Introduction
Colorectal cancer is a major cause of morbidity and
mortality worldwide (1). It is the
third most common malignancy and second most common cause of
cancer-related death in developed countries (2). Intensive surveillance after colorectal
cancer surgery improves survival because early diagnosis of
recurrence increases the frequency of its curative resection
(3). Therefore, identification of the
risk factors for distant metastasis would optimize the treatment of
colorectal cancer.
Tumor angiogenesis (the formation of new blood
vessels) is essential for tumor growth and metastasis (2,4). The
development of new blood vessels is a complex phenomenon involving
growth factors, extracellular matrix enzymes, endothelial cell
migration and proliferation, lumen formation, and anastomosis with
other vessels (5,6). New blood vessel formation facilitates
entry of malignant cells into the circulation, thus increasing the
probability of metastasis (6,7). Assessment of microvessel density (MVD),
a means of quantifying neovascular vessels, involves staining
tissues with pan-endothelial antibodies to antigens such as CD34,
CD31, and von Willebrand factor (6,8). However,
these pan-endothelial markers are also expressed in normal tissues
(9). Currently, CD105 is the
immunohistochemical marker most frequently used to identify
activated endothelial cells (10).
CD105 is reportedly strongly expressed in endothelial cells of
tissues participating in angiogenesis.
We believe that reevaluating the association between
tumor angiogenesis as assessed by monoclonal antibodies to CD105
and distant metastasis is essential for optimal treatment of
colorectal cancer. The purpose of our study was to identify
associations between the presence or absence of distant metastasis
and potential clinicopathological risk factors for tumor
angiogenesis.
Materials and methods
Patients and clinical data
We retrospectively studied 129 T1, T2, T3, and T4
colorectal cancers specimens resected at the Showa University
Northern Yokohama Hospital from January 2009 to September 2009.
Written informed consent was obtained from all patients before
endoscopic therapy or laparoscopic/open surgery. This study was
approved by the Ethics Committee of Showa University Hospital.
The inclusion criteria were as follows: i)
Colorectal cancers that had been surgically resected or
endoscopically resected prior to surgery; and ii) cases without
distant metastasis during follow-up of at least 5 years after
surgery. The exclusion criteria were as follows: Patients who had
i) two or more cancers excluding colorectal mucosal cancer; or ii)
received chemotherapy and/or radiotherapy prior to surgery (because
these factors affect the causal relationship with distant
metastasis.).
Relevant clinicopathological data (age, gender,
tumor size, location and depth, lymphatic infiltration, vascular
infiltration, regional lymph node metastasis, poorly differentiated
or mucinous carcinoma components, adjuvant chemotherapy, and
distant metastases) were extracted from an electronic record system
and reviewed. This study included 72 men (55.8%) and 57 women
(44.2%) aged 31 to 87 years (median, 66 years). Distant metastasis
was defined as metastasis to another organ (such as the liver,
lung, bone, brain, or peritoneum) and/or nonregional lymph node
metastasis.
CD105 immunostaining
Immunohistochemical staining was performed on 4- to
5-µm-thick formalin-fixed and paraffin-embedded sections obtained
from each specimen. Sections containing the most invasive areas of
colorectal cancer were selected. Staining was performed
automatically (BONDIII; Leica Biosystems Melbourne, Melbourne,
Victoria, Australia), using a Bond Polymer Refine Detection kit
(Leica Biosystems, Newcastle, UK), with mouse monoclonal antibodies
to CD105 (clone SN6h; Dako, Kyoto, Japan; working dilution 1:500
for 15 min with bond wash solution buffer) (11).
Stainability of monoclonal antibodies
to CD105 and pan-endothelial antibodies
To assess whether monoclonal antibodies to CD105 are
specific for new tumor blood vessels, we performed a pilot study
comparing microvessels between normal and cancerous areas by
staining with monoclonal antibodies to CD105, CD31, CD34, and von
Willebrand factor. The tissues were examined under high
magnification (x400).
Pathological analysis
Tumor size was measured after formalin fixation. The
specimens were assessed according to World Health Organization
criteria (12) and the Japanese
Society for Cancer of the Colon and Rectum guidelines (13). The histological grade and presence of
regional lymph node metastasis were investigated by examining
hematoxylin and eosin (H&E)-stained specimens. Lymphatic
infiltration was evaluated by examining H&E-stained sections
and/or sections immunostained with anti-D2-40 antibody (Dako North
America, Carpinteria, CA, USA). Vascular infiltration was evaluated
using double staining with H&E and/or Victoria blue (Muto Pure
Chemicals, Tokyo, Japan). The histological grade was assigned
according to the least differentiated tumor component. Poorly
differentiated or mucinous carcinoma components were classified as
present if any part of the lesion contained either of these
features (14).
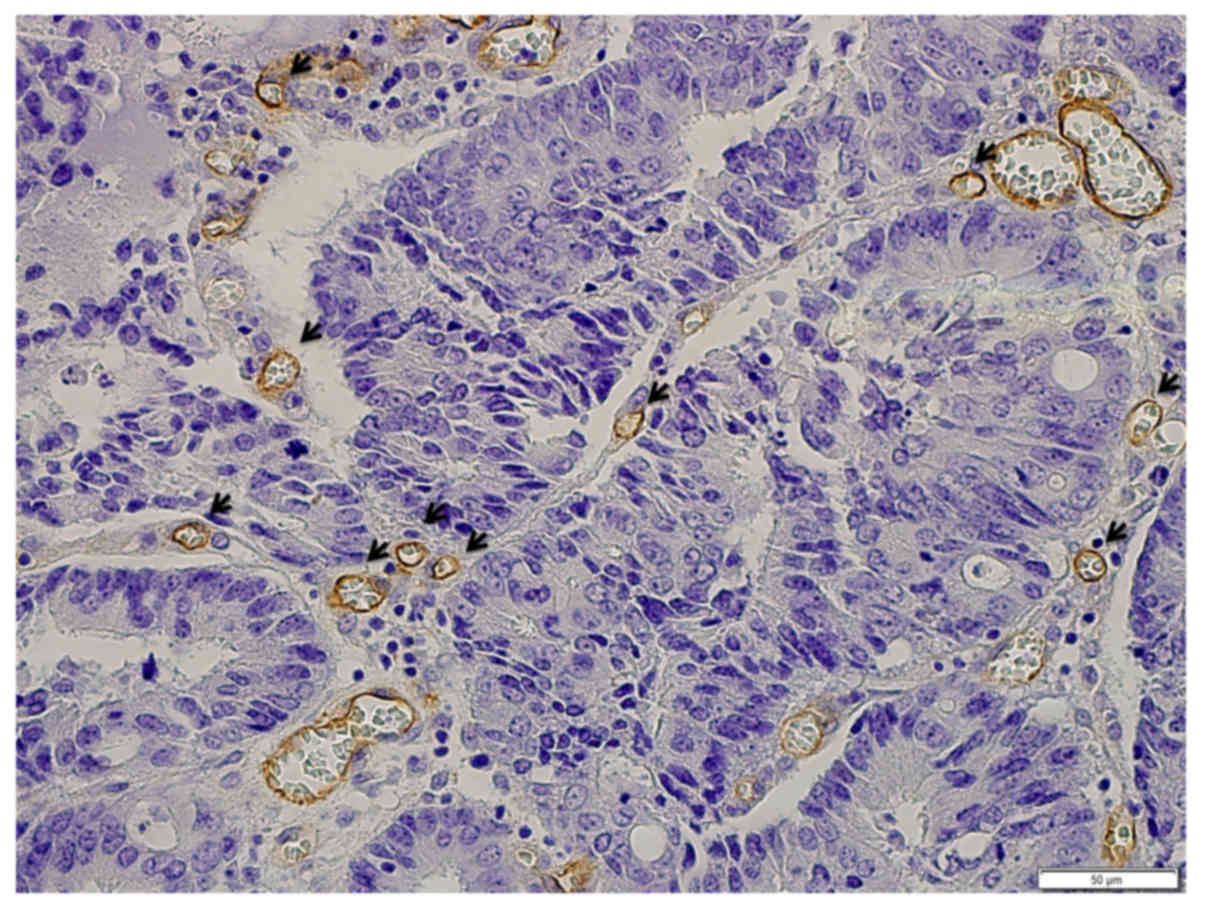
Assessment of MVD
As previously reported, vessels stained with
monoclonal antibodies to CD105 show three basic morphological
features: Round-shape, sinusoid-like, and small vessels without
discernible lumens (endothelial sprouts) (6). Only vessels with discernible lumens of a
caliber smaller than approximately eight blood cells and without
thick muscular walls were counted (15) (Fig. 1).
The procedure used conforms with the international consensus method
for assessing intratumoral MVD (16).
After scanning the immunostained section at low magnifications (x40
and ×100), the three areas with the greatest number of distinctly
highlighted microvessels (so-called hot spots) were selected.
Microvessels at ×400 magnification were enumerated without
knowledge of the patient's status. MVD is expressed as the mean
number of vessels per high-power field (x400) in the three selected
hot spots (6).
Outcome measures and statistical
analysis
Univariate analysis was first performed to identify
associations between distant metastases and potential risk factors
(17). The clinicopathological
factors listed above were then analyzed using Fisher's exact test
and Welch's t-test. A P-value of <0.05 was considered to
indicate a statistically significant difference (14).
Stepwise multivariate logistic regression was then
performed to determine which combination of variables provided the
best estimate of the relative risk of distant metastasis. Odds
ratios and 95% confidence intervals (CIs) were calculated after
accounting for potential confounders. All data are presented as the
mean ± standard deviation. Furthermore, receiver operating
characteristic (ROC) analysis was performed to determine the
optimal cut-off value for MVD. All analyses were performed using
JMP®12 (SAS Institute, Cary, NC, USA).
Results
Total lesions
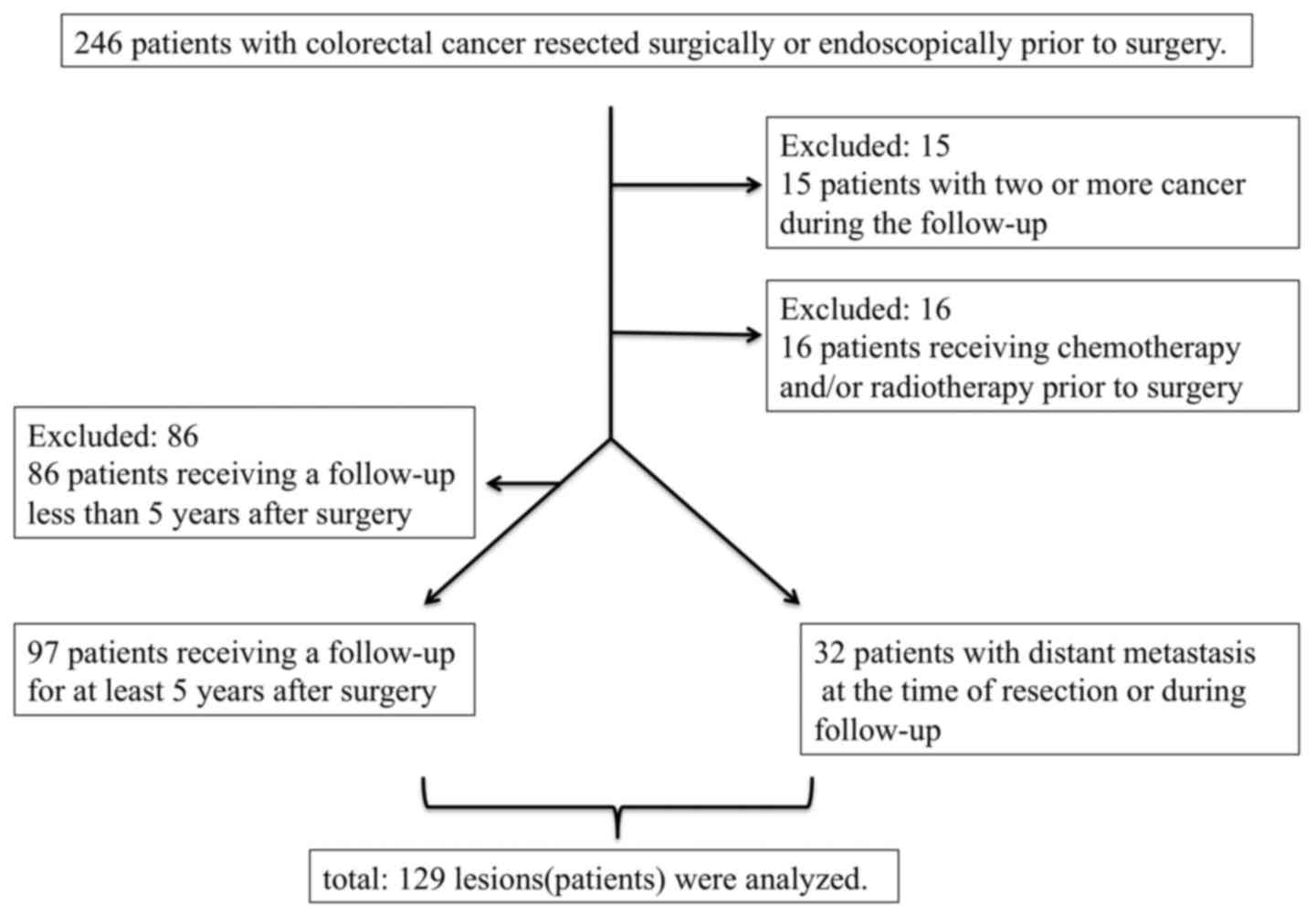
In this study, 129 lesions were analyzed. A flow
chart showing application of the inclusion and exclusion criteria
is shown in Fig. 2. The median
follow-up time was 34 months (range, 6–85 months) in patients with
distant metastasis and 61 months (range, 60–86 months) in patients
without distant metastasis.
Distant metastases
At the time of resection or during follow-up, 32
patients had distant metastases (liver, n=13; lung, n=5;
peritoneum, n=4; liver and peritoneum, n=3; lung and peritoneum,
n=3; liver, lung and peritoneum, n=1; liver and bone, n=1; liver,
lung, distant lymph node, and bone, n=1; and lung, kidney, and
spleen, n=1). Thirteen patients had distant metastasis from the
beginning of the study, and 19 patients had distant metastasis
during follow-up.
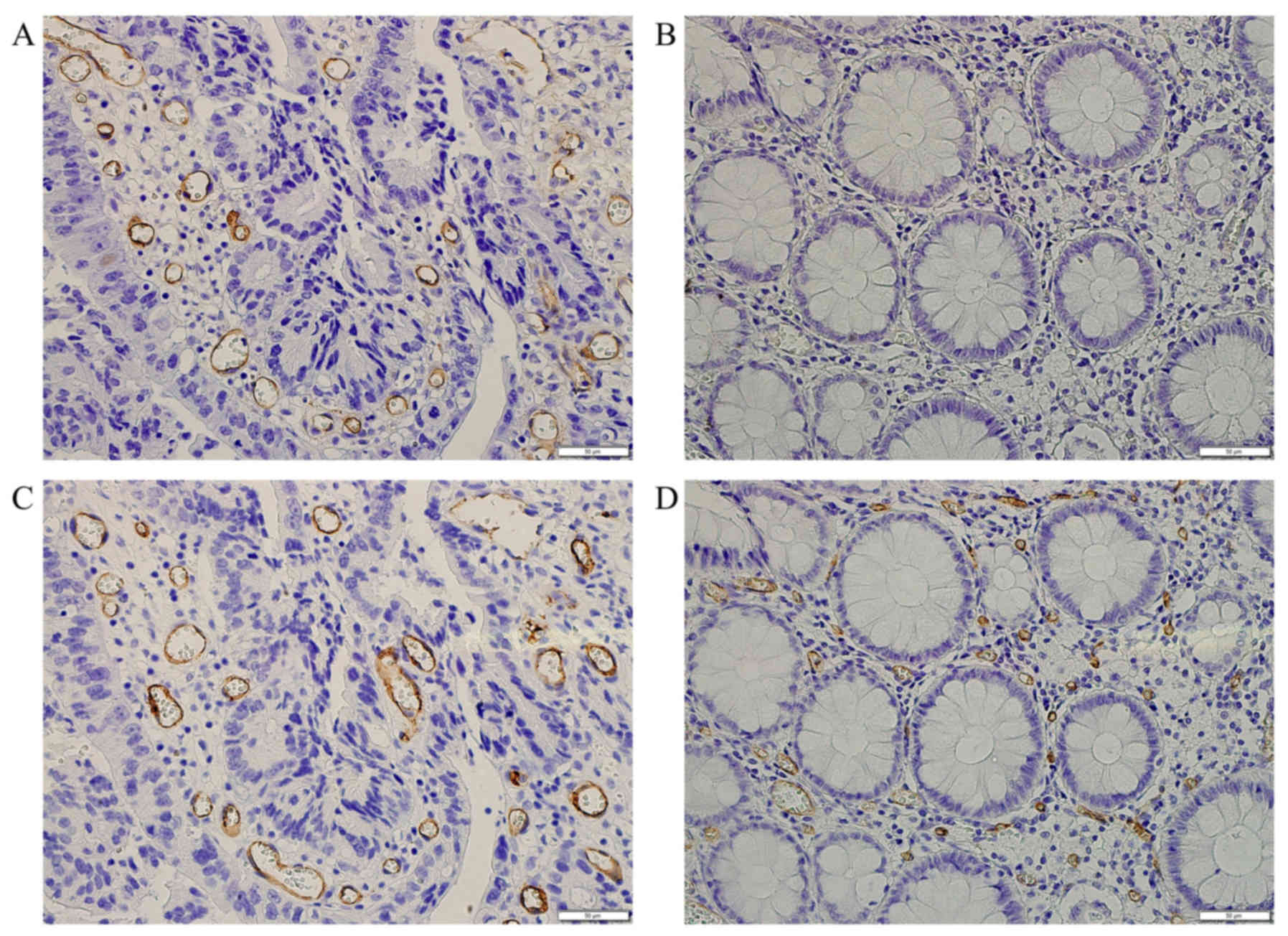
Comparison of staining with monoclonal
antibodies to CD105 and pan-endothelial antibodies for assessing
microvessels
In normal areas, these vessels stained strongly with
CD31, CD34, and von Willebrand factor antibodies, whereas they
stained weakly or not at all with monoclonal antibodies to CD105.
Fig. 3 shows typical examples of
microvessel evaluation between normal and cancerous areas stained
with monoclonal antibodies to CD105 and CD34.
Vessels stained with monoclonal
antibodies to CD105
Fig. 1 shows staining
of microvessels with monoclonal antibodies to CD105, as indicated
by the brown circle lines around angiogenetic vessels. Only vessels
with discernible lumens, of smaller caliber than approximately
eight red blood cells, and without thick muscular walls were
counted.
MVD and distant metastasis
Table I shows the
associations of selected clinicopathological factors with distant
metastasis. The MVD was 10.4±4.9 (mean ± standard deviation) in
patients with distant metastases from colorectal cancer and 7.6±3.3
in those without distant metastases; this difference was
significant according to the univariate analysis (P=0.008, Welch's
t-test).
 | Table I.Relationships between selected
clinicopathological factors and distant metastasis. |
Table I.
Relationships between selected
clinicopathological factors and distant metastasis.
|
|
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|
|
|---|
| Clinicopathological
factors | No. of cases with
metastasis (n=32) | No. of cases
without metastasis (n=97) | OR (95% CI) | P-value | OR (95% CI) | P-value |
|---|
| Aged (≥70 years old/<70) | 14/18 | 38/59 | 1.21
(0.54–2.54) | 0.68a |
|
|
| Genderd (male/female) | 18/14 | 54/43 | 1.02
(0.46–2.46) | 1.00a |
|
|
| Tumor sized (mean ± SD) | 54.1±28.3 | 34.6±18.3 | N/A |
<0.001b | 1.03
(1.01–1.01) | 0.007c |
| Tumor
locationd (rectum/colon) | 12/20 | 24/73 | 1.83
(0.78–4.78) | 0.18a |
|
|
| Tumor depthd (T2-T4/T1) | 31/1 | 66/31 | 14.56
(1.90–111.90) |
<0.001a |
|
|
| Lymphatic
infiltrationd (+/−) | 25/7 | 54/43 | 2.84
(1.12–7.12) | 0.035a |
|
|
| Vascular
infiltrationd (+/−) | 28/4 | 59/38 | 4.51
(1.46–13.46) | 0.0048a |
|
|
| Regional lymph node
metastasisd (+/−) | 21/11 | 21/76 | 6.91
(2.88–16.88) |
<0.001a | 4.76
(1.87–12.87) | 0.001c |
| Por/Muc
componentd (+/−) | 9/23 | 22/75 | 1.33
(0.54–3.54) | 0.63a |
|
|
| Adjuvant chemo
therapyd (+/−) | 15/17 | 23/74 | 2.84
(1.23–6.23) | 0.024a |
|
|
| MVDd (mean ± SD) | 10.4±4.9 | 7.6±3.3 | N/A | 0.0081b | 1.14
(1.02–1.02) | 0.033c |
Associations between
clinicopathological factors other than MVD and distant
metastasis
According to the univariate analysis, there were
also statistically significant differences in tumor size, tumor
depth (T2-4 tumors), lymphatic infiltration, vascular infiltration,
regional lymph node metastasis, and having received adjuvant
chemotherapy between patients with and without metastases from
colorectal cancer (Welch's t-test and Fisher's exact test)
(Table I).
Stepwise multivariate logistic
regression
According to stepwise multivariate logistic
regression, MVD, regional lymph node metastasis, and tumor size
were independent risk factors for distant metastases (Table I).
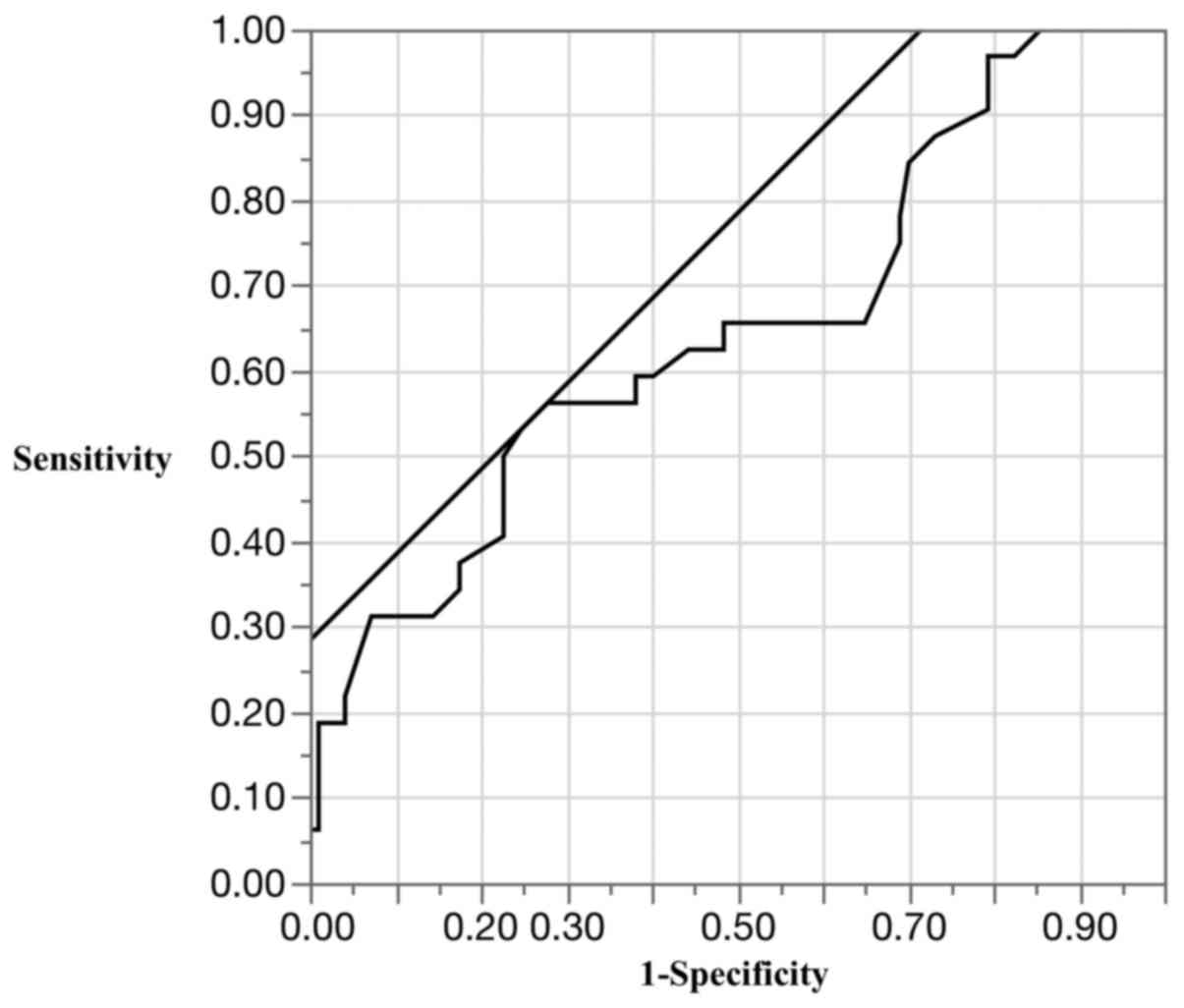
Optimal cut-off value for MVD for
estimation of risk of distant metastasis
To facilitate clinical application of our findings,
we determined the optimal cut-off value for MVD by ROC analysis
(area under the curve, 0.65; cut-off value, 10 vessels/x400 field;
sensitivity, 56.3%; specificity, 72.2%; and accuracy, 68.2%)
(Fig. 4). Patients with cancers that
had ≥10 vessels/x400 field of MVD were at significantly higher risk
of distant metastasis than those with cancers that had <10
vessels/x400 field of MVD (P=0.005, Fisher's exact test).
Discussion
In this study, we found that MVD, regional lymph
node metastasis, and tumor size were significantly associated with
distant metastases from colorectal cancer and that MVD is a more
appropriate risk factor for distant metastasis than is lymphatic or
vascular infiltration.
Because tumor growth and metastasis are dependent on
angiogenesis (2,4), selected possible markers of angiogenesis
have been investigated. It has been repeatedly found that CD105 is
a better marker of tumor angiogenesis than pan-endothelial markers
such as CD31, CD34, and von Willebrand factor (6,18,19). One of the reasons for this is that
CD105 is an accessory receptor for transforming growth factor beta
(TGF-β) (20,21). The main function of TGF-β is mediated
through tyrosine/threonine kinase receptors on the cell surface,
including TGF-β type II receptor, TGF-β type I receptor, and CD105.
TGF-β is known to participate in angiogenesis by stimulating or
inhibiting the activation of endothelial cells through a balance of
activin-like kinase (ALK) 5 and ALK1 signaling. Phosphorylation of
Smad1/5/8 after activation of ALK1 activates endothelial cells to
migrate and proliferate (22).
Immunostaining of tissue sections from various histological types
of human tumors has shown that CD105 is strongly expressed in the
endothelial cells of tumor blood vessels, but is either
undetectable or only weakly present in blood vessels of most normal
tissue (8). MVD estimated by
monoclonal antibodies to CD105 can reportedly be used to
differentiate between low-grade and high-grade dysplasia and
between high-grade dysplasia and colorectal cancer. In contrast,
MVD estimated by monoclonal antibodies to CD34 reportedly cannot be
used to distinguish between these pathologies (9,20). MVD
estimated by monoclonal antibodies to CD105 is inversely correlated
with survival in patients with non-small cell lung cancer,
hepatocellular cancer, and breast cancer, whereas MVD estimated by
monoclonal antibodies to CD34 does not show this inverse
correlation (8,20,23–25).
Additionally, MVD estimated by monoclonal antibodies to CD105
correlates more strongly with the amount of vascular endothelial
growth factor than does MVD estimated by monoclonal antibodies to
CD31 or CD34 (20,24,26).
Accordingly, the most frequently used immunohistochemical marker
for identifying activated endothelial cells is CD105.
Angiogenesis is essential for tumor growth and
metastasis. Therefore, angiogenesis is currently a target of cancer
therapy. For example, bevacizumab is a humanized monoclonal
antibody with a high affinity for circulating vascular endothelial
growth factor A (27). Clinical
trials of first- and second-line treatment of metastatic colorectal
cancer have confirmed that the addition of bevacizumab to standard
first-line chemotherapy regimens significantly improves patient
outcomes (28–31); hence, it is important to investigate
both the relationship between MVD and metastasis and potentially
confounding clinicopathological factors. MVD and regional lymph
node metastasis are reportedly risk factors for distant metastasis
(6,17). However, data on potentially
confounding factors such as lymphatic and vascular infiltration and
tumor size are lacking. Another study has shown that lymphatic and
vascular infiltration are risk factors for recurrence of colorectal
cancer (32). We therefore expected
that the stepwise multiple logistic regression analysis in the
present study would confirm that lymphatic and vascular
infiltration are risk factors for distant metastasis, but the
analysis did not confirm this. One possible explanation for this
apparent discrepancy is that generally, vascular infiltration
reflects the risk of hematogenous metastasis and lymphatic
infiltration reflects the risk of lymphatic metastasis. In this
study, we investigated the risk of distant metastases, including
hematogenous and lymphatic metastasis and peritoneal dissemination.
One of the mechanisms of colorectal peritoneal dissemination is
transcoelomic invasion by the primary cancer (33). Transcoelomic invasion implies prior
primary tumor growth and current tumor growth. Angiogenesis is
essential for tumor growth. Therefore, it is assumed that
angiogenesis is essential for transcoelomic invasion. Moreover, it
has been demonstrated that angiogenesis correlates with both
hematogenous and lymphatic metastasis (7,17).
Accordingly, it is conceivable that MVD is a more appropriate risk
factor for distant metastasis than is lymphatic and vascular
infiltration. This is a novel finding of the present study.
Moreover, to facilitate the clinical application of our findings,
we used an ROC curve to determine the optimal cut-off point for MVD
(10 vessels/x400 field). The incidence of distant metastasis
differed significantly between MVD above and below this cut-off
point. The main objective of surveillance after curative resection
of colorectal cancer is to detect recurrence early (32); intensive surveillance after curative
resection of colorectal cancer reportedly improves prognosis
(3). However, intensive surveillance
is costly, and the optimal duration and frequency of surveillance
has not yet been determined (32).
Determination of appropriate risk factors for distant metastasis
may help to identify patients who need intensive surveillance, thus
improving the efficacy of follow-up.
Another problem is that the areas of a primary tumor
with the highest MVD contain the cells that are most likely to
disseminate systemically. These metastasizing cells are more likely
to express the angiogenic phenotype than are cells escaping from
areas with fewer microvessels. However, it has been shown that
tumor cells that are not angiogenic may form dormant
micrometastases that eventually switch to the angiogenic phenotype
(34). In other words, dormant
micrometastases may become angiogenic and grow long after resection
of the original cancer (35). Thus,
cancers with high MVD may harbor undetectable micrometastases,
increasing the false-negative rate. This problem has not yet been
resolved and thus further study is needed.
This study has some limitations. First, we excluded
patients who had not been followed up for at least 5 years. Second,
this was a single-center retrospective study with the inherent
possibility of selection bias. Third, estimation of tumor budding
in T1 colorectal cancer was not described. It was not an
established outcome because only one patient had distant
metastasis.
In conclusion, our analysis suggests that MVD
estimated by monoclonal antibodies to CD105, regional lymph node
metastasis, and tumor size are a more appropriate risk factors for
distant metastasis from colorectal cancer than other potential
confounding clinicopathological factors.
Acknowledgements
We would like to thank T. Nagai and Y. Sasaki of the
Department of Pathology and Laboratory Medicine, Showa University
School of Medicine for providing valuable assistance with the
immunohistochemical analysis of the tissue samples. Edanz Group
assisted with English language editing.
References
|
1
|
Haggar FA and Boushey RP: Colorectal
cancer epidemiology: Incidence, mortality, survival, and risk
factors. Clin Colon Rectal Surg. 22:191–197. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cidon EU, Alonso P and Masters B: Markers
of response to antiangiogenic therapies in colorectal cancer: Where
are we now and what should be next? Clin Med Insights Oncol. 10
Suppl 1:S41–S55. 2016. View Article : Google Scholar
|
|
3
|
Figueredo A, Rumble RB, Maroun J, Earle
CC, Cummings B, McLeod R, Zuraw L and Zwaal C; Gastrointestinal
Cancer Disease Site Group of Cancer Care Ontario's Program in
Evidence-based Care, : Follow-up of patients with curatively
resected colorectal cancer: A practice guideline. BMC Cancer.
3:262003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zetter BR: Angiogenesis and tumor
metastasis. Annu Rev Med. 49:407–424. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kumar P, Wang JM and Bernabeu C: CD 105
and angiogenesis. J Pathol. 178:363–366. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Romani AA, Borghetti AF, Del Rio P,
Sianesi M and Soliani P: The risk of developing metastatic disease
in colorectal cancer is related to CD105-positive vessel count. J
Surg Oncol. 93:446–455. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Weidner N, Semple JP, Welch WR and Folkman
J: Tumor angiogenesis and metastasis-correlation in invasive breast
carcinoma. N Engl J Med. 324:1–8. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kumar S, Ghellal A, Li C, Byrne G, Haboubi
N, Wang JM and Bundred N: Breast carcinoma: Vascular density
determined using CD105 antibody correlates with tumor prognosis.
Cancer Res. 59:856–861. 1999.PubMed/NCBI
|
|
9
|
Akagi K, Ikeda Y, Sumiyoshi Y, Kimura Y,
Kinoshita J, Miyazaki M and Abe T: Estimation of angiogenesis with
anti-CD105 immunostaining in the process of colorectal cancer
development. Surgery. 131 Suppl 1:S109–S113. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Goldis DS, Sferdian MF, Tarţă C, Fulger
LO, Totolici BD and Neamţu C: Comparative analysis of microvessel
density quantified through the immunohistochemistry expression of
CD34 and CD105 in rectal cancer. Rom J Morphol Embryol. 56:419–424.
2015.PubMed/NCBI
|
|
11
|
Ottaviano G, Cappellesso R, Mylonakis I,
Lionello M, Favaretto N, Giacomelli L, Spoladore C, Marchese-Ragona
R, Marino F, Staffieri A, et al: Endoglin (CD105) expression in
sinonasal polyposis. Eur Arch Otorhinolaryngol. 272:3367–3373.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hamilton SR: Carcinoma of the colon and
rectumWHO Classification of Tumours of the Digestive System. Bosman
FT, Carneiro F, Hruban RH and Theise ND: IARC Press; Lyon: pp.
134–146. 2010
|
|
13
|
Watanabe T, Itabashi M, Shimada Y, Tanaka
S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, et
al: Japanese Society for Cancer of the Colon and Rectum (JSCCR)
guidelines 2010 for the treatment of colorectal cancer. Int J Clin
Oncol. 17:1–29. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Miyachi H, Kudo SE, Ichimasa K, Hisayuki
T, Oikawa H, Matsudaira S, Kouyama Y, Kimura YJ, Misawa M, Mori Y,
et al: Management of T1 colorectal cancers after endoscopic
treatment based on the risk stratification of lymph node
metastasis. J Gastroenterol Hepatol. 31:1126–1132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bosari S, Lee AK, DeLellis RA, Wiley BD,
Heatley GJ and Silverman ML: Microvessel quantitation and prognosis
in invasive breast carcinoma. Hum Pathol. 23:755–761. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Vermeulen PB, Gasparini G, Fox SB,
Colpaert C, Marson LP, Gion M, Beliën JA, de Waal RM, van Marck E,
Magnani E, et al: Second international consensus on the methodology
and criteria of evaluation of angiogenesis quantification in solid
human tumours. Eur J Cancer. 38:1564–1579. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Saad RS, Liu YL, Nathan G, Celebrezze J,
Medich D and Silverman JF: Endoglin (CD105) and vascular
endothelial growth factor as prognostic markers in colorectal
cancer. Mod Pathol. 17:197–203. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Seon BK, Takahashi N, Haba A, Matsuno F,
Haruta Y, She XW, Harada N and Tsai H: Angiogenesis and metastasis
marker of human tumors. Rinsho Byori. 49:1005–1013. 2001.PubMed/NCBI
|
|
19
|
Li C, Gardy R, Seon BK, Duff SE, Abdalla
S, Renehan A, O'Dwyer ST, Haboubi N and Kumar S: Both high
intratumoral microvessel density determined using CD105 antibody
and elevated plasma levels of CD105 in colorectal cancer patients
correlate with poor prognosis. Br J Cancer. 88:1424–1431. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nassiri F, Cusimano MD, Scheithauer BW,
Rotondo F, Fazio A, Yousef GM, Syro LV, Kovacs K and Lloyd RV:
Endoglin (CD105): A review of its role in angiogenesis and tumor
diagnosis, progression and therapy. Anticancer Res. 31:2283–2290.
2011.PubMed/NCBI
|
|
21
|
Sica G, Lama G, Anile C, Geloso MC, La
Torre G, de Bonis P, Maira G, Lauriola L, Jhanwar-Uniyal M and
Mangiola A: Assessment of angiogenesis by CD105 and nestin
expression in peritumor tissue of glioblastoma. Int J Oncol.
38:41–49. 2011.PubMed/NCBI
|
|
22
|
Park S, Sorenson CM and Sheibani N:
PECAM-1 isoforms, eNOS and endoglin axis in regulation of
angiogenesis. Clin Sci (Lond). 129:217–234. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tabata M, Kondo M, Haruta Y and Seon BK:
Antiangiogenic radioimmunotherapy of human solid tumors in SCID
mice using (125)I-labeled anti-endoglin monoclonal antibodies. Int
J Cancer. 82:737–742. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tanaka F, Otake Y, Yanagihara K, Kawano Y,
Miyahara R, Li M, Yamada T, Hanaoka N, Inui K and Wada H:
Evaluation of angiogenesis in non-small cell lung cancer:
Comparison between anti-CD34 antibody and anti-CD105 antibody. Clin
Cancer Res. 7:3410–3415. 2001.PubMed/NCBI
|
|
25
|
Yao Y, Pan Y, Chen J, Sun X, Qiu Y and
Ding Y: Endoglin (CD105) expression in angiogenesis of primary
hepatocellular carcinomas: Analysis using tissue microarrays and
comparisons with CD34 and VEGF. Ann Clin Lab Sci. 37:39–48.
2007.PubMed/NCBI
|
|
26
|
Yao Y, Kubota T, Takeuchi H and Sato K:
Prognostic significance of microvessel density determined by an
anti-CD105/endoglin monoclonal antibody in astrocytic tumors:
Comparison with an anti-CD31 monoclonal antibody. Neuropathology.
25:201–206. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Allegra CJ, Yothers G, O'Connell MJ,
Sharif S, Petrelli NJ, Colangelo LH, Atkins JN, Seay TE,
Fehrenbacher L, Goldberg RM, et al: Phase III trial assessing
bevacizumab in stages II and III carcinoma of the colon: Results of
NSABP protocol C-08. J Clin Oncol. 29:11–16. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Goel S, Duda DG, Xu L, Munn LL, Boucher Y,
Fukumura D and Jain RK: Normalization of the vasculature for
treatment of cancer and other diseases. Physiol Rev. 91:1071–1121.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hurwitz H, Fehrenbacher L, Novotny W,
Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S,
Holmgren E, et al: Bevacizumab plus irinotecan, fluorouracil, and
leucovorin for metastatic colorectal cancer. N Engl J Med.
350:2335–2342. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Saltz LB, Clarke S, Díaz-Rubio E,
Scheithauer W, Figer A, Wong R, Koski S, Lichinitser M, Yang TS,
Rivera F, et al: Bevacizumab in combination with oxaliplatin-based
chemotherapy as first-line therapy in metastatic colorectal cancer:
A randomized phase III study. J Clin Oncol. 26:2013–2019. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Tebbutt NC, Wilson K, Gebski VJ, Cummins
MM, Zannino D, van Hazel GA, Robinson B, Broad A, Ganju V, Ackland
SP, et al: Capecitabine, bevacizumab, and mitomycin in first-line
treatment of metastatic colorectal cancer: Results of the
Australasian Gastrointestinal Trials Group Randomized Phase III MAX
Study. J Clin Oncol. 28:3191–3198. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kobayashi H, Mochizuki H, Ishiguro M and
Sugihara K: Risk factor for distant metastasis from colorectal
cancer and surveillance. Frontier in Colorectal Cancer. 4:264–268.
2008.(In Japanese).
|
|
33
|
Wang Y, Gong C, Yang L, Wu Q, Shi S, Shi
H, Qian Z and Wei Y: 5-FU-hydrogel inhibits colorectal peritoneal
carcinomatosis and tumor growth in mice. BMC Cancer. 10:4022010.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Folkman J: Seminars in Medicine of the
Beth Israel Hospital, Boston. Clinical applications of research on
angiogenesis. N Engl J Med. 333:1757–1763. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Folkman J: Fighting cancer by attacking
its blood supply. Sci Am. 275:150–154. 1996. View Article : Google Scholar : PubMed/NCBI
|