Introduction
In contrast to patients with numerous other
carcinomas in which fatality most often occurs as a result of
disseminated malignant disease, patients with oral, head and neck
carcinoma typically succumb to the disease with a lack of clinical
evidence of metastasis beyond regional or local disease (1). Therefore, use of a neck dissection is
important to control regional spread to the lymph nodes and to
prevent localized spread (2). Neck
dissection involves the neurological and vascular structures of the
neck being exposed and manipulated, which may lead to the
complication of perioperative stroke. The occurrence of
perioperative stroke during neck and head surgery is a severe
complication associated with a high risk of morbidity and
mortality. Nosan et al (3) and
Thompson et al (2) reported
that the incidence rates of perioperative stroke in patients with
head and neck cancers were 4.8 and 0.2%, respectively.
Perioperative stroke is a cerebrovascular incident
that can arise intraoperatively (4).
Carotid artery stenosis is a significant risk factor for stroke,
and is associated with various other factors, including smoking,
peripheral vascular disease, hypertension, diabetes, male gender,
atherosclerotic heart disease, age and external radiotherapy to the
head and neck (5–7). Patients with head and neck cancer
undergoing a neck dissection may demonstrate a number of these risk
factors, therefore predisposing them to perioperative stroke.
The present study describes the case of a female
patient who experienced perioperative stroke during surgery for the
treatment of oral, head and neck cancer.
Case report
In August 2013, an 84-year-old female was referred
to a general dental practitioner for gingival swelling and pain in
the upper left molar region. A red, painful ulcer was noted during
the examination and the patient was subsequently referred to the
Division of Oral and Maxillofacial Surgery, Kagawa Prefectural
Central Hospital (Takamatsu, Japan) for evaluation of a possible
maxillary gingival carcinoma also in August 2013. Extraoral
examination detected slight left-sided facial asymmetry and
tenderness. The upper jugular and left submandibular lymph nodes
were palpable and tender. Intraoral examination detected a 25×35-mm
mass in the palatal and buccal aspect of the left maxillary
edentulous alveolus, in the proximity of the first premolar and the
second molar. The mucosal surface of the mass was rough and tender,
and was covered with numerous pink-red, pebbly, hemorrhagic papules
that bled on palpation. The medical history of the patient included
hypertension and hyperlipidemia, for which the patient was taking
an angiotensin II receptor antagonist (losartan potassium), and a
calcium channel blocker (amlodipine) and a
3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibitor (statin;
pravastatin sodium), respectively. There was no history of cerebral
infarction.
Computed tomography (CT; Aquilion 64; Toshiba
America Medical Systems, Inc., Tustin, CA, USA) revealed a
42×40-cm, enhanced lesion, which extended from the left maxillary
alveolar region to the maxillary sinus, buccal mucosa and hard
palate, in addition to a number of enhanced lymph nodes in the
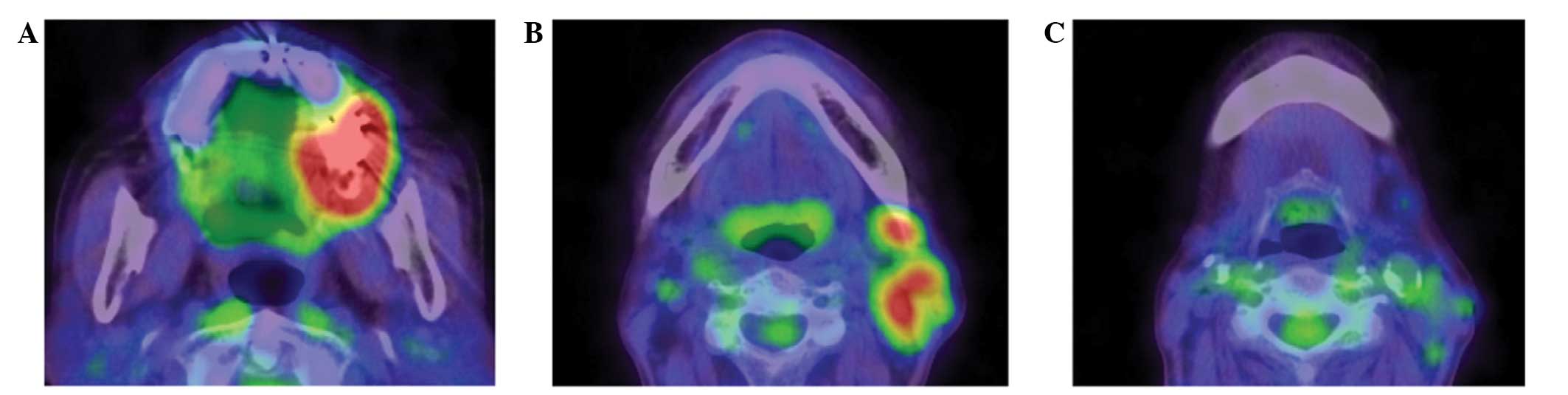
ipsilateral neck. 18F-fluorodeoxyglucose-positron
emission tomography (FDG-PET; Biograph mCT40; Siemens Healthcare,
Erlangen, Germany) detected increased uptake in the left maxilla
[maximum standardized uptake value (SUVmax), 10.5; Fig. 1A] and multiple regional lymph nodes
(SUVmax, 5.0; Fig.1B).
18F-FDG-PET did not demonstrate active uptake in the
calcified carotid artery (Fig. C),
and no abnormal uptake suggestive of second primary or distant
metastasis was detected.
From these observations, the tumor was clinically
staged as T4aN2bM0 in accordance with the 2010 Union for
International Cancer Control system (8). An incisional biopsy was performed and
following inspection (hematoxylin and eosin staining), during which
squamous differentiation was observed in the form of keratinization
with variable pearl formation, loss of the basement membrane and
disturbed architecture of the basal layers of the epithelium, the
lesion was diagnosed as squamous cell carcinoma (SqCC). Thus, a
left subtotal maxillectomy with a left neck dissection was planned.
Pre-operative CT revealed an advanced, calcified plaque in the
contralateral right carotid artery that required neck dissection
(Fig. 2); therefore, the surgery was
performed without discontinuing the statin treatment that the
patient had been administered for several years. In September 2013,
a left subtotal maxillectomy, left neck dissection and tracheotomy
were performed under general anesthesia (Fig. 3).
Following the surgery, the patient was transferred
to the intensive care unit (ICU) of the Kagawa Prefectural Central
Hospital. The respiratory and circulatory systems were managed
under sedation. The patient was maintained on mechanical
ventilation under continuous dexmedetomidine (DEX; 0.2–0.7 µg/kg/h)
sedation. The level of sedation was reduced once the patient
achieved spontaneous, stable breathing, which occurred at 6 h
post-surgery. At that time, the patient was poorly responsive, with
no movement of the right-sided extremities. Brain magnetic
resonance (MR) imaging (Magnetom Avanto; Siemens Healthcare)
revealed a fresh watershed area infarction in the left middle
cerebral artery (Fig. 4), and MR
angiography exhibited no obvious vascular stenosis. Edaravone (60
mg) was administered twice per day for 2 days, and continuous
respiratory and circulatory management was performed. On day 2
post-surgery, the patient began rehabilitation in the ICU. As there
were no complications of the respiratory and circulatory systems or
the surgical site, the patient was discharged from the ICU on day 5
post-surgery. Several days later, the patient demonstrated
progressive improvement. Occupational and physical therapists were
consulted to evaluate and plan rehabilitation. In order to
encourage mobility using a caster walker, the patient was
discharged on day 38 post-surgery. At the 6-month post-operative
follow-up, the patient was able to walk using a walking stick and
perform normal daily tasks with minimal residual weakness.
Approximately 1 year subsequent to surgery, the patient exhibited
recurrence from the primary tumor, and underwent radiation
treatment at Takinomiya General Hospital (Ayauta, Japan). The
patient succumbed to disease due to airway obstruction in June
2015.
Discussion
Lymph node metastases occur in >50% of patients
with oral SqCC, and histological confirmation of metastatic disease
is a key prognostic factor (9).
Localized spread may be prevented by tumor excision and neck
dissection, which aim to control the regional spread to the lymph
nodes (2). In contrast to non-neck
procedures, neck dissections carry a high risk of cerebrovascular
accidents; this is primarily due to the neck often being rotated
and hyperextended during surgery, which may result in plaque
ulceration from turbulent flow or intimal tearing of the carotid
artery and thrombus formation. In addition, the carotid artery is
frequently retracted, which may dislodge a thrombus or plaque
(10).
The incidence of perioperative stroke during the
performance of non-neck and head surgery is 0.08–0.2% (11). There are a limited number of reports
regarding the incidence of perioperative stroke in patients who
undergo neck dissection. Nosan et al (3) retrospectively reviewed 5 patients that
had undergone neck dissection and reported a 4.8% incidence of
perioperative stroke occurring during surgery. A study by Rechtweg
et al (11) described 3 cases
of simultaneous carotid endarterectomy and neck dissection. In the
discussion section, the study reported an unpublished personal
communication from Yoo et al (unpublished data), who
reviewed 441 patients undergoing neck dissections in Toronto,
Canada, and found an incidence of perioperative stroke of 3.2%. By
contrast, Thompson et al (2)
reported that the incidence of perioperative stroke in 499 patients
undergoing a neck dissection for cancer of the neck and head was as
low as 0.2%. However, the data from Thompson et al (2) was obtained from a historical cohort that
analyzed hospital discharge data, and it may be possible that
data-entry errors occurred. Further large-scale clinical studies
are required to confirm these incidence rates.
Carotid artery stenosis is the most significant risk
factor for stroke (12).
Atherosclerotic plaque vulnerability represents a crucial target to
decrease the probability of plaque rupture and the thrombotic
ischemic events that follow (13,14).
CT/FDG-PET facilitates highly precise measurements of the
inflammatory activity of atherosclerotic plaques (15,16). The
patient of the present case presented with a number of risk
factors, including a calcification in the carotid artery revealed
by CT, although an unstable plaque did not exist on FDG-PET/CT.
Therefore, surgery was performed without discontinuing the statin
treatment that the patient had been administered for several years.
Local and systemic inflammatory mediators favor the increase of
plaque vulnerability. Treatment with statins has been demonstrated
to diminish inflammatory processes and increase collagen
stabilization in carotid atherosclerotic plaques (17). Furthermore, it has been reported that
treatment with statins leads to decreased macrophage accumulation
in the carotid plaques of patients with hypercholesterolemia and
significant carotid stenosis when compared with cholestyramine plus
β-sitosterol treatment (18).
Head and neck surgeries can often be prolonged;
thus, patients may require post-operative sedation (19). If it is determined that there is a
high risk of post-operative stroke, neurological assessments are
required while the patient is sedated. Traditional agents,
including propofol, lorazepam and midazolam, induce sedation by
acting on γ-aminobutyric acid receptors; therefore, it is difficult
to judge the neurological state of the patient when treated with
such agents. By contrast, DEX, a selective α2-adrenergic receptor
agonist, sustains a natural sleep pattern and evokes cooperative
sedation from which patients are easily aroused. In addition, DEX
results in reduced impairment of post-operative cognitive function
(20); thus, DEX allows patients to
awaken for neurological evaluation.
In conclusion, the present case demonstrates that
perioperative stroke can occur in patients undergoing surgery for
oral, neck and head cancer. In the current case, there was no
prophylaxis for the occurrence of stroke during the neck
dissection. However, if patients are pre-operatively judged to be
at high risk, pre-operative statins should be administered, the
surgery should be carefully performed, adequate sedation should be
maintained post-operatively and the patient should be cautiously
observed for the early detection of stroke.
References
|
1
|
Coleman JJ and Sultan MR: Tumors of the
head and neckPrinciples of Surgery. 7th. Schwartz SI, Shires GT,
Spencer FC, Daly JM, Fischer JE and Galloway AC: McGraw-Hill; New
York: pp. 601–665. 1999
|
|
2
|
Thompson SK, Southern DA, McKinnon JG,
Dort JC and Ghali WA: Incidence of perioperative stroke after neck
dissection for head and neck cancer: A regional outcome analysis.
Ann Surg. 239:428–431. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nosan DK, Gomez CR and Maves MD:
Perioperative stroke in patients undergoing head and neck surgery.
Ann Otol Rhinol Laryngol. 102:717–723. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kim J and Gelb AW: Predicting
perioperative stroke. J Neurosurg Anesthesiol. 7:211–215. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bashar K, Healy D, Clarke-Moloney M, Burke
P, Kavanagh E and Walsh SR: Effects of neck radiation therapy on
extra-cranial carotid arteries atherosclerosis disease prevalence:
Systematic review and a meta-analysis. PLoS One. 9:e1103892014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lam WW, Yuen HY, Wong KS, Leung SF, Liu KH
and Metreweli C: Clinically underdetected asymptomatic and
symptomatic carotid stenosis as a late complication of radiotherapy
in Chinese nasopharyngeal carcinoma patients. Head Neck.
23:780–784. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cheng SW, Wu LL, Ting AC, Lau H, Lam LK
and Wei WI: Irradiation-induced extracranial carotid stenosis in
patients with head and neck malignancies. Am J Surg. 178:323–328.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Edge S, Byrd DR, Compton CC, Fritz AG,
Greene FL and Trotti A: AJCC Cancer Staging Manual (7th). Springer.
Chicago, IL, USA: 2010.
|
|
9
|
Kowalski LP and Sanabria A: Elective neck
dissection in oral carcinoma: A critical review of the evidence.
Acta Otorhinolaryngol Ital. 27:113–117. 2007.PubMed/NCBI
|
|
10
|
Atik MA, Ates M, Akkus NI, Altundag O and
Altundag K: Preoperative Doppler sonography for prevention of
perioperative stroke in head and neck cancer patients undergoing
neck dissection: Is it beneficial? J Clin Ultrasound. 35:38–39.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rechtweg J, Wax MK, Shah R, Granke K and
Jarmuz T: Neck dissection with simultaneous carotid endarterectomy.
Laryngoscope. 108:1150–1153. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Calliada F, Verga L, Pozza S, Bottinelli O
and Campani R: Selection of patients for carotid endarterectomy:
The role of ultrasound. J Comput Assist Tomogr. 23(Suppl 1):
S75–S81. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Naghavi M, Libby P, Falk E, Casscells SW,
Litovsky S, Rumberger J, Badimon JJ, Stefanadis C, Moreno P,
Pasterkamp G, et al: From vulnerable plaque to vulnerable patient:
A call for new definitions and risk assessment strategies: Part I.
Circulation. 108:1664–1672. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Naghavi M, Libby P, Falk E, Casscells SW,
Litovsky S, Rumberger J, Badimon JJ, Stefanadis C, Moreno P,
Pasterkamp G, et al: From vulnerable plaque to vulnerable patient:
A call for new definitions and risk assessment strategies Part II.
Circulation. 108:1772–1778. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mehta NN, Yu Y, Saboury B, Foroughi N,
Krishnamoorthy P, Raper A, Baer A, Antigua J, Van Voorhees AS,
Torigian DA, et al: Systemic and vascular inflammation in patients
with moderate to severe psoriasis as measured by
[18F]-fluorodeoxyglucose positron emission tomography-computed
tomography (FDG-PET/CT): A pilot study. Arch Dermatol.
147:1031–1039. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yun M, Yeh D, Araujo LI, Jang S, Newberg A
and Alavi A: F-18 FDG uptake in the large arteries: A new
observation. Clin Nucl Med. 26:314–319. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Crisby M, Nordin-Fredriksson G, Shah PK,
Yano J, Zhu J and Nilsson J: Pravastatin treatment increases
collagen content and decreases lipid content, inflammation,
metalloproteinases and cell death in human carotid plaques:
Implications for plaque stabilization. Circulation. 103:926–933.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Puato M, Faggin E, Rattazzi M, Zambon A,
Cipollone F, Grego F, Ganassin L, Plebani M, Mezzetti A and
Pauletto P: Atorvastatin reduces macrophage accumulation in
atherosclerotic plaques: A comparison of a nonstatin-based regimen
in patients undergoing carotid endarterectomy. Stroke.
41:1163–1168. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Paul BS and Paul G: Sedation in
neurological intensive care unit. Ann Indian Acad Neurol.
16:194–202. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yu SB: Dexmedetomidine sedation in ICU.
Korean J Anesthesiol. 62:405–411. 2012. View Article : Google Scholar : PubMed/NCBI
|