Introduction
Colorectal cancer (CRC) is the third most common
cancer and fourth leading cause of cancer-associated mortality
worldwide (1). Despite advances in
surgical procedures and adjuvant chemotherapy, 20–25% of patients
still experience relapse following curative surgery (2). The Union for International Cancer
Control (UICC) tumor node metastasis (TNM) staging system (3) is currently the most reliable indicator
of patient prognosis and is widely used amongst practitioners.
However, there are differences in patient prognosis even within the
same TNM stage. Therefore, more reliable markers are required to
improve predictions of cancer recurrence and patient survival.
It has previously been reported that inflammation is
important in determining cancer progression (4,5).
Inflammation-based indices, such as the C-reactive protein level,
Glasgow prognostic score, and neutrophil-to-lymphocyte ratio; are
useful for predicting the prognosis of patients with CRC as well as
various other types of cancer (6–9). Recent
studies investigating various types of malignancies have
demonstrated a correlation between the lymphocyte-to-monocyte ratio
(LMR), which also reflects the degree of systemic inflammation, and
patient survival (10–14). However, the prognostic value of the
LMR has mainly been investigated in patients with hematological
malignancies, with few reports focusing on patients with solid
tumors. Therefore, the aim of this retrospective study was to
evaluate the prognostic significance of preoperative LMR in
patients with CRC who are able to undergo potentially curative
surgery.
Materials and methods
Patients
A total of 189 patients with CRC were enrolled. All
patients underwent potentially curative surgery for CRC in the
Department of Surgical Oncology, Osaka City University, between
January 2007 and December 2009. Patients who received preoperative
therapy, underwent emergency surgery for perforation/obstruction,
or who had inflammatory bowel disease were excluded from the
study.
The patient characteristics are presented in
Table I. Included in the study were
107 males and 82 females, and median patient age at initial surgery
was 68 years old (range, 26–86 years old). A total of 112 patients
had primary tumors located in the colon and 77 had primary tumors
located in the rectum. Resected specimens were pathologically
classified according to the UICC TNM classification of malignant
tumors, ver. 7 (3). The distribution
of cancer stages was as follows: stage I, 63; stage II, 65; stage
III, 61 patients. All patients underwent regular physical
examinations and blood tests. The levels of tumor markers, such as
carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9
(CA19-9), were measured, and mandatory screening was performed
using colonoscopy and computed tomography until December 2014 (60
months following surgery) or patient mortality.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Characteristic | No. patients |
|---|
| Gender |
|
| Male | 107 |
|
Female | 82 |
| Age, years |
|
| Median
(range) | 68 (26–86) |
| Location of primary
tumor |
|
|
Colon | 112 |
|
Rectum | 77 |
| Tumor depth |
|
| T1-3 | 150 |
| T4 | 39 |
| Tumor diameter,
cm |
|
| Median
(range) | 4.0 (0.2–11.0) |
| Histological
type |
|
| Well or
moderately differentiated | 169 |
| Poorly
differentiated or mucinous | 16 |
| Lymphatic
involvement |
|
|
Negative | 76 |
|
Positive | 113 |
| Venous
involvement |
|
|
Negative | 163 |
|
Positive | 21 |
| Lymph node
metastases |
|
|
Negative | 126 |
|
Positive | 63 |
| Stagea |
|
| I | 63 |
| II | 65 |
|
III | 61 |
| Lymphocyte count,
per mm3 |
|
| Median
(range) | 1690
(432–3891) |
| Monocyte count, per
mm3 |
|
| Median
(range) | 324 (28–792) |
Blood sample analysis
Preoperative blood samples were obtained at the time
of diagnosis prior to surgery. The differential white blood cell
count was analyzed using the Sysmex XE-5000 automated hematology
analyzer™ (Sysmex, Kobe, Japan) following the manufacturer
protocol. LMR was calculated from the preoperative blood samples by
dividing the absolute lymphocyte count by the absolute monocyte
count.
Statistical analysis
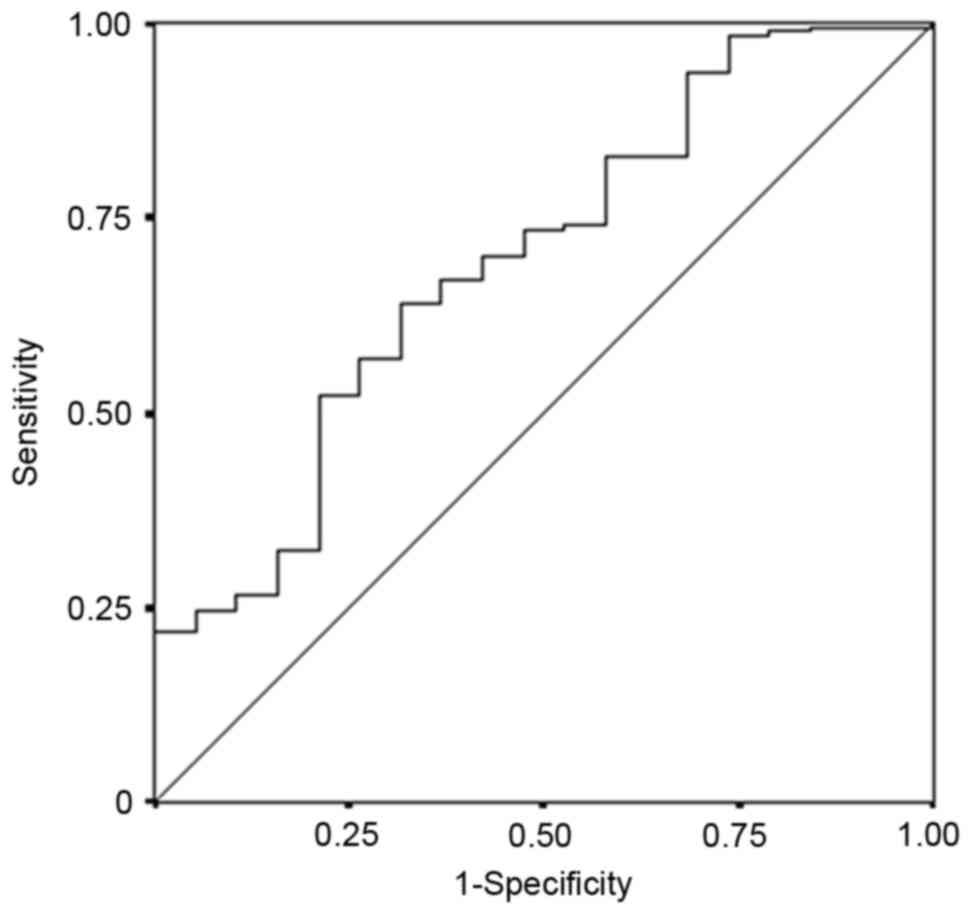
A receiver operating characteristic (ROC) curve was
used to determine an appropriate cut-off value. All patients were
classified into two groups according to the preoperative LMR. The
significance of associations between preoperative LMR and
clinicopathological characteristics was analyzed using
χ2 test and Fisher's exact test. Duration of survival
was calculated according to the Kaplan-Meier method. Differences
between survival curves were assessed with the log-rank test. A
multivariate analysis was performed according to the Cox
proportional hazards model, and all statistical analyses were
performed using the SPSS software package (SPSS Inc., Tokyo,
Japan). P<0.05 was considered to indicate a statistically
significant difference.
Ethical considerations
The current study conformed to the provisions of the
Declaration of Helsinki and was approved by the ethics committee of
Osaka City University. All patients were informed of the
investigational nature of this study and provided written informed
consent.
Results
Survival analysis according to the
lymphocyte/monocyte count
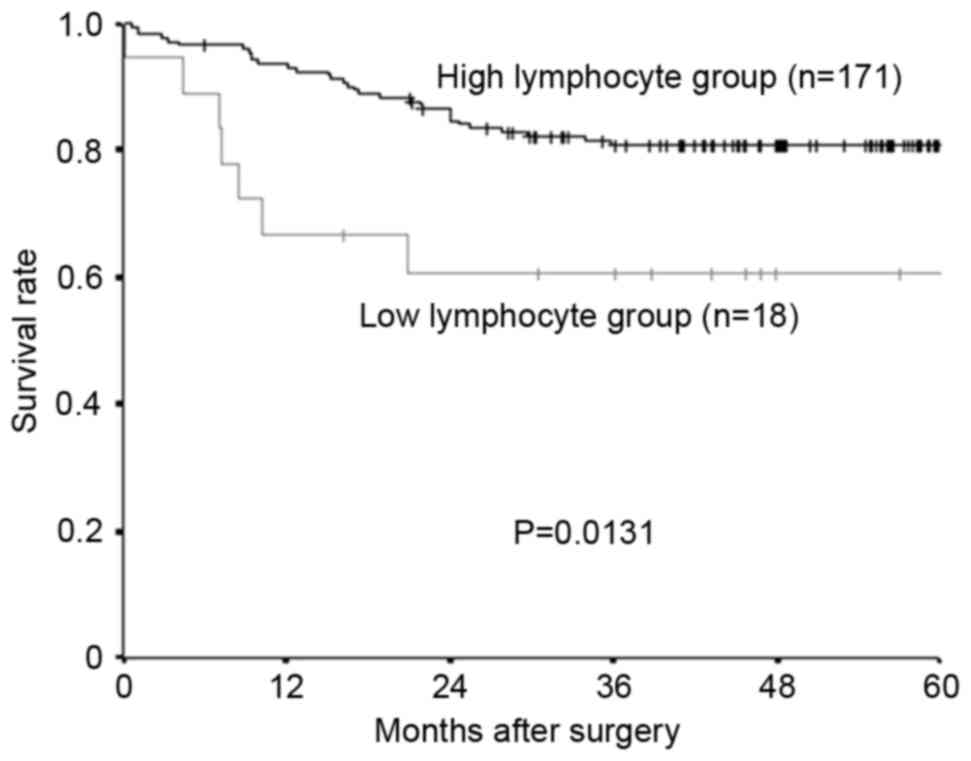
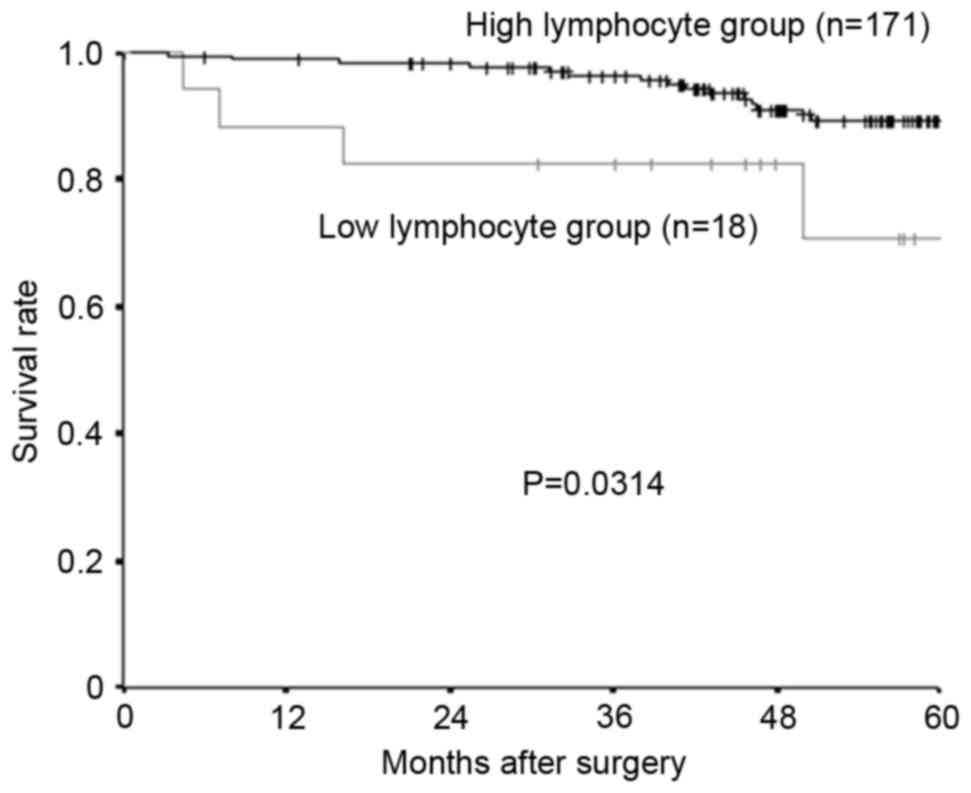
The median preoperative lymphocyte count was
1,690/mm3 (range, 432–3,891), and 1,000 mm3
was set as the cut-off value, in accordance with previous studies
(15). Following the lymphocyte
count, 171 patients were placed into the high-lymphocyte group and
18 patients into the low-lymphocyte group. Relapse-free survival
rate and overall survival rate were significantly lower in the
low-lymphocyte group compared with the high-lymphocyte group
(Fig. 1, relapse-free survival;
P=0.0131; Fig. 2, overall survival;
P=0.0314).
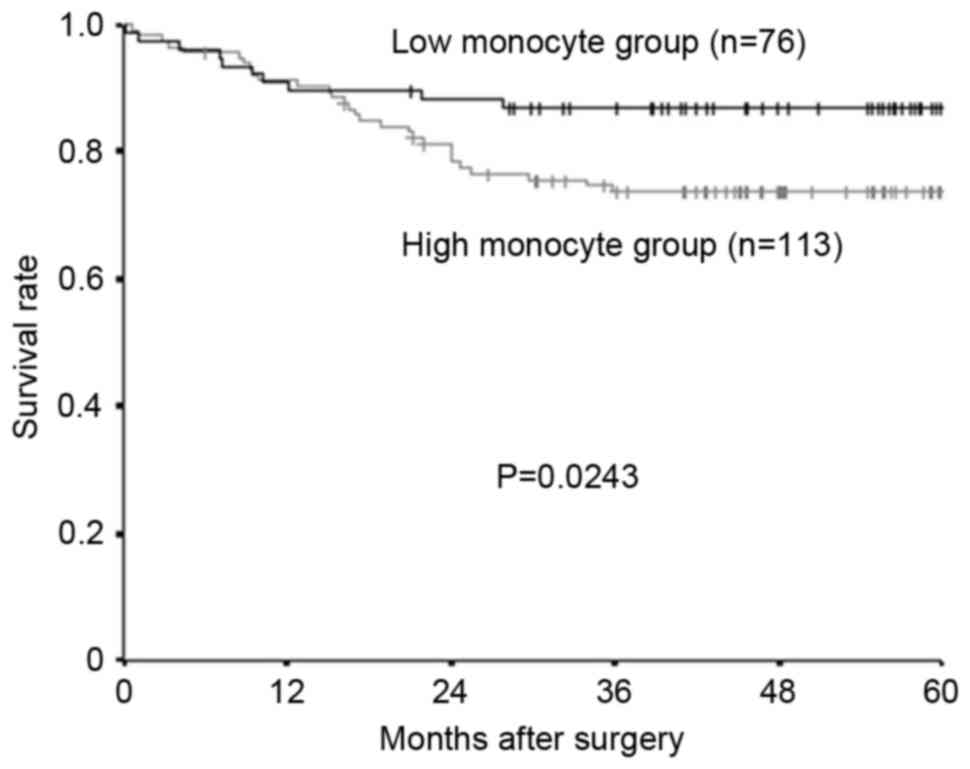
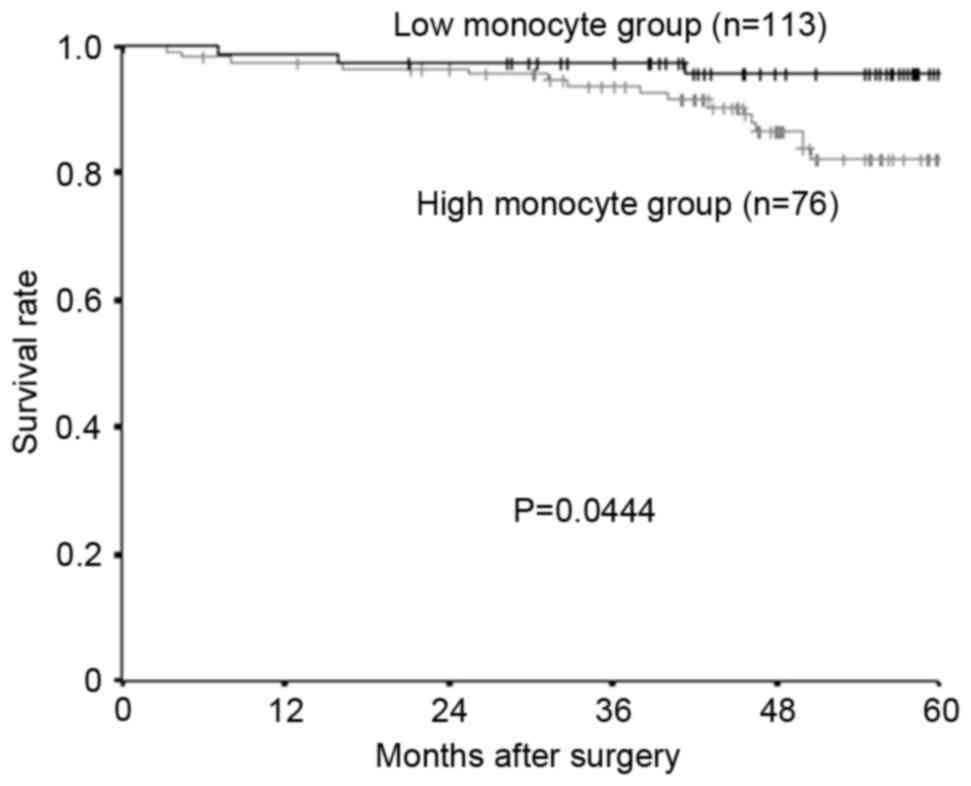
The median preoperative monocyte count was
324/mm3 (range, 28–792), and 300 was set as the cut-off
value, based on previous reports (16). A total of 76 patients were placed into
the high-monocyte group and 113 patients into the low-monocyte
group. Both the relapse-free survival rate and the overall survival
rate were significantly lower in the high-monocyte group compared
with the low-monocyte group (Fig. 3,
relapse-free survival; P=0.0243; Fig.
4, overall survival; P=0.0444).
Cut-off value for the LMR
The median preoperative LMR was 5.429 (range,
1.494–57.500). The continuous variable LMR was used as the test
variable and the 5-year rate survival as the state variable. The
cut-off value for the preoperative LMR was investigated using the
ROC curve, and was determined as 4.8 (the sensitivity was 64.1% and
the specificity was 63.2%; Fig. 5).
Based on this cut-off value, 116 patients were classified into the
high-LMR group and 73 patients were classified into the low-LMR
group.
Correlation between the LMR and
clinicopathological parameters
The associations between preoperative LMR and
clinicopathological parameters are shown in Table II. The only significant relationship
identified was between preoperative LMR and lymphatic involvement
(P=0.013, Table II).
 | Table II.Associations between preoperative LMR
and clinicopathological factors. |
Table II.
Associations between preoperative LMR
and clinicopathological factors.
|
| LMR |
|---|
|
|
|
|---|
| Factors | High | Low | P-value |
|---|
| Age, years |
|
| 0.073 |
|
<70 | 70 | 34 |
|
|
≥70 | 46 | 39 |
|
| Gender |
|
| 0.099 |
|
Male | 60 | 47 |
|
|
Female | 56 | 26 |
|
| Tumor location |
|
| 0.880 |
|
Colon | 68 | 44 |
|
|
Rectum | 48 | 29 |
|
| Tumor depth |
|
| 0.196 |
|
T1-3 | 96 | 54 |
|
| T4 | 20 | 19 |
|
| Tumor diameter,
cm |
|
| 0.063 |
|
<5 | 75 | 37 |
|
| ≥5 | 38 | 34 |
|
| Histological
type |
|
| 0.789 |
|
Well/moderately
differentiated | 105 | 64 |
|
| Poorly
differentiated/mucinous | 9 | 7 |
|
| Lymphatic
involvement |
|
| 0.013 |
|
Negative | 52 | 19 |
|
|
Positive | 61 | 52 |
|
| Venous
involvement |
|
| 0.352 |
|
Negative | 98 | 65 |
|
|
Positive | 15 | 6 |
|
| Lymph node
metastasis |
|
| 0.156 |
|
Negative | 82 | 44 |
|
|
Positive | 34 | 29 |
|
| Preoperative CEA
(>5 ng/ml) |
|
| 1.000 |
|
Negative | 77 | 47 |
|
|
Positive | 38 | 24 |
|
| Stagea |
|
| 0.139 |
| I | 44 | 19 |
|
| II | 40 | 25 |
|
|
III | 32 | 29 |
|
| Adjuvant
chemotherapy |
|
| 0.881 |
| No | 64 | 39 |
|
|
Yes | 52 | 34 |
|
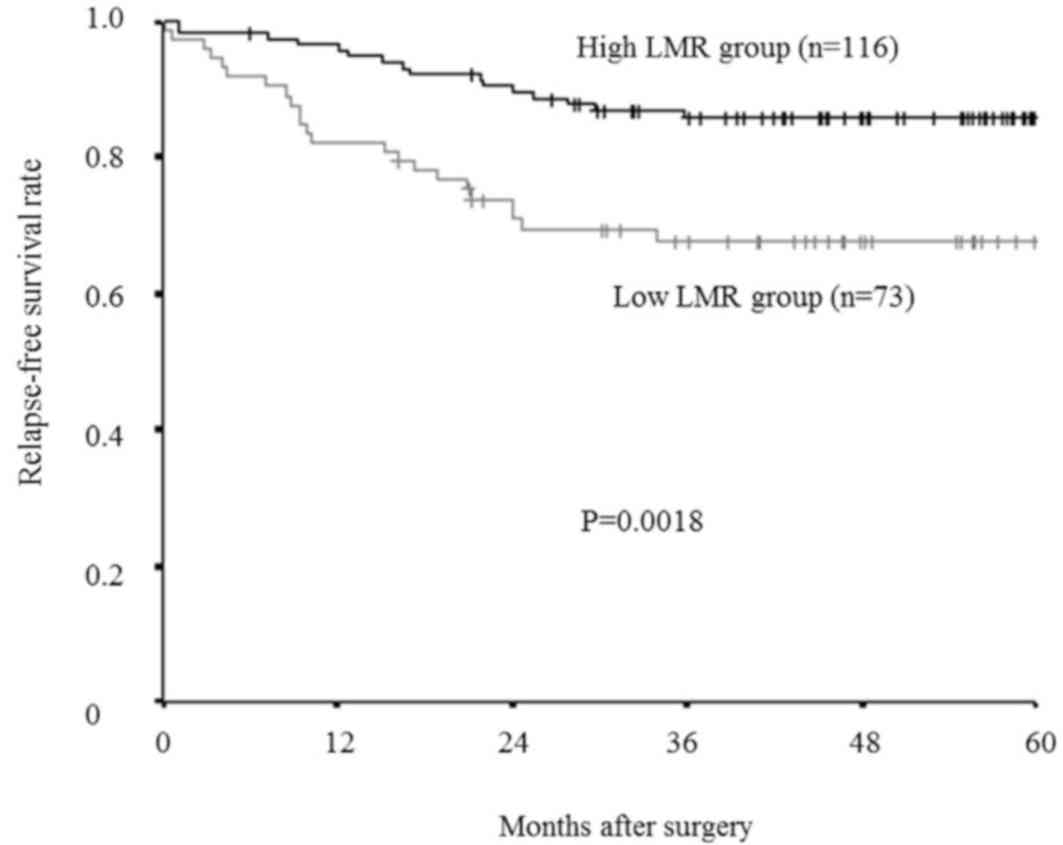
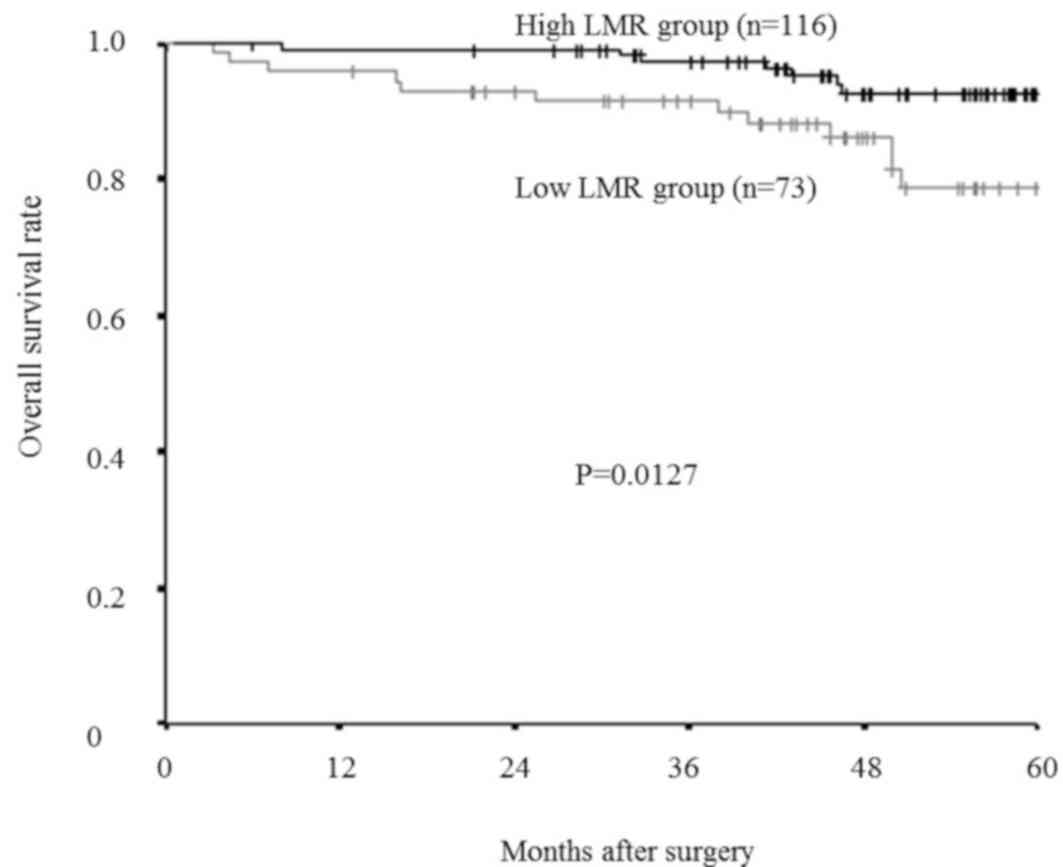
Survival analysis according to the
LMR
The relapse-free survival rate was significantly
lower in the low-LMR group compared with that of the high-LMR group
(P=0.0018; Fig. 6), as was overall
survival rate (P=0.0127; Fig. 7).
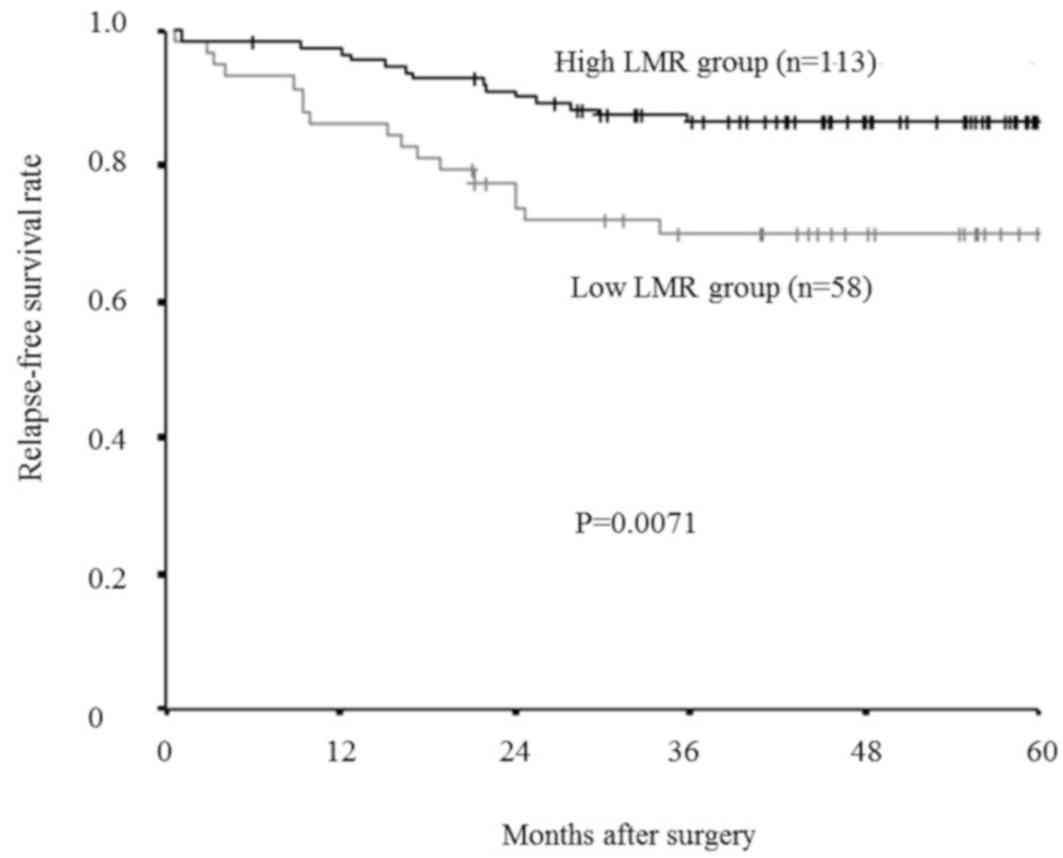
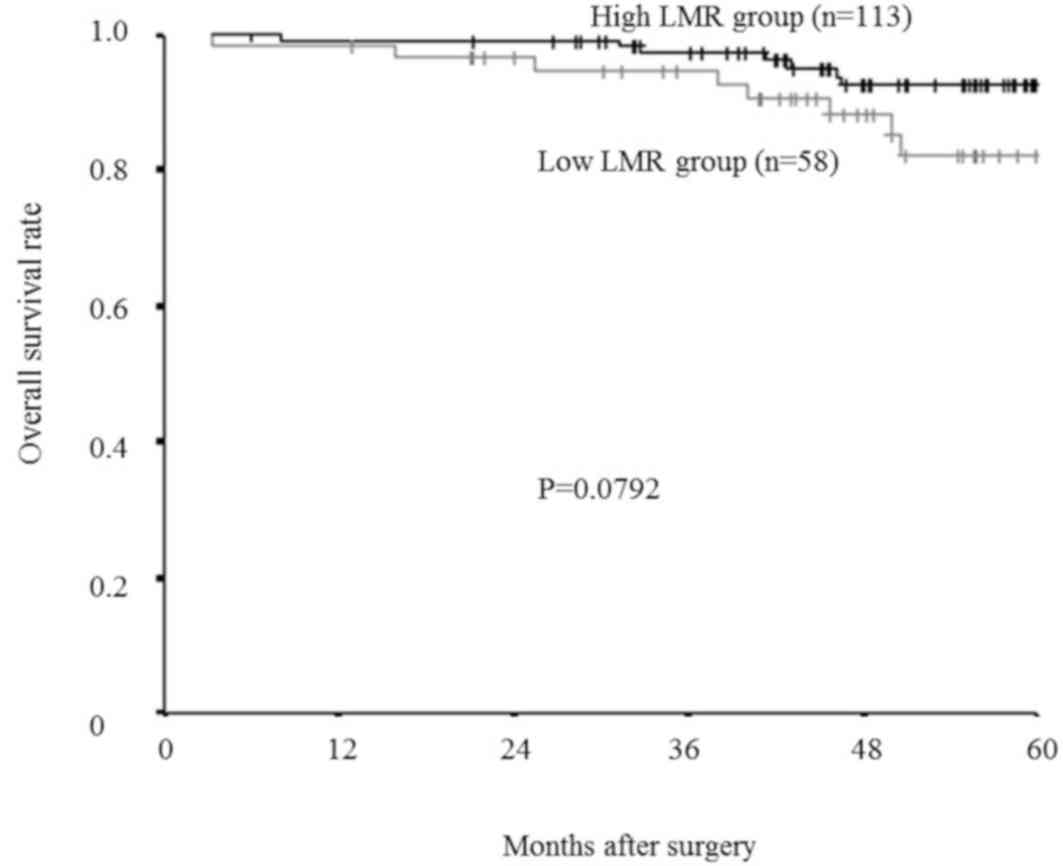
Furthermore, even in an analysis limited to the
patients with a normal lymphocyte count (>1,000/mm3),
relapse-free survival rate was significantly lower in the low-LMR
group than in the high-LMR group (P=0.0071; Fig. 8), and overall survival rate tended to
be lower in the low-LMR group than in the high-LMR group, though
this difference was not significant. (P=0.0792; Fig. 9).
Prognostic factors influencing
relapse-free/overall survival
The associations between relapse-free survival and
various clinicopathological factors are presented in Table III. According to a univariate
analysis, there were significant correlations between relapse-free
survival and tumor diameter, histological type, lymphatic
involvement, lymph node metastasis, preoperative CEA levels and the
preoperative LMR (all P<0.05). Multivariate analysis indicated
that only preoperative LMR was an independent risk factor for a
poor relapse-free survival. The associations between overall
survival and various clinicopathological factors are presented in
Table IV. According to a univariate
analysis, there were significant correlations between overall
survival and both lymph node metastasis and preoperative LMR. In
addition, a multivariate analysis indicated that lymph node
metastasis and preoperative LMR were independent risk factors for
poor overall survival.
 | Table III.Associations between relapse-free
survival and various clinicopathological factors. |
Table III.
Associations between relapse-free
survival and various clinicopathological factors.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Factors | Hazard Ratio | 95% CI | P-value | Hazard Ratio | 95% CI | P-value |
|---|
| Age (>70 years
vs. ≤70 years) | 1.433 | 0.764–2.685 | 0.262 |
|
|
|
| Gender (female vs.
male) | 1.575 | 0.809–3.064 | 0.181 |
|
|
|
| Location of primary
tumor (rectum vs. colon) | 1.545 | 0.824–2.985 | 0.175 |
|
|
|
| Tumor depth (T4 vs.
T1-3) | 1.396 | 0.680–2.865 | 0.363 |
|
|
|
| Tumor diameter
(>5 cm vs. ≤5 cm) | 2.421 | 1.256–4.669 | 0.008 | 1.259 | 0.597–2.655 | 0.546 |
| Histological type
(poor, mucinous vs. well, moderately) | 2.777 | 1.222–6.308 | 0.015 | 1.607 | 0.678–3.805 | 0.281 |
| Lymphatic
involvement (positive vs. negative) | 3.211 | 1.417–7.276 | 0.005 | 1.946 | 0.676–5.600 | 0.217 |
| Venous involvement
(positive vs. negative) | 1.782 | 0.787–4.039 | 0.166 |
|
|
|
| Lymph node
metastasis (positive vs. negative) | 3.362 | 1.775–6.366 |
<0.001 | 2.041 | 0.904–4.606 | 0.086 |
| Preoperative CEA
(>5 ng/ml vs. ≤5 ng/ml) | 2.590 | 1.369–4.899 | 0.003 | 1.923 | 0.913–4.054 | 0.086 |
| Preoperative LMR
(≥4.8 vs. <4.8) | 2.657 | 1.403–5.033 | 0.003 | 2.051 | 1.028–4.090 | 0.041 |
 | Table IV.Correlations between overall survival
and various clinicopathological factors. |
Table IV.
Correlations between overall survival
and various clinicopathological factors.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Factors | Hazard Ratio | 95% CI | P-value | Hazard ratio | 95% CI | P-value |
|---|
| Age (>70 years
vs. ≤70 years) | 1.386 | 0.562–3.416 | 0.479 |
|
|
|
| Gender (female vs.
male) | 1.713 | 0.651–4.508 | 0.275 |
|
|
|
| Location of primary
tumor (rectum vs. colon) | 1.909 | 0.767–4.748 | 0.164 |
|
|
|
| Tumor depth (T4 vs.
T1-3) | 0.689 | 0.201–2.365 | 0.553 |
|
|
|
| Tumor diameter
(>5 cm vs. ≤5 cm) | 1.224 | 0.492–3.047 | 0.664 |
|
|
|
| Histological type
(poor, mucinous vs. well, moderate) | 1.172 | 0.271–5.078 | 0.832 |
|
|
|
| Lymphatic
involvement (positive vs. negative) | 2.379 | 0.790–7.169 | 0.124 |
|
|
|
| Venous involvement
(positive vs. negative) | 2.663 | 0.959–7.396 | 0.060 |
|
|
|
| Lymph node
metastasis (positive vs. negative) | 2.814 | 1.132–6.996 | 0.026 | 2.533 | 1.014–6.328 | 0.047 |
| Preoperative CEA
(>5 ng/ml vs. ≤5 ng/ml) | 2.008 | 0.815–4.946 | 0.130 |
|
|
|
| The preoperative
LMR (≥4.8 vs. <4.8) | 3.081 | 1.212–7.830 | 0.018 | 2.805 | 1.098–7.163 | 0.031 |
Discussion
Inflammation and cancer are closely related.
Inflammation is caused not only by the systemic reaction of the
host to the tumor, but also by inflammatory cytokines and
chemokines released by cancer cells, and tumor-associated
leukocytes that cause tumor growth, invasion, metastasis and
suppression of the host immune system (4,5,17,18). Thus,
inflammation reflects cancer progression, and the significance of
systemic inflammatory markers in predicting the survival of
patients with CRC, as well as other malignancies, has previously
been reported. LMR, which consists of the peripheral lymphocyte and
monocyte counts, also reflects systemic inflammation.
Lymphocytes serve an important role in tumor
suppression. Previous studies have demonstrated a correlation
between lymphopenia and poor prognosis of patients with various
types of cancer (15,19). Lymphocytes induce cytotoxic cell death
and produce cytokines that inhibit cancer cell proliferation and
metastatic activity (4,20,21). The
absolute peripheral lymphocyte count is assumed to reflect the
degree of responsiveness of the entire immune system of a patient
(15,22). Therefore, a low peripheral lymphocyte
count may result in a weak and insufficient immunological reaction
to the tumor, thus promoting tumor progression and metastasis
(23).
By contrast, monocytes play an important role in
tumor progression (4,24). A correlation between monocytosis and
poor prognosis in different types of cancer has previously been
observed (16,25–27).
Monocytes represent a source of chemokines and cytokines that
contribute to inflammation (28).
Inflammation in the cancer microenvironment promotes tumor
progression and metastasis (29).
Moreover, tumor-associated macrophages (TAMs), derived from
circulating monocytes (30), cause
migration, intravasation, tumor cell invasion, tumor-associated
angiogenesis, and the suppression of the anti-tumor immune system
(4,31–33). The
absolute peripheral monocyte count reflects the formation and/or
presence of TAMs (34), thus a high
peripheral monocyte count is responsible for a high tumor burden.
Therefore, low LMR reflects insufficient antitumor immunity and an
elevated tumor burden, and is associated with poor patient
prognosis.
In previous studies, both the lymphocyte and the
monocyte count have been reported as prognostic factors for the
survival of patients with various malignancies, and this was
confirmed in the present study. Furthermore, the prognostic
significance of LMR was investigated, and was demonstrated to be an
accurate prognostic marker. Even in an analysis limited to patients
with a normal lymphocyte count, the LMR identified patients with a
poor prognosis. Therefore, the LMR is considered to be a more
accurate prognostic marker than the lymphocyte count alone.
The cut-off value for the LMR used in the present
study was different from that of previous studies. A cut-off value
of 4.8 was set based on a ROC analysis, and was higher than cut-off
values used in previous studies, which ranged between 2.14–4.19
(12–14,35). Thus,
although LMR is a useful prognostic marker for various solid
tumors, the optimum cut-off value for the LMR may differ according
to the organ, stage or end point (such as disease-free survival,
progression-free survival or overall survival).
There are several limitations associated with the
present study: i) A relatively small number of patients were
evaluated; ii) the study design was retrospective; iii) the results
obtained were not validated in another population; iv) potential
confounding factors, such as infection, ischemia or acute coronary
disease, which may affect the white blood cell count, were not
assessed; v) the optimum cut-off value for the preoperative LMR
remains unknown, although 4.8 was set as the cut-off value using
the results of a ROC analysis. Therefore, a large prospective study
is required to confirm the findings of the current study.
In conclusion, preoperative LMR may be a useful
prognostic marker in patients with CRC able to undergo potentially
curative surgery, and assessing the LMR may enable more informed
decisions regarding choice of therapeutic strategies to be made. It
is quick and easy to obtain a peripheral blood cell count,
therefore, measuring preoperative LMR may become a novel clinical
biomarker for patients with CRC.
Acknowledgements
The authors thank Brian Quinn, who provided medical
writing services on behalf of JMC, Ltd.
References
|
1
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: Estimates of worldwide burden of cancer in
2008: GLOBOCAN 2008. Int J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Edge S, Byrd D, Compton C, Fritz A, Greene
F and Trotti A: AJCC Cancer Staging Manual. 7th. Springer; New
York: pp. 237–246. 2010
|
|
3
|
Sobin LH, Gospodarowicz MK and Wittekind
C: UICC. TNM Classification of Malignant Tumors. 7. Wiley-Liss; New
York: 2009
|
|
4
|
Mantovani A, Allavena P, Sica A and
Balkwill F: Cancer-related inflammation. Nature. 454:436–444. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Balkwill F and Mantovani A: Inflammation
and cancer: Back to Virchow? Lancet. 357:539–545. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shibutani M, Maeda K, Nagahara H, Ohtani
H, Sugano K, Ikeya T, Kimura K, Amano R, Kubo N, Tanaka H, et al:
Elevated preoperative serum C-reactive protein levels are
associated with poor survival in patients with colorectal cancer.
Hepatogastroenterology. 61:2236–2240. 2014.PubMed/NCBI
|
|
7
|
Shibutani M, Maeda K, Nagahara H, Noda E,
Ohtani H, Nishiguchi Y and Hirakawa K: A high preoperative
neutrophil- to-lymphocyte ratio is associated with poor survival in
patients with colorectal cancer. Anticancer Res. 33:3291–3294.
2013.PubMed/NCBI
|
|
8
|
Walsh SR, Cook EJ, Goulder F, Justin TA
and Keeling NJ: Neutrophil-lymphocyte ratio as a prognostic factor
in colorectal cancer. J Surg Oncol. 91:181–184. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Maeda K, Shibutani M, Otani H, Nagahara H,
Sugano K, Ikeya T, Amano R, Kimura K, Sakurai K, Kubo N, et al:
Prognostic value of preoperative inflammation-based prognostic
scores in patients with stage IV colorectal cancer who undergo
palliative resection of asymptomatic primary tumors. Anticancer
Res. 33:5567–5573. 2013.PubMed/NCBI
|
|
10
|
Li YL, Pan YY, Jiao Y, Ning J, Fan YG and
Zhai ZM: Peripheral blood lymphocyte/monocyte ratio predicts
outcome for patients with diffuse large B cell lymphoma after
standard first-line regimens. Ann Hematol. 93:617–626. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Porrata LF, Ristow K, Habermann TM, Witzig
TE, Colgan JP, Inwards DJ, Ansell SM, Micallef IN, Johnston PB,
Nowakowski GS, et al: Peripheral blood lymphocyte/monocyte ratio at
diagnosis and survival in nodular lymphocyte-predominant Hodgkin
lymphoma. Br J Haematol. 157:321–330. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Stotz M, Pichler M, Absenger G, Szkandera
J, Arminger F, Schaberl-Moser R, Samonigg H, Stojakovic T and
Gerger A: The preoperative lymphocyte to monocyte ratio predicts
clinical outcome in patients with stage III colon cancer. Br J
Cancer. 110:435–440. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Huang Y and Feng JF: Low preoperative
lymphocyte to monocyte ratio predicts poor cancer-specific survival
in patients with esophageal squamous cell carcinoma. Onco Targets
Ther. 8:137–145. 2015.PubMed/NCBI
|
|
14
|
Hu P, Shen H, Wang G, Zhang P, Liu Q and
Du J: Prognostic significance of systemic inflammation-based
lymphocyte- monocyte ratio in patients with lung cancer: Based on a
large cohort study. PLoS One. 9:e1080622014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cézé N, Thibault G, Goujon G, Viguier J,
Watier H, Dorval E and Lecomte T: Pre-treatment lymphopenia as a
prognostic biomarker in colorectal cancer patients receiving
chemotherapy. Cancer Chemother Pharmacol. 68:1305–1313. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sasaki A, Iwashita Y, Shibata K, Matsumoto
T, Ohta M and Kitano S: Prognostic value of preoperative peripheral
blood monocyte count in patients with hepatocellular carcinoma.
Surgery. 139:755–764. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Balkwill FR: The chemokine system and
cancer. J Pathol. 226:148–157. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Guthrie GJ, Roxburgh CS, Horgan PG and
McMillan DC: Does interleukin-6 link explain the link between
tumour necrosis, local and systemic inflammatory responses and
outcome in patients with colorectal cancer? Cancer Treat Rev.
39:89–96. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ray-Coquard I, Cropet C, Van Glabbeke M,
Sebban C, Le Cesne A, Judson I, Tredan O, Verweij J, Biron P,
Labidi I, et al: Lymphopenia as a prognostic factor for overall
survival in advanced carcinomas, sarcomas, and lymphomas. Cancer
Res. 69:5383–5391. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Terzié J, Grivennikov S, Karin E and Karin
M: Inflammation and colon cancer. Gastroenterology. 138:2101–2114.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lin EY and Pollard JW: Role of infiltrated
leucocytes in tumour growth and spread. Br J Cancer. 90:2053–2058.
2010. View Article : Google Scholar
|
|
22
|
Kitayama J, Yasuda K, Kawai K, Sunami E
and Nagawa H: Circulating lymphocyte is an important determinant of
the effectiveness of preoperative radiotherapy in advanced rectal
cancer. BMC Cancer. 11:642011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hoffmann TK, Dworacki G, Tsukihiro T,
Meidenbauer N, Gooding W, Johnson JT and Whiteside TL: Spontaneous
apoptosis of circulating T lymphocytes in patients with head and
neck cancer and its clinical importance. Clin Cancer Res.
8:2553–2562. 2002.PubMed/NCBI
|
|
24
|
Evani SJ, Prabhu RG, Gnanaruban V, Finol
EA and Ramasubramanian AK: Monocytes mediate metastatic breast
tumor cell adhesion to endothelium under flow. FASEB J.
27:3017–3029. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sasaki A, Kai S, Endo Y, Iwaki K, Uchida
H, Tominaga M, Okunaga R, Shibata K, Ohta M and Kitano S:
Prognostic value of preoperative peripheral blood monocyte count in
patients with colorectal liver metastasis after liver resection. J
Gastrointest Surg. 11:596–602. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Haruki K, Shiba H, Fujiwara Y, Furukawa K,
Wakiyama S, Ogawa M, Ishida Y, Misawa T and Yanaga K: Perioperative
change in peripheral blood monocyte count may predict prognosis in
patients with colorectal liver metastasis after hepatic resection.
J Surg Oncol. 106:31–35. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lee YY, Choi CH, Sung CO, Do IG, Huh S,
Song T, Kim MK, Kim HJ, Kim TJ, Lee JW, et al: Prognostic value of
pre-treatment circulating monocyte count in patients with cervical
cancer: Comparison with SCC-Ag level. Gynecol Oncol. 124:92–97.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Eruslanov E, Neuberger M, Daurkin I,
Perrin GQ, Algood C, Dahm P, Rosser C, Vieweg J, Gilbert SM and
Kusmartsev S: Circulating and tumor-infiltrating myeloid cell
subsets in patients with bladder cancer. Int J Cancer.
130:1109–1119. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Landskron G, De la Fuente M, Thuwajit P,
Thuwajit C and Hermoso MA: Chronic inflammation and cytokines in
the tumor microenvironment. J Immunol Res. 2014:1491852014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Mantovani A, Bottazzi B, Colotta F,
Sozzani S and Ruco L: The origin and function of tumor-associated
macrophages. Immunol Today. 13:265–270. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Pollard JW: Tumour-educated macrophages
promote tumour progression and metastasis. Nat Rev Cancer. 4:71–78.
2004. View
Article : Google Scholar : PubMed/NCBI
|
|
32
|
Condeelis J and Pollard JW: Macrophages:
Obligate partners for tumor cell migration, invasion, and
metastasis. Cell. 124:263–266. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lievense LA, Bezemer K, Aerts JG and
Hegmans JP: Tumor-associated macrophages in thoracic malignancies.
Lung Cancer. 80:256–262. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Szkandera J, Gerger A, Liegl-Atzwanger B,
Absenger G, Stotz M, Friesenbichler J, Trajanoski S, Stojakovic T,
Eberhard K, Leithner A and Pichler M: The lymphocyte/monocyte ratio
predicts poor clinical outcome and improves the predictive accuracy
in patients with soft tissue sarcomas. Int J Cancer. 135:362–370.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Go SI, Kim RB, Song HN, Kang MH, Lee US,
Choi HJ, Lee SJ, Cho YJ, Jeong YY, Kim HC, et al: Prognostic
significance of the lymphocyte-to-monocyte ratio in patients with
small cell lung cancer. Med Oncol. 31:3232014. View Article : Google Scholar : PubMed/NCBI
|