Introduction
Ovarian cancer is a common malignant tumor seriously
threatening women's lives and health. Its mortality rate ranks
first among all gynecological tumors (1). In the past 10 years, along with the wide
development of cytoreductive surgery, novel chemotherapy drugs have
emerged unceasingly (1). Since
chemotherapy plans are constantly improving, the treatment of
ovarian cancer has greatly improved in recent years, and the
patients' quality of life has improved significantly as a result
(2). However, the 5-year survival
rate is still 30–50%; thus, chemotherapy has not obviously improved
the overall survival rate (3). One of
the main reasons for this observation is primary or secondary drug
resistance during chemotherapy. Previous studies revealed that
tumor drug-resistant mechanisms included oncogene activation,
anti-oncogene inactivation, reduced intracellular drug
concentration, drug target molecular changes, metabolism
detoxification, enhanced DNA damage repair function and inhibition
of tumor cells apoptosis, which is a comprehensive result of
polygenic, multiple factors and multiple steps (2). Ovarian cancer drug resistance has a
great impact on the prognosis of ovarian cancer. Therefore,
studying the occurrence and development mechanisms of ovarian
cancer drug resistance in order to reverse this process could
greatly improve the chemotherapy effect on ovarian cancer. To
identity the regulatory mechanisms responsible for ovarian cancer
chemotherapy drug resistance in order to improve the tumor
sensitivity to chemotherapeutic drugs (particularly in recurrent
tumors) is one of the effective ways to improve the survival rate
of ovarian cancer patients. The current study identified multiple
microRNAs (miRNAs or miRs) that were differentially expressed in
tumor tissue and serum of ovarian cancer patients. These miRNAs
have been reported to be important in the occurrence and
progression of ovarian cancer, and are expected to be used in early
diagnosis, prognosis, recurrence and treatment of ovarian cancer
(4–6).
miRNAs are small non-coding RNAs with gene
regulation function, which are 20–25 nucleotides-long and are
processed from a hairpin-structure precursor (7). Previous studies demonstrated that miRNAs
are mainly involved in the post-transcriptional control of
eukaryotic gene expression by inhibiting the translation of their
target gene or mediating the degradation of their target gene
messenger RNA (mRNA) (7). miRNAs
participate in cell proliferation, differentiation, apoptosis and
cell cycle regulation processes. In recent years, a growing number
of studies demonstrated that miRNAs are involved in multiple
processes, including tumor occurrence, development, invasion,
metastasis and prognosis (8). miRNAs
are important in the occurrence and development of breast,
colorectal, lung, ovarian and liver cancer, as well as other
malignant tumors (9). Kinose et
al (10) noticed that the
expression levels of miR-15a and miR-16 were decreased in ovarian
cancer tissues and cell lines. miR-15a and miR-16 directly acted on
the proto-oncogene (B-cell specific moloney leukemia virus
insertion site 1) Bim-1 and played a role as anti-oncogenes by
inhibiting the expression of Bim-1 (10). Previous studies also demonstrated that
miR-21 was abnormally highly expressed in ovarian cancer tissues,
and was closely associated with the differentiation of tumor cells
and lymph node metastasis, suggesting that miR-21 may promote the
development of ovarian cancer as an oncogene (11). These studies indicated that the
occurrence and development processes of ovarian cancer were closely
associated with miRNA levels (11,12).
miRNAs are closely associated with the drug
sensitivity of numerous tumors. Among them, miRNA let-7i was the
first member of the miRNA family identified to be associated with
tumor drug sensitivity, and was observed to play an indirect
anti-tumor role by increasing the cell sensitivity to
chemotherapeutic drugs (13). Lee
et al (14) demonstrated that
the expression of let-7i was decreased in platinum-resistant
ovarian tumor cells, and downregulation of the expression of let-7i
could increase ovarian cancer resistance to cisplatin, suggesting
that let-7i could be used as a chemical marker to evaluate the
prognosis of ovarian cancer. However, the specific mechanism of
chemotherapy drug resistance remains unclear. Nurkkala et al
(15) demonstrated that inhibition of
phosphatase and tensin homolog (PTEN)-targeted regulation by an AKT
inhibitor or miR-214 directly could reduce the miR-214-mediated
survival rate and cisplatin-resistance through PTEN/AKT signaling
in PTEN/AKT-induced ovarian cancer drug-resistant cells. The above
methods could increase chemotherapy drug sensitivity of ovarian
cancer patients, which could be used in the treatment of recurrent
and chemotherapy-resistant ovarian cancer in order to improve the
treatment of ovarian cancer.
In the present study, using the drug-resistant
characteristics of SKOV3/DDP, SKOV3, COC1/DDP and COC1 cells, the
differences in miRNA expression profiles between the SKOV3/DDP,
SKOV3, COC1/DDP and COC1 cell lines were compared. miRNA expression
in drug-resistant and drug-sensitive ovarian cancer cell lines was
detected. The potential therapeutic target of the ovarian cancer
drug-resistant mechanism and the possible improvement of drug
resistance was investigated at the miRNA level.
Materials and methods
Cells and chip
The drug-resistant and drug-sensitive ovarian cancer
cell lines SKOV3 and COC1 cell lines (SKOV3/DDP, drug-resistant;
SKOV3, drug-sensitive; COC1/DDP, drug-resistant; COC1,
drug-sensitive) were used in the present study. SKOV3/DDP and SKOV3
cells were purchased from the Cancer Institute and Hospital,
Chinese Academy of Medical Sciences (Beijing, China). SKOV3 cells
and SKOV3/DDP cells were cultivated in RPMI-1640 culture medium
containing 10% fetal bovine serum (Gibco®; Thermo Fisher
Scientific, Inc., Waltham, MA, USA) without penicillin or
streptomycin under 5% CO2 and 37°C saturated humidity.
These cells exhibited adherent growth. COC1/DDP and COC1 cells were
purchased from the Wuhan University cell library, and cultivated in
RPMI-1640 culture medium containing 10% fetal bovine serum without
penicillin or streptomycin under 5% CO2 and 37°C
saturated humidity. These cells displayed suspended growth. The
drug-resistant SKOV3/DDP and COC1/DDP maintenance concentration of
cisplatin (Qilu Pharmaceutical Co. Ltd., Jinan, China) was 1
µg/ml.
A total of 924 probes (data from Sanger miRNA
database miRBase 12. 0, August 2012; www.pageinsider.com/microrna.sanger.ac.uk) were
designed for a chip experiment aiming to analyze 677 human, 292 rat
and 461 mice mature miRNAs, using the mammalian miRNA chip V3
(Beijing Bo'ao Hengxin Biotechnology Co., Ltd., Beijing, China).
The probe was arrayed on 75×25-mm, chemically modified glass slides
with chip microarray SmartArrayer™ (CapitalBio Corporation,
Beijing, China). Each probe was repeated three times.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total cell miRNA was extracted using the TaqMan
probe method (Thermo Fisher Scientific, Inc.) and extracted using
mirVana miRNA Isolation kit (Ambion; Thermo Fisher Scientific,
Inc.). miRNA was detected with the Applied Biosystems 7300
Real-Time PCR System (Thermo Fisher Scientific, Inc.) with the
following cycling conditions: 95°C for 10 min, and 40 cycles of
95°C for 15 sec and 60°C for 30 sec, followed by melt-curve
analysis.
Cell transfection
Cell transfection was performed with Lipofectamine
2000, according to the manufacturer's protocol (Invitrogen; Thermo
Fisher Scientific, Inc.). The final concentration of the
miRNA-transfected molecules Homo sapiens (hsa)-miR-30a-5p
precursor molecule pre-hsa-miR-30a-5p, hsa-miR-30a-5p inhibitory
molecule anti-hsa-miR-30a-5p and the corresponding negative
controls pre-scramble and anti-scramble miRNAs (Ambion; Thermo
Fisher Scientific, Inc.) was 30 nmol/l. The cellular total miRNAs
were extracted after transfection for 24 and 48 h.
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)
assay
Cells were digested into a monoplast suspension with
trypsin after transfection for 24 h. The density was adjusted to
1×104 cells/ml and inoculated in a 96-well plate, (100
µl/well). Control groups were established prior to and following
transfection. The cells in the 96-well plate were changed into the
prepared concentration gradient of cisplatin in culture medium 24 h
later. Five wells were set for each concentration, and the cells
were cultured for additional 48 h. Next, 10 µl MTT was added in
each well, and the absorbance of each well was detected at 490 nm
wavelength after being incubated for 4 h in the dark. The median
lethal concentration (IC50) of cisplatin was calculated.
Each experiment was repeated three times, and five wells were set
each time.
Statistical analysis
SPSS version 13.0 software (SPSS, Inc., Chicago, IL,
USA) was used for statistical analysis. Data are presented as the
mean ± standard error of the mean. Student's t-test was used to
compare the mean value between two groups. P<0.05 was considered
to indicate a statistically significant difference.
Results
Identification of mRNA extraction
quality
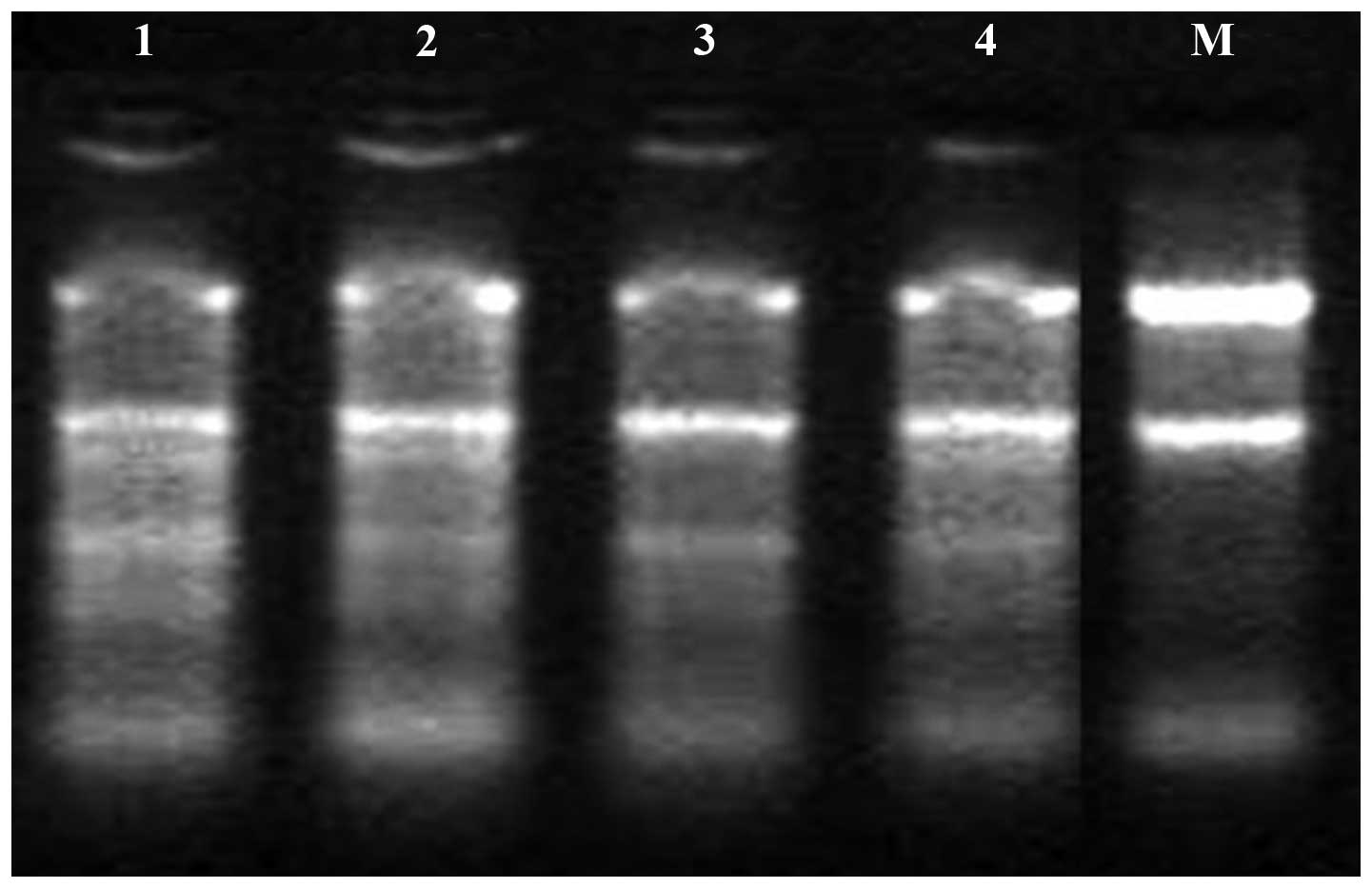
RNA electrophoresis results are shown in Fig. 1. Bands corresponding to 5.8S, 18S and
28S were clearly visible, indicating that non-biodegradable mRNA
was obtained. The electrophoresis results revealed that the band
brightness of RNA 28S was more close to 1:1 than that of 18S mRNA.
Thus, the quality of the mRNA extracted met the experimental
requirements, and the miRNA chip experiment could subsequently be
performed.
Differences in expression profile
analyzed by miRNA microarray chip
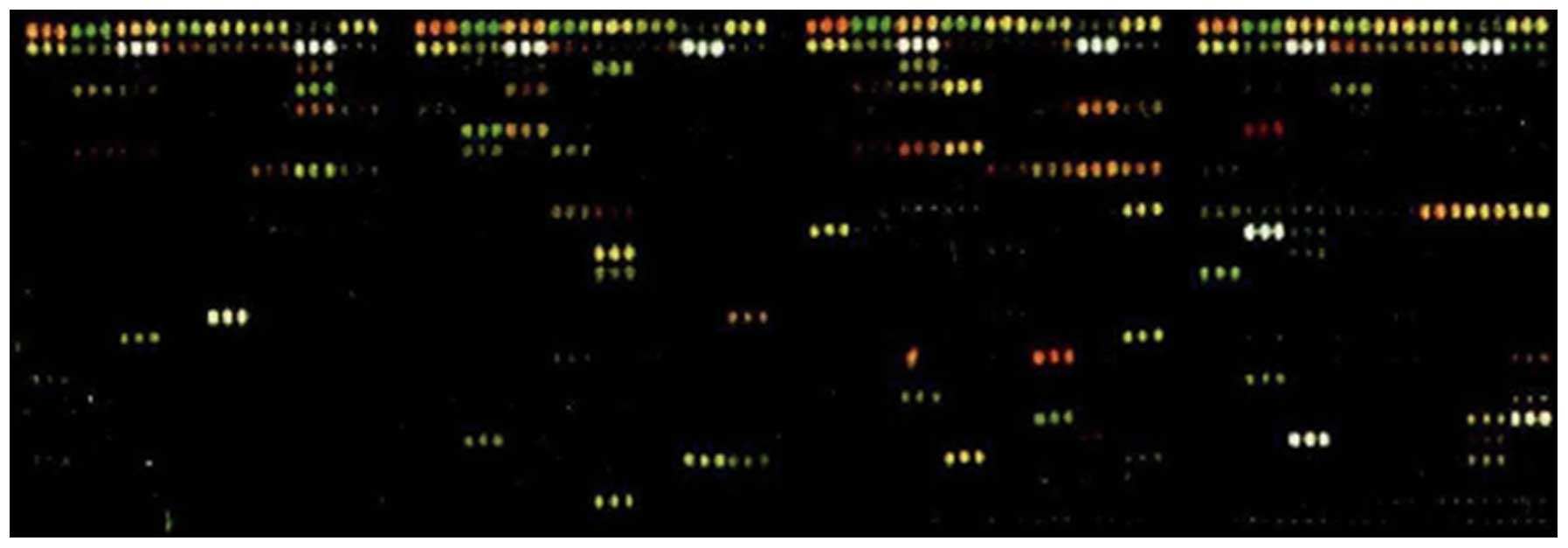
miRNA expression in drug-resistant and
drug-sensitive ovarian cancer cells was detected by gene chip
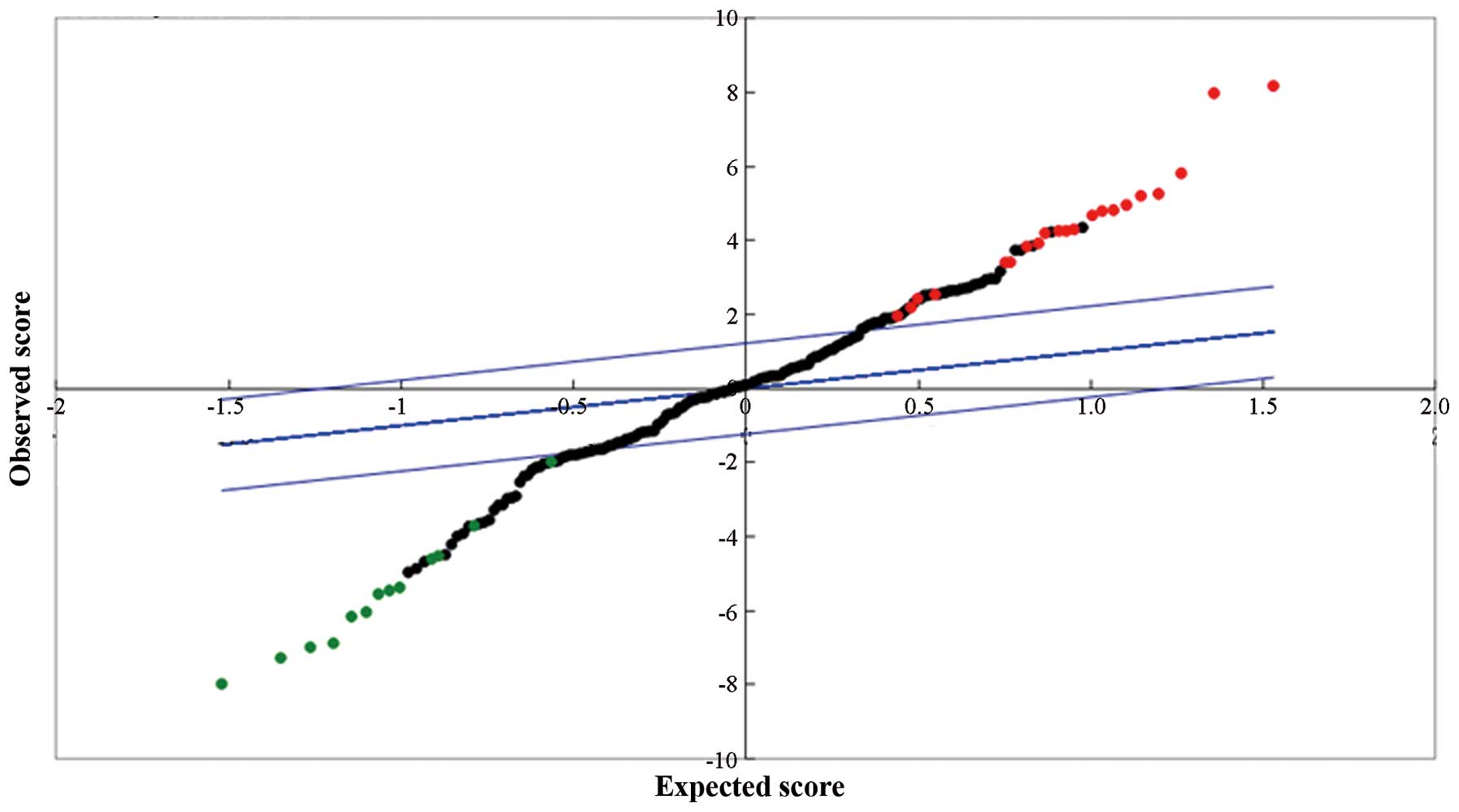
technology. Fig. 2 describes the
miRNA chip hybridization results obtained, while Fig. 3 represents the results of miRNA
statistical scatter diagram.
Compared with the drug-sensitive ovarian cancer
SKOV3 cell line, 19 miRNAs, including hsa-miR-99a-5p,
hsa-miR-30a-5p, hsa-miR-34c-5p, hsa-miR-31-3p and hsa-miR-181d,
were highly expressed in the drug-resistant SKOV3/DPP cell line,
while 20 miRNAs, including hsa-miR-96-5p, hsa-miR-193b-3p and
hsa-miR-200c-3p, were lowly expressed. In addition, 22 miRNAs,
including hsa-miR-34a-5p, hsa-miR-30a-5p and hsa-miR-181c-3p, were
highly expressed in the COC1/DPP cell line compared with the COC1
cell line, while 22 miRNAs, including hsa-miR-892b and
hsa-miR-505-5p, were lowly expressed. Among them, both
hsa-miR-30a-5p and hsa-miR-181 were highly expressed in the two
cell lines.
Detection of miRNA expression by
RT-qPCR
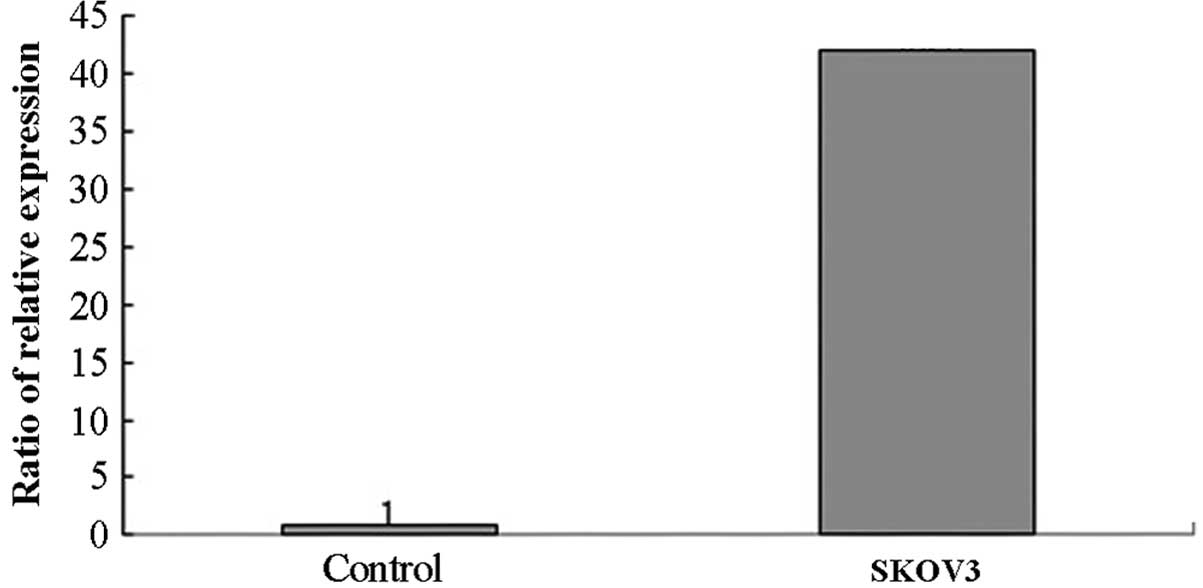
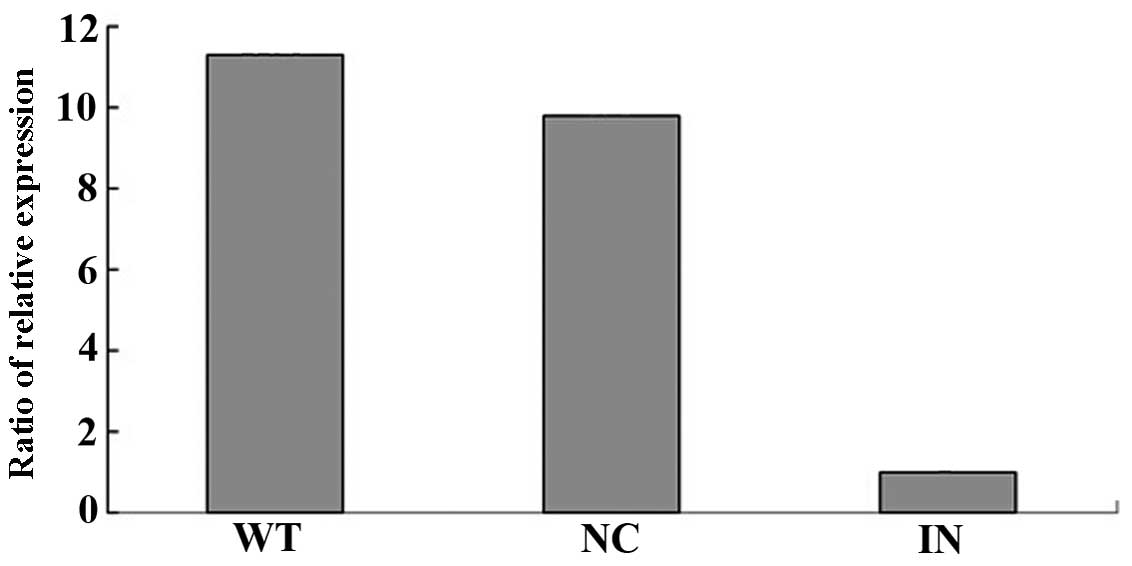
RT-qPCR was used to analyze the expression of
miRNA-30a-5p in SKOV3/DDP and SKOV3 cells after transfection for 24
h. The results revealed that the ΔCq of miRNA-30a-5p was 2.3 after
SKOV3 cell transfection with pre-miR for 24 h, while the ΔCq was
7.7 in the negative control group. The relative expression level of
miRNA-30a-5p was 42.2 times that of the negative control group
after cell transfection with pre-miR for 24 h. The RT-qPCR results
also revealed that the ΔCq of miRNA-30a-5p was 8.9 after SKOV3/DDP
cell transfection with pre-miR inhibitor for 24 h, while the ΔCq of
the negative control group was 5.6. The relative expression of
miRNA-30a-5p was 9.8 times that of the negative control group after
cell transfection with pre-miR inhibitor for 24 h (Figs. 4 and 5).
Effect of miRNA-30a-5p transfection on
SKOV3/DDP and SKOV3 cells drug resistance
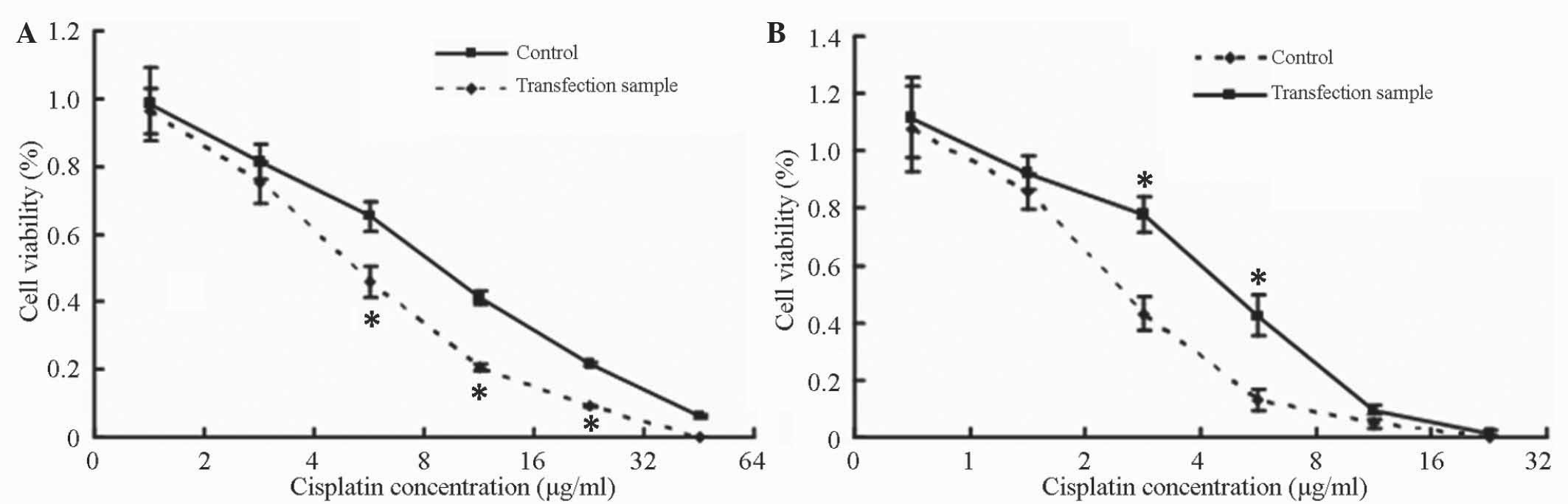
SKOV3/DDP cells exhibited reduced resistance to
cisplatin after transfection with inhibitor. The IC50
value was 7.6±0.38 µg/ml in these cells compared with 13±0.47 µg/ml
in the negative control group. The difference between the two
groups was significant (P<0.05) (Fig.
6A).
SKOV3 cells exhibited increased resistance to
cisplatin after pre-miR transfection (IC50=3.5±0.26
µg/ml vs. 1.8±0.12 µg/ml for the negative control group). The
difference between the two groups was significant (P<0.05)
(Fig. 6B).
Effect of miRNA-30a-5p on SKOV3/DDP
and SKOV3 cell activities
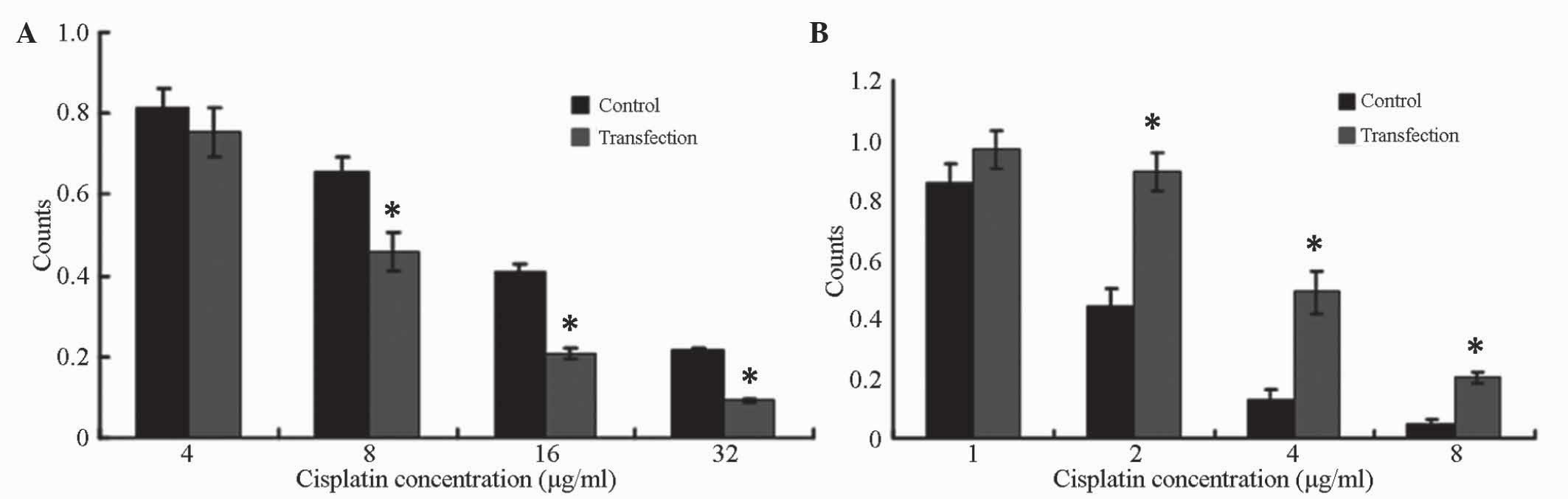
The cell number was significantly lower than that of
the negative control group after 48 h of incubation with different
concentrations of cisplatin following the transfection of SKOV3/DDP
cells with inhibitor for 24 h cells (P<0.05). The cell activity
was decreased significantly (Fig.
7A).
The cell number was significantly higher than that
of the negative control group after 48 h of incubation with
different concentrations of cisplatin following the transfection of
SKOV3 cells with inhibitor for 24 h cells (P<0.05). The cell
activity was increased significantly (Fig. 7B).
Discussion
A number of studies have demonstrated that miRNAs
are involved in the occurrence and development of ovarian cancer
(10–12). Zhang et al (16) reported that miRNA was involved in the
occurrence and development of ovarian cancer drug resistance by
studying a stem cell-like epithelial ovarian cancer line. Li et
al (17) demonstrated that
miRNA-27a was associated with ovarian cancer drug resistance, and
the mechanism was that MDR1/P-GP gene regulated the HIPK2 gene.
Sorrentino et al (8) detected the expression of let-7e,
miR-30C, miR-125b, miR-30a and miR-335 in the wild-type ovarian
cancer cell line A2780, paclitaxel-resistant cell line A2780TAX and
cisplatin-resistant cell line A2780CIS by chip technology. The
authors observed that let-7e was overexpressed in A2780TAX cells,
while miR-125b was lowly expressed in this cell line. Two miRNAs
were inversely expressed in the other cell lines, while miR-30c,
miR-130a and miR-335 were all lowly expressed in the above three
cell lines (8). Therefore, it was
inferred that let-7e had an inverse correlation with miR-125b, and
that miRNA expression in ovarian cancer was associated with drug
resistance of ovarian cancer, which was consistent with other
studies (18–20).
In the present study, a miRNA microarray chip
platform containing 924 probes was used for hybridization. The
differentially expressed miRNAs between chemotherapy resistance and
chemotherapy sensitivity in the ovarian cancer cell lines SKOV3/DDP
and SKOV3 were screened. Among them, 19 miRNAs, including
hsa-miR-99a-5p, hsa-miR-30a-5p, hsa-miR-34c-5p, hsa-miR-31-3p and
hsa-miR-181d, were observed to be highly expressed in SKOV3/DPP vs.
SKOV3 cell lines, while 20 miRNAs, including hsa-miR-96-5p,
hsa-miR-200c-3p and hsa-miR-193b-3p, were lowly expressed. In
addition, 22 miRNAs, including hsa-miR-34a-5p, hsa-miR-30a-5p and
hsa-miR-181c-3p, were observed to be highly expressed in COC1/DPP
vs. COC1 cell lines, while 24 miRNAs, including hsa-miR-892b and
hsa-miR-505-5p, were lowly expressed. Among them, both
hsa-miR-30a-5p and hsa-miR-181 were highly expressed in the two
cell lines. These findings may provide a theoretical basis and a
novel approach to further study the association between miRNA and
cisplatin resistance in ovarian cancer cells, as well as its
possible mechanism.
miRNAs are likely to be important in the occurrence,
development, diagnosis and treatment of ovarian cancer; thus, the
number of studies on abnormal expression profiles of miRNA in serum
and tissue of ovarian cancer patients has increased gradually
(3,21). The future goal should focus on
accurately predicting ovarian cancer-associated miRNA target genes,
studying the specific mechanism, and solving clinical diagnosis,
treatment and prognosis evaluation-associated problems. The
treatment perspective of cancer chemotherapy resistance with miRNA
as a target is very wide. The studies on miRNA as a clinically
therapeutic target are still in their initial stages. Since 1998,
increasing attention has been paid to miRNA and the potential
therapeutic effect of the corresponding exogenous small interfering
RNA (22). miRNA treatment includes
miRNA that substitutes low expression and miRNA that inhibits
overexpression. Previous studies have used agomirs and antagomirs
as analogues and inhibitors, respectively, of miRNAs for the
treatment of cancer, and a large number of experiments in
vivo have been conducted (23–27).
In conclusion, the present study confirmed that
miRNA-30a-5p played a role in the drug-resistant mechanism of
ovarian cancer. Future miRNA-30a-5p expression analysis may become
an effective tool for predicting the effect of ovarian cancer
chemotherapy. The mechanism of miRNA-30a-5p-mediated regulation of
ovarian cancer drug resistance should be further investigated.
Further studies will greatly promote the practical applications of
miRNA in the prevention, diagnosis and treatment of ovarian cancer,
which may provide a more broad application prospect in ovarian
cancer-associated miRNA clinical studies.
References
|
1
|
Greenlee RT, Hill-Harmon MB, Murray T and
Thun M: Cancer statistics, 2001. CA Cancer J Clin. 51:15–36. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Agarwal R and Kaye SB: Ovarian cancer:
Strategies for overcoming resistance to chemotherapy. Nat Rev
Cancer. 3:502–516. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Iorio MV, Visone R, Di Leva G, Donati V,
Petrocca F, Casalini P, Taccioli C, Volinia S, Liu CG, Alder H, et
al: MicroRNA signatures in human ovarian cancer. Cancer Res.
67:8699–8707. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Li L, Sun X, Wang X and Ding C: WITHDRAWN:
MicroRNA-200c and microRNA-141 as potential diagnostic and
prognostic biomarkers for ovarian cancer. Biomed Pharmacother: pii:
S0753-S3322. 00213-3. 2014. View Article : Google Scholar
|
|
5
|
Banno K, Yanokura M, Iida M, Adachi M,
Nakamura K, Nogami Y, Umene K, Masuda K, Kisu I, Nomura H, et al:
Application of microRNA in diagnosis and treatment of ovarian
cancer. Biomed Res Int. 2014:2328172014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu L, Zou J, Wang Q, Yin FQ, Zhang W and
Li L: Novel microRNAs expression of patients with chemotherapy
drug-resistant and chemotherapy-sensitive epithelial ovarian
cancer. Tumour Biol. 35:7713–7717. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Clop A, Marcq F, Takeda H, Pirottin D,
Tordoir X, Bibé B, Bouix J, Caiment F, Elsen JM, Eychenne F, et al:
A mutation creating a potential illegitimate microRNA target site
in the myostatin gene affects muscularity in sheep. Nat Genet.
38:813–818. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sorrentino A, Liu CG, Addario A, Peschle
C, Scambia G and Ferlini C: Role of microRNAs in drug-resistant
ovarian cancer cells. Gynecol Oncol. 111:478–486. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Singh SR and Rameshwar P: MicroRNA in
Development and in the Progression of Cancer (1st). Springer. New
York City, NY: 2014. View Article : Google Scholar
|
|
10
|
Kinose Y, Sawada K, Nakamura K and Kimura
T: The role of microRNAs in ovarian cancer. Biomed Res Int.
2014:2493932014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kan CW, Howell VM, Hahn MA and Marsh DJ:
Genomic alterations as mediators of miRNA dysregulation in ovarian
cancer. Genes Chromosomes Cancer. 54:1–19. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Li Y, Yao L, Liu F, Hong J, Chen L, Zhang
B and Zhang W: Characterization of microRNA expression in serous
ovarian carcinoma. Int J Mol Med. 34:491–498. 2014.PubMed/NCBI
|
|
13
|
Liu N, Zhou C, Zhao J and Chen Y: Reversal
of paclitaxel resistance in epithelial ovarian carcinoma cells by a
MUC1 aptamer-let-7i chimera. Cancer Invest. 30:577–582. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lee IH, Park JB, Cheong M, Choi YS, Park D
and Sin JI: Antitumor therapeutic and antimetastatic activity of
electroporation-delivered human papillomavirus 16 E7 DNA vaccines:
A possible mechanism for enhanced tumor control. DNA Cell Biol.
30:975–985. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nurkkala M, Wassén L, Nordström I,
Gustavsson I, Slavica L, Josefsson A and Eriksson K: Conjugation of
HPV16 E7 to cholera toxin enhances the HPV-specific T-cell recall
responses to pulsed dendritic cells in vitro in women with cervical
dysplasia. Vaccine. 28:5828–5836. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang S, Lu Z, Unruh AK, Ivan C, Baggerly
KA, Calin GA, Li Z, Bast RC Jr and Le XF: Clinically relevant
microRNAs in ovarian cancer. Mol Cancer Res. 13:393–401. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li Z, Hu S, Wang J, Cai J, Xiao L, Yu L
and Wang Z: MiR-27a modulates MDR1/P-glycoprotein expression by
targeting HIPK2 in human ovarian cancer cells. Gynecol Oncol.
119:125–130. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Luo J, Zhou J, Cheng Q, Zhou C and Ding Z:
Role of microRNA-133a in epithelial ovarian cancer pathogenesis and
progression. Oncol Lett. 7:1043–1048. 2014.PubMed/NCBI
|
|
19
|
Zong C, Wang J and Shi TM: MicroRNA 130b
enhances drug resistance in human ovarian cancer cells. Tumour
Biol. 35:12151–12156. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li B, Chen H, Wu N, Zhang WJ and Shang LX:
Deregulation of miR-128 in ovarian cancer promotes cisplatin
resistance. Int J Gynecol Cancer. 24:1381–1388. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Nam EJ, Yoon H, Kim SW, Kim H, Kim YT, Kim
JH, Kim JW and Kim S: MicroRNA expression profiles in serous
ovarian carcinoma. Clin Cancer Res. 14:2690–2695. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhang XY, Ding JX, Tao X and Hua KQ: FSH
stimulates expression of the embryonic gene HMGA2 by downregulating
let-7 in normal fimbrial epithelial cells of ovarian high-grade
serous carcinomas. Exp Ther Med. 5:350–354. 2013.PubMed/NCBI
|
|
23
|
Wan WN, Zhang YQ, Wang XM, Liu YJ, Zhang
YX, Que YH, Zhao WJ and Li P: Down-regulated miR-22 as predictive
biomarkers for prognosis of epithelial ovarian cancer. Diagn
Pathol. 9:1782014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chen S, Chen X, Xiu YL, Sun KX, Zong ZH
and Zhao Y: MicroRNA 490-3P enhances the drug-resistance of human
ovarian cancer cells. J Ovarian Res. 7:842014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhu CL and Gao GS: miR-200a overexpression
in advanced ovarian carcinomas as a prognostic indicator. Asian Pac
J Cancer Prev. 15:8595–8601. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhao H, Liu S, Wang G, Wu X, Ding Y, Guo
G, Jiang J and Cui S: Expression of miR-136 is associated with the
primary cisplatin resistance of human epithelial ovarian cancer.
Oncol Rep. 33:591–598. 2015.PubMed/NCBI
|
|
27
|
Li L, He L, Zhao JL, Xiao J, Liu M, Li X
and Tang H: miR-17-5p up-regulates YES1 to modulate the cell cycle
progression and apoptosis in ovarian cancer cell lines. J Cell
Biochem. 116:1050–1059. 2015. View Article : Google Scholar : PubMed/NCBI
|