Introduction
Hepatocellular carcinoma (HCC) originates in the
liver following long-term infection with the hepatitis B or C virus
(1), and recent research has linked
non-alcoholic steatohepatitis to HCC etiology (2). Current treatments include resection,
local ablation, transcatheter arterial chemoembolization, targeted
chemotherapy, and palliative care (3,4). In
addition, sorafenib, a kinase inhibitor, is increasingly used to
treat HCC (5), however there are
problems associated with its use, most notably, the ability of HCC
cells to develop resistance to it (6,7).
Cancer cells depend on glycolysis for energy
production and survival, and they exhibit significantly higher
rates of glycolysis than healthy tissues even when oxygen is
plentiful, a phenomenon known as the Warburg effect (8). As they require more glucose than healthy
tissue and metabolise this glucose primarily by glycolysis,
inhibiting glycolysis may be a more effective way of eradicating
cancer cells (9), and consequently be
developed as a treatment for cancer (10).
2-Deoxy-d-glucose (2DG) is an analogue of glucose
which cannot undergo glycolysis (11). Cancer cells take up 2DG in a similar
way to glucose, however, they cannot metabolize it to produce
energy. Therefore energy production is impaired, and cancer cells
are damaged (11).
The safety of 2DG in humans has been established
through its application in positron emission tomography (12). If the combination of sorafenib and 2DG
exert significantly stronger anti-tumor effects than either drug
alone, it may provide a novel therapeutic strategy to treat
HCC.
The present study sought to investigate the
suppressive effects of sorafenib and 2DG in combination on the
proliferation and motility of HCC cells compared with sorafenib
alone.
Materials and methods
Cells and cell culture
Human hepatocellula carcinoma cells, HLF cells and
PLC/PRF/5 cells were purchased from the RIKEN BioResource Centre
Cell Bank (Tsukuba, Japan), and cultured in Dulbecco's modified
Eagle's medium (DMEM; Sigma-Aldrich, St. Louis, MO, USA)
supplemented with 10% fetal bovine serum (FBS; Thermo Fisher
Scientific, Inc., Waltham, MA, USA). The cells were cultured in 10
cm dishes (Asahi Techno Glass, Yoshida-cho, Japan) with 5% carbon
dioxide at 37°C in a humidified chamber.
Cell proliferation assay
Cells were trypsinized, harvested, and split onto
96-well plates (Asahi Techno Glass) at a density of 1,000
cells/well. Varying concentrations of sorafenib (JS Research
Chemicals Trading, Wedel, Germany), 0, 1, 3, 10, and 30 µM, were
added to the media, and either 0 or 1 µM 2DG (Sigma-Aldrich) was
added. Following 72 h culture, the cells were subjected to an MTS
assay, (Promega Corporation, Madison, WI, USA) according to the
manufacturer instructions. During the assay, the cells reduce MTS
to a colored formazan product with an absorbance maximum at 490 nm.
The absorbance of the product was subsequently measured using an
iMark Microplate absorbance reader (Bio-Rad Laboratories Inc.,
Hercules, CA, USA).
Scratch assay
HLF and PLC/PRF/5 cells were plated on 4-well
chamber slides (BD Biosciences, Franklin Lakes, NJ, USA), and
scratched with a sterile razor when they reached confluence.
Immediately after scratch, the cells were incubated for 48 h with 1
µM sorafenib, 3 µM 2DG, or a combination of both. Following
incubation, they were stained with hematoxylin and eosin. The
slides were observed under an AX80 microscope (Olympus Corporation,
Tokyo, Japan, magnification ×100), and the distance between the
scratched line and the growing edges of the cells was measured at
five different points.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Cells were cultured in 6-well plates (Asahi Techno
Glass), and when they reached 70% confluence, were incubated with 1
µM sorafenib, 3 µM 2DG, or a combination of both. Following 48-h
culture, RNA was isolated with Isogen (Nippon Gene Co., Tokyo,
Japan) according to the manufacturer's instructions. The isolated
RNA was suspended in autoclaved Tris-EDTA buffer (pH 8.0). Total
RNA (5 µM) was subjected to cDNA synthesis with SuperScript III and
oligo(dT) following manufacturer instructions (Thermo Fisher
Scientific). RT-qPCR was performed using Fast SYBR Green Master Mix
(Thermo Fisher Scientific) with Mini Opticon (Bio-Rad). RT-qPCR was
performed for 40 cycles, with 5 sec of denaturation and 5 sec of
annealing-extension. Primer sequences are presented in Table I. RPL19, a housekeeping gene that is
constitutively expressed (13), was
used as an internal control. The expression levels of gene were
analyzed automatically by the Mini Opticon system (Bio-Rad) based
on delta-delta cycle threshold (ddCt) method. Relative expression
level of a gene was calculated as expression level of a gene
divided by expression level of RPL19.
 | Table I.Primers for real-time quantitative
PCR. |
Table I.
Primers for real-time quantitative
PCR.
| Name | Sequence | Description | Product size, bp | Annealing temp,
°C | Cycle | GenBank |
|---|
| OMC355 |
5′-AGAGGCGGAGGAGAACAAACAG-3′ | Cyclin D1 (F) | 180 | 60 | 40 | NM_053056 |
| OMC356 |
5′-AGGCGGTAGTAGGACAGGAAGTTG-3′ | Cyclin D1 (R) |
|
|
|
|
| OMC749 |
5′-CCTGGGCAGATTCCAAACCT-3′ | MMP9 (F) | 89 | 60 | 40 | NM_004994 |
| OMC750 |
5′-GCAAGTCTTCCGAGTAGTTTTGGAT-3 | MMP9 (R) |
|
|
|
|
| OMC321 |
5′-CGAATGCCAGAGAAGGTCAC-3′ | RPL19 (F) | 157 | 60 | 40 | BC095445 |
| OMC322 |
5′-CCATGAGAATCCGCTTGTTT-3′ | RPL19 (R) |
|
|
|
|
Statistical analysis
One-way analysis of variance (ANOVA) was used for
statistical analysis with JMP software ver. 10.0.2 (SAS Institute,
Cary, NC, USA). P<0.05 was considered to indicate a
statistically significant difference.
Results
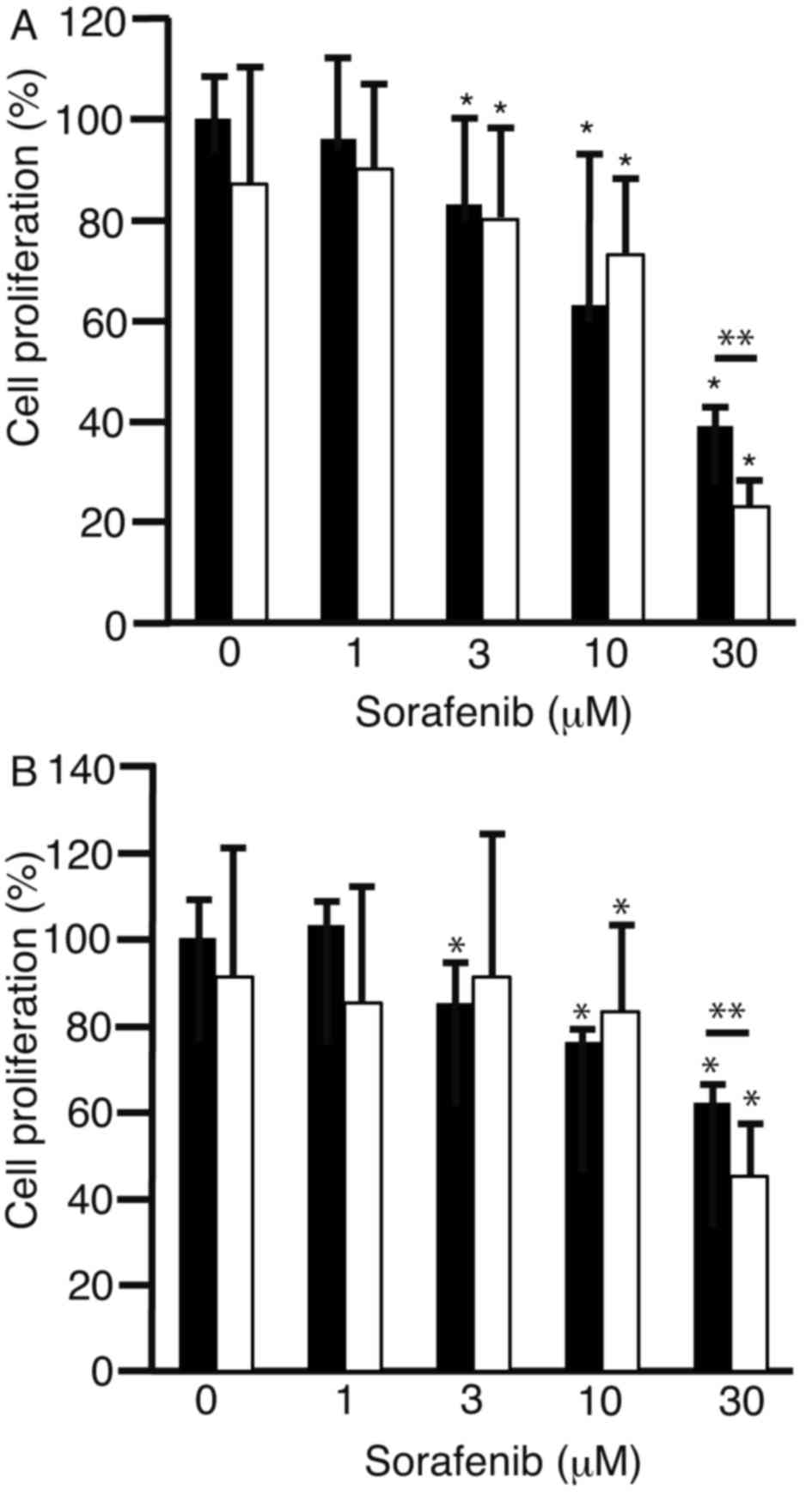
To investigate whether 2DG enhanced the
anti-proliferative effects of sorafenib, HLF cells (Fig. 1A) and PLC/PRF/5 cells (Fig. 1B) were cultured with 0, 1, 3, 10, and
30 µM sorafenib either alone (black bars) or with 2DG (white bars).
The combination of 1 µM 2DG and 30 µM sorafenib markedly suppressed
cell proliferation of both cell types compared to sorafenib alone
(P<0.05). This suggests that 2DG is able able to enhance the
anti-proliferative effects of sorafenib in HLF and PLC/PRF/5
cells.
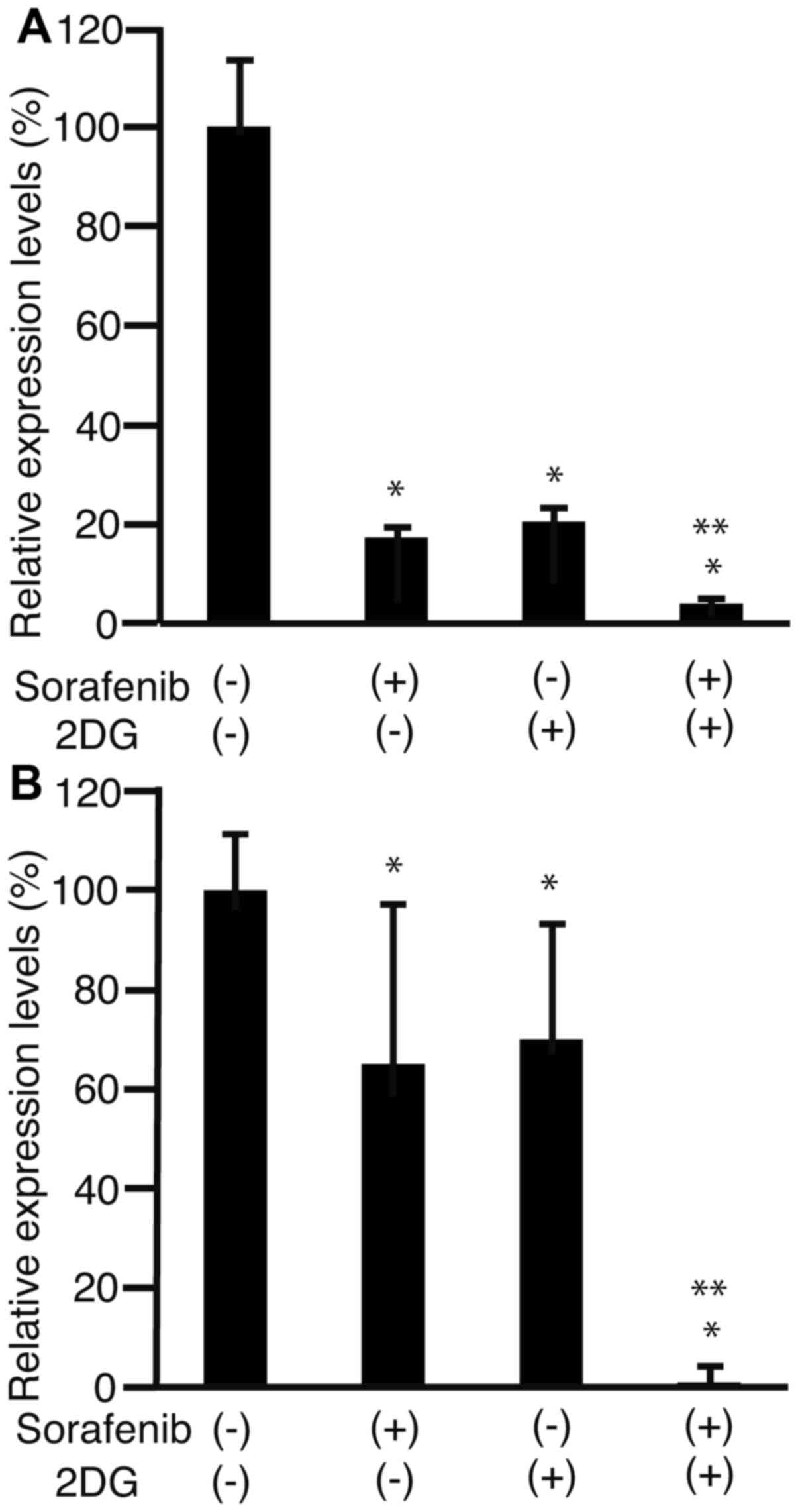
To clarify the effect of sorafenib and 2DG on the
cell cycle, levels of cyclin D1 expression were analyzed by RT-qPCR
in HLF cells (Fig. 2A) and PLC/PRF/5
cells (Fig. 2B). The expression of
cyclin D1 in both cell types decreased more in cells exposed to
sorafenib and 2DG compared with cells exposed to 2DG or sorafenib
alone (P<0.05; Fig. 2). This
demonstrates that sorafenib and 2DG together decrease cyclin D1
expression more effectively than either drug alone.
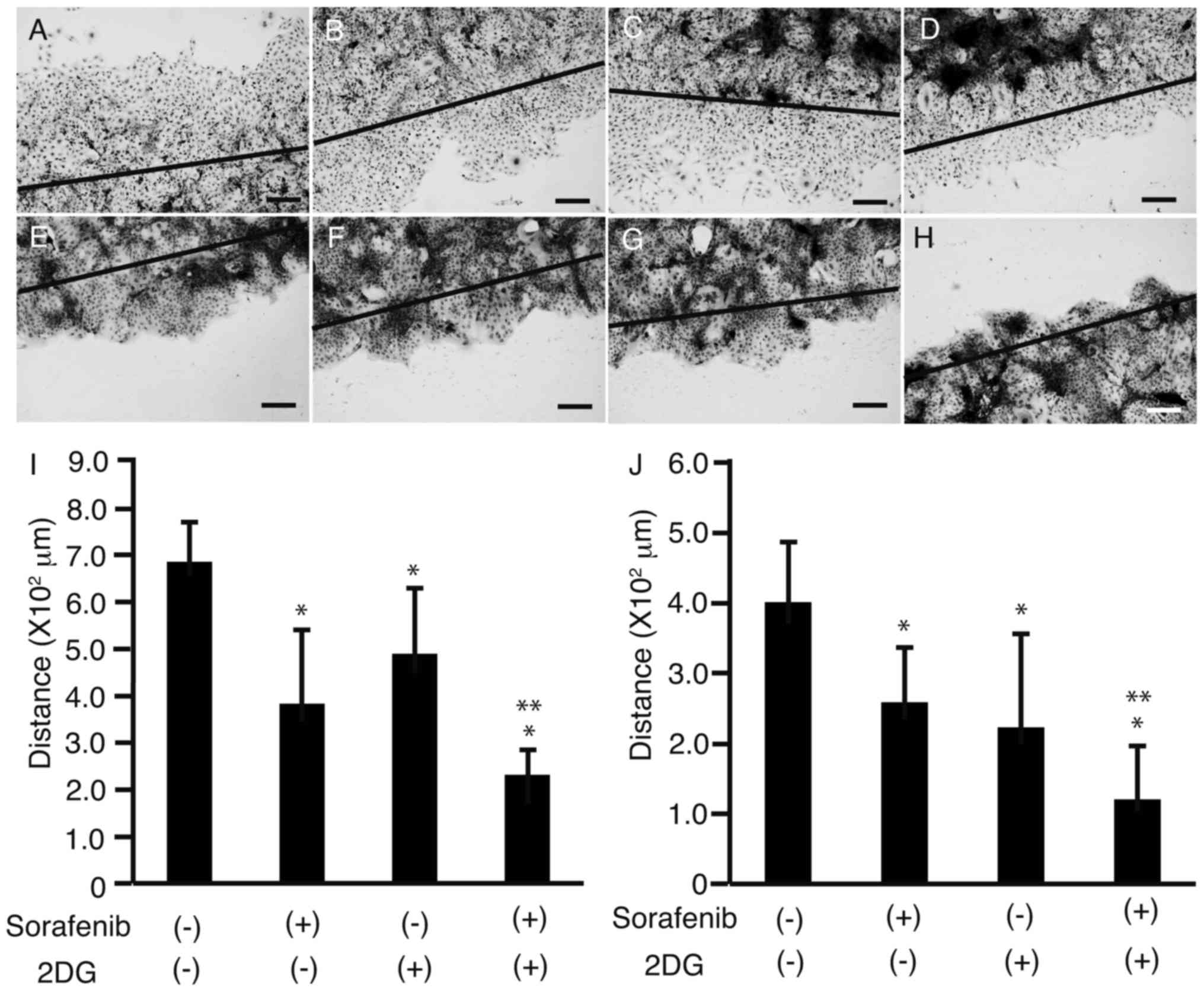
To investigate the effects of sorafenib and 2DG on
cell motility, a scratch assay was performed on HLF cells (Fig. 3A-D) and PLC/PRF/5 cells (Fig. 3E-H). All cells were cultured in 4-well
chamber slides, and following scratching with a sterile razor, 3 µM
sorafenib (Fig. 3B and F), 1 µM 2DG
(Fig. 3C and G), or a combination of
both (Fig. 3D and H) were added.
Cells were then stained, and the distance between the growing edge
of the cell sheet and the scratched line was measured in HLF cells
(Fig. 3I) and PLC/PRF/5 cells
(Fig. 3J). The distance was shorter
in cells cultured with both sorafenib and 2DG than in cells
cultured with 2DG or sorafenib alone (P<0.05; Fig. 3I and J), suggesting that 2DG enhances
the suppressive effects of sorafenib on cell motility.
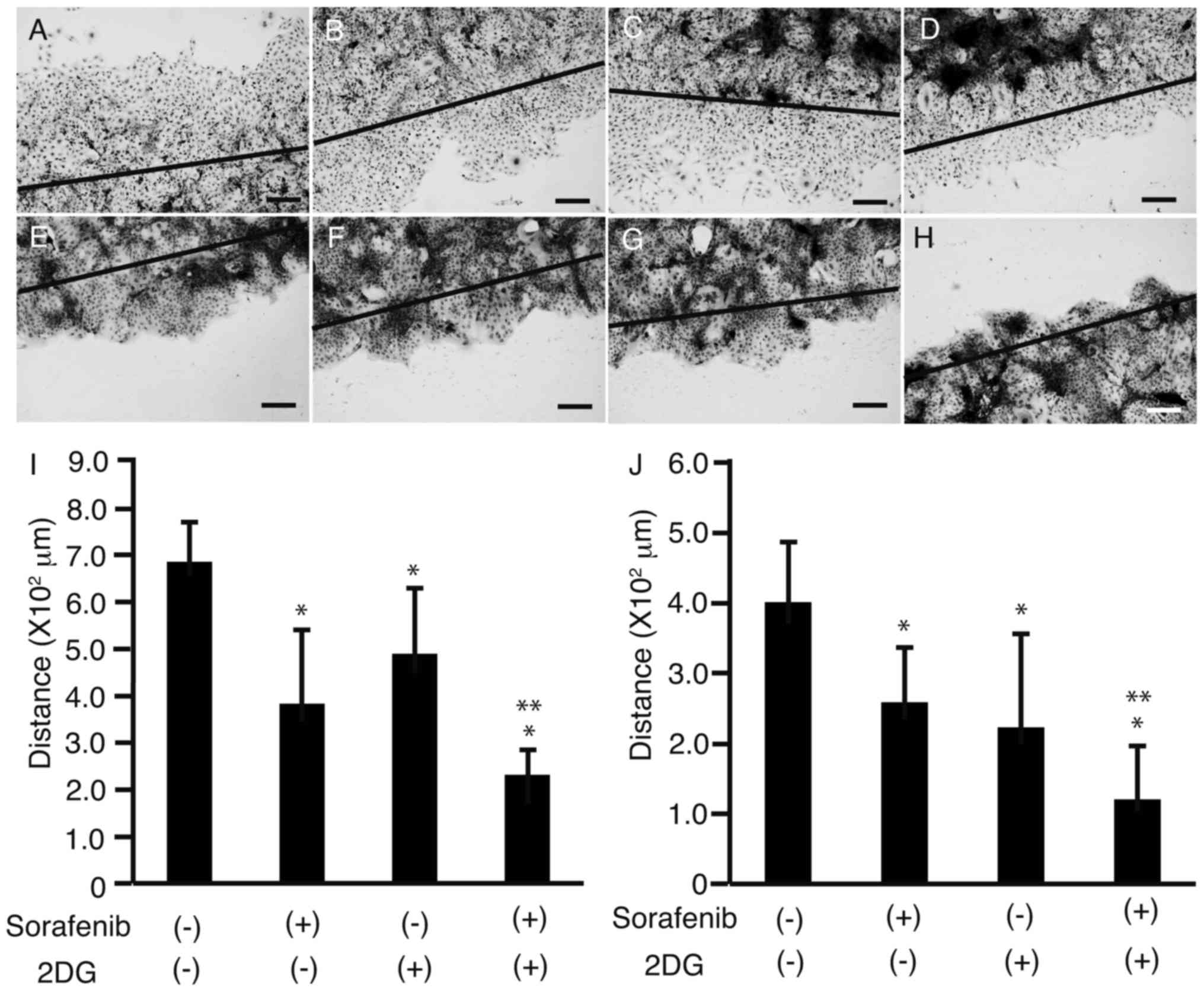 | Figure 3.Scratch assay. HLF cells (A-D) and
PLC/PRF/5 cells (E-H) in 4-well chamber slides were scratched with
a sterile razor. Immediately after the scratch (solid line), no
sorafenib or 2DG (A, E), 3 µM sorafenib (B, F), 1 µM 2DG (C, G), or
both (D, H) were added to the cells. Following 48 h in culture, the
cells were stained with hematoxylin and eosin. Distance between the
growing edge of the cell sheet and the scratched line was measured
at five different points in HLF cells (I) and PLC/PRF/5 cells (J).
Original magnification: ×100, scale bar: 200 µM, *P<0.05 against
sorafenib (−) and 2DG (−), **P<0.05 against sorafenib (−) and
2DG (−), sorafenib (−) and 2DG (+), and sorafenib (+) and 2DG (−),
n=5. HLF, Human liver fibroblast cells; 2DG, 2-deoxyglucose;
PLC/PRF/5 cells, human hepatoma carcinoma cell line. |
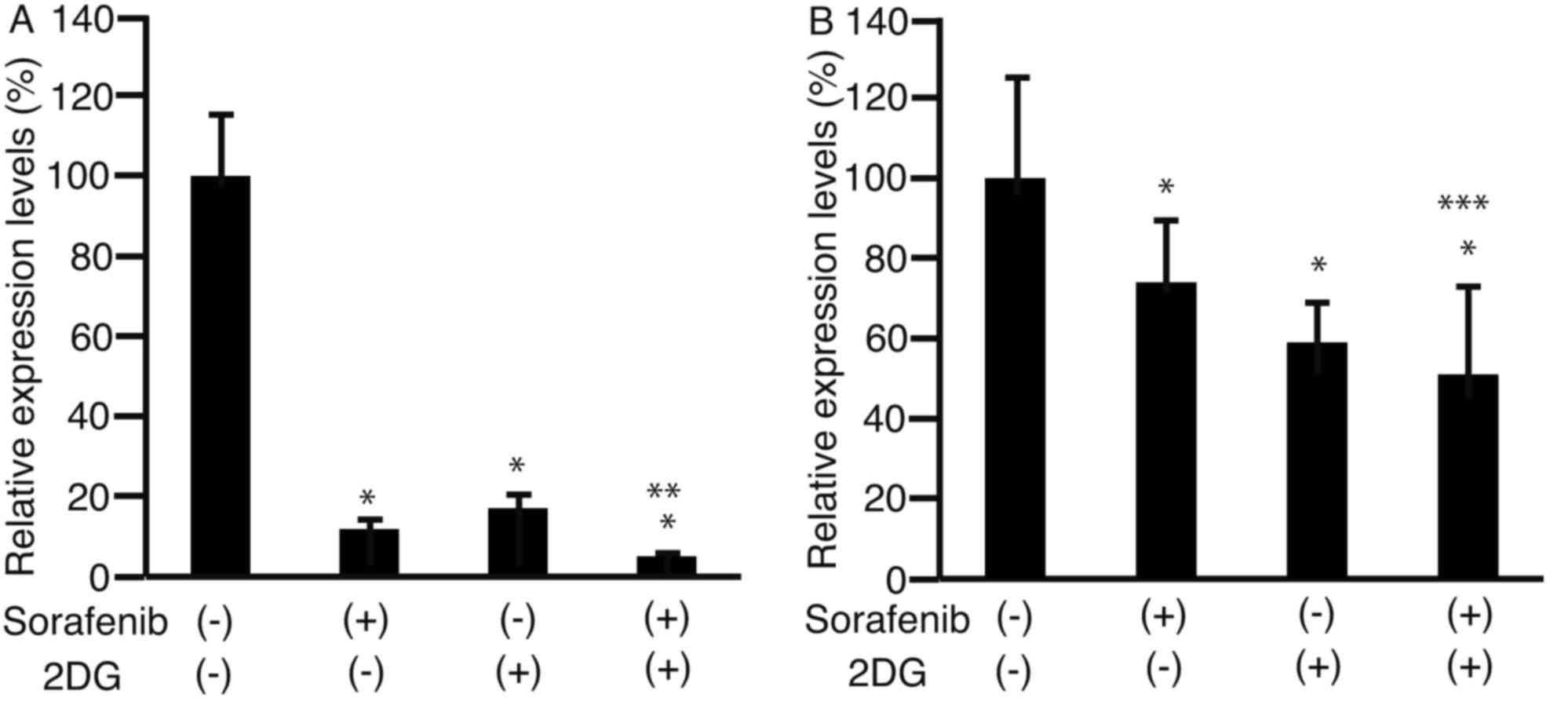
Matrix metalloproteinase 9 (MMP9) is involved in
cell motility and is overexpressed in HCC (14,15). MMP9
expression was analyzed using RT-qPCR in HLF cells (Fig. 4A) and PLC/PRF/5 cells (Fig. 4B), and was significantly lower in
cells cultured with a combination of sorafenib and 2DG than in
cells cultured with either drug alone (P<0.05).
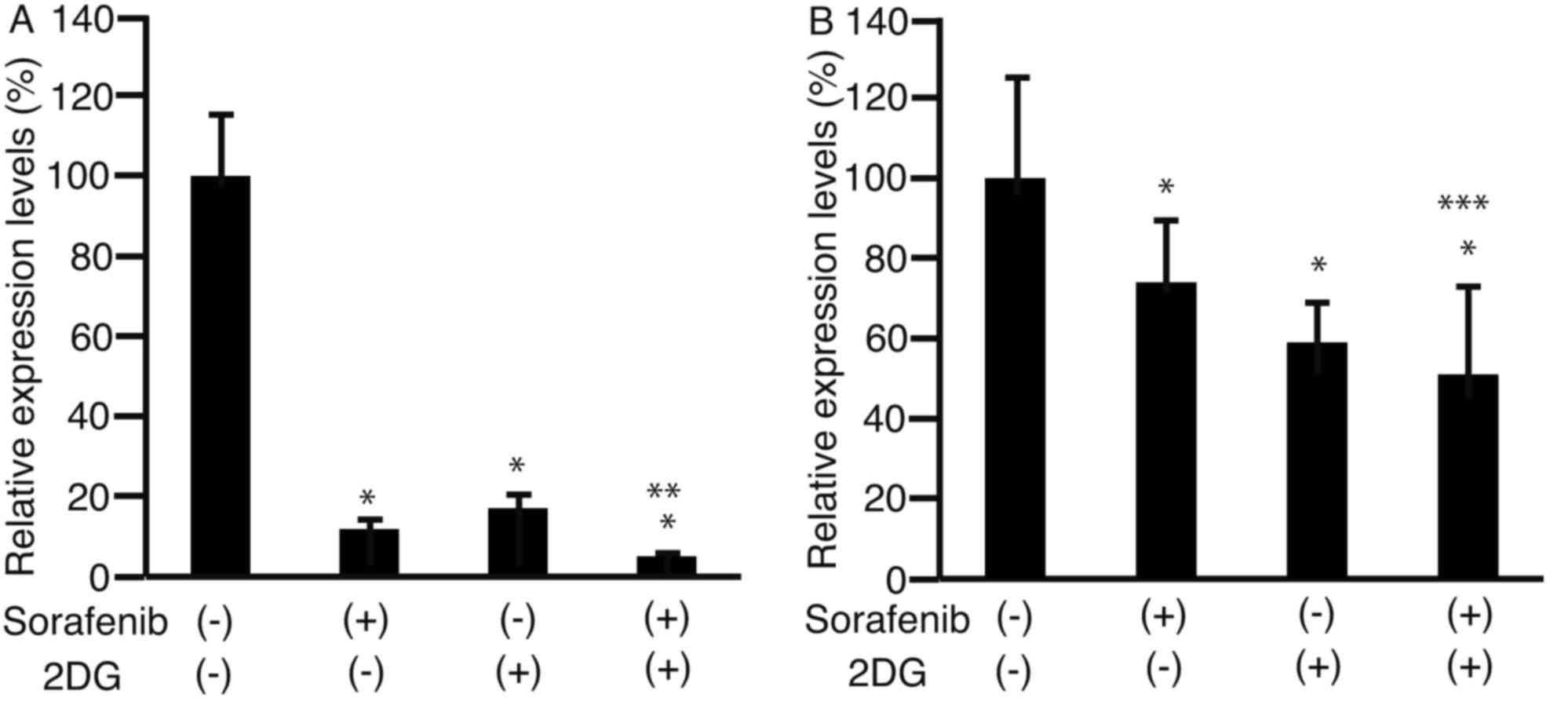 | Figure 4.Expression levels of matrix
metalloproteinase. HLF cells (A) and PLC/PRF/5 cells (B) were
cultured in 6-well plates, and added to 3 µM sorafenib (+), 1 µM
2DG (+), or a combination of both. Following 48 h in culture, RNA
was isolated and subjected to RT-qPCR. Levels of matrix
metalloproteinase expression were analyzed. *P<0.05 against
sorafenib (−) and 2DG (−), **P<0.05 against sorafenib (−) and
2DG (−), sorafenib (−) and 2DG (+), and sorafenib (+) and 2DG (−),
***P<0.05 against sorafenib (−) and 2DG (−), and sorafenib (−)
and 2DG (+), n=3. HLF, Human liver fibroblast cells; 2DG,
2-deoxyglucose; PLC/PRF/5 cells, human hepatoma carcinoma cell
line; RT-qPCR, reverse transcription-quantitative polymerase chain
reaction. |
Discussion
Previous studies have demonstrated that
2-[(3-Carboxy- 1-oxoprogy1) amino]-2-deoxy-D-glucose, another
analogue of glucose similar to 2DG, suppresses the proliferation of
cells from the human HCC HepG2 cell line (16). In the present study, 3 µM 2DG and 30
µM sorafenib significantly suppressed the proliferation of HLF and
HCC PLC/PRF/5 cells. The difference in suppression of proliferation
was significant at sorafenib concentrations >10 µM.
Sorafenib and 2DG independently decrease cyclin D1
expression (Fig. 2), therefore it was
expected that the combination of sorafenib and 2DG would
synergistically suppress HCC proliferation at lower concentrations
of sorafenib. This was observed in both HLF and PLC/PRF/5 cells.
However, the reasons underlying the suppressive effects of 2DG and
sorafenib combination on HCC cell proliferation remain unclear.
Metastasis is a result of HCC cell invasion from the
primary site to local or distant tissue (17). The combination of 2DG and sorafenib
suppressed cell motility more effectively than 2DG or sorafenib
alone (Fig. 3). Additionally,
expression of MMP9 significantly decreased when cells were treated
with a combination of 2DG and sorafenib compared with 2DG or
sorafenib alone (Fig. 4), suggesting
that treatment with both 2DG and sorafenib may effectively inhibit
metastasis.
2DG enhances the anti-tumor effects of other
chemotherapeutic agents (18). In
vivo studies have demonstrated that sections of tumors are
hypoxic (19), and cancer cells are
resistant to 2DG in these hypoxic regions (20). The combination of 2DG and sorafenib
offers a promising strategy to overcome this resistance.
The feasibility of this approach is contingent on
2DG and sorafenib being safe for oral administration. A combination
of 2DG and docetaxel as treatment for solid cancers has been
investigated, and no serious adverse effects were reported
(21). Furthermore, a phase I/II
clinical trial investigating the combination of radiotherapy and
2DG against glioma reported no serious adverse events (22). These reports and the results of the
current study suggest that the combination of 2DG and sorafenib is
safe for oral administration, though further studies are required
to confirm this.
The main limitation of the present study was the
lack of in vivo data from xenograft animal models, therefore
future studies are required that investigate the effects of
systemic 2DG and sorafenib administration in vivo.
In conclusion, the current study demonstrated that
2DG and sorafenib suppressed the proliferation of HCC cells more
effectively than sorafenib alone, and suppressed cell motility more
effectively than 2DG or sorafenib alone. Therefore, combined
treatment of 2DG and sorafenib may be an effective therapeutic
strategy to treat cancer, including HCC.
References
|
1
|
Cameron AM: Screening for viral hepatitis
and hepatocellular cancer. Surg Clin North Am. 95:1013–1021. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Khan FZ, Perumpail RB, Wong RJ and Ahmed
A: Advances in hepatocellular carcinoma: Nonalcoholic
steatohepatitis-related hepatocellular carcinoma. World J Hepatol.
7:2155–2161. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wells SA, Hinshaw JL, Lubner MG,
Ziemlewicz TJ, Brace CL and Lee FT Jr: Liver ablation: Best
practice. Radiol Clin North Am. 53:933–971. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Katano T, Mizoshita T, Senoo K, Sobue S,
Takada H, Sakamoto T, Mochiduki H, Ozeki T, Kato A, Matsunami K, et
al: The efficacy of transcatheter arterial embolization as the
first-choice treatment after failure of endoscopic hemostasis and
endoscopic treatment resistance factors. Dig Endosc. 24:364–369.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Furuse J, Ishii H, Nakachi K, Suzuki E,
Shimizu S and Nakajima K: Phase I study of sorafenib in Japanese
patients with hepatocellular carcinoma. Cancer Sci. 99:159–165.
2008.PubMed/NCBI
|
|
6
|
Kuczynski EA, Lee CR, Man S, Chen E and
Kerbel RS: Effects of sorafenib dose on acquired reversible
resistance and toxicity in hepatocellular carcinoma. Cancer Res.
75:2510–2519. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen J, Jin R, Zhao J, Liu J, Ying H, Yan
H, Zhou S, Liang Y, Huang D, Liang X, et al: Potential molecular,
cellular and microenvironmental mechanism of sorafenib resistance
in hepatocellular carcinoma. Cancer Lett. 367:1–11. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Vaitheesvaran B, Xu J, Yee J, Qy L, Go VL,
Xiao GG and Lee WN: The Warburg effect: A balance of flux analysis.
Metabolomics. 11:787–796. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jang M, Kim SS and Lee J: Cancer cell
metabolism: Implications for therapeutic targets. Exp Mol Med.
45:e452013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Granja S, Pinheiro C, Reis RM, Martinho O
and Baltazar F: Glucose addiction in cancer therapy: Advances and
drawbacks. Curr Drug Metab. 16:221–242. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang D, Li J, Wang F, Hu J, Wang S and
Sun Y: 2-Deoxy- D-glucose targeting of glucose metabolism in cancer
cells as a potential therapy. Cancer Lett. 355:176–183. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Brito AF, Mendes M, Abrantes AM, Tralhão
JG and Botelho MF: Positron emission tomography diagnostic imaging
in multidrug-resistant hepatocellular carcinoma: Focus on
2-deoxy-2-(18F)Fluoro-D-Glucose. Mol Diagn Ther. 18:495–504. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Davies B and Fried M: The L19 ribosomal
protein gene (RPL19): Gene organization, chromosomal mapping, and
novel promoter region. Genomics. 25:372–380. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Vandooren J, Van den Steen PE and
Opdenakker G: Biochemistry and molecular biology of gelatinase B or
matrix metalloproteinase-9 (MMP-9): The next decade. Crit Rev
Biochem Mol Biol. 48:222–272. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang Y, Shen Y, Cao B, Yan A and Ji H:
Elevated expression levels of androgen receptors and matrix
metalloproteinase-2 and −9 in 30 cases of hepatocellular carcinoma
compared with adjacent tissues as predictors of cancer invasion and
staging. Exp Ther Med. 9:905–908. 2015.PubMed/NCBI
|
|
16
|
Wu J, Kou W, Gao MT, Zhou YN, Wang AQ, Xue
QJ and Qiao L: Effects of
{2-[(3-carboxy-1-oxoprogy1)amino]-2-deoxy-D-glucose} on human
hepatocellular carcinoma cell line. Acta Pharmacol Sin. 26:635–640.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tomizawa M, Kondo F and Kondo Y: Growth
patterns and interstitial invasion of small hepatocellular
carcinoma. Pathol Int. 45:352–358. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Takemura A, Che XF, Tabuchi T, Moriya S,
Miyazawa K and Tomoda A: Enhancement of cytotoxic and pro-apoptotic
effects of 2-aminophenoxazine-3-one on the rat hepatocellular
carcinoma cell line dRLh-84, the human hepatocellular carcinoma
cell line HepG2, and the rat normal hepatocellular cell line RLN-10
in combination with 2-deoxy-D-glucose. Oncol Rep. 27:347–355.
2012.PubMed/NCBI
|
|
19
|
Lv Y, Zhao S, Han J, Zheng L, Yang Z and
Zhao L: Hypoxia-inducible factor-1α induces multidrug resistance
protein in colon cancer. Onco Targets Ther. 8:1941–1948. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Maher JC, Wangpaichitr M, Savaraj N,
Kurtoglu M and Lampidis TJ: Hypoxia-inducible factor-1 confers
resistance to the glycolytic inhibitor 2-deoxy-D-glucose. Mol
Cancer Ther. 6:732–741. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Raez LE, Papadopoulos K, Ricart AD,
Chiorean EG, Dipaola RS, Stein MN, Lima CM Rocha, Schlesselman JJ,
Tolba K, Langmuir VK, et al: A phase I dose-escalation trial of
2-deoxy-D-glucose alone or combined with docetaxel in patients with
advanced solid tumors. Cancer Chemother Pharmacol. 71:523–530.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Singh D, Banerji AK, Dwarakanath BS,
Tripathi RP, Gupta JP, Mathew TL, Ravindranath T and Jain V:
Optimizing cancer radiotherapy with 2-deoxy-d-glucose dose
escalation studies in patients with glioblastoma multiforme.
Strahlenther Onkol. 181:507–514. 2005. View Article : Google Scholar : PubMed/NCBI
|