Introduction
Breast cancer has a high incidence of malignant
tumors in women and is currently on the increase, with the
occurrence age becoming increasingly less (1,2). Color
Doppler ultrasound and ultrasound elasticity imaging have an
important clinical value for the diagnosis of breast cancer
(3). However, clinical diagnosis is
difficult for some early stage breast cancers without abnormality
in the non-palpable mass ultrasound examination and with only
manifestations of cluster calcification, structure distortion,
asymmetric density or small nodular changes in mammography
(4).
Previous findings showed that 3D X-ray stereo wire
localization biopsy operation has high precision, with a diagnostic
accordance rate of 90.9%, and an accurate early breast cancer
diagnosis rate of up to 100% (5),
which is useful for clinicians in the selection of an effective
treatment method.
In the present study, a retrospective analysis of
the clinical data of 80 patients with non-palpable breast lesions
diagnosed using molybdenum target X-ray at the Xuzhou Hospital
Affiliated to Southeast University (Jiangsu, China) between June,
2011 and July, 2014, was performed with a comparative analysis of
one-time success rate of lesion resection by general positioning
operation biopsy and 3D stereo wire localization biopsy.
Materials and methods
Subjects
A total of 80 cases diagnosed according to the
preoperative positioning methods were divided into 40 cases of
rough positioning (group A) and 40 cases of 3D solid wire
localization (group B). The inclusion criteria for the study were:
clinical palpation without finding lesions of small sand-like
calcification, suspicious clustered calcifications, structure
distortion, asymmetric dense and suspicious nodules only in
molybdenum target X-ray photography; on the basis of the standard
classification (6) of breast imaging
reporting and data system, BI-RADS of USA Radiological Society, the
patients of class BI-RADS-4 and class BI-RADS-3 (required lesion
biopsy for their anxiety). The exclusion criteria for the study
were: indeterminate class BI-RADS-0 that needed further imaging
examination; class BI-RADS-1, 2 normal and benign lesions; part of
class BI-RADS-3 patients who agreed on 6-month follow-up review;
and class BI-RADS-5 diagnosed with breast cancer.
The molybdenum target X-ray film was read by two
experienced physicians for the diagnosis of breast imaging on the
special workstation. Lesions were classified on the basis of the
BI-RADS standard classification, and if there were differences of
opinion, case discussion was expanded in the department until the
classification results were consistent.
Patients characteristics
Patients in group A were 25–61 years (average age,
44±5 years). In the molybdenum target X-ray examination group,
there were 24 cases of sand-like calcification, 8 cases of small
suspicious distortion, 5 cases of clustered calcifications, and 3
cases of asymmetric structure of dense and suspicious nodules. The
patients in group B were 28–62 years (average age, 45±4 years). The
molybdenum target X-ray examination revealed 26 cases of sand-like
calcification, 7 cases of small suspicious distortion, 5 cases of
clustered calcifications, and 2 cases of asymmetric structure of
dense and suspicious nodules. There was no statistically
significant difference in the age (t=−0.348, P=0.367>0.05) and
results of molybdenum target X-ray examination (U=7.5,
P=0.885>0.05) between the patients of the two groups.
Instruments and equipment
Full digital breast X-ray machine and the supporting
3D stereotactic system (Hologic, Bedford, MA, USA), and double hook
wire localization needle (Budd Co., Philadelphia, PA, USA) were
used for imaging.
Methods
The patients underwent routine mammography axial,
lateral and standard mediolateral oblique radiography.
General positioning method
Each breast was regarded as a clock dial, and
according to the preoperative routine mammography axial and
standard lateral image, the location of the lesion in the quadrant
and the time range of the corresponding clock disc was assessed.
Adobe Photoshop CS version 10.0 (Adobe Systems, Inc., San Jose, CA,
USA) was used to measure the imaging distance from the nipple to
the papillary lesions, and the reports were filled operating
physicians for surgical biopsy.
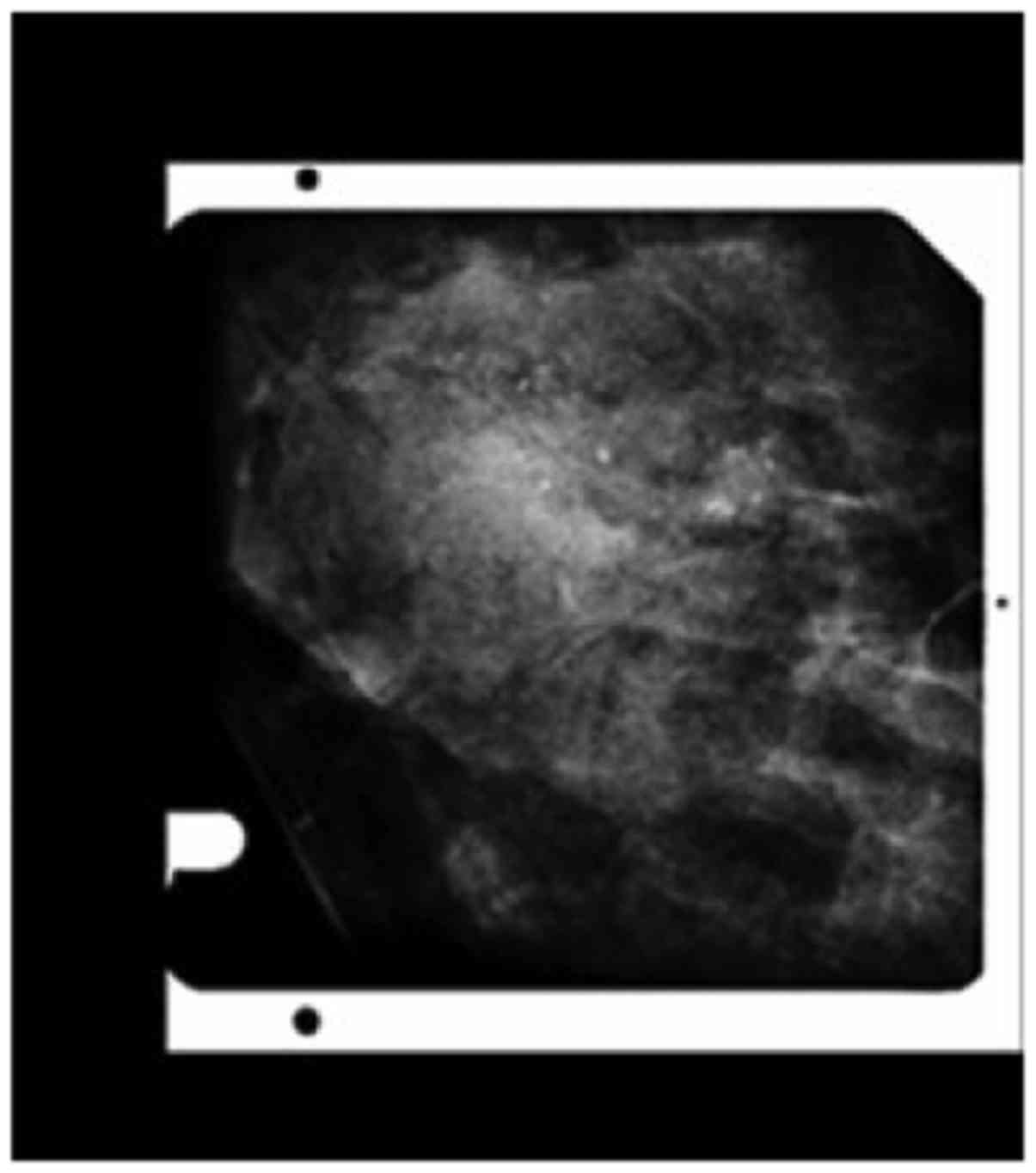
3D stereo wire localization
method
Patients were required to be seated. A puncture rack
was installed, and the lesion puncture was placed into the
placement box, radiography was assessed and the lesions in the
operational range were adjusted (Fig.
1), and fixed by oppression. The position of the needle tip was
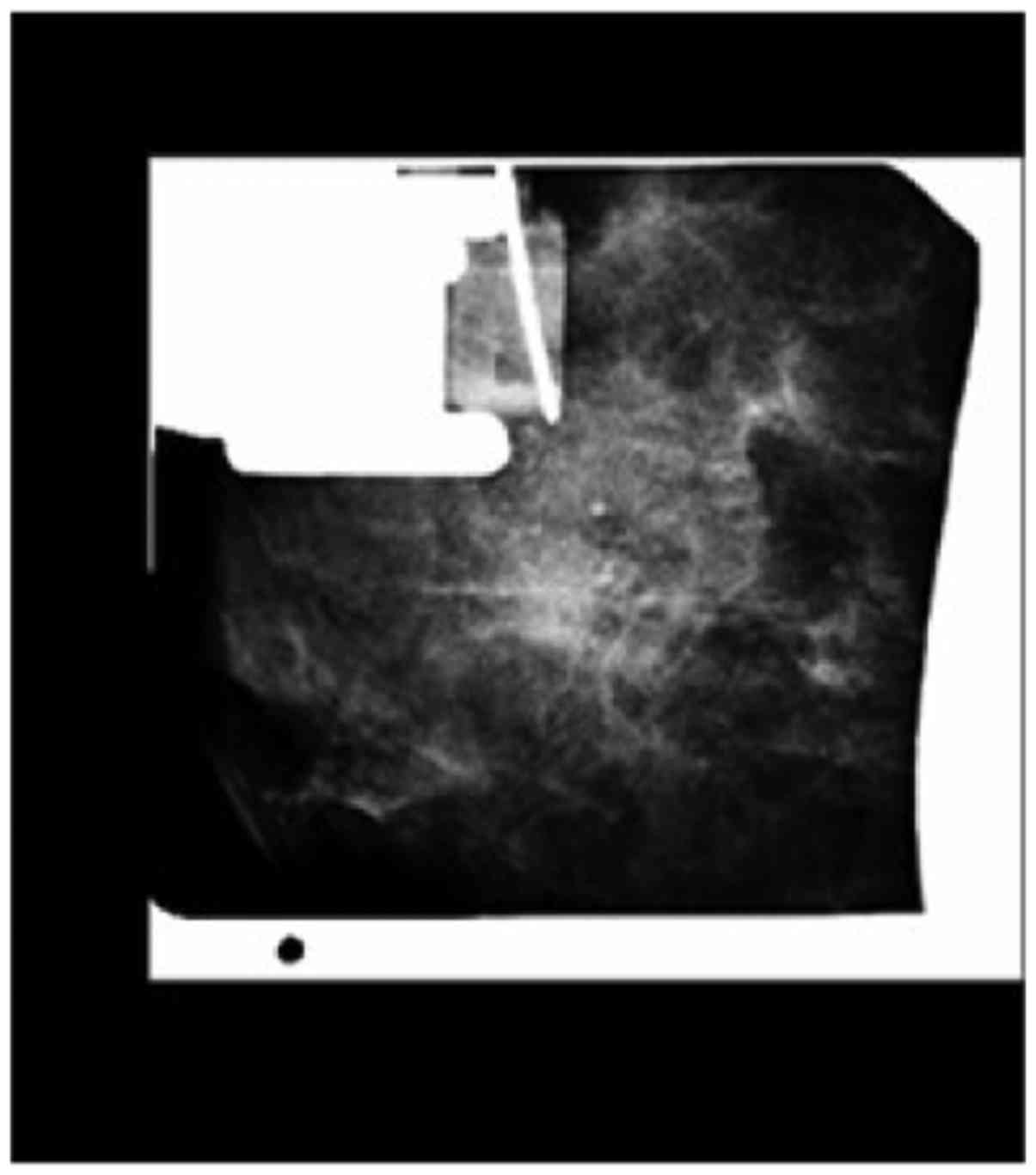
calibrated, and the coordinates were 0.- axis Z. Perturbation of
+15° and −15° film was determined in the digital spot mammography,
the target lesions display system was selected, and the puncture
point x, y and z axes were accurately calculated by computer to
determine the needle point and needle depth. Regular disinfection,
and local anesthesia, were used and the needle puncture was
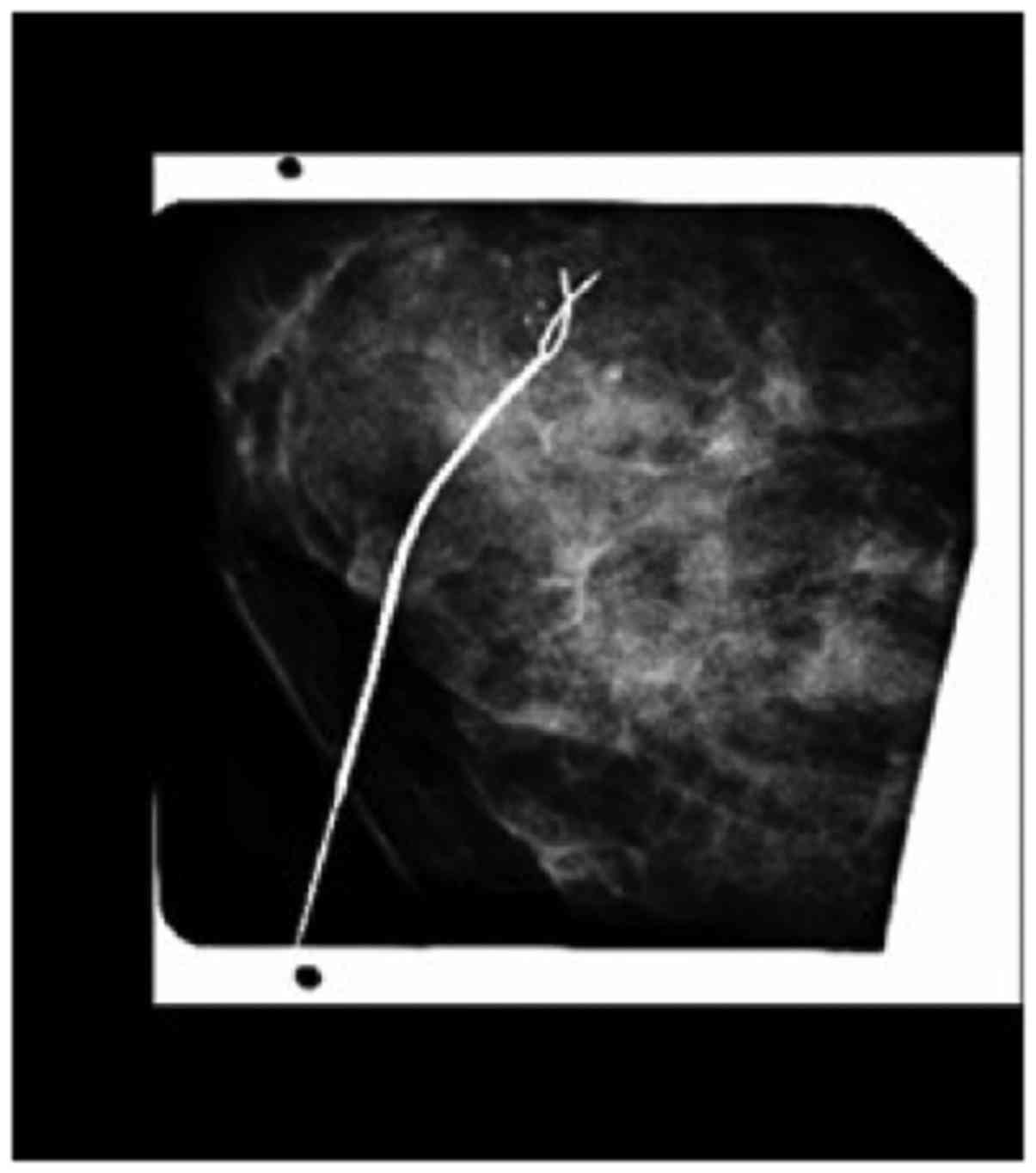
inserted, and radiography confirmed the correct position (Fig. 2). The needle sheath, and indwelling
double hook wire was pulled out (Fig.
3), and the body part of the guide wire was excised and fixed
by ligule tape winding.
Biopsy operation
At the general location of the lesion, the surgeons
made incisions according to the focus range provided by the
radiologists. The operation excision range was generally based on
the lesion size. For the lesions localized by 3D stereo wire, the
surgeons followed guided wire localization to excise the lesion
biopsy; with surgical resection being generally in the range of 20
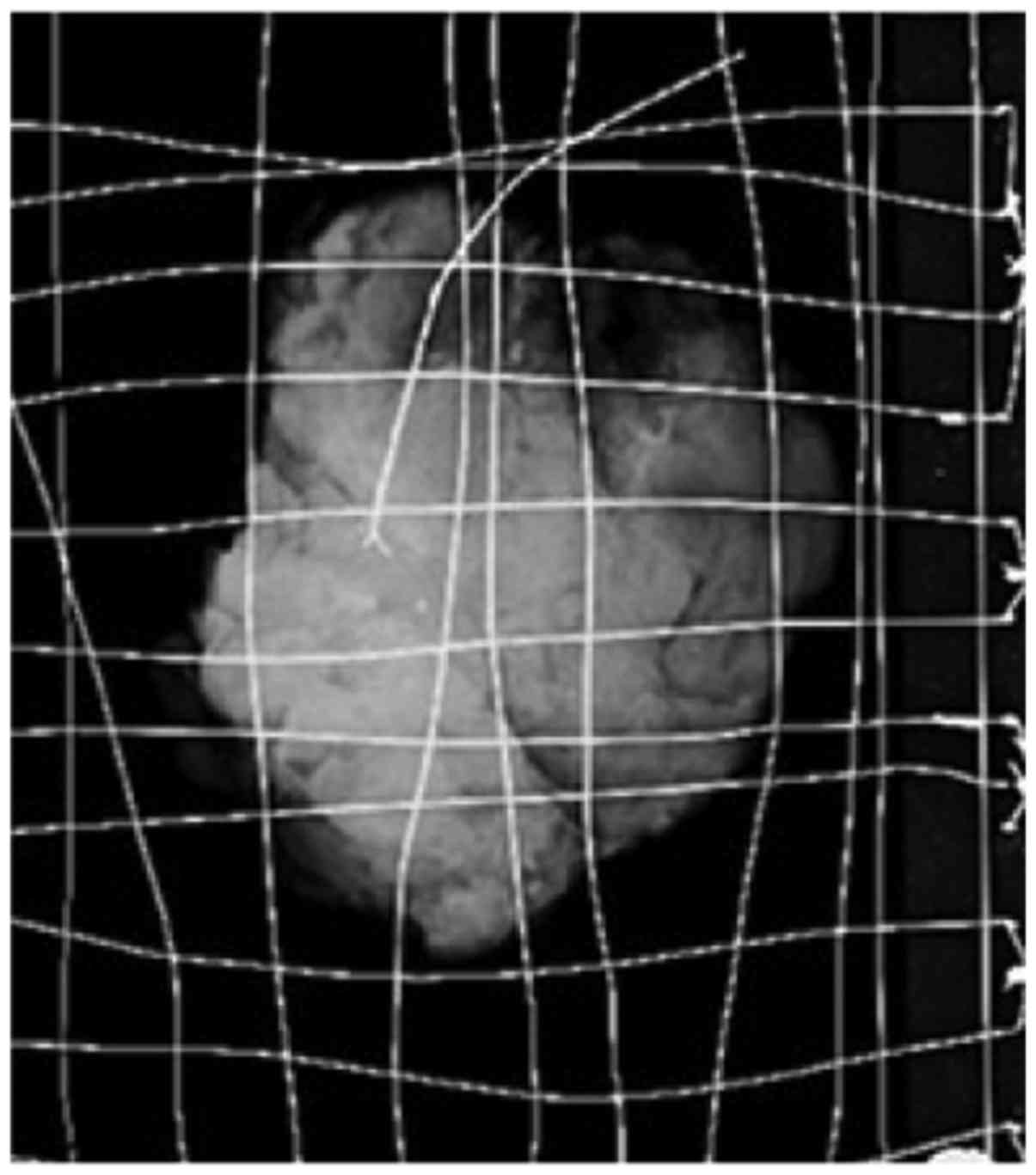
mm around the tip of localization wires. Two groups of cases were
marked long, short, and single, or double line of resection
specimens based on the direction and position in the operation
process, and then the specimen was sent to the radiology
radiograph. The radiologist compared specimen radiography and
preoperative axial and lateral radiographs, and observed the
resected specimen to determine whether lesions were completely
contained. If the lesion size, quantity, and scope were consistent
with previous X-ray film, it was considered as completely removed
(Fig. 4), and the needle head was
inserted into the pathological lesions. However, if the lesion was
not completely removed according to the position of marked lines,
the physician resected the remaining lesions, and the specimens
were sent to the Department of Pathology.
Statistical analysis
Data were analyzed using statistical software SPSS
16.0 (Chicago, IL, USA). The measurement data of approximate normal
distribution are presented as mean ± SD, and the groups were
compared by the independent sample Student's t-test. Measurement
data were obtained using the Mann-Whitney U test, χ2
test and non-parametric test. P<0.05 was considered as the
difference with statistical significance.
Results
Of the 40 cases of group A, 33 cases completed
one-time resection of lesions (82.5% success rate), of which, 5
cases were partially removed, 3 cases underwent a second total
resection, and 2 cases did not cut to the lesion, even after six
months of repositioning of resection. Of the 40 cases of group B,
38 cases completed one-time resection of lesions (95% success
rate), 2 patients had vagal reaction, and were required to rest for
a few minutes, prior to completing positioning with successful
resection.
As the moving range was extremely large prior to the
operation, the biopsy resulted in the guide wire moving, and the
radiologist resected the incomplete resection a second time in two
patients. These results showed that the success rate of one-time
complete lesion resection of group B was significantly higher than
that of group A (95 vs. 82.5%), and the difference was
statistically significant (χ2=3.638, P<0.05).
Discussion
The performance of specific imaging of non-palpable
breast lesions is poor with difficulties for the differentiation of
benign, and malignant lesions (7).
Prior to the introduction of the 3D stereotactic localization
system for the non-palpable lesions that were only displayed using
mammography, the traditional general clinical positioning methods
were used to provide the location of the lesion to surgeons.
General location requirements for the technical level of
radiologists and surgeons are higher, and the positioning range as
well as the operation excision range are larger. At the same time,
because the position in the operation is different from the one in
the film with the breast oppression image, accurate resection of
the lesion becomes difficult due to a deviation in the location of
the lesion during surgery.
At present, some hospitals use molybdenum target 2D
guide wire localization technique, known as 2D wire localization.
It can just provide × and y axes of the target lesions, but the
determination of z axis, the value of the depth of the needle
requires the experience of radiologists, and is bound to cause a
distance error between the tip and target lesion to expand the
scope of operation (8). Although the
2D wire localization technique is relatively more accurate than
that of general positioning, the depth of the needle is easily
influenced by subjective factors, and is less accurate than 3D
stereo positioning. Evidence has shown that, the accuracy of 2D
guided wire localization and the comfort it brings to the patients
is lower than that of 3D stereo wire localization (8).
The 3D stereotactic localization system has been
developed based on 2D wire localization, but adds another
dimension. Additionally, through the computer the exact 3D
coordinates of target lesions can be calculated for more accurate
positioning. It can also determine the resection range of lesions
as well as smaller resection range, once the guide wire is placed
by the surgeon and there is less damage to the normal breast
tissue. The 3D stereo wire localization technique guided by the
molybdenum target may identify an earlier palpation-negative lesion
that can only be found in the X-ray examination through guide wire
orientation to direct clinicians during excision and the
pathological examination. This is important in the precise excision
of the lesion, which can further improve the earlier diagnostic
rate of breast cancer and the accurate rate of resection (9).
To determine the shortest distance from the lesion
to the surface is particularly important to minimize the damage to
the mammary gland during surgery. Finding the shortest path can
reduce normal glandular tissue of the guide wire and resected
tissue during surgery. To achieve this, we improved the manner in
which the axial needle was inserted in different positions selected
for different puncture directions, taking the comfort of patients
into consideration. An axial needle was used for the lesions
generally located in the inner and outer quadrant; for the lesion
located in the lateral or medial quadrant, with the puncture rack
being rotated to the position of 90°; whereas for lesions under the
internal or external quadrant, the puncture rack was generally
rotated to 45° or 60°.
As the precision requirements of 3D stereo wire
localization technique are higher, authors suggest that in the
course of the operation the following points remain to be
clarified: i) after fixing the lesions, patients should remain
stationary during operation; ii) because the patients are seated
and see the surgical procedure, a few patients may have vagal
reaction, and the clinical manifestations thereof are dizziness,
pale, rapid heartbeat, sweating and weakness in the limbs (9). At that time, patients should be allowed
to relax or rest in supine position for a few minutes. Most of the
patients recovered by themselves to complete the positioning
operation; severe clinical manifestations were alleviated after
injection of atropine and patients continued until completion of
the positioning operation, or returned on another day. To avoid the
vagal reaction of patients before and during surgery because of
nervousness, communication should be constant with the patient in
order to relieve the tension; iii) since breast compression is
needed for the guide wire localization, it is not appropriate to
use this for patients with extremely small and thin breasts; iv) it
is not appropriate to use wire localization for the patients whose
lesion location is extremely high and close to the chest wall, and
by adjusting the gantry angle whose lesion cannot be placed in the
positioning frame; and v) although the guide wire localization
technique operation is simple and safe, there is a possibility of
hematoma around the location points. Guide wire localization
technique should also not be used for patients with coagulation
dysfunction.
In conclusion, the 3D stereo wire localization
technique guided by the full digital breast X-ray machine has an
important diagnostic value for the palpation-negative breast
lesions, as it can be useful for earlier identification, diagnosis
and treatment of breast lesions, and through various technical
improvements, positioning may provide a more accurate image with
smaller operation excision scope (10). This meets the demand for esthetic
beauty and quality of life of women and is worthy of clinical
application and promotion. As the study time was short and a small
sample size was included in the present study, there are certain
limitations to the use of the wire localization technique for the
cases whose images had structural distortion and were
asymmetrically dense. Future studies may identify more useful ways
of conducting biopsy for the abovementioned cases.
References
|
1
|
Ly M, Antoine M, Dembélé AK, Levy P,
Rodenas A, Touré BA, Badiaga Y, Dembélé BK, Bagayogo DC, Diallo YL,
et al: High incidence of triple-negative tumors in sub-saharan
Africa: a prospective study of breast cancer characteristics and
risk factors in Malian women seen in a Bamako university hospital.
Oncology. 83:257–263. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mao Z, Zhu Z, Wang H, Han W and Zhao Y:
Modified radical mastectomy with Auchincloss method for 65 cases of
breast cancer. Chin J Anat Clin. 19:313–315. 2014.(In Chinese).
|
|
3
|
Yin R, Yan S and Ling X: Diagnostic value
of color Doppler ultrasound and X-ray mammography in the early
breast cancer. Chin J Anat Clin. 19:299–302. 2014.(In Chinese).
|
|
4
|
Zhang H, Liang F, Jia Z, Jiao J, Peng Y
and Yu Z: Diagnosis and therapy of palpation negative breast
lesion. China J Mod Med. 18:3517–3519. 2008.(In Chinese).
|
|
5
|
Chadwick DR and Shorthouse AJ:
Wire-directed localization biopsy of the breast: an audit of
results and analysis of factors influencing therapeutic value in
the treatment of breast cancer. Eur J Surg Oncol. 23:128–133. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cardeñosa G: Breast Imaging Companion.
3rd. Lippincott Williams & Wilkins; Philadelphia, PA: pp.
465–467. 2008
|
|
7
|
Feng RD, Lu J, Li R, Deng Z and Gao K:
Preoperative wire guided localization under X-ray guidance for
nonpalpable breast lesions. Chin J Med Imaging. 21:341–343.
2013.(In Chinese).
|
|
8
|
Zhao H, Yin C and Zhao A: Comparison of
two-dimensional and three-dimensional X-ray guided wire
localization breast biopsy. Zhongguo Jieru Yingxiang Yu Zhiliaoxue.
8:307–309. 2011.(In Chinese).
|
|
9
|
Fu Y, Ji Z, Ding W, Ye F and Lou C:
Thermoacoustic imaging over large field of view for
three-dimensional breast tumor localization: a phantom study. Med
Phys. 41:1107012014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang G, Zhang J, Hao X, Chang Y, Zhang S,
Yang S and Wei P: Application of 3D X-ray guided wire localization
of non-palpable lesion with microcalcification in breast. J Pract
Radiol. 29:752–754. 2013.(In Chinese).
|