Introduction
Pituitary adenoma (PA) is a benign tumor originating
in adenohypophyseal cells of the anterior lobe of the pituitary
gland (1). The classification of PAs
is based on the secretion of hormones; thus, PA can be a secreting
(functioning) or a non-secreting (non-functioning) tumor (2). According to their size, adenomas are
classified into microadenomas (≤10 mm) and macroadenomas (>10
mm) (2). Women have a 2-fold
increased risk of developing PA in comparison with men (1). Most commonly, PA is a non-malignant
tumor; however, it tends to recur (3). Usually, this tumor is soft and has no
capsule that could isolate it from the surrounding mass of
microglia (1). That is the reason why
it can grow and infiltrate the surrounding structures. Adenomas may
cause symptoms in two ways: i) Due to tumor-related hypersecretion
or hyposecretion of hormones, in which case, the tumor causes
compression to a normally functioning hypophysis; or ii) due to the
compression exerted by the PA on the surrounding structures
(2). Functionally active PAs cause
less damage to the visual function than non-functioning PAs, since
functioning PAs become symptomatic due to hormone secretion,
whereas non-functioning PAs can grow slowly, compress the optic
chiasm (which is located directly above the pituitary gland) and
cause progressive visual loss (4).
The pathogenesis of PA is complex and poorly
understood. It is considered that PA has a multifactorial etiology
that includes genetic factors that have an impact on PA development
(4,5).
Matrix metalloproteinases (MMPs) are a broad family
of zinc-binding endopeptidases that aid to degrade the
extracellular matrix, which is associated with cancer cell
invasion, metastasis and angiogenesis (5). Human MMP-14, a membrane-bound
zinc endopeptidase, is one of the most important cancer targets,
since it plays central roles in tumor growth and invasion (6). MMP-14 is a membrane-type
metalloproteinase with collagenase activity and potential roles in
numerous biological processes in both normal and cancerous tissues
(7). The majority of studies on
MMP-14 primarily focus on angiogenesis and invasion
(8,9).
In addition to invasiveness, oncogenes and tumor suppressor genes
associated with malignant transformation have received attention in
the past years.
Transforming growth factor beta (TGF-β) signaling
functions as a suppressor or a promoter in tumor development,
depending on the tumor stage and type (10,11). TGFβ
signaling is initiated by the binding of ligands (TGFβ1,
TGFβ2 and TGFβ3) to type II TGFβ receptors (TGFβ
RII), followed by the recruitment of type I TGFβ receptor (TGFβ RI)
to form the complex (12–14). Next, TGFβ RII phosphorylates TGFβ RI
to activate it (12–14). The clinical significance of TGFβ
ligands and downstream signaling mediators has been studied in
multiple types of tumors, and the results are discordant (12–14). It is
known that MMP-14 works in the activation of TGF-β1
cytokine, but the MMP-14 molecule does not directly activate
the TGFβ-1 cytokine by causing collagen degradation prior to
the involvement of thrombospondin 1 (15).
To the best of our knowledge, there are no studies
on the role of TGFβ-1 and MMP-14 in patients with PA.
Therefore, the aim of the present study is to investigate the role
of the TGF-β1 and MMP-14 signaling pathways in PA
tumor development.
Materials and methods
Subjects and ethical statement
The promoter methylation status of TGFβ-1 and
MMP-14 was analyzed in 120 PA tumor tissues. All PA tumor
samples were surgically resected in the Department of Neurosurgery,
Hospital of Lithuanian University of Health Sciences Kaunas Clinics
(Kaunas, Lithuania), and were histologically diagnosed in the
Department of Anatomical Pathology, Hospital of Lithuanian
University of Health Sciences Kaunas Clinics. PA samples were
snap-frozen in liquid nitrogen prior to DNA extraction. Approval
(no. P2-9/2003) to undertake the study was obtained from the Kaunas
Regional Biomedical Research Ethics Committee (Kaunas, Lithuania).
The study was conducted in the Departments of Ophthalmology and
Neurosurgery, Hospital of Lithuanian University of Health Sciences
Kaunas Clinics between February 2010 and May 2015. Written patient
consent under the approval of the Ethics Committee of Lithuanian
University of Health Sciences was obtained for every patient.
The inclusion criteria were as follows: i)
Determined and confirmed PA via magnetic resonance imaging (MRI);
ii) patient's general good condition; iii) patient's consent to
participate in the study; iv) patient's age ≥18 years; and v) no
other tumors localized in the brain or other organs. The following
data were determined for each patient: Age at the time of
operation, gender, promoter methylation status of the genes
TGFβ-1 and MMP-14, hormones activity and recurrence
of PA.
Invasiveness evaluation
All PAs were anatomically analyzed based on MRI
findings. PA invasiveness was confirmed by a surgeon. The
suprasellar extension and sphenoid sinus invasion by PAs were
classified according to the Wilson-Hardy classification (Hardy
classification modified by Wilson) (16). The degree of suprasellar and
parasellar extension was graded as stages A-E. The degree of sellar
floor erosion was graded as grades I–IV. Grade III, localized
sellar destruction, and grade IV, diffuse destruction, were
considered as invasive PA. The Knosp classification system was used
to quantify invasion of the cavernous sinus, in which only grades 3
and 4 define true invasion of the tumor into the cavernous sinus:
Grade 0, no cavernous sinus involvement; grades 1 and 2, the tumor
pushes into the medial wall of the cavernous sinus, but does not go
beyond a hypothetical line extending between the centres of the two
segments of the internal carotid artery (grade 1) or it goes beyond
such a line, but without passing a line tangent to the lateral
margins of the artery itself (grade 2); grade 3, the tumor extends
laterally to the internal carotid artery within the cavernous
sinus; and grade 4, total encasement of the intracavernous carotid
artery (17). Therefore, only grade
III and IV tumors were considered to be invasive.
DNA extraction and modification
Tumor DNA was extracted from 50–100 mg of frozen PA
tissue using the salting-out method (12–14). The
methylation status of the MMP-14 and TGFβ-1 genes
promoter was determined by bisulfite treatment of DNA. A total of
400 ng DNA was used for bisulfite modification, which was performed
using an EZ DNA Methylation kit (Zymo Research Corporation, Irvine,
CA, USA), according to the manufacturer's protocol.
Bisulfite-treated DNA was eluted in 40 µl distilled nuclease-free
water, and stored at −80°C until subjected to methylation
specific-polymerase chain reaction (MS-PCR).
MS-PCR
The methylation status of the TGFβ-1 and
MMP-14 promoters region was determined by MS-PCR. Primers
distinguishing unmethylated and methylated alleles were designed
using ‘MethPrimer’ (18), and their
sequences are presented in Table
I.
 | Table I.Methylation specific-polymerase chain
reaction primers. |
Table I.
Methylation specific-polymerase chain
reaction primers.
| Gene | Forward primer
5′-3′ | Reverse primer
5′-3′ |
|---|
| MMP-14 (U) |
TTTATTGAAGATAAACGTGTTTTGA |
CATAAACAAAAAAAACAAAAAACAACA |
| MMP-14 (M) |
TTTATCGAAGATAAAGGCGTTTC |
GTAAACAAAAAAAACAAAAAACAACG |
| TGFβ-1 (U) |
GTGGGTTTTTATTATTAGTATGTGG |
AAATCCTATCCAAACTACAACTCAC |
| TGFβ-1 (M) |
TTGTGGGTTTTTATTATTAGTACGC |
AAATCCTATCCAAACTACGACTCG |
MS-PCR was performed in a total volume of 15 µl,
using Maxima Hot Start Green PCR Master Mix (Thermo Fisher
Scientific, Inc., Waltham, MA, USA) with Hot Start Taq DNA
polymerase and 10 pmol of each primer (Invitrogen; Thermo Fisher
Scientific, Inc.). Each MS-PCR incorporated ~20 ng of
bisulfite-treated DNA as a template. Human blood lymphocyte DNA
treated with bisulfite served as an unmethylated DNA control, while
CpG Methylated Human Genomic DNA (Thermo Fisher Scientific, Inc.)
was used as a positive methylation control. A blank water control
was also included. The conditions for MMP-14 MS-PCR were as
follows: 95°C for 5 min, followed by 39 cycles of 95°C for 15 sec,
57°C for 30 sec and 72°C for 30 sec, and a final step at 72°C for 5
min. The conditions for TGFβ-1 gene amplification were
almost identical to those for MMP-14, with the exception of the
number of cycles (38) and the temperature used in the second step
of each cycle (60°C). The amplified products were analyzed on 2%
agarose gels with 0.5 µg/ml (final concentration) of ethidium
bromide and visualized under ultraviolet light. The presence of PCR
products of the correct molecular weight indicated the presence of
either methylated or unmethylated alleles.
Statistical analysis
For statistical analyses, SPSS version 20 (IBM SPSS,
Armonk, NY, USA) was used. Statistical analyses were conducted to
investigate the association between methylation status, age,
gender, PA tumoral activity and recurrence. Associations between
gene methylation data and clinical features of PA patients were
evaluated using the χ2 test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Characteristics of PA patients
The median age at PA diagnosis was 56.0 years, with
an age range from 18 to 84 years. The male to female ratio was
1:1.35. The median age of males (n=51) was 57.0 years and of
females (n=69) 56.0 years. The samples were divided into two
groups: Functioning (n=56) and non-functioning (n=64) PAs.
Recurrence was observed only in 12 cases out of 120 (3/56
functioning and 9/64 non-functioning) PAs. Invasiveness was
evaluated in 104 (35 non-invasive and 69 invasive) cases of PA.
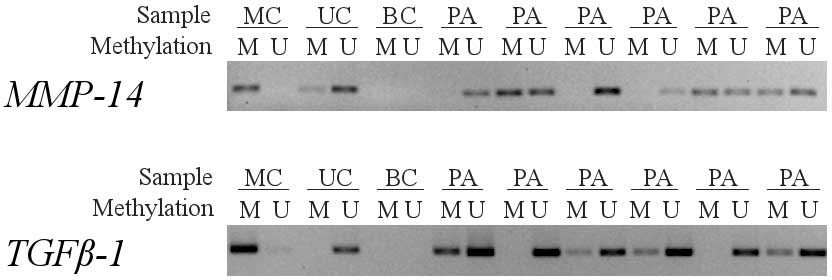
MMP-14 and TGFβ-1 gene promoter
methylation frequency in PA
The methylation status of the MMP-14 and
TGFβ-1 promoters in PA tumor samples was detected by MS-PCR.
The methylation status of the MMP-14 and TGFβ-1
promoters was evaluated in 120 PA tumors. Representative samples
are shown in Fig. 1. The detection of
bands with both primer sets was observed in a number of samples but
not in all PA tumor samples, probably due to the existence of
non-malignant cells in a fraction of the samples or to the
methylation of only one allele of the gene. MMP-14 promoter
hypermethylation was detected in 30.00% (36/120) of PAs, while the
TGFβ-1 gene promoter was methylated in 13.33% (16/120) of
patients with PA. Both genes were methylated in only 5 samples.
Statistical analysis of age and genes methylation
revealed no correlation between them (χ2 test; age and MMP-14
methylation, P=0.952; and age and TGFβ-1, P=0.971).
MMP-14 methylation was significantly
associated with male gender (58.8 vs. 35.7%, P=0.022), while
unmethylated MMP-14 was associated with female gender (64.3 vs.
41.7%, P=0.027). It was also observed that 45/51 males had
non-silenced TGFβ-1 gene. However, this was not significant
(χ2 test, P=0.664). Associations between methylation status and PA
functioning or recurrence were not identified (P>0.05) (Table II).
 | Table II.Associations between clinical data of
patients and genes methylation. |
Table II.
Associations between clinical data of
patients and genes methylation.
|
|
| MMP-14 | TGFβ-1 |
|---|
|
|
|
|
|
|---|
| Factor | N (%) | U, N (%) | M, N (%) | U, N (%) | M, N (%) |
|---|
| Age, years |
|
|
≤56 | 60 (50.0) | 42 (70.0) | 18 (30.0) | 52 (86.7) | 8
(13.3) |
|
>56 | 59 (49.2) | 41 (69.5) | 18 (30.5) | 51 (86.4) | 8
(13.6) |
|
|
|
| P=0.952 |
| P=0.971 |
| Gender |
|
|
Females | 69 (57.5) | 44 (78.3) | 15 (21.7) | 59 (85.5) | 10 (14.5) |
|
Males | 51 (42.5) | 30 (58.8) | 21 (41.2) | 45 (88.2) | 6
(11.8) |
|
|
| P=0.027 | P=0.022 |
| P=0.664 |
| Hormones
activity |
|
|
None | 64 (53.3) | 45 (70.3) | 19 (29.7) | 57 (89.1) | 7
(10.9) |
|
Appear | 56 (46.7) | 39 (69.6) | 17 (30.4) | 47 (83.9) | 9
(16.1) |
|
|
|
| P=0.936 |
| P=0.409 |
| Recurrence |
|
None | 108 (90.0) | 76 (70.4) | 32 (29.6) | 94 (87.0) | 14 (13.0) |
|
Appear | 12 (10.0) | 8
(66.7) | 4
(33.3) | 10 (83.3) | 2
(16.7) |
|
|
|
| P=0.751 |
| P=0.662 |
| N (%) | 120 (100.0) | 84 (70.0) | 36 (30.0) | 104 (86.7) | 16 (13.3) |
| Invasiveness |
|
|
None | 35 (33.7) | 27 (77.1) | 8
(22.9) | 29 (82.9) | 6
(17.1) |
|
Appear | 69 (66.3) | 44 (63.8) | 25 (36.2) | 62 (89.9) | 7
(10.1) |
|
|
|
| P=0.166 |
| P=0.308 |
| N (%) | 104 (100.0) | 71 (68.3) | 33 (31.7) | 91 (87.5) | 13 (12.5) |
Invasiveness and methylation of both genes had no
correlation (χ2 test, P=0.166 and P=0.308). However, >50%
(62/104) of PAs were invasive and had an unmethylated TGFβ-1 gene.
A correlation between invasiveness and age groups was also
observed, since 40/69 PAs corresponded to patients who were ≤56
years old (χ2 test, P=0.037).
Discussion
PA is a common benign monoclonal neoplasm accounting
for 15–20% of all primary intracranial tumors (19). Pituitary tumors are benign, but not
uncommonly, they invade locally into adjacent tissues such as the
cavernous sinus and dura (20). Early
prediction of which pituitary tumors will recur and/or exhibit an
invasive phenotype remains difficult despite the introduction of
several tissue-based molecular markers (20).
It is known that promoter hypermethylation silences
gene transcription, resulting in a shortage of expression of one or
another protein (21). Membrane
type-1 (MT1)-MMP is an activator of soluble MMP-2 (22). The activity of both MMPs is regulated
by their physiological inhibitor, tissue inhibitor of
metalloproteinase (TIMP)-2 (22). An
MT1-MMP/MMP-2/TIMP-2 axis plays a key role in the invasive behavior
of numerous cell types (22). It was
observed that hypermethylation of the MMP-14 and
MMP-2 genes correlates with non-invasive tumor behavior
(22). To the best of our knowledge,
there are no studies that have explored the association between
MMP-14 methylation status and the development of PA.
Previously, Altaş et al (23)
investigated single nucleotide polymorphism (SNP) in the promoter
of another gene of same MMP family, and analyzed how that
polymorphism is linked to PA development. It is known that
MMP-14 and MMP-1 function similarly in the
degradation of collagen fibers (22).
In agreement with this, Altaş et al observed that SNP of the
MMP-1 gene promoter in both alleles caused a higher risk of
PA development and invasiveness than SNP of the MMP-1 gene
promoter in only one allele (23). In
addition, high expression of the MMP-14 gene was detected in
invasive PA and was associated with invasiveness (24).
The present study examined whether alterations in a
gene promoter are associated with PA occurrences. The current study
analyzed 120 PA patients for MMP-14 promoter methylation.
The results demonstrated that promoter methylation of MMP-14
correlated with male gender (58.8 vs. 35.7%, P=0.022), while
unmethylated (non-silenced) MMP-14 correlated with female
gender (64.3 vs. 41.7%, P=0.027). It is known that the incidence of
PA is double in females compared with males (1). That is why it can be assumed that the
non-silenced MMP-14 gene may be associated with PA cases in
females.
The present study also investigated the methylation
status of the promoter of the TGFβ-1 gene. However, no
associations between the promoter methylation status of the
TGFβ-1 gene and the age and gender of PA patients, PA
hormone activity or recurrence were identified. By contrast, it was
observed that the majority of the males' PA samples were in the
TGFβ-1 unmethylated group. In other studies on PA using
animal models it was noticed that there was a higher expression of
the TGF-β1 cytokine in male than in female individuals
(15). Therefore, the expression of
this gene may be associated with male gender, although further
research is required. There are no studies on potential
associations between methylation of the TGFβ-1 gene and the
secreting function of PA. However, TGF-β1 activity was
observed in hormonally active PA (15,25). In
other studies, which compared healthy and unhealthy pituitary
tissue, low TGFβ-1 gene expression was detected in both
non-invasive and invasive hormonally inactive PA (26). This demonstrates that TGFβ-1
gene transcription happens depending on the type of cancer and the
stage of the cancer process; therefore, further research is
required to identify how this gene is effected by regulating its
expression in the cell.
In another study, Elenkova et al (27) reported that TGF-β1 could be a
predictive blood serum marker for the invasiveness of PA. The
TGFβ-1 gene has been widely studied in other tumors. Chen
et al studied the expression of this gene in patients with
breast cancer and established links with poorer patient clinic
outcome (28). Studies involving lung
tumor cell lines have demonstrated that this gene is important in
cell proliferation (29).
TGF-β1 is also commonly used in cancer studies. There are
in vitro studies on TGF-β1 function in cancer cell
lines other than lung cancer and pituitary adenoma cells (30). Xiao et al analyzed the risks of
radiation-induced pneumonia manifestation in patients with thoracic
tumors, and TGF-β1 SNP was considered as a possible risk
factor (31).
The role of the aforementioned genes has been
studied in cancer and various other disorders. Previous studies
have reported that MMP-14 is associated with tuberculosis by
regulating monocyte migration and collagen destruction (32), and with macrophage activation in
atherosclerosis (33). TGF-β1
function has been observed in brain and nerve damage (34). Thus, these genes appear to be
responsible for a number of molecular mechanisms that are important
in the etiology of various pathological processes.
In conclusion, to the best of our knowledge, the
present study is the first to examine in a large population with PA
(n=120) the association between the MMP-14 and TGFβ-1
promoters methylation status and the development of PA. The present
study has demonstrated for the first time that promoter methylation
of MMP-14 correlates with male gender and unmethylated
(non-silenced) MMP-14 correlates with female gender. Further
investigation is required to evaluate the effect of promoter
methylation of MMP-14 on the development of PA.
References
|
1
|
Nistor R: Pituitary tumors. Neuro Rew.
57:264–272. 1996.
|
|
2
|
Kovacs K, Scheithauer BW, Horvath E and
Lloyd RV: The world health organization classification of
adenohypophysial neoplasms: A proposed five-tier scheme. Cancer.
78:502–510. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Monteiro ML, Moura FC and Cunha LP:
Frequency doubling perimetry in patients with mild and moderate
pituitary tumor-associated visual field defects detected by
conventional perimetry. Arq Bras Oftalmol. 70:323–329. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jagannathan J, Dumont AS, Prevedello DM,
Lopes B, Oskouian RJ, Jane JA Jr and Laws ER Jr: Genetics of
pituitary adenomas: Current theories and future implications.
Neurosurg Focus. 19:E42005.PubMed/NCBI
|
|
5
|
Yadav L, Puri N, Rastogi V, Satpute P,
Ahmad R and Kaur G: Matrix metalloproteinases and cancer-roles in
threat and therapy. Asian Pac J Cancer Prev. 15:1085–1091. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nam DH and Ge X: Direct production of
functional matrix metalloproteinase-14 without refolding or
activation and its application for in vitro inhibition assays.
Biotechnol Bioeng. 113:717–723. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lehti K, Allen E, Birkedal-Hansen H,
Holmbeck K, Miyake Y, Chun TH and Weiss SJ: An MT1-MMP-PDGF
receptor-beta axis regulates mural cell investment of the
microvasculature. Genes Dev. 19:979–991. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sabeh F, Ota I, Holmbeck K,
Birkedal-Hansen H, Soloway P, Balbin M, Lopez-Otin C, Shapiro S,
Inada M, Krane S, et al: Tumor cell traffic through the
extracellular matrix is controlled by the membrane-anchored
collagenase MT1-MMP. J Cell Biol. 167:769–781. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jiang WG, Davies G, Martin TA, Parr C,
Watkins G, Mason MD and Mansel RE: Expression of membrane type-1
matrix metalloproteinase, MT1-MMP in human breast cancer and its
impact on invasiveness of breast cancer cells. Int J Mol Med.
17:583–590. 2006.PubMed/NCBI
|
|
10
|
Massagué J: TGFbeta in Cancer. Cell.
134:215–230. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wakefield LM and Roberts AB: TGF-beta
signaling: Positive and negative effects on tumorigenesis. Curr
Opin Genet Dev. 12:22–29. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Johnson MD, Shaw AK, O'Connell MJ, Sim FJ
and Moses HL: Analysis of transforming growth factor beta receptor
expression and signaling in higher grade meningiomas. J Neurooncol.
103:277–285. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bruna A, Darken RS, Rojo F, Ocaña A,
Peñuelas S, Arias A, Paris R, Tortosa A, Mora J, Baselga J and
Seoane J: High TGFbeta-Smad activity confers poor prognosis in
glioma patients and promotes cell proliferation depending on the
methylation of the PDGF-B gene. Cancer Cell. 11:147–160. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wu Y, Li Q, Zhou X, Yu J, Mu Y, Munker S,
Xu C, Shen Z, Müllenbach R, Liu Y, et al: Decreased levels of
active SMAD2 correlate with poor prognosis in gastric cancer. PLoS
One. 7:e356842012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Recouvreux MV, Lapyckyj L, Camilletti MA,
Guida MC, Ornstein A, Rifkin DB, Becu-Villalobos D and Díaz-Torga
G: Sex differences in the pituitary transforming growth factor-β1
system: Studies in a model of resistant prolactinomas.
Endocrinology. 154:4192–4205. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wilson CB: Neurosurgical management of
large and invasive pituitary tumors. Clinical Management of
Pituitary Disorders. Tindall GT and Collins WF: New York Raven
Press. (New York). 335–342. 1979.
|
|
17
|
Knosp E, Steiner E, Kitz K and Matula C:
Pituitary adenomas with invasion of the cavernous sinus space: A
magnetic resonance imaging classification compared with surgical
findings. Neurosurgery. 33:610–617; discussion 617–618. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li LC and Dahiya R: MethPrimer: Designing
primers for methylation PCRs. Bioinformatics. 18:1427–1431. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Page RB: Sellar and parasellar tumors.
Neurosurgery. Wilkins RH and Rengachary SS: McGraw-Hill. 791–804.
1996.
|
|
20
|
Heaney A: Management of aggressive
pituitary adenomas and pituitary carcinomas. J Neurooncol.
117:459–468. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kulis M and Esteller M: DNA methylation
and cancer. Adv Genet. 70:27–56. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chernov AV, Sounni NE, Remacle AG and
Strongin AY: Epigenetic control of the invasion-promoting
MT1-MMP/MMP-2/TIMP-2 axis in cancer cells. J Biol Chem.
284:12727–12734. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Altaş M, Bayrak OF, Ayan E, Bolukbasi F,
Silav G, Coskun KK, Culha M, Sahin F, Sevli S and Elmaci I: The
effect of polymorphisms in the promoter region of the MMP-1 gene on
the occurrence and invasiveness of hypophyseal adenoma. Acta
Neurochir (Wien). 152:1611–1617; discussion 1617. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hui P, Xu X, Xu L, Hui G, Wu S and Lan Q:
Expression of MMP14 in invasive pituitary adenomas: Relationship to
invasion and angiogenesis. Int J Clin Exp Pathol. 8:3556–3567.
2015.PubMed/NCBI
|
|
25
|
Recouvreux MV, Camilletti MA, Rifkin DB,
Becu-Villalobos D and Díaz-Torga G: Thrombospondin-1 (TSP-1)
analogs ABT-510 and ABT-898 inhibit prolactinoma growth and recover
active pituitary transforming growth factor-β1 (TGF-β1).
Endocrinology. 153:3861–3871. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhenye L, Chuzhong L, Youtu W, Xiaolei L,
Lei C, Lichuan H, Hongyun W, Yonggang W, Fei W and Yazhuo Z: The
expression of TGF-β1, Smad3, phospho-Smad3 and Smad7 is correlated
with the development and invasion of nonfunctioning pituitary
adenomas. J Transl Med. 12:712014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Elenkova A, Atanassova I, Kirilov G,
Vasilev V, Kalinov K and Zacharieva S: Transforming growth factor
β1 is not a reliable biomarker for valvular fibrosis but could be a
potential serum marker for invasiveness of prolactinomas (pilot
study). Eur J Endocrinol. 169:299–306. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen C, Zhao KN, Masci PP, Lakhani SR,
Antonsson A, Simpson PT and Vitetta L: TGFβ isoforms and receptors
mRNA expression in breast tumors: Prognostic value and clinical
implications. BMC Cancer. 15:10102015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Liu ZY, Zhang GL, Wang MM, Xiong YN and
Cui HQ: MicroRNA-663 targets TGFB1 and regulates lung cancer
proliferation. Asian Pac J Cancer Prev. 12:2819–2823.
2011.PubMed/NCBI
|
|
30
|
Wang Y, Jiang M, Li Z, Wang J, Du C,
Yanyang L, Yu Y, Wang X, Zhang N, Zhao M, et al: Hypoxia and TGF-β1
lead to endostatin resistance by cooperatively increasing cancer
stem cells in A549 transplantation tumors. Cell Biosci. 5:722015.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Xiao Y, Yuan X, Qiu H and Li Q:
Single-nucleotide polymorphisms of TGFβ1 and ATM associated with
radiation-induced pneumonitis: A prospective cohort study of
thoracic cancer patients in China. Int J Clin Exp Med.
8:16403–16413. 2015.PubMed/NCBI
|
|
32
|
Sathyamoorthy T, Tezera LB, Walker NF,
Brilha S, Saraiva L, Mauri FA, Wilkinson RJ, Friedland JS and
Elkington PT: Membrane type 1 matrix metalloproteinase regulates
monocyte migration and collagen destruction in tuberculosis. J
Immunol. 195:882–891. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Johnson JL, Jenkins NP, Huang WC, Di
Gregoli K, Sala-Newby GB, Scholtes VP, Moll FL, Pasterkamp G and
Newby AC: Relationship of MMP-14 and TIMP-3 expression with
macrophage activation and human atherosclerotic plaque
vulnerability. Mediators Inflamm. 2014:2764572014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Vincze C, Pál G, Wappler EA, Szabó ER,
Nagy ZG, Lovas G and Dobolyi A: Distribution of mRNAs encoding
transforming growth factors-beta1, −2 and −3 in the intact rat
brain and after experimentally induced focal ischemia. J Comp
Neurol. 518:3752–3770. 2010. View Article : Google Scholar : PubMed/NCBI
|