Introduction
Chondrosarcoma is a malignant tumor characterized by
the formation of cartilage by tumor cells (1). Chondrosarcomas have been widely reported
in the literature and may arise in any region where cartilage is
present (2). In total, 5–12% of
chondrosarcomas occur in the head and neck region, accounting for
5–10% of all bone neoplasms occurring in this location; the larynx
and maxillo-nasal region are the most common sites for
chondrosarcomas to originate (3).
Chondrosarcomas located in the mandible region are rare and mostly
occur in the mandibular symphyseal region (4–6). The
majority of chondrosarcomas exhibit an indolent growth pattern, and
more aggressive, high-grade tumors have been previously observed
(7). Forming a pre-operative
diagnosis for chondrosarcomas is challenging due to the atypical
symptoms and imaging manifestations; therefore, diagnosis primarily
depends on the post-operative pathological examination. To date,
the clinical course, histogenesis, cytogenetics and prognosis for
chondrosarcomas remain largely unknown (8). The treatment for the tumor depends on
the outcome of surgical resection, and the prognosis for patients
with chondrosarcomas is good when the tumors are completely
resected (9). The occurrence of
chondrosarcoma in the mental foramen region of the mandible is an
exceptional event. The present study describes the case of a
patient with chondrosarcoma in the right mental foramen region of
the mandible. Written informed consent was obtained from the
patient for the publication of the present study.
Case report
An 18-year-old man was referred to Jining First
People's Hospital (Jining, China) in December 2009 with swelling
over the labial aspect of the right mandible that had occured for
~3 months. The swelling had increased gradually in size during that
period. The patient did not have a history of trauma or pain, but
reported that the anterior mandible felt swollen and that there was
a slight loosening of the lower anterior teeth.
Extraoral examination demonstrated no sign of facial
swelling or asymmetry. No lymph node involvement was observed, and
all the cranial nerves were uninjured, since there was no facial
palsy observed. Intraoral examination revealed a swelling,
~1.5×2.0×2.0 cm in size, at the sulcus vestibularis of the lower
right canine and lateral incisor. The hard, painless mass was fixed
to the mandible and covered with normal mucosa. No swelling was
observed at the lingual aspect. The mandible swelling had caused
displacement of the crown of the lower right canine and lateral
incisor; however, the patient experienced no numbness or limitation
in mouth opening.
Panoramic radiographs revealed a radiolucent lesion
with irregular bone diffusion, which displaced the roots of the
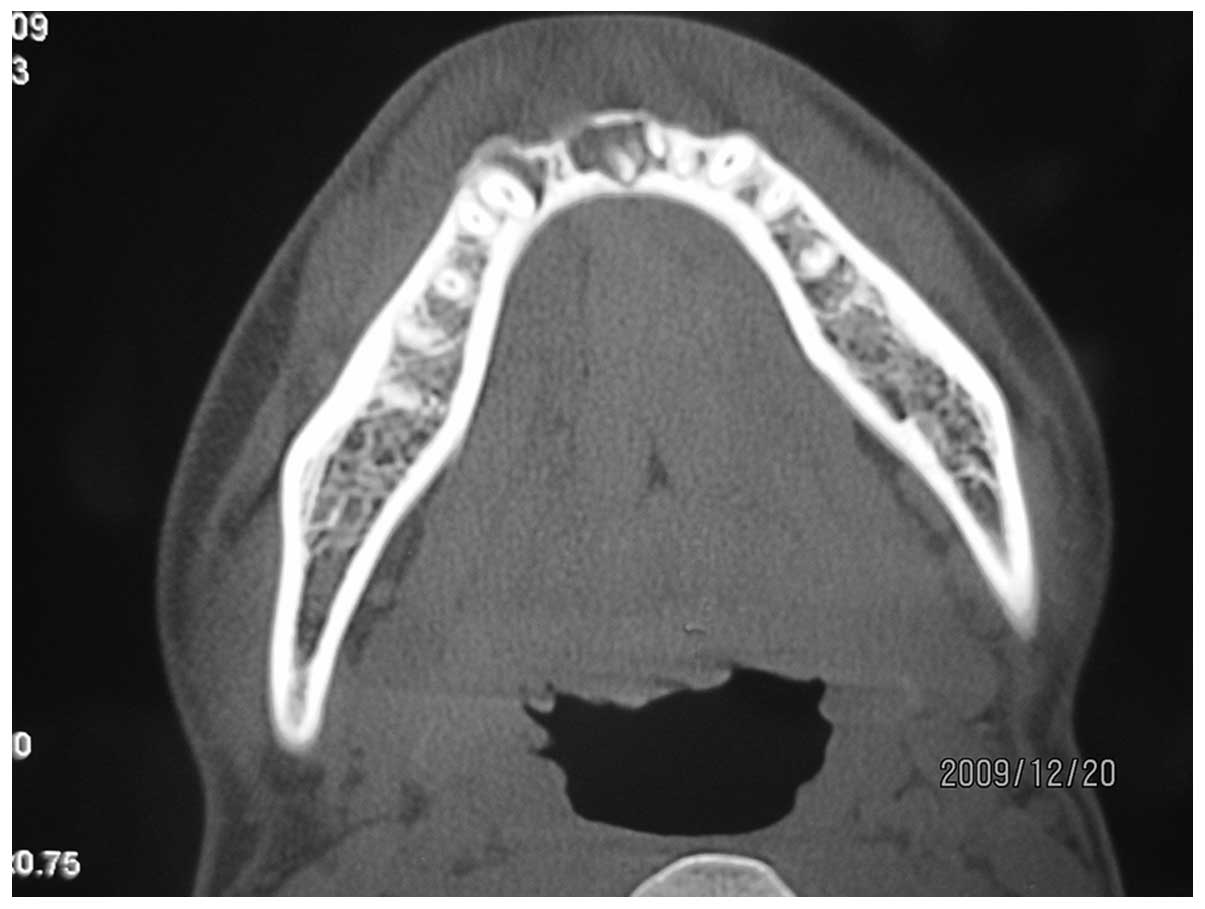
lower right canine and lateral incisor. Next, 64-multidetector-row
computed tomography (CT) (Somatom Definition AS; Siemens Medical
Solutions, Forchheim, Germany) demonstrated bone absorption around
the roots of the lower central and lateral incisors, and a widening
of the parodontium (Fig. 1).
Three-dimensional imaging (Somatom Definition AS; Siemens Medical
Solutions) revealed that there was destruction of the bone at the
right mental foramen region of the mandible (Fig. 2).
The patient was advised to undergo surgery, and the
tumor was resected by segmental mandibulectomy between the lower
right first molar and the lower left first premolar. The defect in
the mandible was reconstructed with a free vascularized fibula
flap.
Resected tissue specimens were formalin-fixed,
paraffin-embedded, cut into 5-µm sections and stained with
hematoxylin and eosin (Sigma-Aldrich, St. Louis, MO, USA).
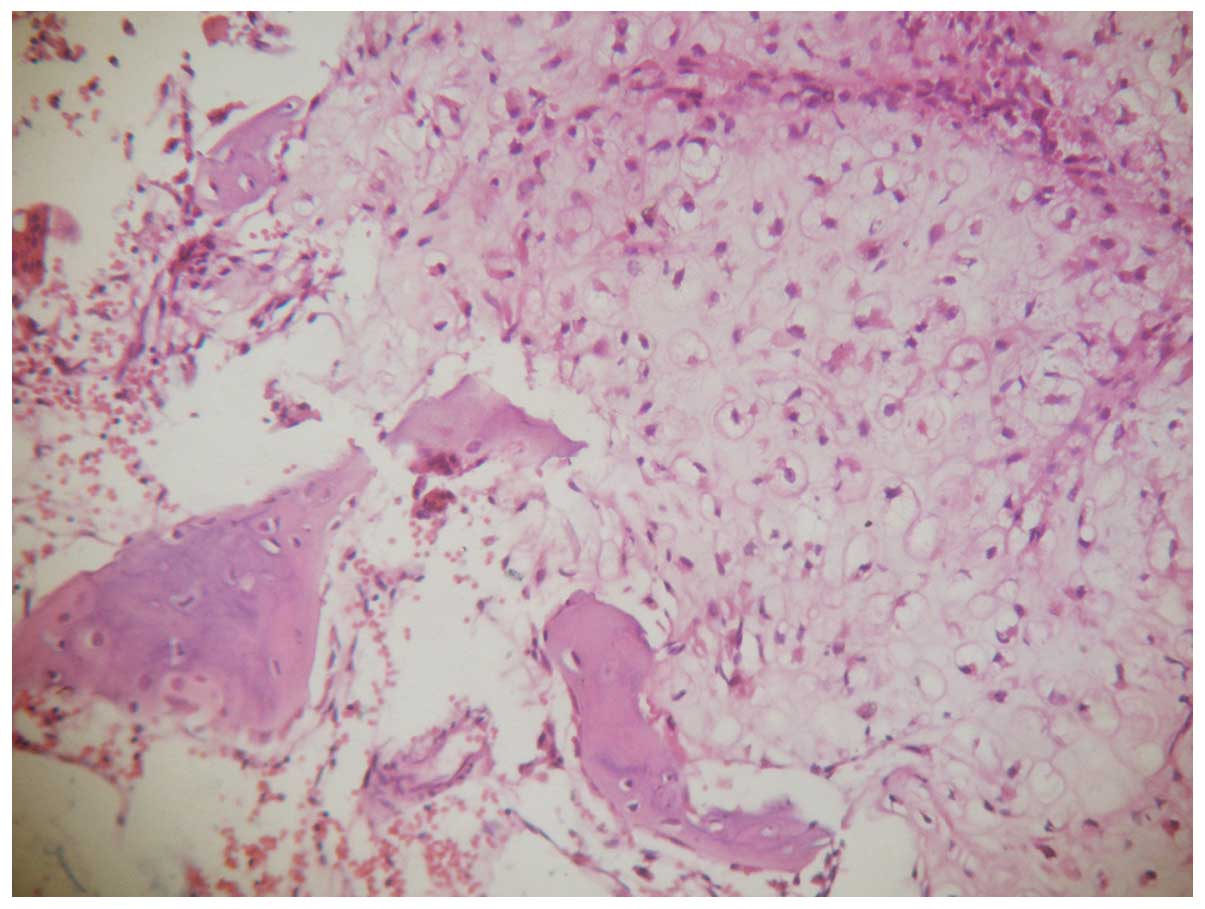
Post-operative histopathological examination of the mandibular
lesion demonstrated that the lesion was a neoplasm composed of
lobular cartilage cell clumps, which had invaded the surrounding
tissue. Under low magnification (×40), the tumor cells were
lobulated with rich chondromyxoid stroma. The tumor cells were
basophilic and infiltrated the surrounding normal bone tissue.
Under high magnification (×200), the tumor cells were abundant and
of various sizes. The nuclei of the cells were enlarged and were
heavily stained, with moderate heterotypical alterations compared
with normal cells. Binuclear cells were rarely observed (Fig. 3). Cobas® CORE II Automated
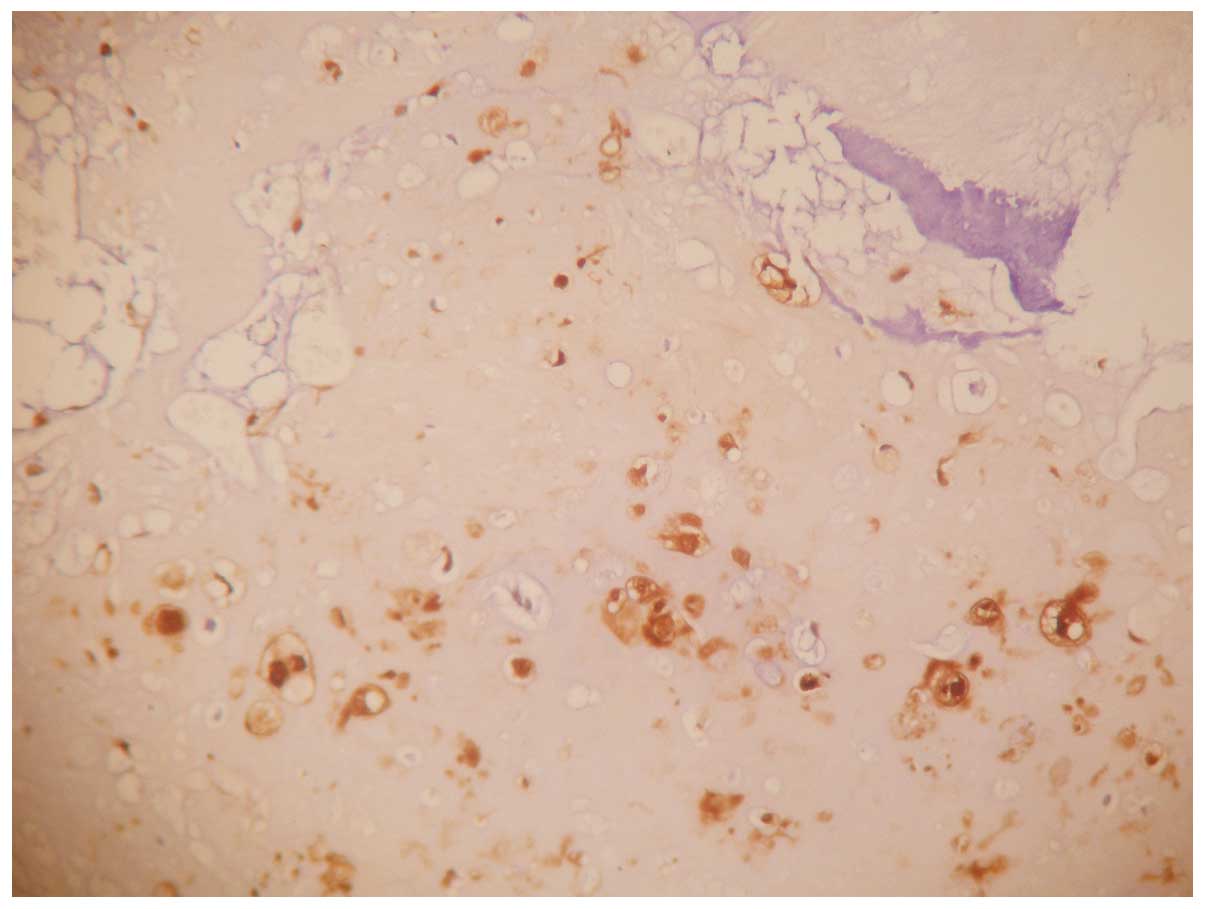
Immunity System (Roche Diagnostics GmbH, Mannheim, Germany) was
used to quantitatively detect the levels of the S-100 protein. The
slides were blocked with 10% goat serum (ZSGB-BIO, Beijing, China)
for 30 min, then incubated with mouse anti-human monoclonal S-100
antibody (cat. no. Kit-0007; dilution, 1:100; Fuzhou Maixin
Biotechnology Co., Ltd., Fuzhou, China). Immunohistochemistry
demonstrated that 80% of the tumor cells exhibited S-100 protein
(Fig. 4). A diagnosis of grade II
chondrosarcoma was provided as a result (10).
The post-operative course was uneventful and the
patient was not referred for radiation therapy, since all margins
of the resected region were tumor-free. Post-treatment follow-up
evaluations every 6 months indicated no evidence of recurrence 3
years following surgery, as observed by CT. There was no evidence
of recurrence 3 years after surgery, and the patient continues to
undergo routine follow-up examinations.
Discussion
Chondrosarcoma accounts for ~11% of all primary
malignant bone tumors. The tumor is commonly observed in the pelvic
bones, the proximal femur, the proximal humerus, the distal femur
and the ribs; 5–12% of chondrosarcomas occur in the head and neck
region (11). The most common sites
for chondrosarcoma in the head and neck region have been reported
as the jaw bones, paranasal sinuses, nasal cavity, maxilla and
vertebrae (3,12,13). The
occurrence of chondrosarcoma in the mandible is rare. The molar
region and, in decreasing order, the symphysis and the coronoid
process may be involved, but occurrence in the mental foramen
region is extremely uncommon (12,14).
Chondrosarcoma in the mandible is characterized by the presence of
a swelling mass with or without pain, loosening and displacement of
involved teeth, and widening of the parodontium (4). Clinical features, including loss of
nerve sensation and dysesthesia, are used to distinguish a
malignant neoplasm from osteomyelitis.
Radiographically, chondrosarcomas exhibit a range of
features consistent with their malignant nature. In general, the
margins of the lesion are ill-defined, with a holey, lytic
appearance. Radiographical findings provide a certain amount of
evidence for the diagnosis of chondrosarcoma, such as loosening of
the involved teeth and widening of the periodontal ligament space
(4).
The final diagnosis relies on histological and
immunohistochemical examination of the lesion. Low magnification
microscopy reveals a spectrum of findings, which are similar to
those of chondrosarcomas located in other regions of the body. The
lesions appear lobulated and infiltrate the surrounding normal bone
tissue. Under high magnification microscopy, the tumor cells
exhibit a hyaline cartilaginous proliferation, with a sarcomatous
stroma containing stellate, spindle-shaped or round cells. Cell
nuclei are enlarged, heavily stained and have moderate
heterotypical alterations. The presence of binuclear cells is rare.
Immunohistochemical analysis demonstrates that tumor cells express
the S-100 protein. The study by Evans et al (10) classified chondrosarcoma into three
grades (I, II and III), based on the frequency of mitosis,
cellularity and the dimensions of the nuclei. The present case was
classified as grade II chondrosarcoma. It may be difficult to
distinguish well-differentiated chondrosarcoma (grade I or II) from
a chondroma as chondrosarcomas exhibit various histological
patterns, which range from undifferentiated neoplasms to benign
chondroid tumors.
Wide surgical resection is known to be the most
effective treatment for chondrosarcoma (1). For these tumors, local recurrence is
more common than distant metastasis (15), and there is a relatively good
association between tumor grade and prognosis. Tumor grade and
resectability are the most important prognostic factors for head
and neck chondrosarcomas (9). These
factors make the early diagnosis and complete resection of the
tumor extremely important for the prognosis of the patient
(16). Radiotherapy for
chondrosarcoma is generally accepted as an adjuvant therapy in
cases of residual disease rather than as the initial treatment
(17,18).
Overall, chondrosarcoma is a malignant tumor with a
relatively low rate of lymph node involvement or distant
metastasis. Therefore, an early diagnosis and complete resection
are extremely important for a good prognosis, and elective neck
dissection is not usually required. Radiotherapy is only
recommended for adjuvant purposes when the margin is positive or
the tumor is unresectable. In the present case, the patient
underwent successfully underwent a resection only, and there was no
evidence of disease at 3 years post-surgery.
References
|
1
|
Koch BB, Karnell LH, Hoffman HT,
Apostolakis LW, Robinson RA, Zhen W and Menck HR: National cancer
database report on chondrosarcoma of the head and neck. Head Neck.
22:408–425. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Garrington GE and Collett WK:
Chondrosarcoma. I. A selected literature review. J Oral Pathol.
17:1–11. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Burkey BB, Hoffman HT, Baker SR, Thornton
AF and McClatchey KD: Chondrosarcoma of the head and neck.
Laryngoscope. 100:1301–1305. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Saini R, Abd Razak NH, Ab Rahman S and
Samsudin AR: Chondrosarcoma of the mandible: A case report. J Can
Dent Assoc. 73:175–178. 2007.PubMed/NCBI
|
|
5
|
Izadi K, Lazow SK, Solomon MP and Berger
JR: Chondrosarcoma of the anterior mandible. A case report. NY
State Dent J. 66:32–34. 2000.
|
|
6
|
Ormiston IW, Piette E, Tideman H and Wu
PC: Chondrosarcoma of the mandible presenting as periodontal
lesions: Report of 2 cases. J Craniomaxillofac Surg. 22:231–235.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Riedel RF, Larrier N, Dodd L, Kirsch D,
Martinez S and Brigman BE: The clinical management of
chondrosarcoma. Curr Treat Options Oncol. 10:94–106. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sammartino G, Marenzi G, Howard CM, Minimo
C, Trosino O, Califano L and Claudio PP: Chondrosarcoma of the jaw:
A closer look at its management. J Oral Maxillofac Surg.
66:2349–2355. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee SY, Lim YC, Song MH, Seok JY, Lee WS
and Choi EC: Chondrosarcoma of the head and neck. Yonsei Med J.
46:228–232. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Evans HL, Ayala AG and Romsdahl MM:
Prognostic factors in chondrosarcoma of bone: A clinicopathologic
analysis with emphasis on histologic grading. Cancer. 40:818–831.
1977. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Schajowicz F, Ackerman LV and Sissons HA:
Histological Typing of Bone Tumors. International Histological
Classification of Tumors (2nd). World Health Organization.
(Geneva). 1972.
|
|
12
|
Weiss WW Jr and Bennett JA:
Chondrosarcoma: A rare tumor of the jaws. J Oral Maxillofac Surg.
44:73–79. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ruark DS, Schlehaider UK and Shah JP:
Chondrosarcomas of the head and neck. World J Surg. 16:1010–1016.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hackney FL, Aragon SB, Aufdemorte TB, Holt
GR and Van Sickels JE: Chondrosarcoma of the jaws: Clinical
findings, histopathology and treatment. Oral Sur Oral Med Oral
Pathol. 71:139–143. 1991. View Article : Google Scholar
|
|
15
|
Sesenna E, Tullio A and Ferrari S:
Chondrosarcoma of the temporomandibular joint: A case report and
review of the literature. J Oral Maxillofac Surg. 55:1348–1352.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tullio G and D'Errico P: Chondrosarcoma of
the mandible. Clinical and histological considerations. Ann
Stomatol (Roma). 23:191–206. 1974.(In Italian). PubMed/NCBI
|
|
17
|
Harwood AR, Krajbich JI and Fornasier VL:
Radiotherapy of chondrosarcoma of bone. Cancer. 45:2769–2777. 1980.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
McNaney D, Lindberg RD, Ayala AG, Barkley
HT Jr and Hussey DH: Fifteen year radiotherapy experience with
chondrosarcoma of bone. Int J Radiat Oncol Biol Phys. 8:187–190.
1982. View Article : Google Scholar : PubMed/NCBI
|