Introduction
Osteomas are benign neoplasms consisting of mature
normal osseous tissue (1). Osteomas
of the head often arise from the periosteum of the skull, sinuses
and mandible (1). Intracranial
osteomas are rare, and usually arise from the inner table of the
skull (1). Intracranial osteomas
completely unrelated to osseous tissues are extremely rare, and are
classified into intraparenchymal osteomas and dural osteomas
(1). Despite a series of 10 autopsy
cases of dural osteomas, the clinical features and surgical
strategy remain unclear (2). The
present report describes a rare surgical case of intracranial
osteoma arising from the falx, and discusses the clinical features,
intraoperative findings and management strategy of this
disease.
Case report
In March 2014, a 40-year-old female was admitted to
Teishinkai Hospital (Hokkaido, Japan) due to persistent headache.
On admission, neurological examination revealed no abnormalities.
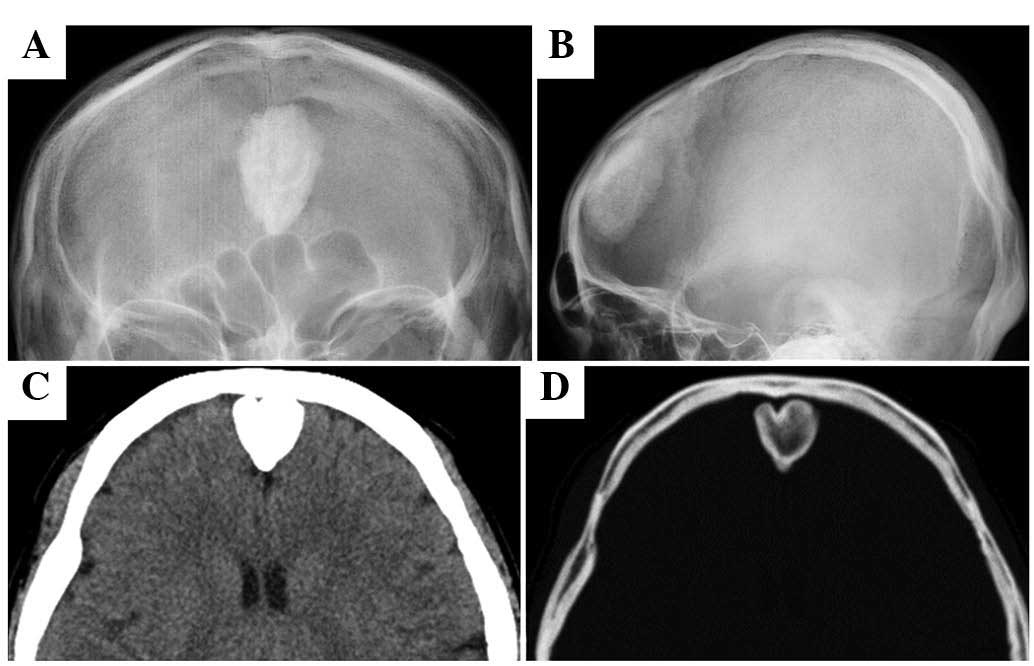
Skull radiography revealed a radiopaque lesion in the frontal area
(Fig. 1A and B), while computed
tomography (CT) and bone window CT revealed an ossified lesion in
the frontal area (Fig. 1C and D).
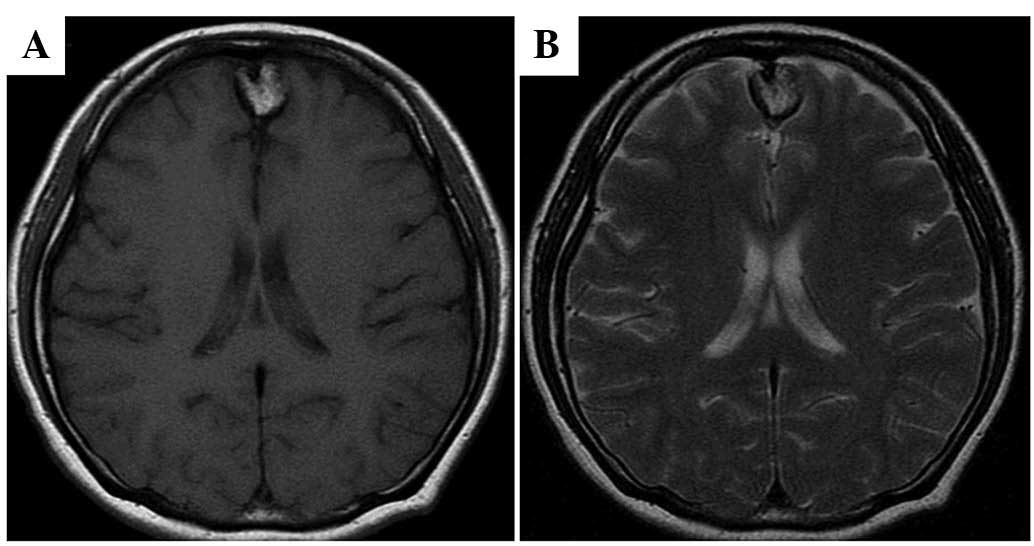
Magnetic resonance imaging revealed a mass appearing as
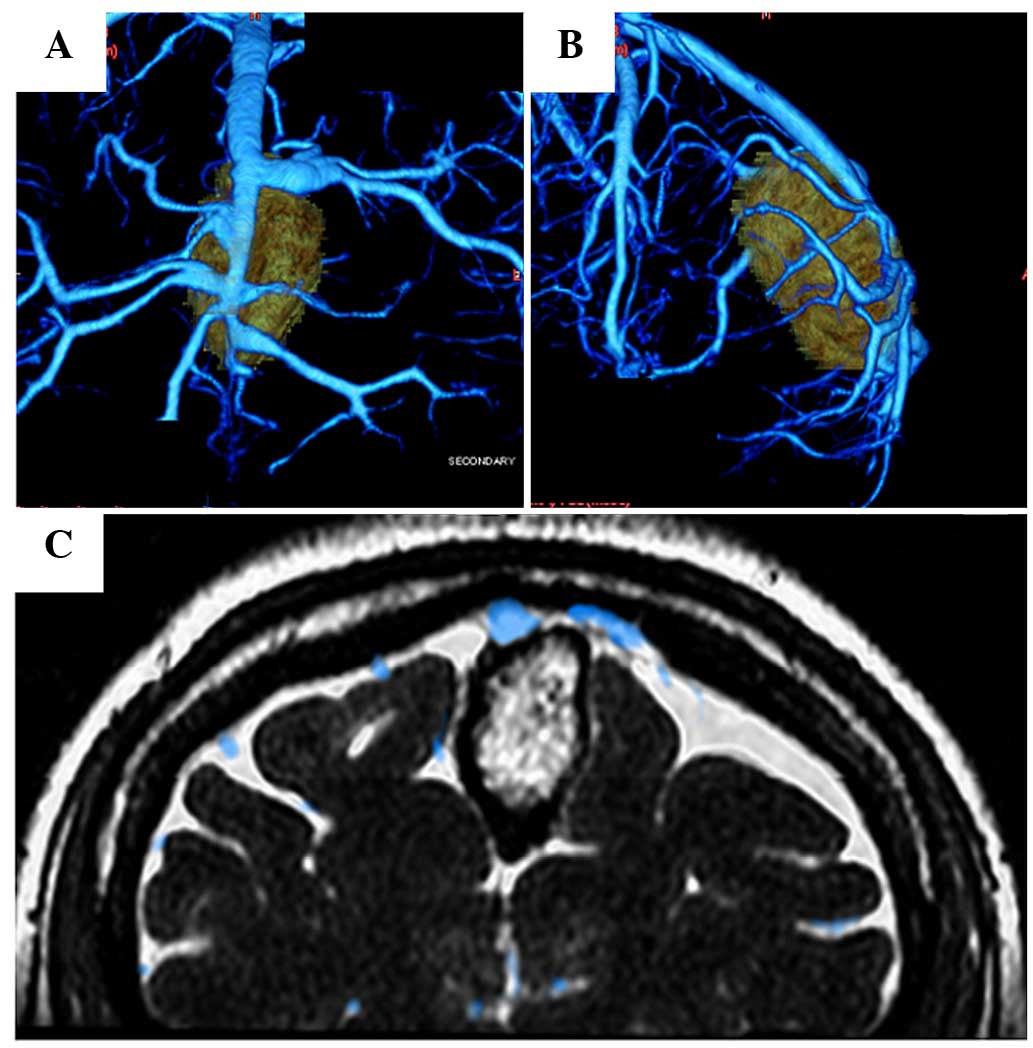
hyperintense on both T1- and T2-weighted images (Fig. 2). Three-dimensional CT venography
(Fig. 3A and B) and fast imaging
employing steady-state acquisition (FIESTA)/CT venography fusion
imaging (Fig. 3C) demonstrated that
the mass was located just below the superior sagittal sinus and
cortical veins, and had adhered partially to these veins. The
provisional diagnosis was calcified falx meningioma or osteoma
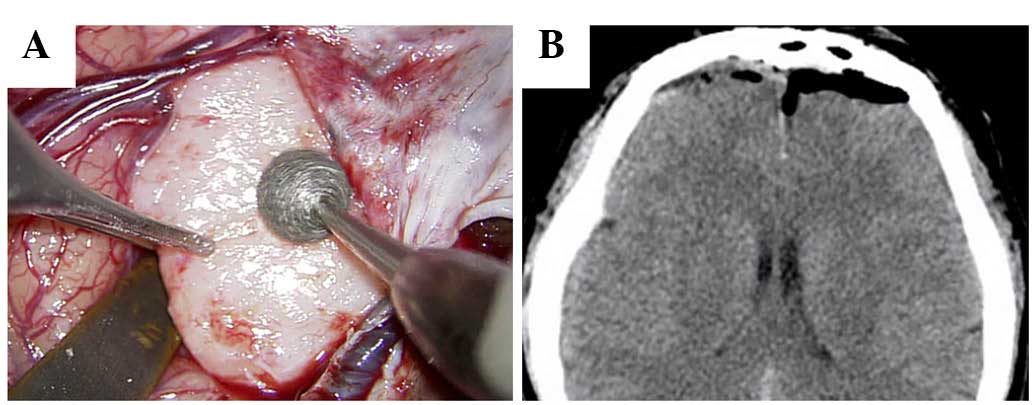
originating from the falx. Bilateral frontal craniotomy was
performed. Opening of the dura revealed that the mass was attached
to the falx in the mesial frontal lobes extra-axially, without
dural attachment. The hard bony mass was removed with a drill and a
rongeur (Fig. 4A). The cortical veins
and superior sagittal sinus were preserved completely.
Postoperative CT demonstrated complete tumor resection without
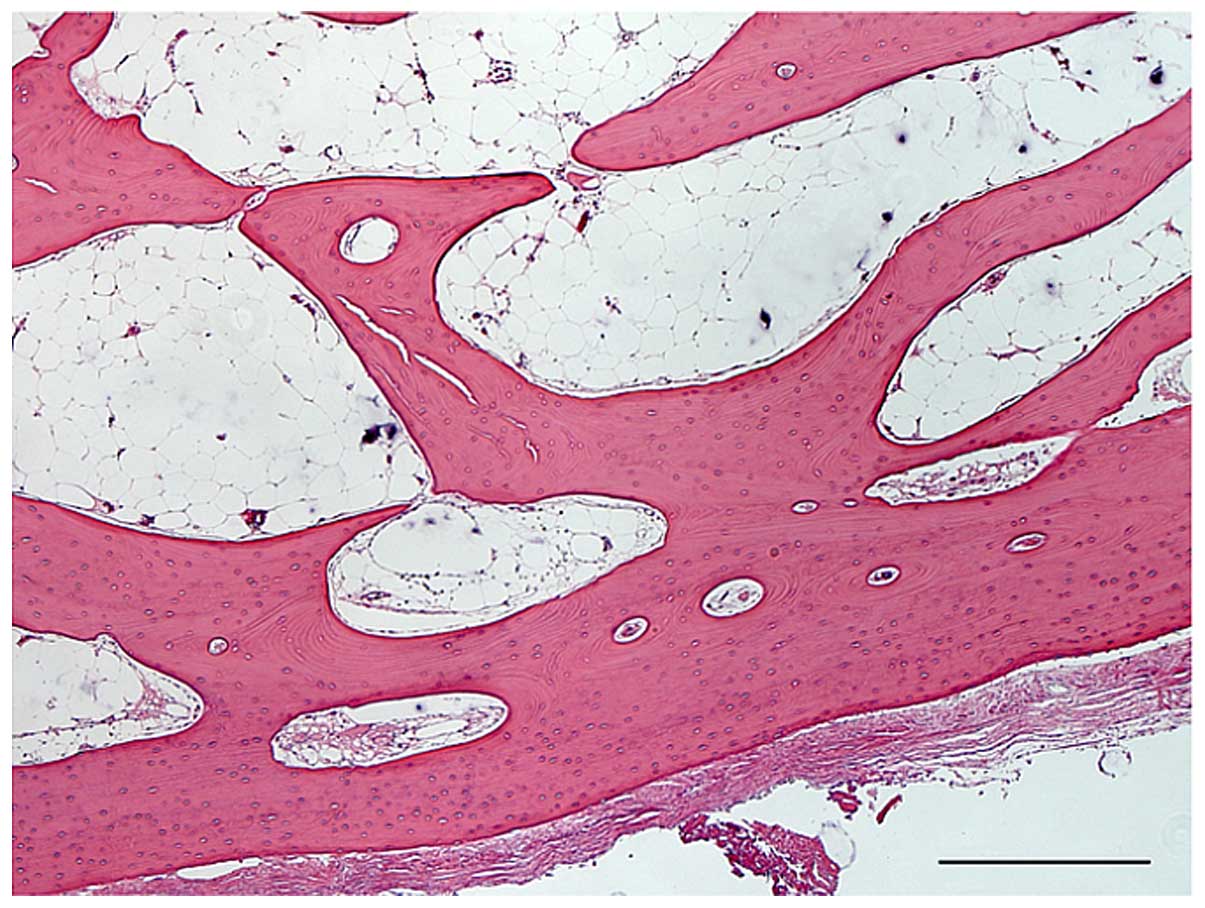
complication (Fig. 4B). Histological
examination (hematoxylin and eosin staining) revealed lamellated
bony trabeculae lined with osteoblasts, and the intertrabecular
marrow spaces occupied by adipose tissue. These findings are
compatible with osteoma (Fig. 5). The
postoperative course was uneventful, and the symptoms disappeared
after surgery. The patient was discharged 12 days after surgery
without neurological deficit. The patient was followed up for 12
months without any recurrence.
Written informed consent was obtained from the
patient for publication of the present case report and any
accompanying images.
Discussion
Intracranial osteomas are rare, with only 12
surgical cases of osteomas without association with the bone being
reported in the literature so far, including the present case, as
summarized in Table I (3–13). The
male to female ratio was 1:2, and the age of the patients was 16–64
years (mean, 39.8 years). The most common symptom was headache,
which occurred in 8 of the 12 cases. The tumors were described as
‘completely surrounded by cerebral tissue’, with ‘no connections
with the dura or the skull’, or ‘covered with the arachnoid
membrane’ in 5 cases. The tumors were attached to the inner dural
surface in 5 cases, and to the falx in 2 cases, indicating dural
osteomas. Therefore, the present case is the second surgical case
of intracranial osteoma originated from the falx. The outcome was
good in 10 patients, whereas 1 patient succumbed to disease. Venous
infarction developed in 1 case (10).
 | Table I.Surgical cases of intracranial osteoma
without connections with the skull. |
Table I.
Surgical cases of intracranial osteoma
without connections with the skull.
| Author (year)
(ref) | Age,
years/gender | Symptom | Location | Size | Surgical finding | Outcome |
|---|
| Vakaet et al
(1983) (3) | 16/F | Headache,
seizure | Frontal
inter-callosum | 5.0×5.0×6.0
cm3 | Completely surrounded
by cerebral tissue | Dead (postoperative
hemorrhage) |
| Choudhury et
al (1995) (4) | 20/F | Headache | Right frontal
convexity | 1.0 cm in
diameter | Attached to the inner
dural surface | Good |
| Lee and Lui (1997)
(5) | 28/F | Headache | Left frontal
convexity | 4.0×2.5×0.5
cm3 | Covered with
arachnoid membrane | Good |
| Aoki et al
(1998) (6) | 51/F | Headache | Right frontal
convexity | 1.1×1.5×0.7
cm3 | Partially adherent to
the inner dural surface | Good |
| Sugimoto et al
(2001) (7) | 35/M | Vertigo | Right frontal
convexity | 5.0×5.0×2.0
cm3 | Attached to the inner
dural surface | Not described |
| Cheon et al
(2002) (8) | 43/F | Headache | Left frontal
convexity | 1.2×2.0×0.7
cm3 | Attached to the inner
dural surface | Good |
| Pau et al
(2003) (9) | 33/F | None | Left frontal
convexity | 3.0×2.0×2.0
cm3 | No connections with
the dura | Good |
| Akiyama et al
(2005) (10) | 24/M | Headache | Right frontal
convexity | Not described
(multiple) | Covered with
arachnoid membrane | Good (venous
infarction) |
| Jung et al
(2007) (11) | 60/M | Headache | Right frontal
convexity | Not described | Attached to the inner
dural surface | Good |
| Barajas et al
(2012) (12) | 63/F | Altered mental
status | Right middle cranial
fossa | 4.5×3.7×2.5
cm3 | No connections with
the dura | Good |
| Chen et al
(2013) (13) | 64/M | Tinnitus,
dizziness | Right mesial frontal
lobe | 2.5×2.0×2.0
cm3 | Attached to the
falx | Good |
| Present case
(2016) | 40/F | Headache | Interhemispheric
space | 2.2×1.7×2.5
cm3 | Attached to the
falx | Good |
Intracranial osteoma usually has a wide base and
grows inward as an expanding mass with a well-defined border
(4). The present case occurred as a
nodule with a narrow neck attached to the falx, similar to a
previous case (13). The pathogenesis
of osteoma without bone involvement is still unknown. In the
present case, new bone generation from the falx is a possible
cause, since the meninges may function as the periosteum of the
inner table of the skull (2,5,8). A history
of head trauma has been noted in patients with intracranial
osteomas. Therefore, head trauma may be one of the trigger
mechanisms of intracranial osteoma (14); however, the present patient had no
such history.
No standardized treatment algorithm has been
established for this condition. If the patient is asymptomatic,
conservative therapy is one of the choices, since the natural
history of intracranial osteomas is more benign than that of
osteomas of the frontal sinuses (3).
The present patient complained of intractable headache, which could
be resolved by surgical tumor removal, since such pain is
considered to be due to irritation and compression of the adjacent
dural membrane (10). Therefore,
surgery was performed in the present case, and the pain disappeared
completely.
Surgeons should pay particular attention to possible
adhesion of intracranial osteoma to the blood vessels. In a
previous case, the osteoma had adhered tightly to the superficial
cortical veins, which were sacrificed, thus leading to
postoperative venous congestion (10). In the present case, preoperative
FIESTA/CT venography fusion imaging was very useful to demonstrate
that the mass was located just below the superior sagittal sinus
and cortical veins, and had adhered partially to these veins.
Complete preservation of these structures was carefully achieved
during surgery. Reconstruction via saphenous vein graft and patch
is recommended if the superior sagittal sinus or cortical vein is
injured (15,16).
In conclusion, the present case of intracranial
osteoma originating from the falx was successfully treated
surgically. Preoperative FIESTA/CT venography fusion imaging was
very useful to demonstrate adhesion between the mass and the
superior sagittal sinus and cortical veins.
Glossary
Abbreviations
Abbreviations:
|
CT
|
computed tomography
|
|
FIESTA
|
fast imaging employing steady-state
acquisition
|
References
|
1
|
Haddad FS, Haddad GF and Zaatari G:
Cranial osteomas: Their classification and management. Report on a
giant osteoma and review of the literature. Surg Neurol.
48:143–147. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fallon MD, Ellerbrake D and Teitelbaum SL:
Meningeal osteomas and chronic renal failure. Hum Pathol.
13:449–453. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vakaet A, De Reuck J, Thiery E and vander
Eecken H: Intracerebral osteoma: A clinicopathologic and
neuropsychologic case study. Childs Brain. 10:281–285.
1983.PubMed/NCBI
|
|
4
|
Choudhury AR, Haleem A and Tjan GT:
Solitary intradural intracranial osteoma. Br J Neurosurg.
9:557–559. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lee ST and Lui TN: Intracerebral osteoma:
Case report. Br J Neurosurg. 11:250–252. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Aoki H, Nakase H and Sakaki T: Subdural
osteoma. Acta Neurochir (Wien). 140:727–728. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sugimoto K, Nakahara I, Nishikawa M,
Tanaka M, Terashima T, Yanagihara H and Hayashi J: Osteoma
originating in the dura: A case report. No Shinkei Geka.
29:993–996. 2001.(In Japanese). PubMed/NCBI
|
|
8
|
Cheon JE, Kim JE and Yang HJ: CT and
pathologic findings of a case of subdural osteoma. Korean J Radiol.
3:211–213. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pau A, Chiaramonte G, Ghio G and Pisani R:
Solitary intracranial subdural osteoma: Case report and review of
the literature. Tumori. 89:96–98. 2003.PubMed/NCBI
|
|
10
|
Akiyama M, Tanaka T, Hasegawa Y, Chiba S
and Abe T: Multiple intracranial subarachnoid osteomas. Acta
Neurochir (Wien). 147:1085–1089. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jung TY, Jung S, Jin SG, Jin YH, Kim IY
and Kang SS: Solitary intracranial subdural osteoma: Intraoperative
findings and primary anastomosis of an involved cortical vein. J
Clin Neurosci. 14:468–470. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Barajas RF Jr, Perry A, Sughrue M, Aghi M
and Cha S: Intracranial subdural osteoma: A rare benign tumor that
can be differentiated from other calcified intracranial lesions
utilizing MR imaging. J Neuroradiol. 39:263–266. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen SM, Chuang CC, Toh CH, Jung SM and
Lui TN: Solitary intracranial osteoma with attachment to the falx:
A case report. World J Surg Oncol. 11:2212013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dukes HT and Odom GL: Discrete intradural
osteoma. Report of a case. J Neurosurg. 19:251–253. 1962.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hakuba A, Huh CW, Tsujikawa S and
Nishimura S: Total removal of a parasagittal meningioma of the
posterior third of the sagittal sinus and its repair by autogenous
vein graft. Case report. J Neurosurg. 51:379–382. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Murata J, Sawamura Y, Saito H and Abe H:
Resection of a recurrent parasagittal meningioma with cortical vein
anastomosis: Technical note. Surg Neurol. 48:592–595; discussion
595–597. 1997. View Article : Google Scholar : PubMed/NCBI
|