Introduction
Treatment of symptomatic multiple myeloma has
significantly improved progression-free and overall survival times
over the past 20 years, with the introduction of autologous blood
stem cell transplantation (ASCT) in the early 1990s and
subsequently the approval of proteasome-inhibitors and
immunomodulatory drugs (IMiDs) (1–3).
The 5-year overall survival rate has increased from
35% for the years of 1999–2001, to 44% for the years of 2006–2009.
In particular, the survival of patients aged <50 years has
significantly improved, with 10-year survival rates increasing from
25 to 41% (4,5).
These improvements in survival are not based on a
single agent or single treatment strategy, but rather on the
selection of sequential regimens and design of combination
therapies. Prognostic tests have been developed simultaneously with
the integration of novel agents into the treatment algorithms. In
particular, molecular markers have been identified that may support
treatment decisions (6).
The optimal integration of novel agents and the
future development of effective combination therapies is a major
goal in myeloma research. Several sets of guidelines have been
published and revised over time that outline recommendations for
first-line therapy, but also for relapsed and refractory patients
(2,3,7,8). Importantly, current treatment
recommendations and guidelines integrate prognostic factors into
the treatment decisions (7).
Nonetheless, myeloma treatment still requires additional
improvement, as many patients suffer from treatment-related
complications and ultimately will succumb to disease
progression.
The present survey was conducted with the goal of
investigating whether recent international treatment guidelines
were applied to the routine diagnostic work-up of myeloma patients
and were used for treatment decisions. The matter of how the
diagnostic and treatment decisions have changed over time was also
examined by comparison with previously published surveys (9).
The current study sought to provide information on
real-world treatment and diagnostic decisions to support
information on which regimen and treatment pathways are currently
favoured by clinicians, and which regimen could be the basis for
the future development of myeloma care.
Patients and methods
Study design
The goal of the current study was to analyse the
pattern of multiple myeloma management in clinical practice. The
analysis was based on an epidemiological database (TherapyMonitor
compiled by OncologyInformationService, Freiburg, Germany),
comprising 478 patients from 58 centres in Germany, namely 10
university hospitals, 27 community hospitals, and 21 office-based
haematologists, with a treatment decision made for multiple myeloma
in the 1st-2nd quarter of 2011. This constitutes a representative
statistical sample regarding the distribution of treated patients
with multiple myeloma (‘treated prevalence’).
Selection of the centres was based on a two-step
procedure. A total of 817 centres involved in the treatment of
multiple myeloma, including university hospitals (n=36), community
hospitals (n=355) and office-based haematologists (n=426), were
contacted, and 15% of centres responded to provide their number of
multiple myeloma patients (corresponding to 13% of the expected
national prevalence). Based on this information, the distribution
of multiple myeloma patients across the three main care providers
was determined as follows: university hospitals, 20%; community
hospitals, 40%; and office-based haematologists, 40%. The total
patient sample (n=500) eligible for analysis after the quality
check (n=478) was defined by taking into account the treated
prevalence per type of institution, the regional population density
and health care structure. Reporting centres were selected randomly
among the responders according to the date of response to the
mailing. In the second step, demographic and clinical data were
collected retrospectively in an online case report based on data in
the clinical files. Patients who met the following criteria were
included: Therapeutic decision (start, change, or end of therapy)
between January and June 2011. Data was verified by central
monitoring.
Demographics and clinical data
Patients' baseline characteristics [demographics,
medical history, including comorbidity status, and multiple myeloma
stage at initial diagnosis according to Durie-Salmon staging
(10)] and clinical data were
retrospectively extracted from chart reviews. All variables were
reported by the treating physician and pseudonymised according to
the available information in the patient chart. The online and
external monitoring systems assessed the plausibility and
completeness of the data. To descriptively assess the diagnostic,
prognostic and treatment patterns according to age, information on
cytogenetic testing (yes/no, results), and treatment (including its
objective and reasons for starting therapy) was analysed for all
patients. Patient characteristics are displayed in Table I.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Characteristics (at
initial diagnosis)a | 2011 (n=478) | 2009 (n=275) | 2008 (n=386) |
|---|
| Age (mean in
years) | 67.9 | 67.6 | 66.4 |
| Gender (%
female) | 43 | 49 | 41 |
| Malignant disease in
medical history (%) | 6 | 8 | 15 |
| Durie-Salmon stage
(%) |
|
|
|
| Stage
I | 21 | 11 | 16 |
| Stage
II | 22 | 16 | 20 |
| Stage
III | 57 | 68 | 61 |
| IgG type
(%)b |
|
|
|
| IgG | 55 | Not asked | Not asked |
| IgA | 25 |
|
|
| IgM | 3 |
|
|
| IgD | 0 |
|
|
| Cytogenetic
evaluation (FISH, aberrations with frequency ≥5%) |
|
|
|
| Del
13 | 38 | 57 | 65 |
| Del
17 | 12 | 16 | 10 |
|
t(4;14) | 19 | 14 | 14 |
|
t(p16;q32) | 5 | 2 | 1 |
|
β2-microglobulin (median in
mg/dl) | 4.8 | 4.5 | 3.7 |
| Albumin (g/dl) |
|
|
|
|
Median | 4.4 | 4.3 | 28.0 |
| Mean | 15.7 | 15.1 | 22.9 |
| First line therapy
(n) | 429 | 242 | 335 |
| Concomitant
diseasec (n) |
|
|
|
| Renal
insufficiency | 20 | 17 | 17 |
|
Arterial hypertension | 35 | 41 | 30 |
|
Coronary heart disease | 20 | 16 | 13 |
|
Arrhythmia | 11 | 7 | 8 |
| Cardiac
insufficiency | 16 | 13 | 12 |
|
Diabetes mellitus | 15 | 17 | 10 |
|
Psychiatric diagnosis
(including depression) | 6 | 7 | 5 |
Statistical analysis
Data presented in this article were analysed using
descriptive and explorative methods. Diagnostic and treatment
patterns were reported as absolute and relative frequencies.
For exploratory analyses, subgroup comparisons as
well as bivariate analysis were performed. Differences in treatment
patterns between subgroups and predictive factors were analysed
using χ2 and Fisher's exact tests. All P-values are
given as two-sided values, and P<0.05 was considered to indicate
a statistically significant difference. SPSS software, version 20
(IBM SPSS, Armonk, NY, USA) was used for analysis.
Results
Baseline diagnostics, prognostic
laboratory tests and patient characteristics
The patient data reflected a representative multiple
myeloma population, with a mean age of 67.9 years and a balanced
distribution across the participating institutions. Patient
characteristics are summarised in Table
I.
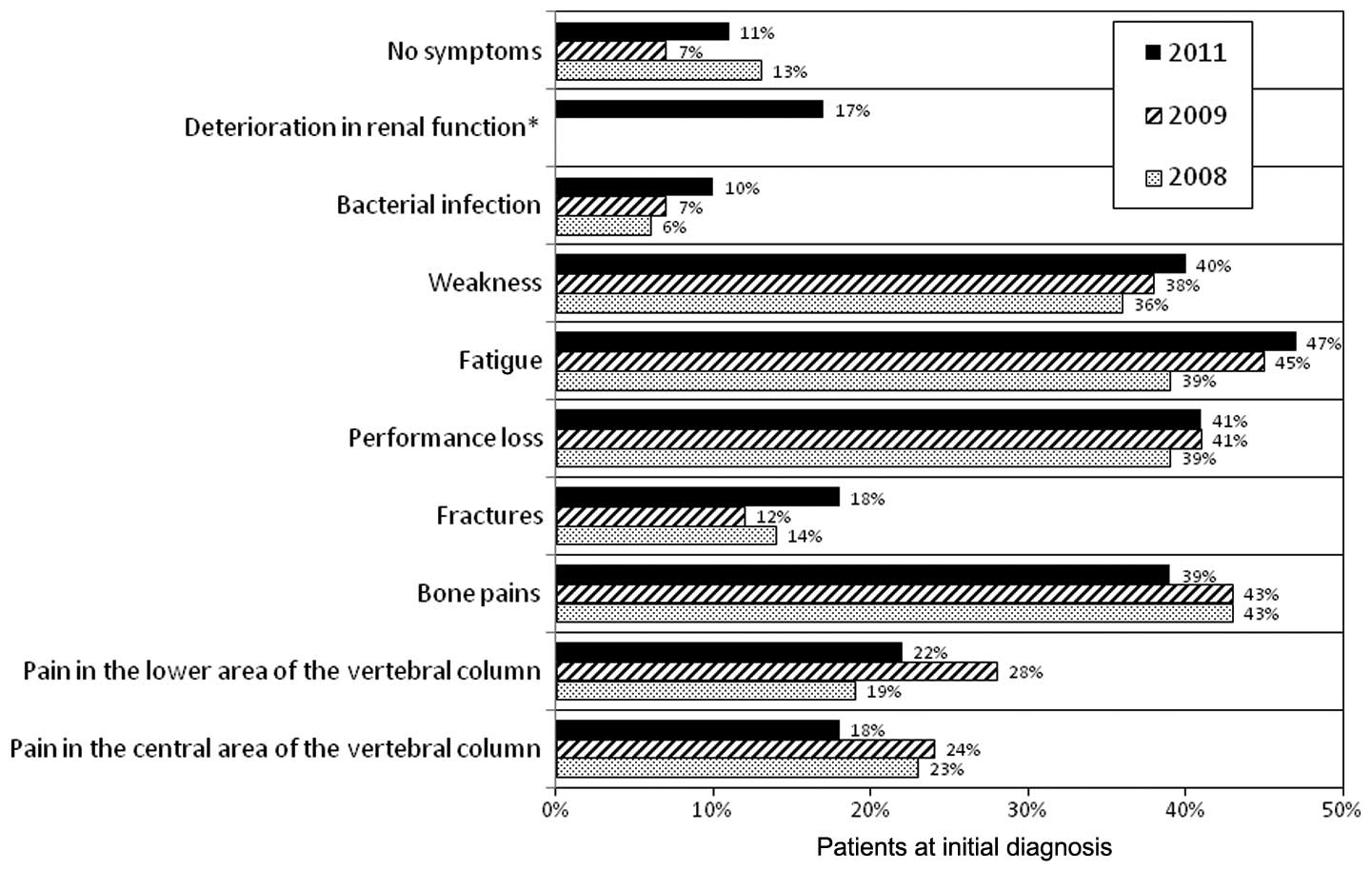
Leading symptoms (largely unchanged over time) at
diagnosis were non-specific (see summary in Fig. 1), as expected: Fatigue (47%), bone
pain (39%), weakness (40%) and decreased performance (41%) were the
most common.
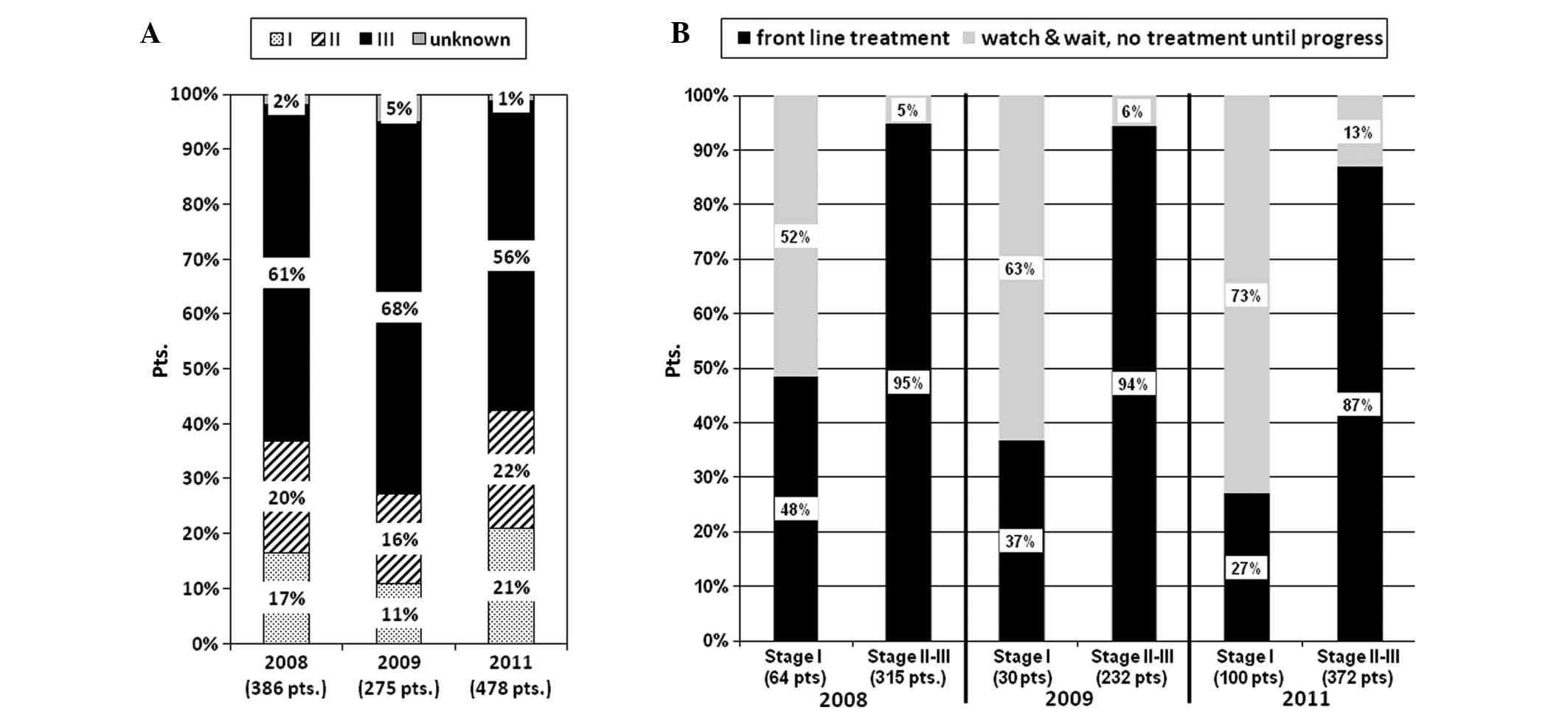
The majority of patients (79%) were in Durie-Salmon
stage II and III at time of initial diagnosis. The concomitant
disease spectrum was headed by renal insufficiency (23%) and
arterial hypertension (36%). Importantly, the percentage of
preexisting polyneuropathy was 5%, and an additional 5% of patients
had a psychiatric diagnosis, predominantly depression. The
percentage of patients with malignant disease in their medical
history has decreased over time, from 15% (2008), to 8% (2009), to
5% (2011).
A trend for a lower burden of disease at first
diagnosis was observed, as 21% of patients were in Durie-Salmon
stage I/II in 2011, whereas only 11% and 17% were in Durie-Salmon
stages I/II in 2009 and 2008, respectively. Notably, the percentage
of patients requiring systemic treatment in Durie-Salmon stage I/II
did not increase, but rather decreased (Fig. 2A and B).
The acceptance of the International Staging System
(ISS) (11) as a key prognostic
factor was confirmed, as 75% of patients received a classification
according to ISS in the current study, whereas <20% had an ISS
classification in the 2009 survey.
Compared with the previous survey, the acceptance of
cytogenetic testing has increased from 23% in 2008 (9) and 35% in 2009, to 53% in the current
analysis across the institutional segments.
The decision tree method was used to identify the
factors with major impacts on the choice of cytogenetic testing at
initial diagnosis of multiple myeloma. In the group of patients
without β2-microglobulin (β2-MG) assessment
and aged >69 years, only 16% of patients underwent cytogenetic
testing. By contrast, 94% patients in stage II without a
concomitant disease received cytogenetic testing if a
β2-MG assessment was performed. In summary,
β2-MG and cytogenetic tests were often performed
simultaneously or not performed at all.
Treatment within clinical trials
Overall, 5% of patients received first-line
treatment within clinical studies. University hospitals were
leading with 11% of patients enrolled into clinical studies, while
non-university hospitals and office-based haematologists recruited
4% of their first-line patients for clinical trials.
A total of 33% (155 of 475) of reported patients
were considered eligible for ASCT following high-dose chemotherapy
(Fig. 3A). Only 47% of this eligible
population (representing 19% of the survey population) actually
received ASCT as part of the first-line treatment. Another 8% of
patients received ASCT procedure in relapse, leading to total of
27% of patients treated with ASCT. Only a minority of
ASCT-candidates received tandem ASCT (2% of total patients, 6% of
ASCT candidates). There was no obvious change in the ASCT treatment
pattern; in the previous survey, a similar percentage of patients
was treated with this approach (9).
First-line treatment
The median age at the time of the front-line
treatment decision was 69 years in the current survey, and 42% of
patients were aged >70 years. A minority of patients >65
years of age were considered for ASCT (66–70 years, 29%; >70
years, 5%). As expected, age was the most significant factor
(P<0.001) influencing the decision for ASCT in the front-line
setting (Fig. 3B). The decision
matrix for patients above and below 69 years of age was
investigated using a univariate logistical regression analysis. For
elderly patients (aged >69 years), more advanced Durie-Salmon
stage, presence of CRAB criteria (3),
and presence of bone lesions were identified as factors that
influenced the decision in favour of ASCT (Fig. 4A). Similarly, in the younger patient
population (aged <69 years), more severe disease (defined by
CRAB criteria) (P=0.005) or diagnosis of bone lesions (P<0.001)
influenced the decision in favour of conducting ASCT (Fig. 4B).
The decision regarding ASCT as a possible treatment
option influenced the choice of chemotherapy regimen for tumour
mass reduction (Fig. 5).
Nevertheless, ~60% of patients considered not to be an ASCT
candidate received a bortezomib regimen. Despite the great variety,
bortezomib-containing regimens were most frequently used in the
non-intensive group (those not treated by high-dose melphalan and
ASCT). Bortezomib in combination with chemotherapy was administered
in 60% of patients (Fig. 5);
chemotherapy combination partners were cyclophosphamide,
doxorubicin (Adriamycin), melphalan and bendamustine. Bortezomib
single-agent therapy was only used for 3% of the patients. Therapy
with IMiDs or IMiD-combination therapies were applied in 18% of
patients that were not planned for ASCT. Only a minority (24%) of
patients received a bortezomib/IMiD-free single-agent or
chemo/steroid combination therapy. Melphalan (9%) or bendamustine
(8%) were the most commonly used chemotherapies (as single agents)
used in combination with corticosteroids in the current survey.
Only a small percentage of patients were treated with
Adriamycin-containing combinations (4%) or steroid monotherapy (1%)
(Fig. 5).
The vast majority (83%) of patients who were
scheduled for ASCT were treated in the induction phase with
bortezomib-based combination therapies (Fig. 5). The most frequently used bortezomib
containing regimens were bortezomib+ Adriamycin+ dexamethasone
(42%), bortezomib+ cyclophosphamide+ dexamethasone (31%) and
bortezomib+ thalidomide+prednisolone (10%).
Among patients treated with ASCT, consolidation
therapy was performed in 2% and maintenance therapy was performed
in 24% of patients. Maintenance therapy was conducted within a
clinical study in 38%. The following medications were used for
maintenance therapy with decreasing frequency: Thalidomide,
lenalidomide and bortezomib. A small percentage (5%) of patients
received additional prednisone; however, the majority of patients
were treated with a single-agent approach in the maintenance
therapy period.
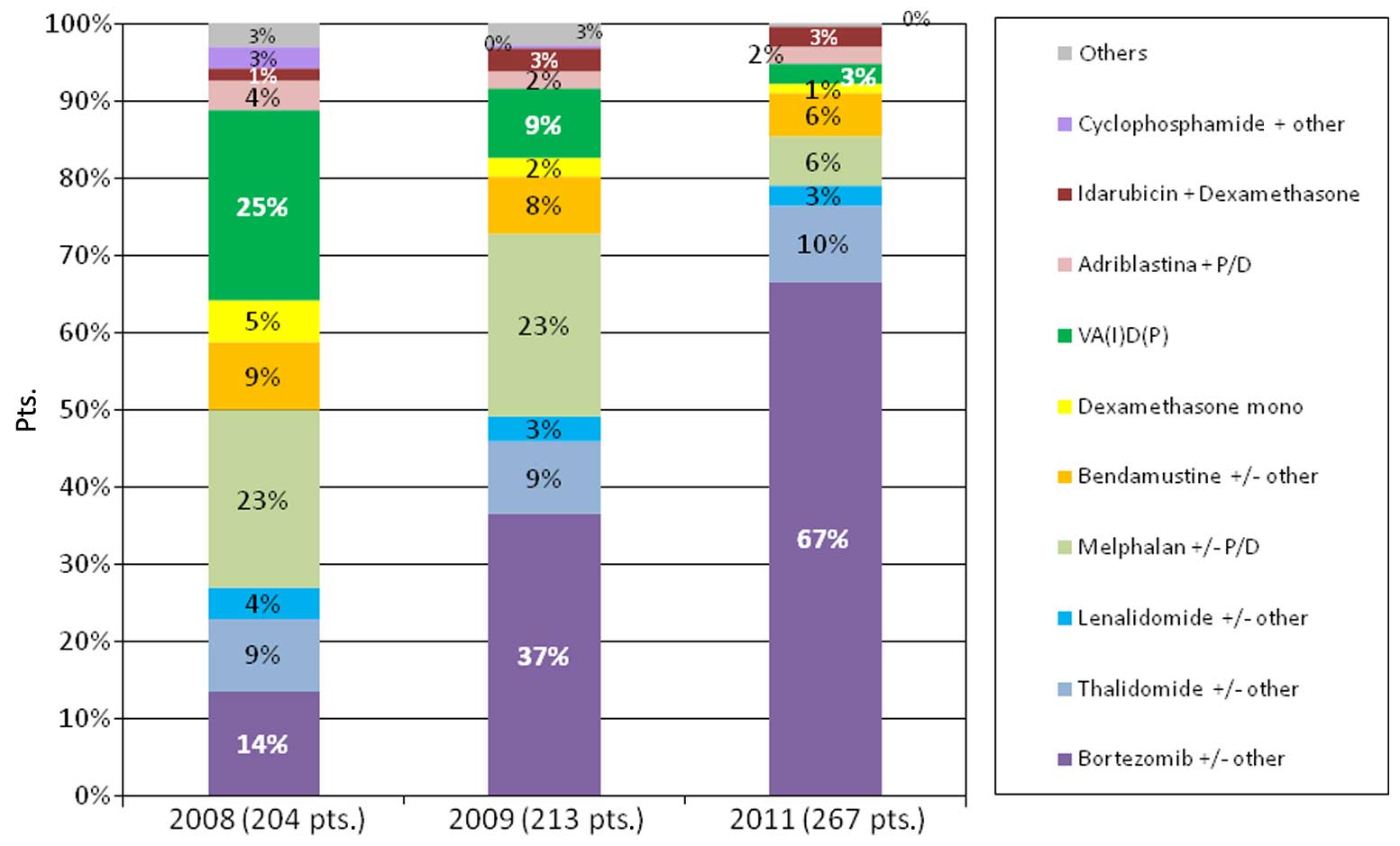
There was a remarkable shift in the treatment of
first-line patients during 2008–2011. The change in the first-line
treatment strategy over time is outlined in Fig. 6. As described, bortezomib combinations
have predominantly substituted all traditional novel-agent-free
chemotherapy regimens, such as melphalan+prednisone and
vincristin+Adriamycin+dexamethasone. Currently, the IMiDs
thalidomide and lenalidomide serve a remarkably constant, but
substantially smaller, role in first-line treatment.
Impact of concomitant disease,
particularly renal impairment, on treatment decisions
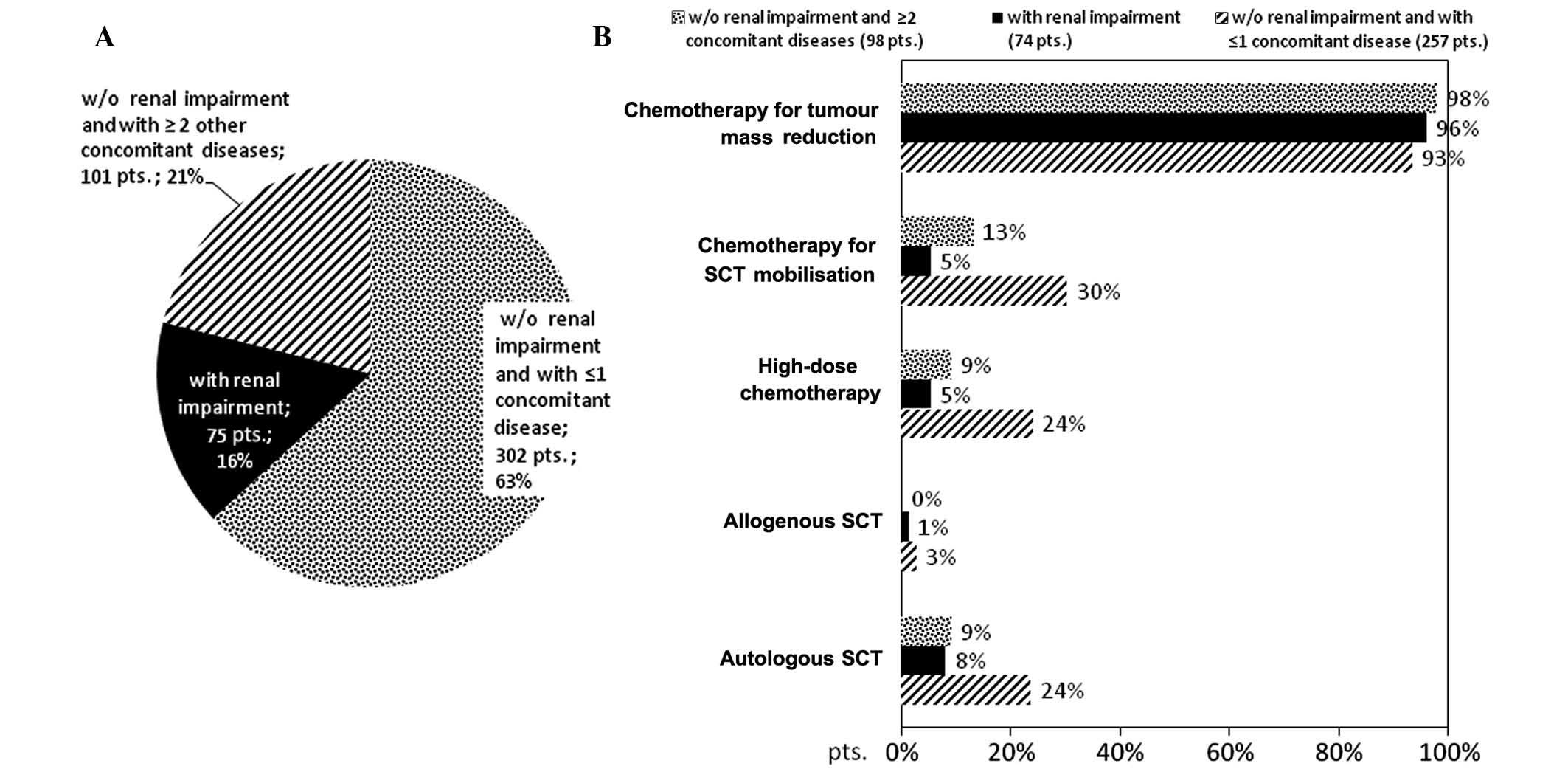
In the current survey, 16% of patients in the
first-line setting suffered from renal impairment (Fig. 7A). For a majority of patients (63%),
no renal impairment and only one concomitant disease was reported,
and multimorbidity without renal impairment was reported in 21% of
patients. The analysis of treatment patterns in these three patient
subgroups revealed a significant (P<0.001) impact of the
morbidity on the treatment pattern. While 27% of patients with ≤1
concomitant disease were treated with ASCT, <10% of patients
with renal impairment or with ≥2 concomitant diseases received ASCT
(Fig. 7B).
As indicated in Fig.
8, the agents used for the treatment of patients with renal
impairment are similar to the agents used for first-line treatment
in patients with normal renal function (P=0.097).
Therapy in first relapse
Fig. 9 indicates the
treatment approach selected for first-relapse. Since bortezomib was
approved (in 2008) and adopted rapidly in the first-line treatment
setting, the number of patients treated with bortezomib in the
second-line setting decreased. A substantial increase in
IMiD-containing, and particularly lenalidomide-containing, regimens
was observed. A switch from bortezomib in the first-line to
lenalidomide was performed, in particular, for patients in whom the
response duration to the bortezomib first-line regimen was <6
months. Overall, therapy with lenalidomide and, to a smaller
extent, thalidomide has become an important aspect of treatment for
relapsed disease. Melphalan+corticosteroid regimens have almost
disappeared from second-line treatment.
Supportive therapy
As expected, >90% of patients received at least
some form of supportive care with first-line treatment. As
indicated in Fig. 10, treatment with
bisphosphonates was the leading supportive care therapy. There
appears to be a declining necessity for additional supportive
therapy since 2008 (Fig. 10); in
particular, there is a trend for reduced use of
erythropoietin-stimulating agents (ESAs), granulocyte
colony-stimulating factor (G-CSF) and substitution of red blood
cells and platelets, respectively. ESA use was reduced by 90%,
while G-CSF, red blood cell and platelet transfusions were reduced
by 50%.
Discussion
The current analysis of data regarding multiple
myeloma patients provides information on real-world treatment and
diagnostic decisions to clarify the information on which regimen
and treatment pathways are currently favoured by clinicians and on
which regimen could be the basis for the future development of
myeloma care.
The patient population was very comparable between
the surveys with regard to participating institutions, covering
office-based haemato-oncologists, non-academic hospitals and
university hospitals. Age range, and the percentages of patients in
each Durie-Salmon stage and asymptomatic patients, were comparable
across the participating institutions. There are four major
findings from the current study:
Firstly, there was a clear increase of cytogenetic
assessment, from 22% of patients analysed in the 2008 survey, to
53% of patients in the current survey. The cytogenetic risk profile
as well as the β2-MG level can be demonstrated to be
integrated into the treatment decisions (12). As age and comorbidity are the most
important factors for selection of treatment regimen, elderly
patients (aged >69 years) with reduced performance status had
the lowest frequency for cytogenetic testing. Thus, treating
physicians demonstrated great consideration towards resource
utilisation in the diagnostic setting.
Secondly, bortezomib-based regimens have become the
standard of care for first-line therapy for German myeloma
patients, regardless of whether the patients are eligible for ASCT,
or are treated in a university hospital or community-based centre.
ASCT for eligible patients is still recognised as an essential
component of therapy. Although novel agents substantially improved
the outcome of first-line therapy, the use of ASCT has not declined
over the past years. Importantly, despite data showing that overall
survival does not differ comparing upfront and delayed ASCT
(13), the following arguments still
favour ASCT for eligible patients: The long treatment-free
interval, the high quality of life following ASCT, and the
possibility for long-term disease-free survival beyond 14 years
(14). In consequence, only 8% of
patients in the current survey received a delayed ASCT procedure
(13,15). The concept of upfront ASCT was
recently validated by Palumbo et al (16) in a randomised phase III study that
demonstrated the advantage of front-line ASCT compared to therapy
with a novel agent-containing regimen. The present survey also
indicates that the decision for ASCT is based on various factors,
including age and myeloma-induced organ dysfunction; this is
unexpected, as most guidelines indicate the decision for ASCT as an
age-dependent decision, but one independent of myeloma-related
disease (17).
Maintenance treatment was used in 24% of patients
subsequent to ASCT, and in 38% of patients within a clinical study.
Several clinical studies suggest that maintenance therapy improves
progression-free survival and overall survival times, despite some
remaining concern regarding the rate of secondary malignancy in
patients undergoing long-term IMiD treatment (18–21).
Overall, we conclude that it is becoming a broader consensus in the
community to focus on improving the response quality and using
maintenance treatment as part of this strategy.
The third important finding from the current study
is that the use/switch of novel agents for relapsed disease is in
line with international standards (2). For patients relapsing within 6 months
after primary therapy, lenalidomide is the most commonly applied
agent; whereas, in patients with prolonged remission after primary
therapy, re-treatment with bortezomib is a considered a valid
option. Furthermore, thalidomide appeared to be used more
frequently in community-based offices as third-line treatment as
compared with university hospitals. This finding may reflect cost
considerations, taking into account the expensiveness of
lenalidomide. Although it has been demonstrated that autologous
re-transplantation is suitable for patients with sustained
remission following initial ASCT (22), the current survey indicates that this
has only a marginal relevance in general practice. The same holds
true for allogeneic transplantation in relapsed disease.
The fourth major finding was that the general need
for supportive care in addition to bisphosphonates declined in the
last years. We hypothesise that the improved treatment outcomes
reduced the requirement for supportive care such as pain relief and
haematopoietic growth factors. It is also likely that the use of
IMiDs, which have an erythrocyte-stimulating side effect,
contributed to this. As economical discussions will go on, it is
important to integrate assessment of quality of life and individual
work performance into phase III and IIIb/IV clinical studies
(8).
With the aforementioned measures, care was taken to
counteract the potential limitations of the data collection
approach in the current study. The consistency of some of the key
parameters, such as patient characteristics, across the treatment
survey indicates that the presented data are robust. In addition,
response data was not presented in this data analysis, as this
information would be largely unreliable and a topic for prospective
clinical studies.
In conclusion, the current study demonstrates a
significant modification of treatment patterns for elderly and
younger multiple myeloma patients based on the findings of
international studies, indicating a rapid adoption of clinical
study results into clinical practice. The survey also indicates
that four-drug combinations in first-line treatment are not well
established.
References
|
1
|
Merz M, Neben K, Raab MS, Sauer S, Egerer
G, Hundemer M, Hose D, Kunz C, Heiß C, Ho AD, et al: Hillengass
Autologous stem cell transplantation for elderly patients with
newly diagnosed multiple myeloma in the era of novel agents. Ann
Oncol. 25:189–195. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ludwig H, Avet-Loiseau H, Bladé J,
Boccadoro M, Cavenagh J, Cavo M, Davies F, de la Rubia J, Delimpasi
S, Dimopoulos M, et al: European perspective on multiple myeloma
treatment strategies: Update following recent congresses.
Oncologist. 17:592–606. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ludwig H, Miguel JS, Dimopoulos MA,
Palumbo A, Sanz R Garcia, Powles R, Lentzsch S, Chen W Ming, Hou J,
Jurczyszyn A, et al: Durie International myeloma working group
recommendations for global myeloma care. Leukemia. 28:981–992.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pulte D, Gondos A and Brenner H:
Improvement in survival of older adults with multiple myeloma:
Results of an updated period analysis of SEER data. Oncologist.
16:1600–1603. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Brenner H, Gondos A and Pulte D: Recent
major improvement in long-term survival of younger patients with
multiple myeloma. Blood. 111:2521–2526. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Klein B, Seckinger A, Moehler T and Hose
D: Molecular pathogenesis of multiple myeloma: Chromosomal
aberrations, changes in gene expression, cytokine networks, and the
bone marrow microenvironment. Recent Results Cancer Res. 183:39–86.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Engelhardt M, Terpos E, Kleber M, Gay F,
Wäsch R, Morgan G, Cavo M, van de Donk N, Beilhack A, Bruno B, et
al: European myeloma network recommendations on the evaluation and
treatment of newly diagnosed patients with multiple myeloma.
Haematologica. 99:232–242. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gaultney JG, Redekop WK, Sonneveld P and
Uyl-de Groot CA: Novel anticancer agents for multiple myeloma: A
review of the evidence for their therapeutic and economic value.
Expert Rev Anticancer Ther. 12:839–854. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Knauf W, Kellermann L, Poenisch W, Einsele
H, Straka C, Frohn C and Goldschmidt H: How to treat multiple
myeloma - a representative multicentre treatment survey. Onkologie.
33:604–610. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Durie BG and Salmon SE: A clinical staging
system for multiple myeloma. Correlation of measured myeloma cell
mass with presenting clinical features, response to treatment, and
survival. Cancer. 36:842–854. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Greipp PR, San Miguel J, Durie BGM,
Crowley JJ, Barlogie B, Blade J, Boccadoro M, Child A, Avet-Loiseau
H, Kyle RA, et al: International staging system for multiple
myeloma. J Clin Oncol. 23:3412–3420. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Moreau P, Cavo M, Sonneveld P, Rosinol L,
Attal M, Pezzi A, Goldschmidt H, Lahuerta JJ, Marit G, Palumbo A,
et al: Combination of international scoring system 3, high lactate
dehydrogenase and t (4;14) and/or del (17p) identifies patients
with multiple myeloma (MM) treated with front-line autologous
stem-cell transplantation at high risk of early MM
progression-related death. J Clin Oncol. 32:2173–2180. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fermand JP, Ravaud P, Chevret S, Divine M,
Leblond V, Belanger C, Macro M, Pertuiset E, Dreyfus F, Mariette X,
et al: High-dose therapy and autologous peripheral blood stem cell
transplantation in multiple myeloma: Up-front or rescue treatment?
Results of a multicenter sequential randomized clinical trial.
Blood. 92:3131–3136. 1998.PubMed/NCBI
|
|
14
|
van Rhee F, Giralt S and Barlogie B: The
future of autologous stem cell transplantation in myeloma. Blood.
124:328–333. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fermand JP, Katsahian S, Divine M, Leblond
V, Dreyfus F, Macro M, Arnulf B, Royer B, Mariette X, Pertuiset E,
et al: High-dose therapy and autologous blood stem-cell
transplantation compared with conventional treatment in myeloma
patients aged 55 to 65 years: Long-term results of a randomized
control trial from the Group Myelome-Autogreffe. J Clin Oncol.
23:9227–9233. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Palumbo A, Cavallo F, Gay F, Di Raimondo
F, Ben Yehuda D, Petrucci MT, Pezzatti S, Caravita T, Cerrato C,
Ribakovsky E, et al: Autologous transplantation and maintenance
therapy in multiple myeloma. N Engl J Med. 371:895–905. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ludwig H, Beksac M, Bladé J, Boccadoro M,
Cavenagh J, Cavo M, Dimopoulos M, Drach J, Einsele H, Facon T, et
al: Current multiple myeloma treatment strategies with novel
agents: A European perspective. Oncologist. 15:6–25. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sonneveld P, Schmidt-Wolf IG, van der Holt
B, El Jarari L, Bertsch U, Salwender H, Zweegman S, Vellenga E,
Broyl A, Blau IW, et al: Bortezomib induction and maintenance
treatment in patients with newly diagnosed multiple myeloma:
Results of the randomized phase III HOVON-65/ GMMG-HD4 trial. J
Clin Oncol. 30:2946–2955. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Palumbo A, Hajek R, Delforge M, Kropff M,
Petrucci MT, Catalano J, Gisslinger H, Wiktor-Jędrzejczak W,
Zodelava M, Weisel K, et al: Continuous lenalidomide treatment for
newly diagnosed multiple myeloma. N Engl J Med. 366:1759–1769.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
McCarthy PL, Owzar K, Hofmeister CC, Hurd
DD, Hassoun H, Richardson PG, Giralt S, Stadtmauer EA, Weisdorf DJ,
Vij R, et al: Lenalidomide after stem-cell transplantation for
multiple myeloma. N Engl J Med. 366:1770–1781. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Palumbo A, Bringhen S, Kumar SK,
Lupparelli G, Usmani S, Waage A, Larocca A, van der Holt B, Musto
P, Offidani M, et al: Second primary malignancies with lenalidomide
therapy for newly diagnosed myeloma: A meta-analysis of individual
patient data. Lancet Oncol. 15:333–342. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sellner L, Heiss C, Benner A, Raab MS,
Hillengass J, Hose D, Lehners N, Egerer G, Ho AD, Goldschmidt H and
Neben K: Autologous retransplantation for patients with recurrent
multiple myeloma: A single-center experience with 200 patients.
Cancer. 119:2438–2446. 2013. View Article : Google Scholar : PubMed/NCBI
|