patellar symbiotic tumors is considerably more
rare. GCT combined with ABC accounts for 14% of all GCTs (2), and has also been reported in other bone
locations, such as the rib (3),
calcaneus (4), talus (5), spine (6)
and radius (7). Only Marudanayagam
and Gnanadoss (8) have reported
patellar symbiotic tumors thus far. Imaging data is helpful for the
diagnosis of GCTs and ABCs and surgery is the main treatment used
for the two tumors. More studies are required to raise awareness of
this special type of tumor and to gain diagnostic and treatment
experience. In the present study, a case of GCT of the patella with
a secondary ABC is reported. Written informed consent was obtained
from the patient for the publication of the present study.
Case report
On 10th March, 2014, a 27-year-old male patient
visited the outpatient clinic of the Department of Orthopedics at
The First Affiliated Hospital of Dalian Medical University (Dalian,
China) complaining of right patellar pain, swelling and limited
mobility for 10 days subsequent to an unexpected fall. The patient
had no history of weight loss or exposure to tuberculosis.
Upon physical examination, swelling and localized
tenderness was detected by palpation in the front aspect of the
mid-patella. The right knee of the patient exhibited a decreased
range of motion and severe pain upon reaching maximal knee flexion.
The float and grinding tests of the whirlbone were positive.
However, there was no evidence of a soft-tissue mass and overlying
skin lesion. Furthermore, no joint effusion or synovial thickening
was noted.
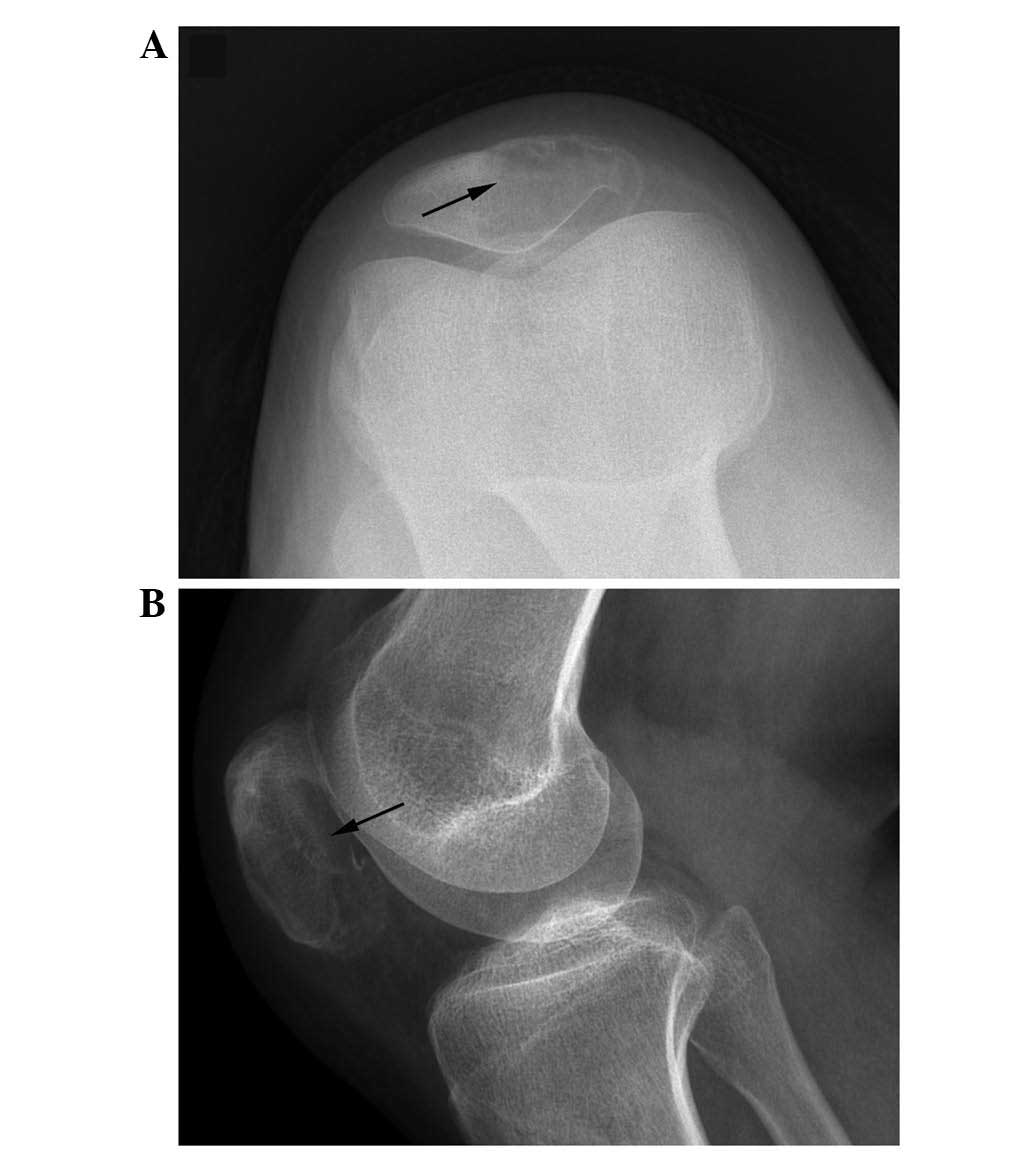
Direct radiographs (Figs.
1 and 2) and computed tomography
(CT) scans (SOMATOM Definition; Siemens Healthcare, Forchheim,
Germany) of the knee were performed. Radiographic examination
revealed a well-defined lytic lesion with a thin cortex occupying
2/3 of the patella, and no pathologic fracture or periosteal
reaction was observed. Bone tracer scanning (Infinia Hawkeye 4; GE
Healthcare Life Sciences, Pittsburgh, PA, USA) with
99mTc-methylene diphosphonate (Jiangsu Institute of
Nuclear Medicine, Wuxi, China) revealed a moderate tracer uptake in
the right patella. CT scan of the chest revealed no pulmonary
metastasis.
Following laboratory tests, only the levels of
C-reactive protein were observed to be slightly increased, at 13.5
mg/l (normal range, 0–10 mg/l). All other test results were within
the normal ranges.
Intraoperatively, no abnormality was noticed in the
soft tissue around the patella. The lesion was cystic and cavitary,
and contained granulation tissue in addition to 2 ml light bloody
fluids, which were discharged from the cavity. Subsequently, the
patient underwent curettage of the lesion using a high-speed burr
(Stryker, Mahwah, NJ, USA) through a 3×2-cm2 window
performed on the medial aspect of the patella. The material was
sent for formal histopathological examination. Following massive
saline irrigation, the cavities in the patella were filled with
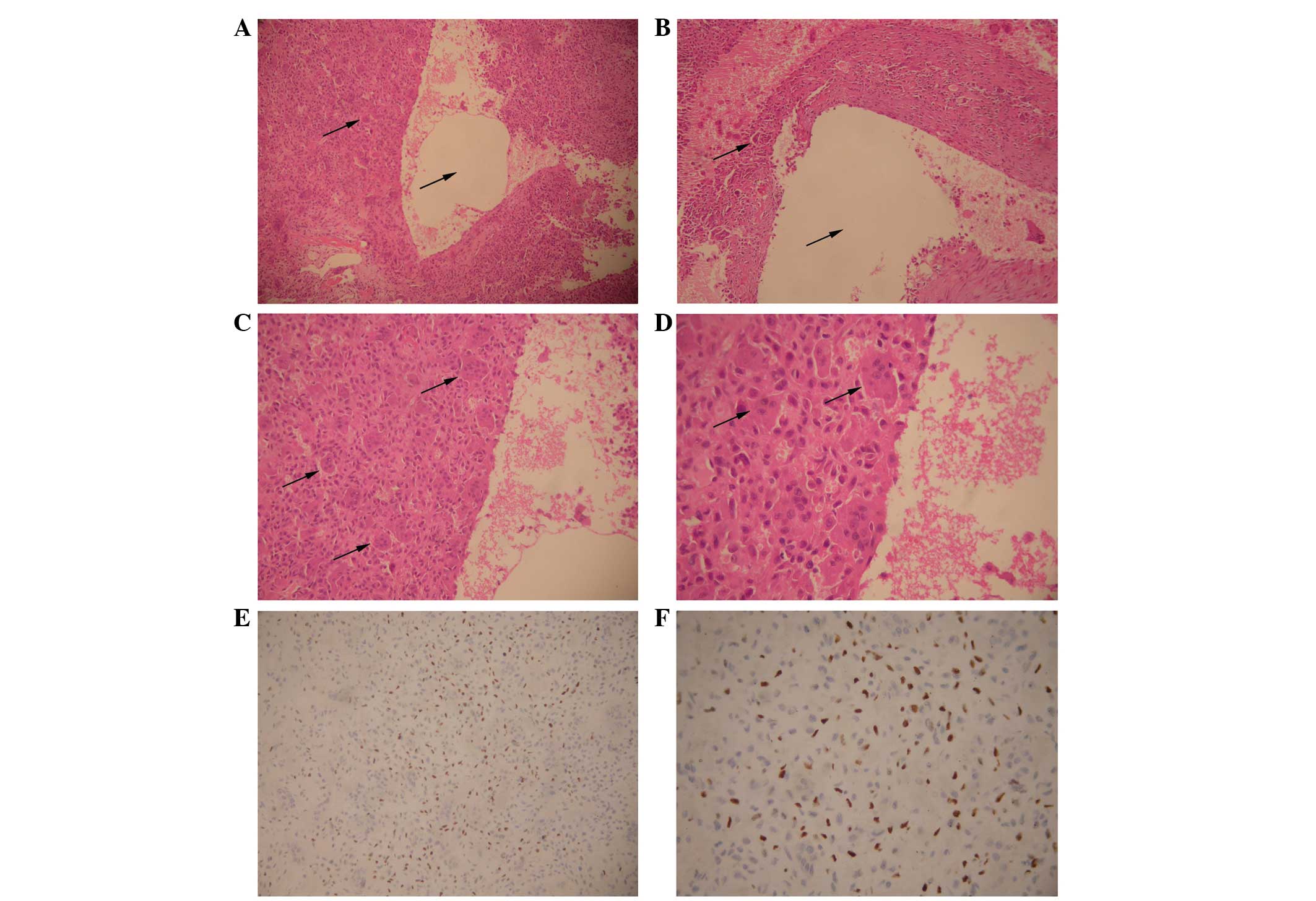
autogenic iliac bone and allograft bone graft. Histopathological
findings revealed features of GCT with ABC. Macroscopically, the
resected tumor tissue was grey, red and white; no necrosis was
observed. An ABC component was found, with clotted blood filling
the cystic cavities. Microscopic analysis (Leica DM-2500; Leica
Microsystems, Wetzlar, Germany) (Fig.
3) revealed typical characteristics of benign GCT, including
polygonal or cuboidal tumor cells, mitosis, thickened nuclear
membranes and multinucleated giant cells. The resected margin was
tumor-free. Immunohistochemistry results indicated that the tumor
cells were partly positive for P63 (monoclonal mouse anti-human
p63; #sc-8431; dilution, 1:1000), and negative for P53 (monoclonal
mouse IgG2a anti-human p53; #sc-126; dilution, 1:500)
and cluster of differentiation 68 (monoclonal mouse IgG1
anti-human CD68; #sc-20060; dilution, 1:100) (all antibodies from
Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA).
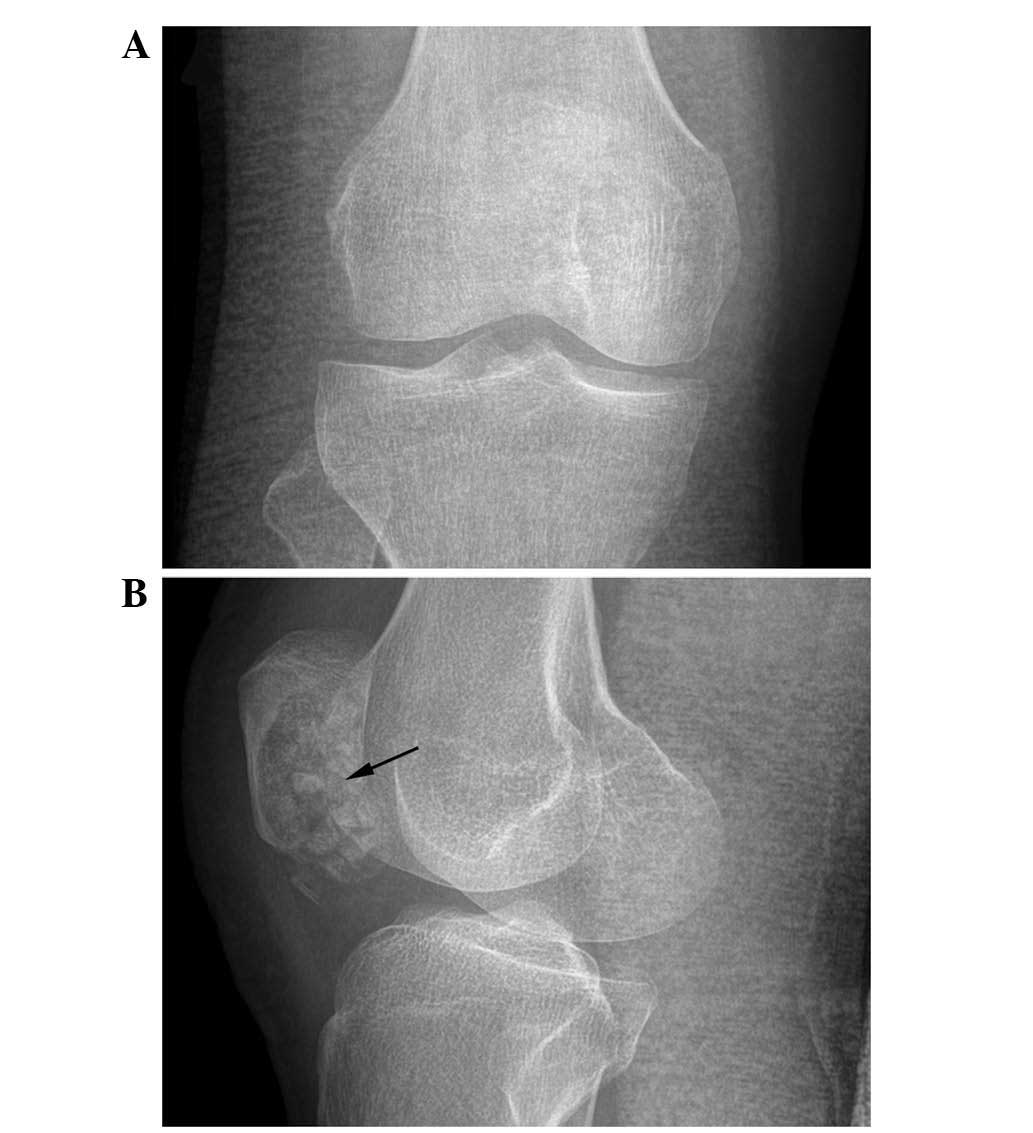
Following surgery, the patient visited the
outpatient clinic on a regular basis. Clinical and radiological
examinations, including palpation and plain radiography, were
performed (Fig. 4). No local
recurrence or distant metastasis were identified 12 months
following surgery. The patient had good functional outcome and
obtained a full range of motion on the right knee.
Discussion
Primary bone tumors originating from the patella are
rare lesions. In a review by Mercuri and Casadei (1), it was reported that benign tumors of the
patella are more frequent than malignant tumors. The most common
diagnosis of patellar tumors is GCT, accounting for 33% of all
patellar tumors, while patellar ABC accounts for only 5% of all
patellar tumors (1). Despite the fact
that GCT combined with ABC has also been reported in other bone
locations, including the rib (3),
calcaneus (4), talus (5), spine (6)
and radius (7), only 1 case of
patellar symbiotic tumors has been reported to date (8).
GCT of the bone is a common benign, locally
aggressive bone tumor that rarely metastasizes or causes mortality.
Recurrent and malignant GCTs have been associated with higher rates
of aneusomy than those exhibited by benign, diploidic GCT lesions.
GCT has been reported to account for ~5% of all pathologically
diagnosed primary bone tumors in Western populations (9–11) and 20%
of all biopsy-analyzed primary bone tumors in the Chinese
population (12). It can affect
individuals of any age, but tends to occur in young adults aged
20–45 years. Women are considerably more susceptible to GCT than
men. The majority of GCTs are located in the epiphyseal regions of
long bones, with the sacrum or spine as secondary sites of
involvement (13). Regional pain and
tenderness upon palpation are the most common symptoms of GCT
(14). Certain patients may present
with a visible or palpable mass. In addition, effusion, decreased
range of motion, activity-related pain or pathological fractures
may also be observed (15).
Radiographically, GCT may involve the diseased
patella, while ill-defined margins and pathological fractures are
frequently observed (16). CT scan
demonstrates cortical expansion and destruction, while magnetic
resonance imaging (MRI) reveals the presence of intra-articular
fluid, as well as the involvement of any ligament, tendon and
surrounding tissue and/or joint (17).
The typical histological appearance of GCT is that
of a locally destructive neoplasm with tumors composed of
mesenchymal fibroblast-like stromal cells (13). Other histological characteristics
include the presence of monocytic, mononuclear cells of myeloid
lineage and osteoclast-like, multinucleated giant cells (13). Treatment of GCT mainly includes
curettage, followed by bone grafting, excision, irradiation,
amputation (for certain patients who suffer from malignant GCT) and
adjuvant therapy (such as polymethylmethacrylate, phenol and
aqueous zinc chloride) following surgery (18).
ABC is a benign bone tumor with a low incidence (~5%
of all patellar tumors) that may manifest as a primary or secondary
lesion to another neoplasm, such as a GCT of the bone or
chondroblastoma (1). The majority of
ABC patients are females aged <20 years (19). Any bone may be affected by ABC;
however, the most common location is the metaphysis of long bones,
most frequently those of the lower extremities (20). Although the clinical manifestations of
ABC highly vary, the most common ones are pain and swelling.
Physical activity may aggravate the pain (15). The skin around the region of the cyst
may display inflammation and tenderness upon palpation (15). ABC near a joint may be the reason for
a decreased range of motion, while spinal ABC may cause nerve and
cord impingement. Pathological fractures due to ABC occur in ≤20%
of all ABC cases (21). Small lesions
display minor or no symptoms, and may be discovered by radiographs
following a pathological fracture, or incidentally. Plain film
imaging reveals a radiolucent lytic lesion in the metaphysis of the
bone, which is commonly eccentric and displays thinning of the
cortex. ABCs are often described as ‘soap bubbles’ due to their
expansile nature (20). CT scan may
indicate the presence of fluid in the bone and soft tissue
involvement, while MRI scan reveals multiple fluid-fluid levels
within the lesion. In MRI, the outline of the cyst appears as an
enhanced ring around the lesion, and is observed on T1- and
T2-weighted images (20).
Macroscopically, the appearance of ABC is similar to
that of a blood-filled sponge with a thin periosteal membrane
(20). Microscopically, the lesion is
composed of blood-filled spaces separated by connective tissue
septa containing fibroblasts, osteoclast-type giant cells and
reactive woven bone (22). Effective
radical treatment of primary and recurring ABC includes complete
resection of all tissues lining the cyst and any of its components
from the surrounding soft tissues (23). Following resection, the cavity could
be filled with bone chips, mesenchymal stem cells or
polymethylmethacrylate bone cement (20). According to the position and size of
the lesion, internal fixation may be used to maintain
stabilization. Embolization has also been used for larger lesions
(20).
The present study reported an unusual case of GCT
combined with ABC in the patella. Despite numerous reports on GCT
or ABC characteristics, the association between GCT and secondary
ABC remains poorly understood. Due to the limited number of
reports, the possibility of concurrent GCT with ABC may be easily
overlooked. The aim of the present study was to supply clinical
information in order to identify this rare type of patellar
tumor.
Glossary
Abbreviations
Abbreviations:
|
GCT
|
giant cell tumor
|
|
ABC
|
aneurysmal bone cyst
|
|
CT
|
computed tomography
|
|
MRI
|
magnetic resonance imaging
|
References
|
1
|
Mercuri M and Casadei R: Patellar tumors.
Clin Orthop Relat Res. 389:35–46. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Murphey MD, Nomikos GC, Flemming DJ,
Gannon FH, Temple HT and Kransdorf MJ: From the archives of AFIP.
Imaging of giant cell tumor and giant cell reparative granuloma of
bone: Radiologic-pathologic correlation. Radiographics.
21:1283–1309. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Locher GW and Kaiser G: Giant-cell tumors
and aneurysmal bone cysts of ribs in childhood. J Pediatr Surg.
10:103–108. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yale JF and Kaplan JA: Aneurysmal bone
cyst arising from a giant cell tumor of the calcaneus. J Am Podiatr
Med Assoc. 85:708–709. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kinley S, Wiseman F and Wertheimer SJ:
Giant cell tumor of the talus with secondary aneurysmal bone cyst.
J Foot Ankle Surg. 32:38–46. 1993.PubMed/NCBI
|
|
6
|
Wu Z, Yang X, Xiao J, Feng D, Huang Q,
Zheng W, Huang W and Zhou Z: Aneurysmal bone cyst secondary to
giant cell tumor of the mobile spine: A report of 11 cases. Spine
(Phila Pa 1976). 36:E1385–E1390. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Athanasian EA: Aneurysmal bone cyst and
giant cell tumor of bone of the hand and distal radius. Hand Clin.
20:269–281. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Marudanayagam A and Gnanadoss JJ:
Secondary aneurysmal bone cyst of the patella: A case report. Iowa
Orthop J. 26:144–146. 2006.PubMed/NCBI
|
|
9
|
Hoch B, Inwards C, Sundaram M and
Rosenberg AE: Multicentric giant cell tumor of bone.
Clinicopathologic analysis of thirty cases. J Bone Joint Surg Am.
88:1998–2008. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Donthineni R, Boriani L, Ofluoglu O and
Bandiera S: Metastatic behaviour of giant cell tumour of the spine.
Int Orthop. 33:497–501. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lewis VO, Wei A, Mendoza T, Primus F,
Peabody T and Simon MA: Argon beam coagulation as an adjuvant for
local control of giant cell tumor. Clin Orthop Relat Res.
454:192–197. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sung HW, Kuo DP, Shu WP, Chai YB, Liu CC
and Li SM: Giant-cell tumor of bone: Analysis of two hundred and
eight cases in Chinese patients. J Bone Joint Surg Am. 64:755–761.
1982.PubMed/NCBI
|
|
13
|
Steensma MR, Tyler WK, Shaber AG, Goldring
SR, Ross FP, Williams BO, Healey JH and Purdue PE: Targeting the
giant cell tumor stromal cell: Functional characterization and a
novel therapeutic strategy. PLoS One. 8:e691012013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Compere EL: The diagnosis and treatment of
giant cell tumors of bone. J Bone Joint Surg Am. 35:822–830.
1953.PubMed/NCBI
|
|
15
|
Goldenberg RR, Campbell CJ and Bonfiglio
M: Giant cell tumor of bone. An analysis of two hundred and
eighteen cases. J Bone Joint Surg Am. 52:619–664. 1970.PubMed/NCBI
|
|
16
|
Song M, Zhang Z, Wu Y, Ma K and Lu M:
Primary tumors of the patella. World J Surg Oncol. 13:1632015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Casadei R, Kreshak J, Rinaldi R, Rimondi
E, Bianchi G, Alberghini M, Ruggieri P and Vanel D: Imaging tumors
of the patella. Eur J Radiol. 82:2140–2148. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Amanatullah DF, Clark TR, Lopez MJ, Borys
D and Tamurian RM: Giant cell tumor of bone. Orthopedics.
37:112–120. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rădulescu R, Bădilă A, Manolescu R, Sajin
M and Japie I: Aneurysmal bone cyst - clinical and morphological
aspects. Rom J Morphol Embryol. 55:977–981. 2014.PubMed/NCBI
|
|
20
|
Whitmore A: Aneurysmal bone cysts. JAAPA.
26:56–57. 2013.PubMed/NCBI
|
|
21
|
Casadei R, Ruggieri P, Moscato M, Ferraro
A and Picci P: Aneurysmal bone cyst and giant cell tumor of the
foot. Foot Ankle Int. 17:487–495. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fletcher CD, Unni KK and Mertens F: World
Health Organization Classification of Tumours. Pathology and
Genetics of Tumours of Soft Tissue and Bone. IARC Press. (Lyon,
France). 247–251. 2002.
|
|
23
|
Tomasik P, Spindel J, Miszczyk L, Chrobok
A, Koczy B, Widuchowski J, Mrozek T, Matysiakiewicz J and Pilecki
B: Treatment and differential diagnosis of aneurysmal bone cyst
based on our own experience. Ortop Traumatol Rehabil. 11:467–475.
2009.(In English and Polish). PubMed/NCBI
|