Introduction
Breast cancer is a heterogeneous group of diseases
that develops from the mammary gland. It varies in morphology,
biological characteristics, behavior and response to therapy
(1). However, the complex
associations between various tumor characteristics and patient age
at the time of diagnosis have not yet been elucidated. A large
number of risk factors for breast cancer have now been identified.
These include: Geographic variations; race and ethnicity (2,3); prolonged
exposure to exogenous estrogens post-menopausally (including
hormone replacement therapy used in the prevention of osteoporosis)
(4–7);
obesity (due to estrogens produced by the adipose tissue) (8–10); alcohol
abuse (11); genetic inheritance
(mutations in breast cancer 1 and 2) (12–14); lack
of physical activity (15); ionizing
radiation to the chest (depending on radiation dose, age and time
following exposure) (16–19); and early age at menarche or late age
of pregnancy and menopause (20).
It is also established that the incidence of breast
cancer increases with age. The number of elderly patients with
breast cancer is increasing and the majority of females who succumb
to breast cancer are >65 years old (21). However, older patients are more likely
to present with tumors that are estrogen receptor (ER)- and
progesterone receptor (PR)-positive and human epidermal growth
factor receptor 2 (HER2)-negative, and these tumors are associated
with improved prognosis and clinical outcomes (22,23). By
contrast, younger patients with triple-negative and HER2-positive
breast cancers have an increased risk of relapse within 5 years of
diagnosis (24). Breast cancer that
arises in young females is associated with reduced survival and
higher incidence of unfavorable prognostic and predictive tumor
markers (25–28).
Using gene expression analysis, breast cancer is
able to be divided into six intrinsic molecular subtypes: Luminal A
(ER+ and/or PR+, HER2− and Ki-67
<14%), luminal B (ER+ and/or PR+,
HER2− and Ki-67 ≥14%, or ER+ and/or
PR+ and HER2+), HER2-enriched
(ER−, PR− and HER2+),
basal-like/triple-negative (ER−, PR− and
HER2−), normal breast-like and claudin-low [cluster of
differentiation (CD)44+ and CD24− or low]
(29,30). Molecular subtyping using four
biomarkers (ER, PR, HER2 and Ki-67) and dividing tumors into four
subtypes (basal cell-like, HER2 positive luminal A and luminal B)
also provide clinically useful information concerning the biology
of tumors and their clinical behavior. Therefore, they have been
proposed for use in determining the efficacy of therapy and
surveillance strategies (31–37).
To the best of our knowledge, no comprehensive
prognostic or predictive marker analysis has been performed to date
in association with age in patients with breast cancer. The present
study therefore aims to correlate the comprehensive basic
clinicopathological data with age.
Materials and methods
Patients and diagnostic tests
The present study analyzed the age-specific presence
of prognostic and predictive markers in a sample of 632
formalin-fixed, paraffin-embedded breast cancer samples obtained
from core-cut biopsies or mastectomies performed at the Department
of Clinical and Molecular Pathology, University Hospital, Palacky
University (Olomouc, Czech Republic) between January 2010 and April
2014, using standard immunohistochemistry (IHC) and fluorescence in
situ hybridization (FISH). The present study was approved by the
Ethics Committee of the University Hospital and the Faculty of
Medicine and Dentistry of Palacky University. Informed consent was
obtained from patients for the use of their tissues. The median
patient age was 65 years (range, 26–95 years). Sections of breast
cancer samples (5-µm thick) were used for examination of ER and PR
expression, HER2 protein expression, markers of proliferation
[including proliferating cell nuclear antigen (PCNA) and Ki-67],
and B-cell lymphoma (Bcl)-2 and HER2 gene amplification. The
clinicopathological data were obtained from the primary pathology
reports. All findings were verified by two independent pathologists
of the Department of Clinical and Molecular Pathology, University
Hospital, Palacky University.
Immunohistochemistry (IHC)
The protocol for IHC was as follows: Slides were
deparaffinized, exposed to heat-induced antigen retrieval in a
microwave oven for 15 min at 121°C in a 10 mM sodium citrate buffer
(pH 6.0; cat. no. C8532; Sigma-Aldrich; Merck KGaA, Darmstadt,
Germany), and endogenous peroxidase activity was blocked by
incubation with a 5% hydrogen peroxide blocking solution (0.01 M
PBS, pH 7.4, containing 0.01% thimerosal) for 10 min. The sections
were incubated with diluted primary antibodies for 60 min at room
temperature (RT) and subsequently with the secondary antibody Dako
EnVision+ Dual Link System-HRP (cat. no. K4061; Agilent
Technologies, Inc., Santa Clara, CA, USA) for 60 min at room
temperature. The Dako Liquid DAB+ Substrate Chromogen System (cat.
no. K3468; Agilent Technologies, Inc., Santa Clara, CA, USA) was
used for the visualization according the manufacture's protocol.
Sections were then counterstained with hematoxylin, dehydrated,
cleared, mounted and covered. IHC evaluation of ER expression was
performed using monoclonal mouse anti-human primary antibody, clone
1D5 (cat. no. M7047; dilution, 1:20; Dako; Agilent Technologies,
Inc., Santa Clara, CA, USA). PR expression was determined by
monoclonal mouse anti-human antibody, clone PgR 636 (cat. no.
M3569; dilution, 1:100; Dako; Agilent Technologies, Inc., Santa
Clara, CA, USA). The proliferative markers PCNA and Ki-67 were
detected using monoclonal mouse anti-PCNA, clone PC10 (cat. no.
M0879; dilution, 1:1,500; Dako; Agilent Technologies, Inc.) for
PCNA and monoclonal mouse anti-human Ki-67 antigen, clone MIB-1
(cat. no. M7240; dilution, 1:200; Dako; Agilent Technologies, Inc.)
for Ki-67. Bcl-2 was determined by anti-Bcl-2 oncoprotein, clone
100, which reacts with Bcl-2 alpha oncoprotein (Cat. no. AM287-10M;
dilution, 1:10; BioGenex; Fremont, CA, USA). Hormone receptors (ER
and PR), PCNA, Ki-67 and Bcl-2 were evaluated using the
histological score (H-score) as follows: Percentage of positive
cells × intensity of staining (1, 2 or 3). The age distribution of
the analyzed markers was evaluated. Due to the small number of
patients aged 20–29 and 90–99 years, the 20–29 years group was
combined with the 30–39 years group and the 80–89 years group was
combined with the 90–99 years group for statistical evaluation.
HER2 protein expression was determined according manufacturer's
protocol using the in vitro diagnostic certified kit
HercepTest™ (Dako; Agilent Technologies, Inc., Catalogue No.
K5204). The expression of HER2 was scored on a qualitative scale
from 0 to 3+ according to the Dako manual (Agilent Technologies,
Inc.) and the guidelines for HER2 testing in breast cancer from the
American Society of Clinical Oncology (ASCO)/College of American
Pathologists (CAP) (38). A score of
0 or 1+ was assessed as negative, 2+ as moderately positive and 3+
as positive (uniform intense staining of >30% of invasive tumor
cells). IHC with HercepTest™ and anti-hormone receptor primary
antibodies were performed on the invasive breast cancer tissue
samples.
Fluorescence in situ
hybridization
The HER2 gene status was assessed using FISH
analysis, which was performed according to the manufacturer's
protocol on formalin-fixed, paraffin-embedded tissues.
Locus-specific identifier HER2/neu (Spectrum Orange™) and
chromosome 17 centromere (CEP17; Spectrum Green™) probes (cat. no.
IM_001; IntellMed, Ltd., Olomouc, Czech Republic) were used for
gene/chromosome copy number enumeration. The signals were observed
and counted using fluorescence microscopy. At least 100
non-overlapping nuclei were selected in each sample. Cut-off levels
were determined according to the ASCO/CAP recommendations. A
HER2/CEP17 ratio of >2.2 was considered as positive (38,39).
Statistical analysis
The data were evaluated using IBM SPSS version 22.0
(IBM SPSS, Armonk, NY, USA). The correlation analysis for ER, PR,
PCNA, Ki-67, Bcl-2, HER2 protein (using IHC) and HER2 gene (using
FISH) expression with age and tumor grade was performed using the
Spearman's rank correlation coefficient. The associations between
ER, PR, PCNA, Bcl-2, Ki-67, grade, HER2 protein and HER2 gene with
histological type and molecular subtype were evaluated using the
Kruskal-Wallis test. Mann-Whitney U-tests with Bonferroni
correction were used for pairwise comparisons. The data
distribution was presented using box graphs. To examine the
correlations between HER2 protein expression and molecular subtype
or between histological type and molecular subtype, Fisher's exact
test was used. P<0.05 was considered to indicate a statistically
significant difference.
Results
Age-specific associations with hormone
receptors
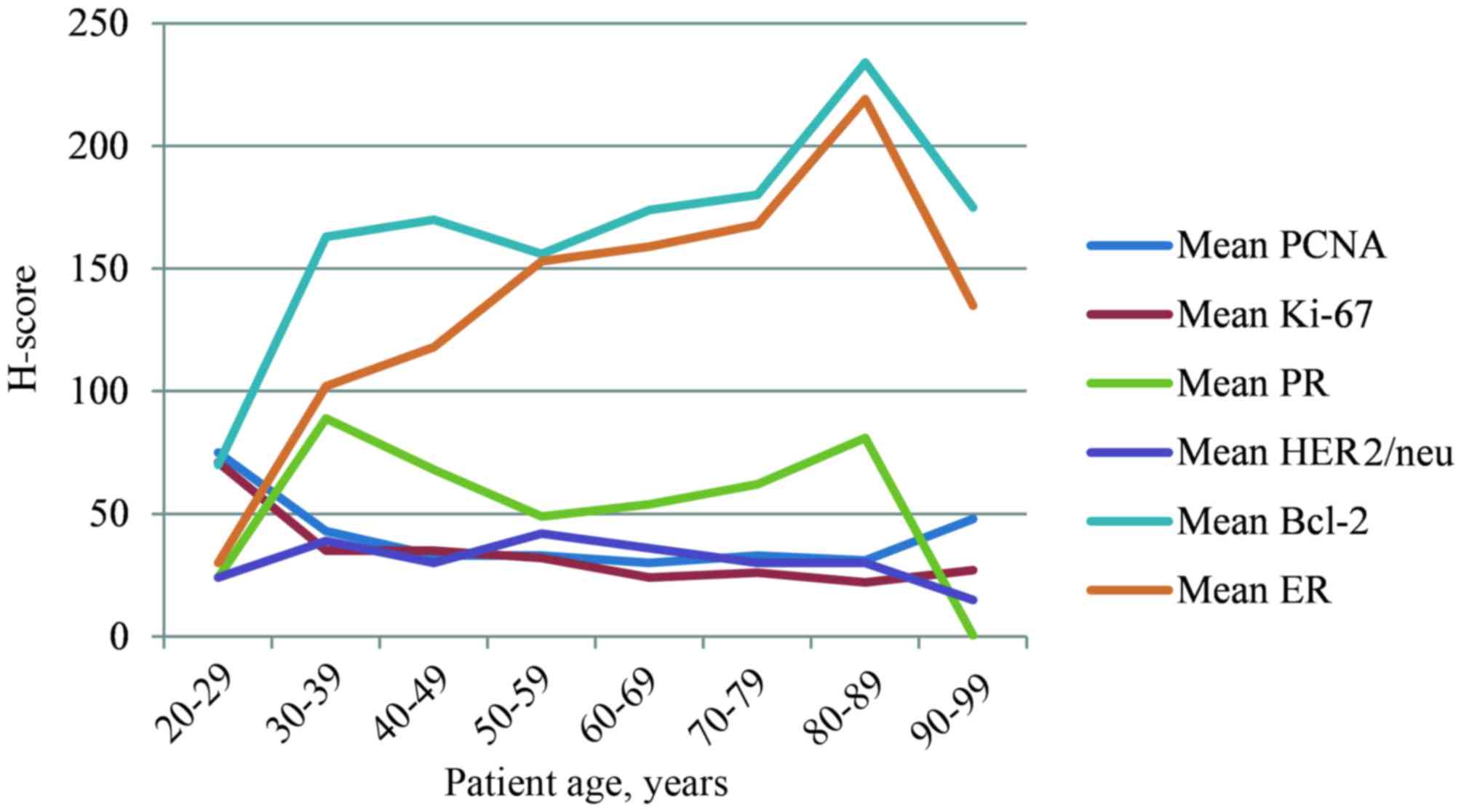
The present study identified a significant positive
correlation between age and ER expression, between ER and PR
expression and between Bcl-2 expression and molecular subtypes (all
P<0.0001). By contrast, an inverse association between ER
expression and the grade of tumor (P<0.0001), amplification of
the HER2 gene [all P<0.0001; odds ratio (OR), 1.003; 95%
confidence interval (CI), 1.000–1.005] and the markers of
proliferation PCNA and Ki-67 (P<0.0001) was detected. No
statistically significant correlation between age and PR expression
was identified; however, there were positive associations between
PR expression and the expression of HER2 protein (P=0.001), Bcl-2
protein (P<0.0001) and molecular subtypes (P<0.0001). By
contrast, there were inverse associations with tumor grade
(P<0.0001), PCNA (P=0.004) and Ki-67 (P<0.0001). The highest
levels of ER and Bcl-2 expression were observed in patients aged
70–79 years old, whereas PR expression was highest in patients aged
30–39 years old (Fig. 1).
Age-specific associations with HER2
protein expression
A statistically significant positive correlation
between HER2 protein expression and PR expression (P=0.001),
amplification of the HER2 gene (P<0.0001; OR, 1,290; 95% CI,
1.000–1.665) and tumor grade (P=0.0002), and a negative correlation
between HER2 expression and Bcl-2 expression (P=0.003) were
identified. No statistically significant negative correlation was
identified between age and HER2 protein expression (P=0.159).
Age-specific associations with
proliferative markers
A significant negative correlation was identified
between age and Ki-67 expression (P<0.0001). Ki-67 also
exhibited an inverse association with Bcl-2 (P<0.0001), and was
associated with tumor grade (P<0.0001), HER2 protein expression
(P=0.032), HER2 gene amplification (P=0.007), PCNA expression
(P<0.0001), histological type (P<0.0001) and molecular
subtype (P<0.0001). No significant associations between age and
PCNA expression were identified.
Age-specific associations with Bcl-2
expression
A statistically significant positive correlation
between Bcl-2 and hormone receptor expression and molecular subtype
was identified. High levels of Bcl-2 expression in luminal A and
luminal B subtypes were observed in comparison with the
HER2+ and triple-negative breast cancer (TNBC) molecular
subtypes. The significant correlation between Bcl-2 expression
levels and hormone receptor expression, demonstrates that Bcl-2 is
a potential effective marker of breast cancer hormonal
responsiveness. By contrast, an inverse association was identified
between Bcl-2 and HER2 protein expression levels and proliferative
markers.
Age-specific associations between
tumor grade and histological type
A statistically significant positive correlation
between tumor grade and HER2 protein expression (P=0.0002), Ki-67
(P<0.0001) and molecular subtype (P<0.0001) was identified.
Conversely an inverse association was detected between tumor grade
and hormone receptor (ER and PR) expression levels. In the present
study of 632 breast cancer tissue samples, the following
distribution of histological types was observed: Invasive ductal
breast cancer [invasive cancer of no special type according to the
WHO Classification of Tumors of the Breast (1)], 82.0%; in situ ductal breast cancer,
9.7%; invasive lobular breast cancer, 5.8%; breast cancers with
poor prognosis, including metaplastic and micropapillary breast
cancer, 0.5%; medullary breast cancer, 0.3%; and other types of
breast cancer with improved prognosis (tubular, mucinous,
cribriform and papillary; 1.7%) (Table
I). The highest incidence of invasive and non-invasive ductal
breast cancer cases was observed in patients aged 60–69 years (mean
age, 65 years). The occurrence of these types of breast cancer was
predominant also in younger patients (<50 years old), and these
two histological types exhibited the highest levels of HER2
expression. The incidence of invasive lobular breast cancer
increased between the ages of 50 and 70 years.
 | Table I.Age-associated distribution of tumor
histological types. |
Table I.
Age-associated distribution of tumor
histological types.
|
|
|
| Histological
typea |
|---|
|
|
|
|
|
|---|
| Age, years | Number of
patients | Mean age,
years | 1 | 2 | 3 | 4 | 5 | 6 |
|---|
| 20–29 |
4 | 29 |
4 | 0 | 0 | 0 | 0 | 0 |
| 30–39 | 30 | 36 | 25 | 4 | 1 | 0 | 0 | 0 |
| 40–49 | 79 | 46 | 66 | 8 | 4 | 0 | 0 | 1 |
| 50–59 | 158 | 56 | 130 | 16 | 8 | 0 | 1 | 3 |
| 60–69 | 203 | 65 | 163 | 25 | 10 | 2 | 0 | 3 |
| 70–79 | 111 | 75 | 88 | 7 | 11 | 1 | 1 | 3 |
| 80–89 | 41 | 84 | 36 | 1 | 3 | 0 | 0 | 1 |
| 90–99 |
6 | 93 |
6 | 0 | 0 | 0 | 0 | 0 |
| Total | 632 | 61 | 518 | 61 | 37 | 3 | 2 | 11 |
Age-specific associations with
molecular subtypes
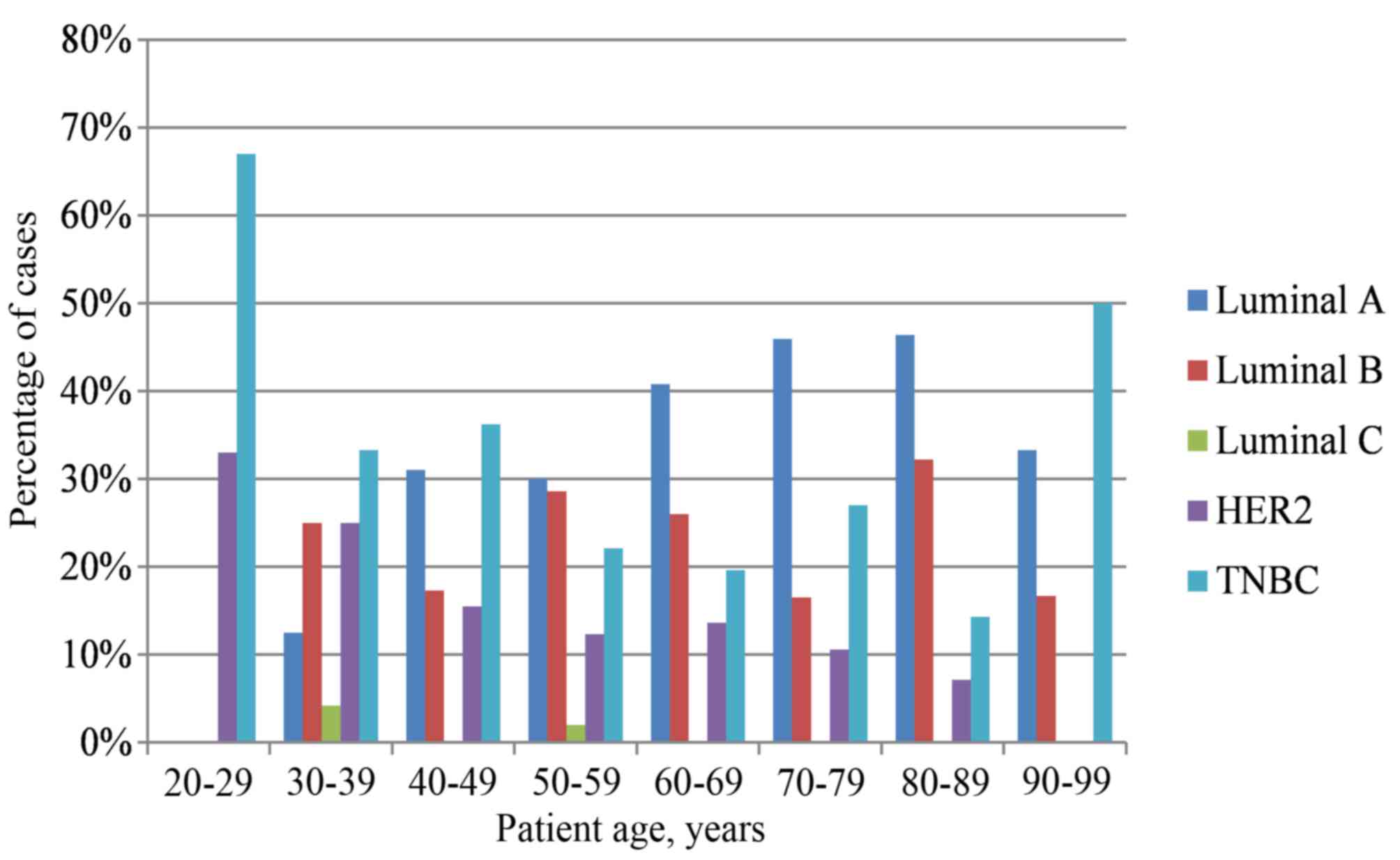
The distribution of molecular subtypes was as
follows: 35% luminal A, 25% luminal B, 1% luminal C, 14%
HER2+ and 25% TNBC. The highest incidence of TNBC and
HER2-positive breast cancer was detected in the youngest patient
groups (20–39 years old). However, in patients aged ≥40 years old,
the luminal A molecular subtype was most commonly observed
(Table II and Fig. 2). The age of patients with luminal A
breast cancer was statistically significantly higher compared with
that of patients with the HER2+ and TNBC molecular
subtypes (P<0.0001). Statistically significant positive
correlations between molecular subtypes and ER expression
(P<0.0001), PR expression (P<0.0001), Ki-67 expression
(P<0.0001), PCNA expression (P<0.0001), tumor grade
(P<0.0001), histological type (P<0.0001), expression of HER2
protein (P<0.0001), and amplification of the HER2 gene
(P<0.0001) and the Bcl-2 proto-oncogene (P<0.0001) were also
observed. Those breast cancer cases that were identified as luminal
A molecular subtype were exclusively composed of the most favorable
histological types in terms of prognosis, including mucinous,
tubular and papillary cribriform breast cancer. Luminal B molecular
subtype cancer cases had a significantly higher grade than luminal
A cancer cases (P=0.001) and a significantly lower grade than
HER2+ cases (P<0.0001). The distribution of invasive
and non-invasive ductal breast cancer [invasive ductal carcinoma
(IDC) or ductal carcinoma in situ (DCIS)] between molecular
subtypes was more heterogeneous (IDC: 35.8% luminal A, 24.7%
luminal B, 10.9% HER2+ and 27.9% TNBC; and DCIS: 26.7%
luminal A, 26.7% luminal B, 33.3% HER2+ and 11.7% TNBC).
In the IDC and DCIS groups, the highest incidence of HER2
positivity was identified. The overexpression and amplification of
HER2 were significantly higher in HER2+ and luminal B
molecular subtypes compared with the other molecular subtypes. The
distribution of invasive and non-invasive lobular breast cancer was
divided between the luminal A (53.3%), luminal B (33.3%) and
HER2+ (13.3%) subtypes. The expression levels of Ki-67
and PCNA were significantly higher in the HER2+ and TNBC
molecular subtypes than in the two luminal subtypes.
 | Table II.Age-associated distribution of
molecular subtypes. |
Table II.
Age-associated distribution of
molecular subtypes.
| Age, years | Luminal A, % | Luminal B, % | Luminal C, % | HER2, % | TNBC, % |
|---|
| 20–29 |
0.00 |
0.00 | 0.00 | 33.00 | 67.00 |
| 30–39 | 12.50 | 25.00 | 4.20 | 25.00 | 33.30 |
| 40–49 | 31.00 | 17.30 | 0.00 | 15.50 | 36.20 |
| 50–59 | 30.00 | 28.60 | 2.00 | 12.30 | 22.10 |
| 60–69 | 40.80 | 26.00 | 0.00 | 13.60 | 19.60 |
| 70–79 | 45.90 | 16.50 | 0.00 | 10.60 | 27.00 |
| 80–89 | 46.40 | 32.20 | 0.00 |
7.10 | 14.30 |
| 90–99 | 33.30 | 16.70 | 0.00 |
0.00 | 50.00 |
Discussion
The present study aimed to elucidate the
associations between common clinicopathological characteristics of
breast cancer and the patient age distribution. The results
revealed that these prognostic and predictive markers have an
age-specific distribution. More aggressive breast cancers were
observed primarily in younger patients (20–39 years old), whereas
the breast cancer types with improved prognosis were associated
with older patients (≥40 years old). Proliferative activity
declined with age, and the expression of hormone receptors and
Bcl-2 increased with age. Young females exhibited tumors with a
higher grade and HER2+ and TNBC molecular subtypes. To
the best of our knowledge, no comprehensive analysis of all these
characteristics has been performed to date, and there are limited
previous studies concerning this subject. Diab et al
(22) described the association
between increasing age at the time of diagnosis and HER2 protein
expression in patients with breast cancer who were ≥55 years old.
Benz (25) compared the biology of
early-onset with late-onset breast cancer, and demonstrated that
late-onset tumors develop more slowly and are biologically less
aggressive than early-onset tumors. Anders et al (40) revealed that young females have lower
ER positivity, larger tumors, higher levels of human epidermal
growth factor receptor 2 expression, higher-grade tumors, lymph
node positivity and a tendency towards reduced disease-free
survival.
In the present study, the age of patients with
luminal A breast cancer was significantly higher compared with that
of patients with the HER2+ and TNBC molecular subtypes.
Furthermore, de Kruijf et al (41) also identified a statistically
significant association (P=0.02) between patient age and tumor
molecular subtype with luminal tumors being more frequently
identified in elderly patients, whereas HER2+,
basal-like and unclassified subtypes were more commonly detected in
younger patients. A similar trend was described in the study by
Park et al (33), in which
poor patient outcomes were associated with an increased frequency
of triple-negative/HER2 subtypes and more aggressive clinical
behavior in young patients, in contrast to ER-positive tumors in
older patients. Jenkins et al (42) examined the association between age and
subtype, and recurrence-free, disease-specific and overall survival
in older females. In this previous study, the incidence of luminal
subtypes increased with age and had improved outcomes compared with
those of basal-cell like and HER2-enriched subtypes. Prat et
al (43) reported that
HER2-positive breast cancer cases had a higher frequency compared
with the HER-negative types of breast cancer of the HER2-enriched
subtype (47.0 vs. 7.1%) and a lower frequency of the basal-like
(14.1 vs. 23.4%) and luminal A (10.7 vs. 39.0%) subtypes. In this
previous study, the HER2 gene and protein expression levels were
statistically significantly higher in the HER2-enriched and
basal-like subtypes compared with those in the luminal subtype.
In the present cohort of patients, the distribution
of particular molecular subtypes was 35% luminal A, 25% luminal B,
1% luminal C, 14% HER2+ and 25% TNBC. The expression of
Ki-67 and PCNA was significantly higher in HER2+ and
TNBC subtypes compared with that in either luminal subtype. By
contrast, Ihemelandu et al (26) classified breast cancer into four
molecular subtypes (basal cell-like, HER2/neu, luminal A and
luminal B) and analyzed the prevalence and clinicopathological
associations for these molecular subtypes in pre- and
post-menopausal African-American females. The luminal A type was
the most prevalent (55.4%), whereas the basal cell-like form was
the most prevalent in the age group <35 years old, and also
exhibited an age-specific bimodal distribution, with a peak in
patients aged <35 and 51–65 years old (26). The basal cell-like and
HER2+ subtypes had a stronger association with a more
aggressive clinical course than the luminal A subtype (26). Park et al (33,44)
revealed that luminal A tumors were well differentiated and more
frequently co-expressed hormone receptors than the luminal B type.
Patients with TNBC tumors were younger at the time of diagnosis and
had larger, more undifferentiated tumors with a higher
proliferation rate and frequent visceral metastases (33).
A previous study made notable progress in aiding the
understanding of the role of the pro-survival protein Bcl-2, which
has an important role in regulating the pro-apoptotic effector
proteins Bcl-2 homologous antagonist/killer and Bcl-2-associated X
protein, and also neutralizes a group of sensor proteins, including
Bcl-2-like protein 11, which are triggered by cytotoxic stimuli
such as chemotherapy (45). The
correlation between Bcl-2 expression and patient outcome has been
the focus of a number of studies on primary breast cancer and,
paradoxically, Bcl-2 was identified to be a marker of improved
prognosis (45) across molecular
subtypes (46–49). The explanation for this paradox may be
that Bcl-2 is an estrogen-responsive gene (50) or that high levels of pro-apoptotic
Bcl-2 trigger mitochondrial priming (51). However, a previous study reported that
Bcl-2 expression is an independent factor predicting poor prognosis
in patients with hormone receptor-negative breast cancer or TNBC
who did not undergo adjuvant therapy, particularly in
post-menopausal females (52). The
present study reveals high expression levels of Bcl-2 in the
luminal A and luminal B subtypes of breast cancer in comparison
with that in the HER2+ and triple-negative molecular
subtypes. These results are concordant with those from Seong et
al (53), which also described a
significant association between Bcl-2-positive tumors, and a
younger patient age, early stage, lower grade, positive expression
of ER and PR, and negative expression of HER2. Patients with
Bcl-2/ER/PR-positive and HER2-negative tumors in this previous
study also exhibited an improved prognosis (53). A significant correlation between Bcl-2
expression levels and hormone receptor status demonstrates that
Bcl-2 is a potential effective marker of hormonal responsiveness in
patients with ER/PR positive breast cancer.
The present study provides a comprehensive look at
natural relations between levels of the most important breast
cancer prognostic and predictive biomarkers and the age of the
patients. It was demonstrated that there was an age-specific
distribution in the breast cancer patient population, and therefore
suggested the significance of age as an additional factor for an
increase in the reliability of estimation of disease progression.
The present study seeks to encourage oncologists to recognize Bcl-2
expression in estrogen receptor positive breast cancer samples as a
reliable indicator of the functional estrogen driven axis for
patients being considered for hormonal treatment.
Acknowledgements
The authors thank Dr Kateřina Langová, Department of
Medical Biophysics, Faculty of Medicine and Dentistry, Palacky
University, Olomouc, Czech Republic, for statistical analysis. The
present study was funded by the Czech Agency for Health Research
(grant no. 16-31997A).
References
|
1
|
Lakhani SR, Ellis IO, Schnitt SJ, Tan PH
and van de Vijver MJ: WHO Classification of Tumours of the
BreastInternational Agency for Research on Cancer. Lyon: 2012,
View Article : Google Scholar
|
|
2
|
Clarke CA, Keegan TH, Yang J, Press DJ,
Kurian AW, Patel AH and Lacey JV Jr: Age-specific incidence of
breast cancer subtypes: Understanding the black-white crossover. J
Natl Cancer Inst. 104:1094–1101. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kurian AW, Fish K, Shema SJ and Clarke CA:
Lifetime risks of specific breast cancer subtypes among women in
four racial/ethnic groups. Breast Cancer Res. 12:R992010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Olsson HL, Ingvar C and Bladström A:
Hormone replacement therapy containing progestins and given
continuously increases breast carcinoma risk in Sweden. Cancer.
97:1387–1392. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Clavel-Chapelon F and Hill C: Hormone
replacement therapy in menopause and risk of breast cancer. Presse
Med. 29:1688–1693. 2000.(In French). PubMed/NCBI
|
|
6
|
Bae JM and Kim EH: Hormone replacement
therapy and risk of breast cancer in Korean women: A quantitative
systematic review. J Prev Med Public Health. 48:225–230. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Predná L, Habánová M, Sláviková E and Wyka
J: Hormonal contraceptives and hormone replacement therapy as a
possible factor of breast cancer. Rocz Panstw Zakl Hig. 66:269–274.
2015.PubMed/NCBI
|
|
8
|
Orecchioni S, Reggiani F, Talarico G and
Bertolini F: Mechanisms of obesity in the development of breast
cancer. Discov Med. 20:121–128. 2015.PubMed/NCBI
|
|
9
|
Bertolini F: Adipose tissue and breast
cancer progression: A link between metabolism and cancer. Breast.
22:(Suppl 2). S48–S49. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bertolini F, Petit JY and Kolonin MG: Stem
cells from adipose tissue and breast cancer: Hype, risks and hope.
Br J Cancer. 112:419–423. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jayasekara H, MacInnis RJ, Room R and
English DR: Long-term alcohol consumption and breast, upper
aero-digestive tract and colorectal cancer risk: A systematic
review and meta-Analysis. Alcohol Alcohol. 51:315–330. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
van den Broek AJ, Schmidt MK, van't Veer
LJ, Tollenaar RA and van Leeuwen FE: Worse breast cancer prognosis
of BRCA1/BRCA2 mutation carriers: What's the evidence? A systematic
review with meta-analysis. PLoS One. 10:e01201892015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Llort G, Peris M and Blanco I: Hereditary
breast and ovarian cancer: Primary and secondary prevention for
BRCA1 and BRCA2 mutation carriers. Med Clin (Barc). 128:468–476.
2007.(In Spanish). View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Calderon-Margalit R and Paltiel O:
Prevention of breast cancer in women who carry BRCA1 or BRCA2
mutations: A critical review of the literature. Int J Cancer.
112:357–364. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Olsen CM, Wilson LF, Nagle CM, Kendall BJ,
Bain CJ, Pandeya N, Webb PM and Whiteman DC: Cancers in Australia
in 2010 attributable to insufficient physical activity. Aust N Z J
Public Health. 39:458–463. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Drooger JC, Hooning MJ, Seynaeve CM,
Baaijens MH, Obdeijn IM, Sleijfer S and Jager A: Diagnostic and
therapeutic ionizing radiation and the risk of a first and second
primary breast cancer, with special attention for BRCA1 and BRCA2
mutation carriers: A critical review of the literature. Cancer
Treat Rev. 41:187–196. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tang J, Fernandez-Garcia I, Vijayakumar S,
Martinez-Ruis H, Illa-Bochaca I, Nguyen DH, Mao JH, Costes SV and
Barcellos-Hoff MH: Irradiation of juvenile, but not adult, mammary
gland increases stem cell self-renewal and estrogen receptor
negative tumors. Stem Cells. 32:649–661. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Clemons M, Loijens L and Goss P: Breast
cancer risk following irradiation for Hodgkin's disease. Cancer
Treat Rev. 26:291–302. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Haffty BG: Radiation therapy and the risk
of contralateral breast cancer. Int J Radiat Oncol Biol Phys.
56:920–921. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kato I, Tominaga S and Suzuki T: Factors
related to late menopause and early menarche as risk factors for
breast cancer. Jpn J Cancer Res. 79:165–172. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Altekruse SF, Kosary CL, Krapcho M, Neyman
N, Aminou R, Waldron W, Ruhl J, Howlader N, Tatalovich Z, Cho H, et
al: SEER Cancer Statistics Review, 1975–2007. Bethesda, MD:
National Cancer Institute; 2010
|
|
22
|
Diab SG, Elledge RM and Clark GM: Tumor
characteristics and clinical outcome of elderly women with breast
cancer. J Natl Cancer Inst. 92:550–556. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Jenkins EO, Deal AM, Anders CK, Prat A,
Perou CM, Carey LA and Muss HB: Age-specific changes in intrinsic
breast cancer subtypes: A focus on older women. Oncologist.
19:1076–1083. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Walter LC and Covinsky KE: Cancer
screening in elderly patients: A framework for individualized
decision making. JAMA. 285:2750–2756. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Benz CC: Impact of aging on the biology of
breast cancer. Crit Rev Oncol Hematol. 66:65–74. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ihemelandu CU, Leffall LD Jr, Dewitty RL,
Naab TJ, Mezghebe HM, Makambi KH, Adams-Campbell L and Frederick
WA: Molecular breast cancer subtypes in premenopausal and
postmenopausal African-American women: Age-specific prevalence and
survival. J Surg Res. 143:109–118. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Eppenberger-Castori S, Moore DH Jr, Thor
AD, Edgerton SM, Kueng W, Eppenberger U and Benz CC: Age-associated
biomarker profiles of human breast cancer. Int J Biochem Cell Biol.
34:1318–1330. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Quong J, Eppenberger-Castori S, Moore D
III, Scott GK, Birrer MJ, Kueng W, Eppenberger U and Benz CC:
Age-dependent changes in breast cancer hormone receptors and
oxidant stress markers. Breast Cancer Res Treat. 76:221–236. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Camerlingo R, Ferraro GA, De Francesco F,
Romano M, Nicoletti G, Di Bonito M, Rinaldo M, D'Andrea F and
Pirozzi G: The role of CD44+/CD24-/low biomarker for screening,
diagnosis and monitoring of breast cancer. Oncol Rep. 31:1127–1132.
2014.PubMed/NCBI
|
|
30
|
Gudadze M, Kankava Q, Mariamidze A and
Burkadze G: Features of CD44+/CD24-low phenotypic cell distribution
in relation to predictive markers and molecular subtypes of
invasive ductal carcinoma of the breast. Georgian Med News.
228:81–87. 2014.
|
|
31
|
Eroles P, Bosch A, Pérez-Fidalgo JA and
Lluch A: Molecular biology in breast cancer: Intrinsic subtypes and
signaling pathways. Cancer Treat Rev. 38:698–707. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Morrison DH, Rahardja D, King E, Peng Y
and Sarode VR: Tumour biomarker expression relative to age and
molecular subtypes of invasive breast cancer. Br J Cancer.
107:382–387. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Park S, Koo JS, Kim MS, Park HS, Lee JS,
Lee JS, Kim SI and Park BW: Characteristics and outcomes according
to molecular subtypes of breast cancer as classified by a panel of
four biomarkers using immunohistochemistry. Breast. 21:50–57. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Reis-Filho JS and Tutt AN: Triple negative
tumours: A critical review. Histopathology. 52:108–118. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Rakha EA and Ellis IO:
Triple-negative/basal-like breast cancer: Review. Pathology.
41:40–47. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Prat A, Parker JS, Karginova O, Fan C,
Livasy C, Herschkowitz JI, He X and Perou CM: Phenotypic and
molecular characterization of the claudin-low intrinsic subtype of
breast cancer. Breast Cancer Res. 12:R682010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Santos C, Sanz-Pamplona R, Nadal E,
Grasselli J, Pernas S, Dienstmann R, Moreno V, Tabernero J and
Salazar R: Intrinsic cancer subtypes-next steps into personalized
medicine. Cell Oncol (Dordr). 38:3–16. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Wolff AC, Hammond ME, Hicks DG, Dowsett M,
McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M,
Fitzgibbons P, et al: Recommendations for human epidermal growth
factor receptor 2 testing in breast cancer: American Society of
Clinical Oncology/College of American Pathologists clinical
practice guideline update. Arch Pathol Lab Med. 138:241–256. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
LSI Her-2/neu (Orange)/CEP 17 (Green)
Users guide. Intellmed s.r.o.Olomouc; Czech Republic: 2006
|
|
40
|
Anders CK, Hsu DS, Broadwater G, Acharya
CR, Foekens JA, Zhang Y, Wang Y, Marcom PK, Marks JR, Febbo PG, et
al: Young age at diagnosis correlates with worse prognosis and
defines a subset of breast cancers with shared patterns of gene
expression. J Clin Oncol. 26:3324–3330. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
de Kruijf EM, Bastiaannet E, Rubertá F, de
Craen AJ, Kuppen PJ, Smit VT, van de Velde CJ and Liefers GJ:
Comparison of frequencies and prognostic effect of molecular
subtypes between young and elderly breast cancer patients. Mol
Oncol. 8:1014–1025. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Jenkins EO, Deal AM, Anders CK, Prat A,
Perou CM, Carey LA and Muss HB: Age-specific changes in intrinsic
breast cancer subtypes: A focus on older women. Oncologist.
19:1076–1083. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Prat A, Carey LA, Adamo B, Vidal M,
Tabernero J, Cortés J, Parker JS, Perou CM and Baselga J: Molecular
features and survival outcomes of the intrinsic subtypes within
HER2-positive breast cancer. J Natl Cancer Inst. 106:dju1522014.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Park YH, Lee SJ, Jung HA, Kim SM, Kim MJ,
Kil WH, Lee JE, Nam SJ, Ahn JS and Im YH: Prevalence and clinical
outcomes of young breast cancer (YBC) patients according to
intrinsic breast cancer subtypes: Single institutional experience
in Korea. Breast. 24:213–217. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Merino D, Lok SW, Visvader JE and Lindeman
GJ: Targeting BCL-2 to enhance vulnerability to therapy in estrogen
receptor-positive breast cancer. Oncogene. 35:1877–1887. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Dawson SJ, Makretsov N, Blows FM, Driver
KE, Provenzano E, Le Quesne J, Baglietto L, Severi G, Giles GG,
McLean CA, et al: BCL2 in breast cancer: A favourable prognostic
marker across molecular subtypes and independent of adjuvant
therapy received. Br J Cancer. 103:668–675. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Choi JE, Kang SH, Lee SJ and Bae YK:
Prognostic significance of Bcl-2 expression in non-basal triple
negative breast cancer patients treated with anthracycline-based
chemotherapy. Tumour Biol. 35:12255–12263. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Bouchalova K, Kharaishvili G, Bouchal J,
Vrbkova J, Megova M and Hlobilkova A: Triple negative breast
cancer-BCL2 in prognosis and prediction. Review. Curr Drug Targets.
15:1166–1175. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Bouchalova K, Svoboda K, Kharaishvili G,
Vrbkova J, Bouchal J, Trojanec R, Koudelakova V, Radova L, Cwiertka
K, Hajduch M and Kolar Z: BCL2 is an independent predictor of
outcome in basal-like triple-negative breast cancers treated with
adjuvant anthracycline-based chemotherapy. Tumour Biol.
36:4243–4252. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Perillo B, Sasso A, Abbondanza C and
Palumbo G: 17beta-estradiol inhibits apoptosis in MMCF-7 cells,
including bcl-2 expression via two estrogen-responsive elements
present in the coding sequence. Mol Cell Biol. 20:2890–2901. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Certo M, Del Gaizo Moore V, Nishino M, Wei
G, Korsmeyer S, Armstrong SA and Letai A: Mitochondria primed by
death signals determine cellular addiction to antiapoptotic BCL-2
family members. Cancer Cell. 9:351–365. 2015. View Article : Google Scholar
|
|
52
|
Honma N, Horii R, Ito Y, Saji S, Younes M,
Iwase T and Akiyama F: Differences in clinical importance of Bcl-2
in breast cancer according to hormone receptor status or adjuvant
endocrine therapy. BMC Cancer. 15:6982015. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Seong MK, Lee JY, Byeon J, Sohn YJ, Seol
H, Lee JK, Kim EK, Kim HA and Noh WC: Bcl-2 is a highly significant
prognostic marker of hormone-receptor-positive, human epidermal
growth factor receptor-2-negative breast cancer. Breast Cancer Res
Treat. 150:141–148. 2015. View Article : Google Scholar : PubMed/NCBI
|