Introduction
Ductal carcinoma in situ (DCIS) is a type of
non-invasive cancer confined to the breast ductal system, without
involvement of the basement membrane or the surrounding
interstitium (1,2). It is characterized by significant
epithelial hyperplasia and presents characteristic mild to severe
cellular atypism, which increases its risk of development into an
invasive breast cancer (1).
Therefore, the early detection and treatment are not only very
effective but also imperative.
Newly identified DCIS cases account for 7.8–18.8% of
breast cancer patients in China annually (2). Clinically, mammography X-ray and color
ultrasound are the most commonly used diagnostic techniques.
However, each method has important limitations: X-ray is only
sensitive to calcification; and conventional ultrasound can be
useful in estimating tumor size, echogenicity, morphology,
perfusion, and other characteristics (3). Nevertheless, the results are highly
variable and quantitative analyses cannot be conducted. An
automated breast volume scanner (ABVS) can obtain cross-sectional,
vertical, coronal and any other plane images, reflecting tumor
features more clearly (4).
Additionally, computer automatic orientation and calculations can
make the results more objective and operator-independent (4). Furthermore, the breast imaging reporting
and data system (BI-RADS) may be used to classified the benign and
malignant tumors to guide the surgical treatment (5).
The aim of the study was to assess use of the ABVS
and analyze the effects and prognosis of breast conservation
surgery for DCIS to provide a reference for clinical treatment. The
results showed that in the diagnosis of DCIS, ABVS is superior to
conventional ultrasound scanner in guiding breast conservation
surgery and predicting recurrence.
Subjects and methods
Subject information
A total of 142 DCIS female patients with breast
lesions initially presented to The First People's Hospital of
Hangzhou (Hangzhou, China) between January, 2011 and January, 2014
were selected for participation in the study. Eight patients did
not present any abnormalities following examinations via
mammography, MRI and fiberoptic ductoscopy, and were excluded. The
remaining 134 patients that were enrolled had surgical pathology
results. The remaining 134 patients had had a single lesion and
presented clinical features including plasmatic or serous nipple
discharge, breast mass and nipple Paget disease. These patients
underwent mammography X-ray, color ultrasound and ABVS, and they
all had breast conservation surgery indications without
contraindications. The same surgical and nursing teams in The First
People's Hospital of Hangzhou performed all the surgeries in
accordance with standard operation procedures.
The ethics committee of The First People's Hospital
of Hangzhou approved the study. Patients and their relatives
provided written informed consent.
ABVS examination method
The Acuson S2000 ABVS system (Seattle, WA, USA), a
14L5BV high frequency linear array probe, and 11 MHz of center
frequency were used to complete conventional three-dimensional
scans of each side of each breast including the middle, inside and
lateral positions, and the scanning orientation was increased when
the breast was large. After scanning, volume data were transferred
to the ABVS workstation to obtain plane basic images, and perform
three-dimensional reconstructions with basic images of the whole
breast including the vertical and coronal plane. Additionally,
18L6HD high frequency linear array probes made additional scannings
for areas of interest to measure color Doppler parameters. The
independent workstation of the ABVS system analyzed previously
obtained DICOM data, measured the sizes of three lesion diameters
of the largest plane of the three, and determined the shape, edge,
internal echogenicity, and association with surrounding tissues
rigorously. Image data were observed and analyzed independently by
two experienced doctors. Assessment indexes for final
classifications were based on the BI-RADS fifth version
(ultrasound) revised by the American College of Radiology in 2013
(6), and suspected lesions were
recorded, evaluated and compared uniformly and then divided into
grade 0–6 according to the degree of danger, where grade ≥4 were
considered malignant tumors.
Clinical observations
Patients underwent a 3-year follow-up, where ABVS
image characteristics were analyzed, and tumor diameter, BI-RADS
grading and tumor recurrence were identified and recorded.
Statistical analysis
SPSS 19.0 software (SPSS, Inc., Chicago, IL, USA)
was used for recording data and statistical analysis. Quantified
data were presented as mean ± standard deviation, and inter-group
comparisons were carried out using the t-test. Qualitative data
were presented as cases or percentages (%), and inter-group
comparisons were performed using the χ2 test. P<0.05
was statistically significant.
Results
DCIS detection using BI-RADS
category
In the cases studied, DCIS was found in all of the
breast quadrants. Typical manifestations included duct ectasia and
filling in 23 cases, a mass in 38 cases, calcification in 33 cases,
architectural distortion in 23 cases, and solid complex masses in
17 cases. According to the BI-RADS classification, there were 24
probably benign grade ≤3 cases (17.9%); 54 probably malignant
lesions needing biopsy (40.2%): 9 grade 4A cases, 20 grade 4B
cases, and 25 grade 4C cases; 26 highly suspected grade 5 malignant
lesions requiring surgical resection (19.3%); and 30 grade 6
malignant lesions (22.3%). A total of 110 malignant cases were
found using the ABVS system, and the detection rate was 82.1%. By
contrast, 92 cases (68.7%) were considered malignant lesions using
conventional ultrasound, the difference being statistically
significant (χ2=268.000; P<0.001) (Table I).
 | Table I.DCIS detection and tumor
diameters. |
Table I.
DCIS detection and tumor
diameters.
| Parameters | Detection rate No.
(%) | Tumor diameter
(cm) |
|---|
| BI-RADS category | 110 (82.1) | 4.5±0.8 |
| Ultrasonography | 92
(68.7) | 2.0±0.9 |
| t-test/χ2
test | 268.000 | 6.325 |
| P-value | <0.001 | 0.034 |
Tumor diameters
ABVS showed the tumor diameter to range from 0.6 to
9.6 cm (4.5±0.8 cm on average), while conventional ultrasound
showed the diameters to range from 0.8 to 4.2 cm (2.0±0.9 on
average). The tumor diameter using ABVS was significantly larger
than that measured using conventional ultrasound, (t=6.325,
P=0.034) (Table I).
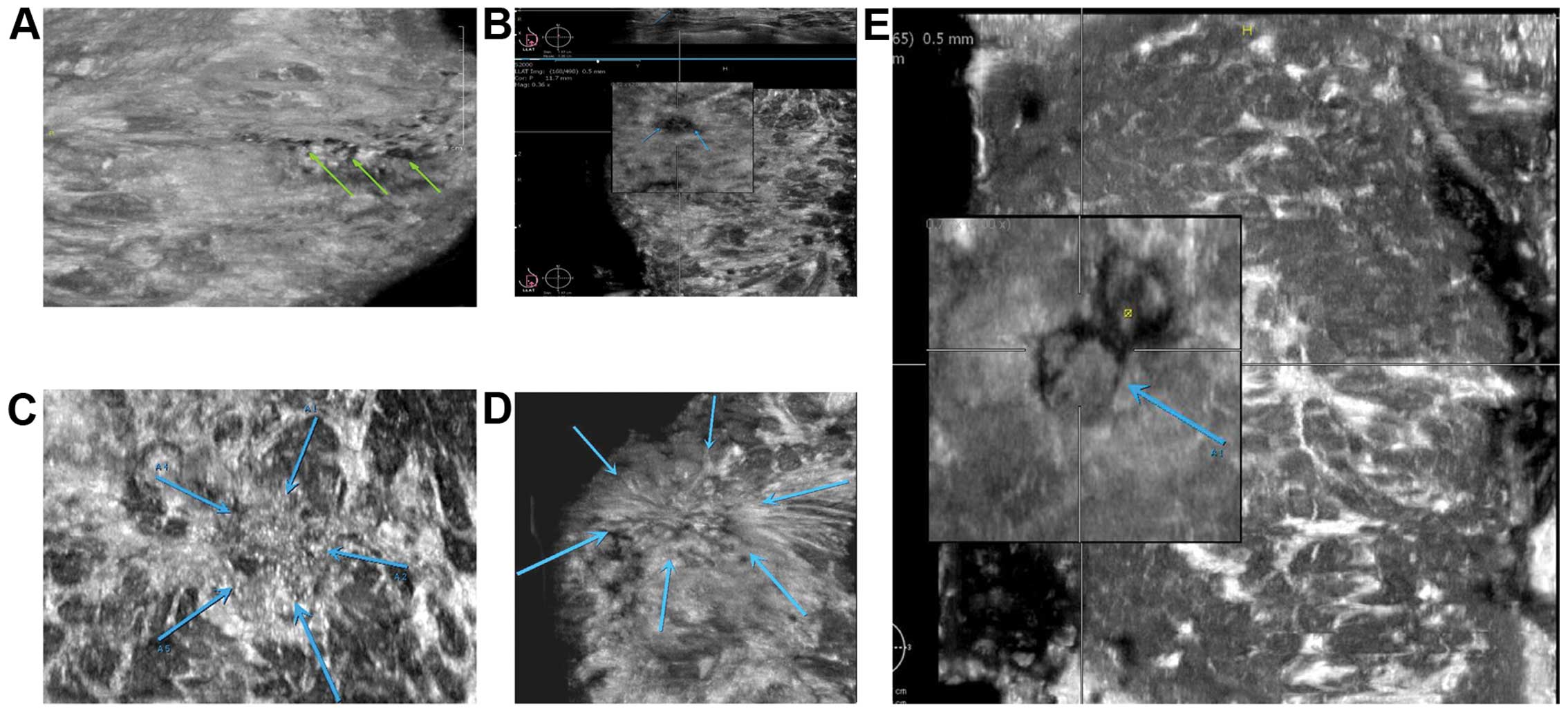
Eight cases (5.6%) of recurrence of DCIS, and their
tumor diameters were the largest by ABVS. However, their diameters
were not larger when examined using conventional ultrasound
(Fig. 1).
Discussion
On ABVS ultrasonography, duct ectasia and filling
reflect local duct expansions, and dilating ducts are evident with
or without a solid hyperechoic mass. In particular, on the coronal
plane, ducts form ‘tree branch’ structures, and tufted calcified
plaques can be detected in the vicinity. This provides clear signs
for diagnosing DCIS (7). Common
reasons for mistreatment in DCIS include instances where no clear
malignant characteristics can be found, when there are intact
edges, mean echogenicities, undetected calcifications,
inconspicuous blood signals in manual scanning, and BI-RADS grades
≤3 (8). Grit-like calcifications are
scattering hyper-echoic calcification distributions, low glandular
tissue echogenicity, and increased local blood flow signals
(9). Architectural distortion
manifests as local gland thickening and echo change with a range of
2.0–10.0 cm, calcification plaques, and different blood flow
signals (10). Complex masses
manifest as mixed cystic and solid echogenic masses with unclear
boundaries between the thick wall and solid part, and present rich
blood flow signals in the solid portions via manual scanning
(11).
The ABVS breast coronal images obtained based on
three-dimensional reconstruction can automatically measure the
distance between the lesion, skin and nipple, and position the mass
clearly within the breast boundaries, providing accurate location
information regarding the mass (12).
The maximum tumor diameter, one of the two biological indexes to
predict breast cancer prognosis, has a negative correlation with
the survival rate, provides evidence for tumor T phasing and
affects the decision for the need of adjuvant chemotherapy, and is
therefore an important index for preoperative evaluation before
breast conservation surgery (13).
Conventional ultrasound obtains the maximum value mainly through
analysis of tumor cross-section and longitudinal section
morphology. However, distortions of shape, position and brightness
on ultrasonography may cause errors in its measurement (14). On the other hand, the ABVS coronal
image conforms to the surgical vision, thus, it can better reflect
edge features of the lesion and more easily identify the invasive
range of cancers (15). The visual
field width of the conventional ultrasound of 3–4 cm, limits to
some extent the measurements of breast tumors with larger ranges,
particularly DCIS in the form of continuous three-dimensional
growths along a duct (16). The
visual field width of ABVS is 15.4 cm, which means it is able to
avoid errors in measurement data caused by image mosaicisms
(17). Notably, previous findings
showed that, the size of breast tumor measured by ABVS is 98%
accurate with a length deviation of <2 cm, supporting the
hypothesis that ABVS can be used for planning breast conservation
surgery (18).
ABVS has the following disadvantages: i) There are
some patients who cannot have their breasts compressed or have poor
scanning results, such as in cases of advanced breast cancer with
diabrotic skin surface. ii) Cross sectional images, useful in the
identification of superficial masses that are prone to slipping
cannot be made. iii) Since ABVS provides two-dimensional grey-scale
images, color Doppler, spectral Doppler and elasticity scanners are
required to provide more complete information. iv) ABVS requires a
large computer and a long period of time to process.
In summary, the detection rate of malignant tumors
was higher than that of conventional ultrasound, and the tumor
diameter detected using ABVS was also more accurate. Therefore,
ABVS is superior to conventional ultrasound in diagnosing DCIS,
guiding breast conservation surgery and predicting recurrence. The
sensitivity, specificity, and accuracy of ABVS for evaluating
suspicious breast lesions should be analyzed in a random clinical
control trial with larger samples in order to provide the best
reference for guiding surgery and improve prognosis.
Acknowledgements
The study was supported by the Science and
Technology Program of Hangzhou (grant no. 20150633B18).
References
|
1
|
Yang WT and Zhu XZ: The introduction of
2012 WHO classification of tumours of the breast. Zhonghua Bing Li
Xue Za Zhi. 42:78–80. 2013.(In Chinese). PubMed/NCBI
|
|
2
|
Si W, Li Y, Han Y, Zhang F, Wang Y, Li Y,
Linghu RX, Zhang X and Yang J: epidemiological and
clinicopathological trends of breast cancer in Chinese patients
during 1993 to 2013: A retrospective study. Medicine (Baltimore).
94:e8202015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bok SK, Jeon Y and Hwang PS:
Ultrasonographic evaluation of the effects of progressive resistive
exercise in breast cancer-related lymphedema. Lymphat Res Biol.
14:18–24. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wojcinski S, Farrokh A, Hille U,
Wiskirchen J, Gyapong S, Soliman AA, Degenhardt F and Hillemanns P:
The automated breast volume scanner (ABVS): Initial experiences in
lesion detection compared with conventional handheld B-mode
ultrasound: A pilot study of 50 cases. Int J Womens Health.
3:337–346. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shen WC, Chang RF and Moon WK: Computer
aided classifications system for breast ultrasound based on Breast
Imaging Reporting and Data System (BI-RADS). Ultrasound Med Biol.
33:1688–1698. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wöhrle NK, Hellerhoff K, Notohamiprodjo M,
Reiser MF and Clevert DA: Automated breast volume scanner (ABVS): A
new approach for breast imaging. Radiologe. 50:973–981. 2010.(In
German). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tozaki M, Isobe S, Yamaguchi M, Ogawa Y,
Kohara M, Joo C and Fukuma E: Optimal scanning technique to cover
the whole breast using an automated breast volume scanner. Jpn J
Radiol. 28:325–328. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shin HJ, Kim HH, Cha JH, Park JH, Lee KE
and Kim JH: Automated ultrasound of the breast for diagnosis:
Interobserver agreement on lesion detection and characterization.
AJR Am J Roentgenol. 197:747–754. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang Q, Hu B, Hu B and Li WB: Detection
of breast lesions using an automated breast volume scanner system.
J Int Med Res. 40:300–306. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Isobe S, Tozaki M, Yamaguchi M, Ogawa Y,
Homma K, Satomi R, Saito M, Joo C and Fukuma E: Detectability of
breast lesions under the nipple using an automated breast volume
scanner: Comparison with handheld ultrasonography. Jpn J Radiol.
29:361–365. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li N, Jiang YX, Zhu QL, Zhang J, Dai Q,
Liu H, Yang Q, Wang HY, Lai XJ and Sun Q: Accuracy of an automated
breast volume ultrasound system for assessment of the pre-operative
extent of pure ductal carcinoma in situ: Comparison with a
conventional handheld ultrasound examination. Ultrasound Med Biol.
39:2255–2263. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kim YW, Kim SK, Youn HJ, Choi EJ and Jung
SH: The clinical utility of automated breast volume scanner: A
pilot study of 139 cases. J Breast Cancer. 16:329–334. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Golatta M, Franz D, Harcos A, Junkermann
H, Rauch G, Scharf A, Schuetz F, Sohn C and Heil J: Interobserver
reliability of automated breast volume scanner (ABVS)
interpretation and agreement of ABVS findings with hand held breast
ultrasound (HHUS), mammography and pathology results. Eur J Radiol.
82:e332–e336. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Garcia-Uribe A, Erpelding TN, Krumholz A,
Ke H, Maslov K, Appleton C, Margenthaler JA and Wang LV:
Dual-modality photoacoustic and ultrasound imaging system for
noninvasive sentinel lymph node detection in patients with breast
cancer. Sci Rep. 5:157482015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen L, Chen Y, Diao XH, Fang L, Pang Y,
Cheng AQ, Li WP and Wang Y: Comparative study of automated breast
3-D ultrasound and handheld B-mode ultrasound for differentiation
of benign and malignant breast masses. Ultrasound Med Biol.
39:1735–1742. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hao SY, Ou B, Li LJ, Peng YL, Wang Y, Liu
LS, Xiao Y, Liu SJ, Wu CJ, Jiang YX, et al: Could ultrasonic
elastography help the diagnosis of breast cancer with the usage of
sonographic BI-RADS classification? Eur J Radiol. 84:2492–2500.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Giuliano V and Giuliano C: Improved breast
cancer detection in asymptomatic women using 3D-automated breast
ultrasound in mammographically dense breasts. Clin Imaging.
37:480–486. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tozaki M and Fukuma E: Accuracy of
determining preoperative cancer extent measured by automated breast
ultrasonography. Jpn J Radiol. 28:771–773. 2010. View Article : Google Scholar : PubMed/NCBI
|