Introduction
B-cell lymphoma (BCL), unclassifiable, with features
intermediate between diffuse large BCL (DLBCL) and classical
Hodgkin's lymphoma (CHL), also known as ‘large BCL (LBCL) with
Hodgkin features’ and ‘Hodgkin-like anaplastic large cell lymphoma’
(HD-like ALCL), is a borderline lymphoma with features of LBCL and
CHL (1). These tumors are rare
aggressive lymphomas, often associated with mediastinal disease,
and similar cases have reported the peripheral lymph node groups as
a primary site (1). Occasionally,
these lymphomas may spread to the lung, liver, spleen and bone
marrow. These lymphoma are most common in young men, and the
majority of cases have been reported from Western countries, being
less common in African-American and Asian populations. No consensus
exists regarding the optimum treatment for this tumor. The present
study reports the case of patient with one such lymphoma that
occurred in the spleen.
Case report
A 48-year-old female Chinese patient presented to
the Department of Pathology of Beijing Shijitan Hospital (Beijing,
China) on May 2013 with light pain in the upper left abdomen that
had lasted for 1 year. The pain did not radiate to the shoulders
and back and the pain worsened when the patient was tired or
changed position. The patient demonstrated no B symptoms, including
fever, night sweats or weight loss. On investigation, the complete
blood count (CBC) and the bone marrow biopsy of the patient were
normal, and the liver and renal functions were within the normal
range. The ultrasound and computed tomography (CT) scans showed
splenomegaly without hepatomegaly, and a focal mass in the spleen.
A CT scan revealed movable enlarged lymph nodes in left neck and
bilateral inguinal folds, which measured 3 and 4 cm in diameter,
respectively, and were not accompanied by pain or fever. The
patient had previously received a uterectomy due to the presence of
a uterine leiomyoma half a year prior to presentation.
The patient underwent a full splenectomy for
diagnosis on May 2013. Intra-operatively, the spleen was found to
be enlarged and congested, and one polar adhered to pancreas.
Macroscopically, the spleen measured 14.5×11.5×8.5 cm and was 602 g
in mass. A solitary mass with scalloped margins and a grayish-white
color was located at one end of the spleen and involved the splenic
capsule.
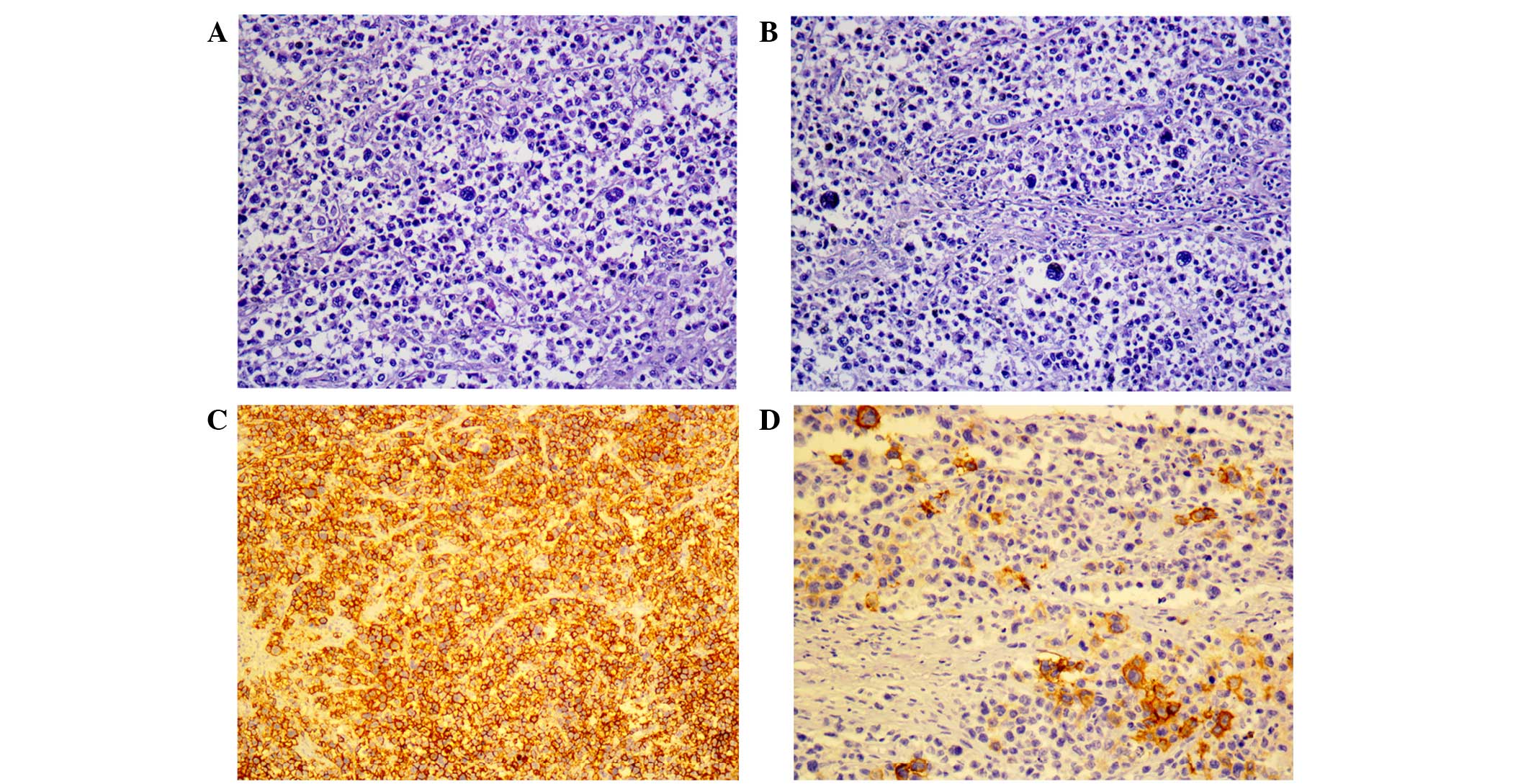
The surgical specimen was fixed by 4% neutral
formaldehyde, and subjected to paraffin embedding, conventional
sectioning and hematoxylin and eosin staining. The
histopathological sections revealed that the tumor was composed of
large atypical pleomorphic lymphoid cells with prominent nuclei and
open chromatin, and collagen bands (Fig.
1A). Lacunar, Hodgkin and multinuclear giant cells were also
present among large atypical cells, scattered lymphocytes,
eosinophilic granulocytes, neutrophile granulocytes and histocytes
(Fig. 1B). Immunohistochemical (IHC)
examination was performed using the EnVision method with FLEX
Ready-to-Use and Autostainer Link Solution for IHC (Dako, Glostrup,
Denmark). Table I contains detailed
information about the antibodies used for the analysis, which were
purchase from Dako. By IHC, the large atypical lymphoid, Hodgkin
and multinuclear giant cells were positive for cluster of
differentiation (CD)20, CD79α, melanoma associated antigen
(mutated) 1 (MUM1), BCL6, CD15 and CD30 (Fig. 1C-F), but negative for CD3, CD10,
anaplastic lymphoma receptor tyrosine kinase (ALK) and CD45RO.
These tumor cells demonstrated a negative reaction in the
Epstein-Barr virus (EBV)-encoded small RNA assay (EBV kit;
catalogue number ISH-5021; OriGene Technologies, Inc., Rockville,
MD, USA). Polymerase chain reaction (PCR) analysis was conducted
with IdentiClone™ IGH Gene Clonality Assay (catalogue number
9-101-0020; Invivoscribe Technologies, Inc., San Diego, CA, USA)
under the following cycling conditions: Denaturation at 95°C for 7
min, followed by 35 cycles of 95°C for 45 sec, 60°C for 45 sec and
72°C for 90 sec and a final extension at 72°C for 10 min. The PCR
results demonstrated a clonal rearrangement of the genes coding for
immunoglobulin (Ig) heavy chains.
 | Table I.Antibodies used for
immunohistochemistry. |
Table I.
Antibodies used for
immunohistochemistry.
| Antibody target
antigen | Characteristics | Catalogue number |
|---|
| CD3 | Polyclonal rabbit
anti-human | IR503 |
| CD20 | Monoclonal mouse
anti-human | IR604 Clone L26 |
| CD30 | Monoclonal mouse
anti-human | IR602 Clone
Ber-H2 |
| CD15 | Monoclonal mouse
anti-human | IR062 Clone
Carb-3 |
| CD10 | Monoclonal mouse
anti-human | IR648 Clone 56C6 |
| CD79a | Monoclonal mouse
anti-human | IR621 Clone
JCB117 |
| CD45RO | Monoclonal mouse
anti-human | IR751 Clone
2B11+PD7/26 |
| BCL2 | Monoclonal mouse
anti-human | IR614 Clone 124 |
| BCL6 | Monoclonal mouse
anti-human | ir625 clone
pg-b6p |
| ALK | Monoclonal Rabbit
Anti-Human | CD246 |
Based on these findings, the patient was diagnosed
with splenic LBCL, with features between DLBCL and CHL. Following
diagnosis, the patient received 7 cycles of the CHOP regimen,
consisting of 1 g cyclophosphamide (day 1), 80 mg pirarubicin (day
1), 4 mg vindesine (day 1) and 15 mg dexamethasone (days 1–5), and
she has been in good general condition and tumor-free for 17
months.
The patient, who is currently under follow-up,
provided written informed consent for the publication of the
present case report.
Discussion
Common lymphomas that have been reported in the
spleen include DLBCL, marginal zone BCL, Hodgkin's lymphoma,
follicular lymphoma and the rare type of lymphoma reported in the
present study (2–7). The current classification of lymphoid
neoplasms is based on clinical information, morphology,
immunophenotype and molecular genetic characteristics (1–6). Despite
technical and scientific progress, certain aggressive BCLs with
features that overlap two types of lymphoma remain a challenge to
classify. The updated 2008 World Health Organization classification
of Tumours of the Hematopoietic and Lymphoid Tissues has addressed
this problem by creating two novel provisional categories of BCLs:
Unclassifiable, i) with features intermediate between DLBCL and
CHL; or ii) with features intermediate between DLBCL and Burkitt's
lymphoma (1). The former is the
lymphoma reported in the present study, and is a B lineage lymphoma
that demonstrates overlapping clinical, morphological and
immunophenotypical features, between CHL and DLBCL. These lymphomas
are most common in young men, and the majority of cases reported
have been from Western countries (1).
These are rare aggressive lymphomas that are often associated with
mediastinal disease; similar cases have been reported that show the
peripheral lymph node groups as a primary site, and the tumors are
rarely found in the spleen (6,8,9). The present patient is a 48-year-old
Chinese woman and the lymphoma occurred in spleen.
The present patient had no severe complications and
underwent a splenectomy. Pathology showed that the lymphoma was
composed of a confluent, sheet-like growth of pleomorphic tumor
cells in a diffusely fibrotic stroma. The cells were larger and
more pleomorphic compared with typical cases of DLBCL, and a few
centroblast-like cells were present. Pleomorphic cells resembling
lacunar cells and Hodgkin cells comprised the majority of the
infiltrate. Scattered eosinophils, lymphocytes and histocytes were
present and the necrotic regions did not contain neutrophilic
infiltrates. According to IHC, the lymphoma cells expressed CD45,
CD20, CD79a, MUM1, Bcl6, CD30 and CD15, but not CD3, CD10, ALK or
CD45RO. These tumor cells can often be found using EBV-encoded
small RNA assays and PCR analysis, which demonstrate clonal
rearrangements of the genes coding for Ig heavy chains (8–10). No EBV
infection was identified in the present case. BCL, unclassifiable,
with features intermediate between DLBCL and CHL have a
differential diagnosis compared with with DLBCL, CHL and anaplastic
large cell lymphoma.
BCL, unclassifiable, with features intermediate
between DLBCL and CHL generally have a more aggressive clinical
course and a poorer outcome compared with CHL and DLBCL (6,9). No
consensus exists regarding the optimum treatment for the tumor;
however, certain studies propose that therapy for an aggressive
LBCL has been effective, while others propose the use of a
Hodgkin-type regimen (9,11–15).
Certain studies suggest that the transitional lymphoma is
relatively resistant to Hodgkin-based chemotherapy (9). Wang et al (16) reported 16 cases of this type of
lymphoma, the majority of which appeared to be insensitive to
immunochemotherapy (CHOP regimen), and only 4/13 cases had partial
response. Of these, 2 cases received radiotherapy subsequent to
chemotherapy and 2 cases were subjected to autologous stem cell
transplantation. In the present case report, the patient received 7
cycles of the CHOP regimen and has been in a good general condition
and tumor-free for 17 months following the splenectomy.
In conclusion, the present study reports a case of
primary splenic BCL, unclassifiable, with features intermediate
between DLBCL and HCL, which occurred in a 48-year-old Chinese
woman. This lymphoma is rarely found to occur in the spleen. The
patient has received 7 cycles of the CHOP regimen and has been
tumor-free for 17 months. The lymphoma is rare and the most
appropriate treatment remains controversial, hence additional
studies are required to analyze the best treatment plan.
References
|
1
|
Swerdlow SH, Campo E, Harris NL, Jaffe ES,
Pileri SA, Stein H, Thiele J and Vardiman JW: WHO classification of
tumours. WHO Classification of Tumours of Haematopoietic and
Lymphoid Tissues. 2:(4th). IARC Press. (Lyon). 267–268. 2008.
|
|
2
|
Iriyama N, Horikoshi A, Hatta Y, Kobayashi
Y, Sawada S and Takeuchi J: Localized, splenic, diffuse large
B-cell lymphoma presenting with hypersplenism: Risk and benefit of
splenectomy. Inter Med. 49:1027–1030. 2010. View Article : Google Scholar
|
|
3
|
Kurup SK, Levy-Clarke G, Calvo KR, Jaffe
ES, Nussenblatt RB and Chan CC: Primary diffuse large B-cell
lymphoma of the spleen with coincident serous retinal detachments
responsive to corticosteroids. Clin Experiment Ophthalmol.
35:468–472. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ding YL and Wang SY: Gastrosplenic fistula
due to splenic large B-cell lymphoma. J Res Med Sci. 17:805–807.
2012.PubMed/NCBI
|
|
5
|
Matutes E: Splenic marginal zone lymphoma:
Disease features and management. Expert Rev Hematol. 6:735–745.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Asano N, Suzuki R, Matsuo K, Kagami Y,
Ishida F, Tamaru JI, Jin GS, Sato Y, Shimoyama Y, Yoshino T, et al:
Cytotoxic molecule expression is predictive of prognosis in
Hodgkin's-like anaplastic large cell lymphoma. Histopathology.
50:705–715. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kim JK, Hahn JS, Kim GE and Yang WI: Three
cases of diffuse large B-cell lymphoma presenting as primary
splenic lymphoma. Yonsei Med J. 46:703–709. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gardner RV, Velez MC, Ode DL, Lee JW and
Correa H: Gamma/delta T-cell lymphoma as a recurrent complication
after transplantation. Leuk Lymphoma. 45:2355–2359. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Travers-Glehen A, Pittaluga S, Gaulard P,
Sorbara L, Alonso MA, Raffeld M and Jaffe ES: Mediastinal gray zone
lymphoma: The missing link between classic Hodgkin's lymphoma and
mediastinal large B-cell lymphoma. Am J Surg Pathol. 29:1411–1421.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rüdiger T, Jaffe ES, Delsol G,
deWolf-Peeters C, Gascoyne RD, Georgii A, Harris NL, Kadin ME,
MacLennan KA, Poppema S, et al: Workshop report on Hodgkin's
disease and related diseases (‘gray zone’ lymphoma). Ann Oncol.
9(Suppl 5): S31–S38. 1998. View Article : Google Scholar
|
|
11
|
Portlock CS, Donnelly GB, Qin J, Straus D,
Yahalom J, Zelenetz A, Noy A, O'Connor O, Horwitz S, Moskowitz C
and Filippa DA: Adverse prognostic significance of CD20 positive
Reed-Sternberg cells in classical Hodgkin's disease. Br J Haematol.
125:701–708. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tzankov A, Krugmann J, Fend F, Fischhofer
M, Greil R and Dirnhofer S: Prognostic significance of CD20
expression in classical Hodgkin lymphoma: A clinicopanthological
study of 119 cases. Clin Cancer Res. 9:1381–1386. 2003.PubMed/NCBI
|
|
13
|
Grant C, Dunleavy K, Eberle FC, Pittaluga
S, Wilson WH and Jaffe ES: Primary mediastinal large B-cell
lymphoma, classic Hodgkin lymphoma presenting in the mediastinum,
and mediastinal gray zone lymphoma: What is the oncologist to do?
Curr Hematol Malig Rep. 6:157–163. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dunleavy K, Grant C, Eberle FC, Pittaluga
S, Jaffe ES and Wilson WH: Gray zone lymphoma: Better treated like
Hodgkin lymphoma or mediastinal large B-cell lymphoma? Curr Hematol
Malig Rep. 7:241–247. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Parikh JG, Strom T and Stone I: MYC
negative rectal B-cell lymphoma, unclassifiable, with features
intermediate between diffuse large B-cell lymphoma and Burkitt's
lymphoma in an immunocompetent patient. Case Rep Pathol.
2013:3023042013.PubMed/NCBI
|
|
16
|
Wang L, Wang W, Li X, Guo Y and Zhu X:
Grey zone lymphoma with features intermediate between diffuse large
B-cell lymphoma and classical Hodgkin lymphoma: Clinicopathologic
characterization of 16 cases showing different patterns. Zhonghua
Bing Li Xue Za Zhi. 43:307–312. 2014.(In Chinese). PubMed/NCBI
|