Introduction
At present, uterine cervical cancer is a common
malignant neoplasm in females (1),
and 40% of cervical cancer patients are diagnosed during
reproductive age. Therefore, invasive surgeries to remove cervical
cancer should be avoided in suitable cases to preserve childbearing
abilities (2).
While the Pap smear is the standard cervical cancer
screening method, the overall sensitivity (65%) of the Pap smear is
not satisfactory (3). Abnormal
results from a Pap-screening test are followed by a colposcopy for
histological confirmation. However, colposcopy also fails to detect
30–50% of prevalent high-grade squamous intraepithelial lesions
(4). While the current colposcopic
classification system intends to improve the performance of
colposcopy, accurate diagnostic yield is still <55%, even for
cervical cancer (5).
Narrow band imaging with magnifying endoscopy
(NBI-ME), which is useful for the assessment of micro-vessels, has
demonstrated outstanding ability for the detection of early
gastrointestinal (GI) epithelial neoplasia (6–12).
Magnifying endoscopy enables the capture of images ≤80-fold
compared with conventional endoscopy. The NBI system is an advanced
optical system, which enhances the visualization of micro-vascular
architecture and micro-surface structures using narrower bands of
blue and green filters compared with conventional white light
imaging (13). Therefore, ME-NBI, a
combination of magnification endoscopy and NBI, may improve the
detection and diagnosis of GI neoplasia with specific
micro-vascular and surface abnormalities. The associations between
ME-NBI appearance and pathology of non-neoplastic and neoplastic
lesions have been demonstrated with strong clinical evidence. A
number of diagnostic classification systems for GI neoplasia have
been established by clarifying these characteristic ME-NBI findings
(6,7,12).
Notably, the ME-NBI findings of irregular micro-vascular pattern
with a demarcation line and/or irregular micro-surface pattern with
a demarcation line have been proposed to be essential for accurate
diagnosis of early gastric cancer (7). Therefore, ME-NBI may have important
roles in the diagnosis of distinguishing between GI cancerous and
noncancerous lesions.
Therefore, the ability of NBI-ME to diagnose uterine
cervical lesions was determined by performing a collaborative study
with GI endoscopists and gynecologists.
Patients and methods
Patients and methods
Flexible NBI-ME was performed in patients with
squamous cell cervical lesions that required further examinations
based on their Pap smear results (cytology ≥ low-grade squamous
intraepithelial lesion) at Kagawa University Hospital (Miki,
Japan). Patients with cervical adenocarcinoma were excluded. A
total of 10 patients with a mean age of 39 years (range, 29–65
years) who underwent NBI-ME between April 2014 and April 2015 were
enrolled in the present study. A magnifying endoscope (GIF-H260Z;
Olympus Corporation, Tokyo, Japan) with an NBI system (EVIS EXERA
II; Olympus Corporation) was used during all procedures. Two
experienced endoscopists performed endoscopic examinations of the
cervix with one senior gynecologist. The present study was approved
by the Ethics Committee of Kagawa University Hospital and was
registered under the UMIN no. 000014933. Written informed consent
was obtained from all patients.
Endoscopic procedure
Transvaginal endoscopic examination was performed by
an endoscopist at the endoscopy unit (Kagawa University Hospital)
and a gynecologist, who assisted using a Cusco speculum to obtain
cervical visibility. The entire circumference of the cervix was
observed under white light imaging, and NBI-ME was continuously
utilized. The observation procedure was performed at long, middle,
and short distances (max 80 power zoom; similar to endoscopic
examination of the GI tract). The NBI-ME findings were recorded to
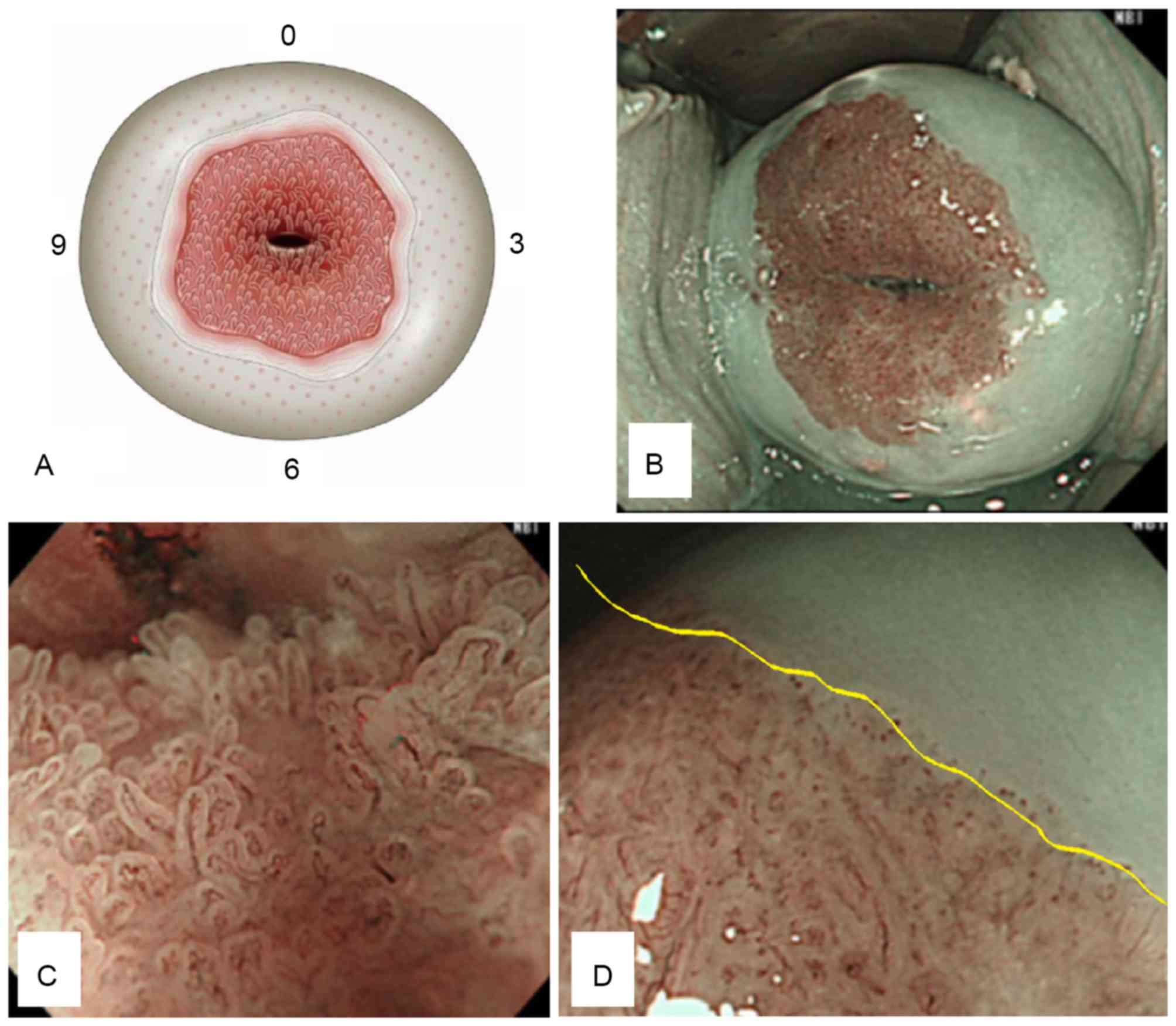
develop a schema of the cervix (Fig.
1A). A normal uterine cervix was characterized by an internal
ostium of the uterus with columnar, transitional and squamous
epithelium in order from the inside. Intrapapillary protruded loop
vessels, which appeared in the area of transitional and squamous
epithelium were defined as dot vessels. A representative normal
uterine cervix is presented in Fig.
1B-D.
A gynecologist then performed a routine colposcopy
and obtained punch biopsies at the abnormal site (according to the
NBI-ME examinations). An abnormal appearance during a colposcopy is
defined as mucosal thickness with whitish or abnormal vessels
(mosaic or punctuated patterns). Histological results were
confirmed with punch biopsies obtained during colposcopy or
conization and extended hysterectomies. Biopsy tissues were fixed
in 10% neutral-buffered formalin and were further processed into
paraffin-embedded blocks. Sections (3 µm) were cut from each
paraffin block. Pathology was assessed by three experienced
pathologists using a light microscope (Eclipse 55i; Nikon
Corporation, Tokyo, Japan) based on hematoxylin and eosin
staining.
Outcome measures
NBI-ME findings concordant with the punch biopsy
sites were compared with the histological results. A retrospective
review of the NBI-ME images identified the following abnormal
NBI-ME findings regarding micro-vascular patterns: i) presence of
dot vessels, where a dot was defined as a dilatation of an
intrapapillary protruded loop vessel; ii) irregular arrangement of
dots; iii) high density of dots; iv) caliber change of the
micro-vasculature; and v) new tumor vessels, defined as a dilated
vessel two times larger than the perivascular vessels. All images
were categorized as having abnormal features by the consensus of
two experienced endoscopists.
Results
A total of 10 patients underwent endoscopic
examinations using NBI-ME for the detection of cervical
abnormalities. The final diagnoses (based on histology) were as
follows: Negative for intraepithelial lesion or malignancy (NILM;
n=1), CIN1 (n=2), CIN2 (n=2), CIN3 (n=1), CIS (n=2), microinvasive
cancer (MIC; n=1), and invasive cancer (IC; n=1; Table I). The detection rate of abnormal
cervical lesions was 90% (9/10), excluding one normal case.
 | Table I.Clinicopathological data of 10
patients who underwent endoscopic examinations using flexible
NBI-ME. |
Table I.
Clinicopathological data of 10
patients who underwent endoscopic examinations using flexible
NBI-ME.
| No. | Age (years) | Pre-examination
details | NBI findings
(microvascular) | Location of
lesion | Colposcopic
findings | Diagnostic
method | Circumference: Final
diagnosis |
|---|
| 1 | 33 | Pregnant, following
chemotherapy for SCC | Irregular arrangement
High density Caliber change New tumor vessels | 9′-11′ | W2 | Extended
hysterectomy | 9′-11′ SCC |
| 2 | 54 | During CIN1
follow-up | Presence of dot-like
vessels Regular arrangement | 11′ | W1 | Punch biopsy by
colposcopy | 11′ CIN1 |
| 3 | 31 | Pregnant, during CIN1
follow-up | Presence of dot-like
vessels Regular arrangement | 6′ | W1 | Punch biopsy by
colposcopy | 6′ CIN1 |
| 4 | 33 | During CIN1-2
follow-up | Presence of dot-like
vessels Regular arrangement | 7′ | 12′,7′ W1 | Punch biopsy by
colposcopy | 7′ CIN1 12′ CIN2 |
| 5 | 29 | During CIN1-3
follow-up | Presence of dot-like
vessels Regular arrangement | 6′ | 5′,6′ W1 | Punch biopsy by
colposcopy | 5′,6′ CIN2 |
| 6 | 65 | Introduction with
MIC | Presence of dot-like
vessels Irregular arrangement High density | 12′-4′, 6′-8′ | W1-2 | Conization | 2′-11′CIN3-CIS |
| 7 | 35 | During ASC-US
follow-up | There are no dot-like
vessels | 11′-3′ | W1 | Punch biopsy by
colposcopy | Normal finding |
| 8 | 33 | Pregnant, during
ASC-H follow-up | Irregular arrangement
High density Caliber change | 12′, 2′-5′ | M2 | Conization | 7′ CIN3 2–5′ MIC |
| 9 | 30 | Introduction with
CIN3 | Presence of dot-like
vessels Irregular arrangement High density | 1′,8′-12′ | 9′ W2 | Conization | 5′-12′ CIN1 1′-4′
CIN3 |
| 10 | 55 | During CIN1
observation | Presence of dot-like
vessels Irregular arrangement High density | 5′ | 5′,6′ W2 | Conization | 5′ CIS |
Microvascular features of the uterine cervix were
evaluated by NBI-ME. The vascular patterns of the cervical tumors
at each stage were different. Dot like vessels were observed in 7
patients with cervical disease: CIN1 (n=2), CIN2 (n=2), CIN3 (n=1),
and CIS (n=2). Irregular arrangements were observed in 5 patients:
CIN3 (n=1), CIS (n=2), MIC (n=1), and IC (n=1). Tumor stage was
similar in patients with high density dots compared with patients
with irregular arrangements. Caliber changes were observed in 2
cases: MIC (n=1) and IC (n=1). New tumor vessels were observed in
one case: IC (n=1). No adverse events resulted from the NBI-ME
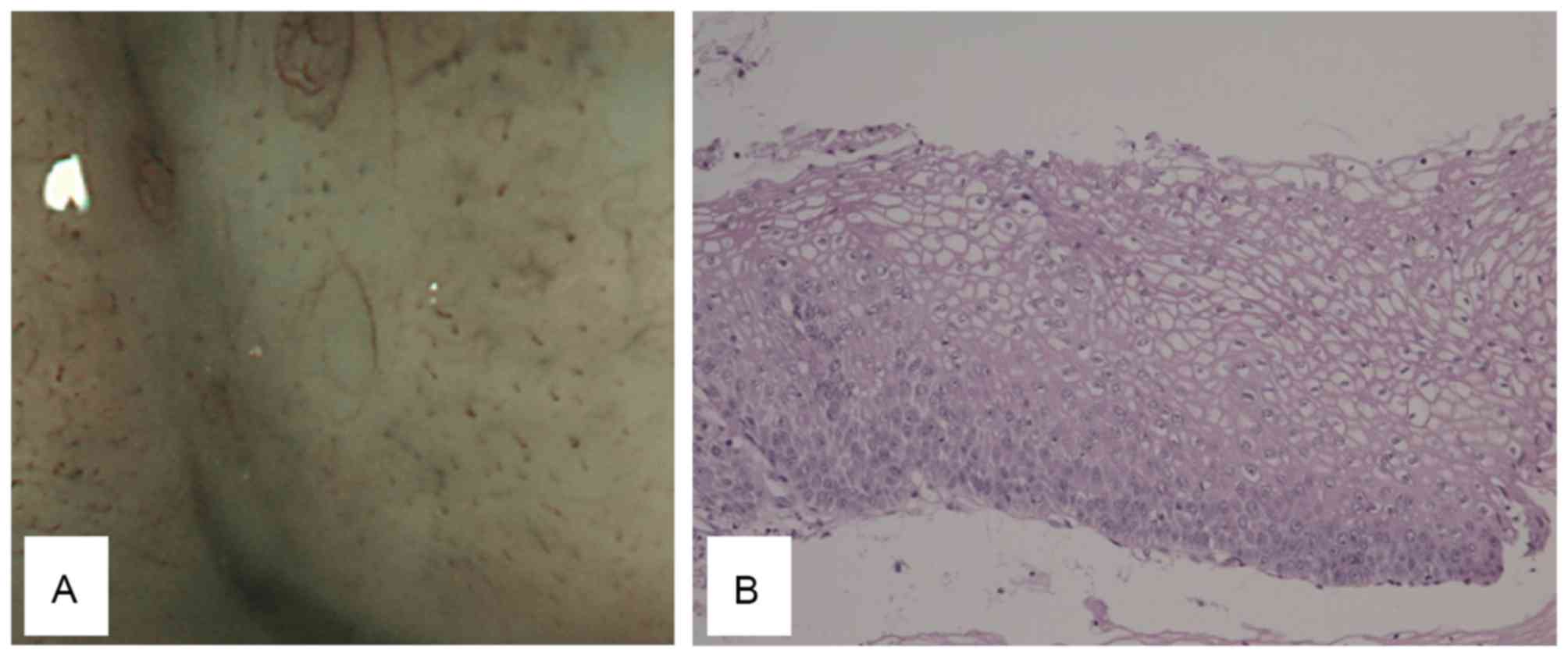
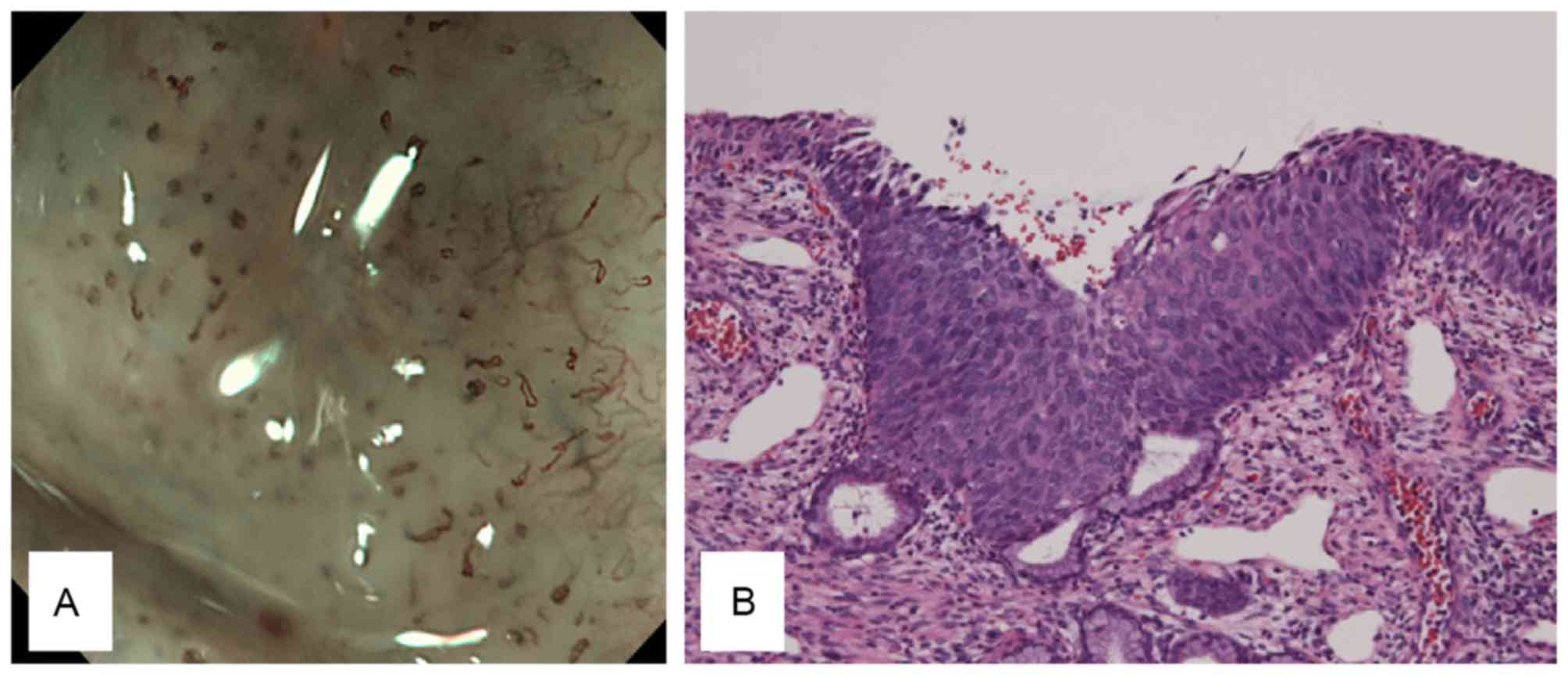
observations. The NBI-ME findings from patients with CIN1, CIN2,
CIN3, CIS, MIC, and IC are summarized in Table II. CIN1 was defined as a slight
increase in the number of dots compared with normal tissues
(Fig. 2). CIN2 was defined as a mild
increase in the number of dots compared with normal tissues
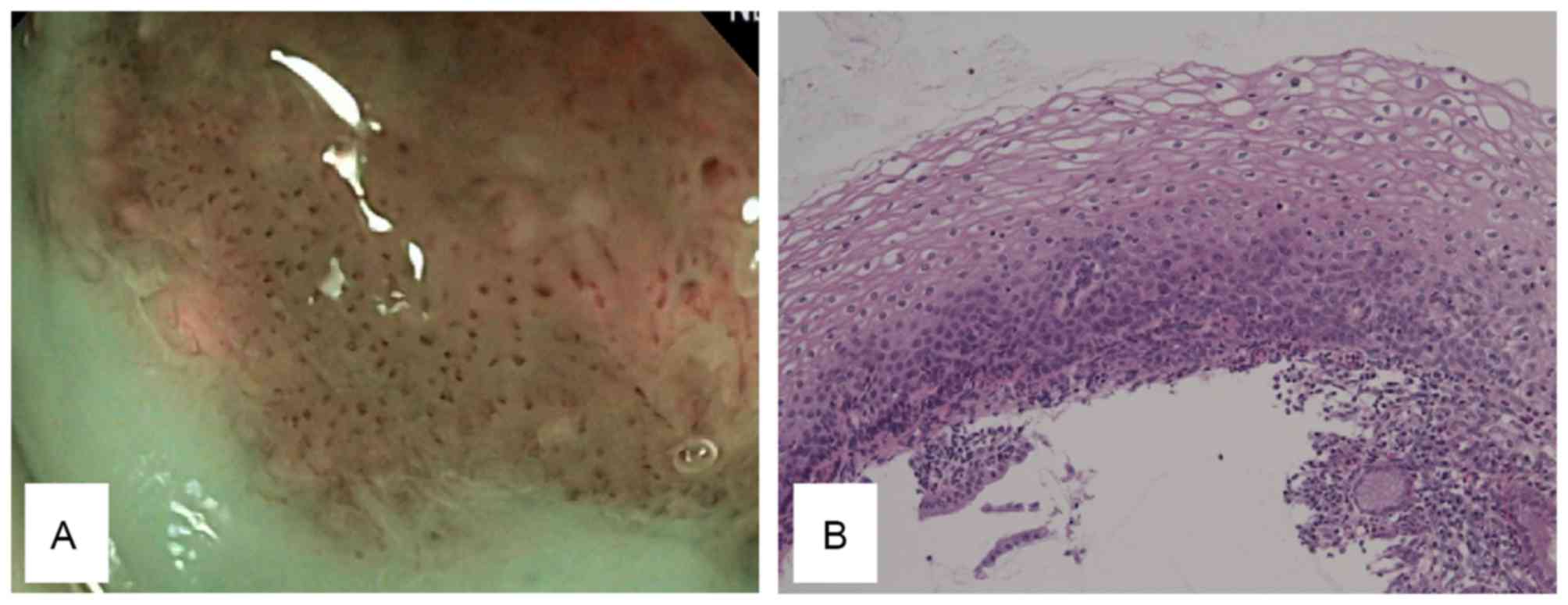
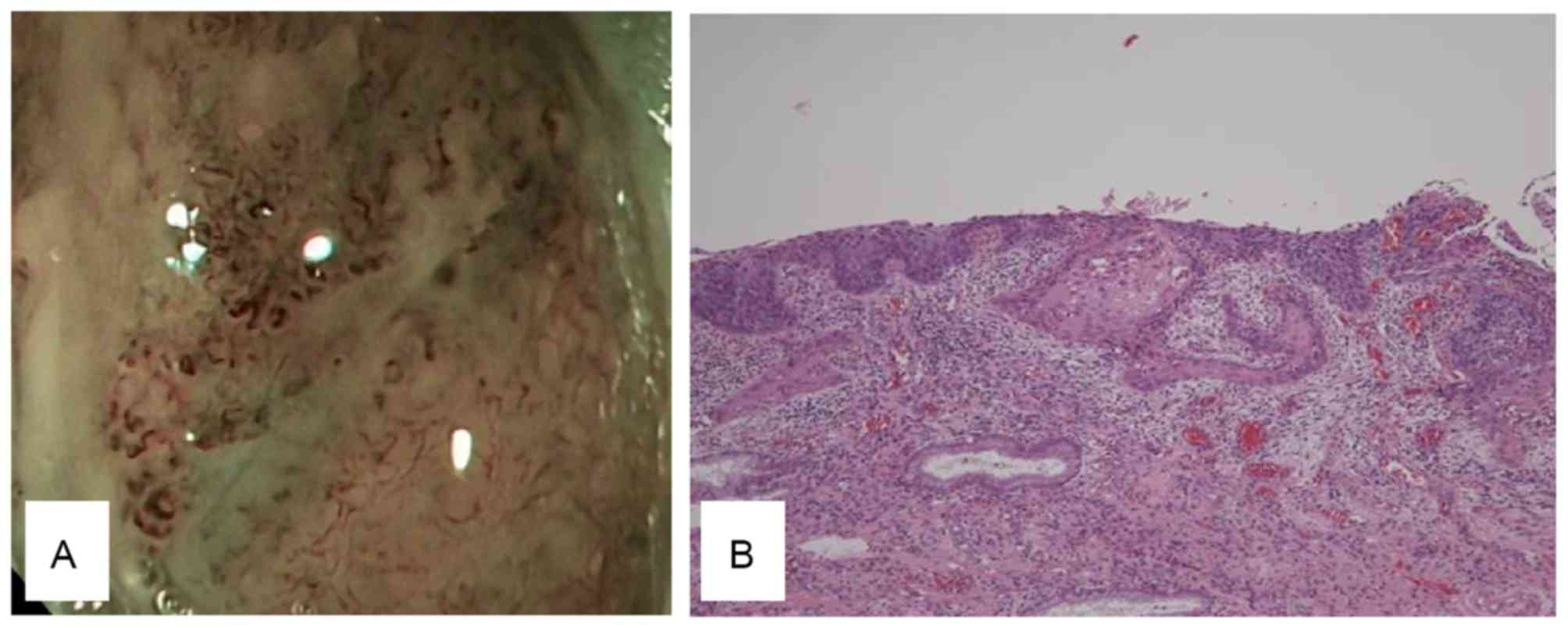
(Fig. 3). CIN3 was defined as the
elongation of dots with slightly irregular arrangements and a large
increase in the number of dots compared with normal tissues
(Fig. 4). CIS was defined as the
elongation of dots with severely irregular arrangements and a large
increase in the number of dots compared with normal tissues
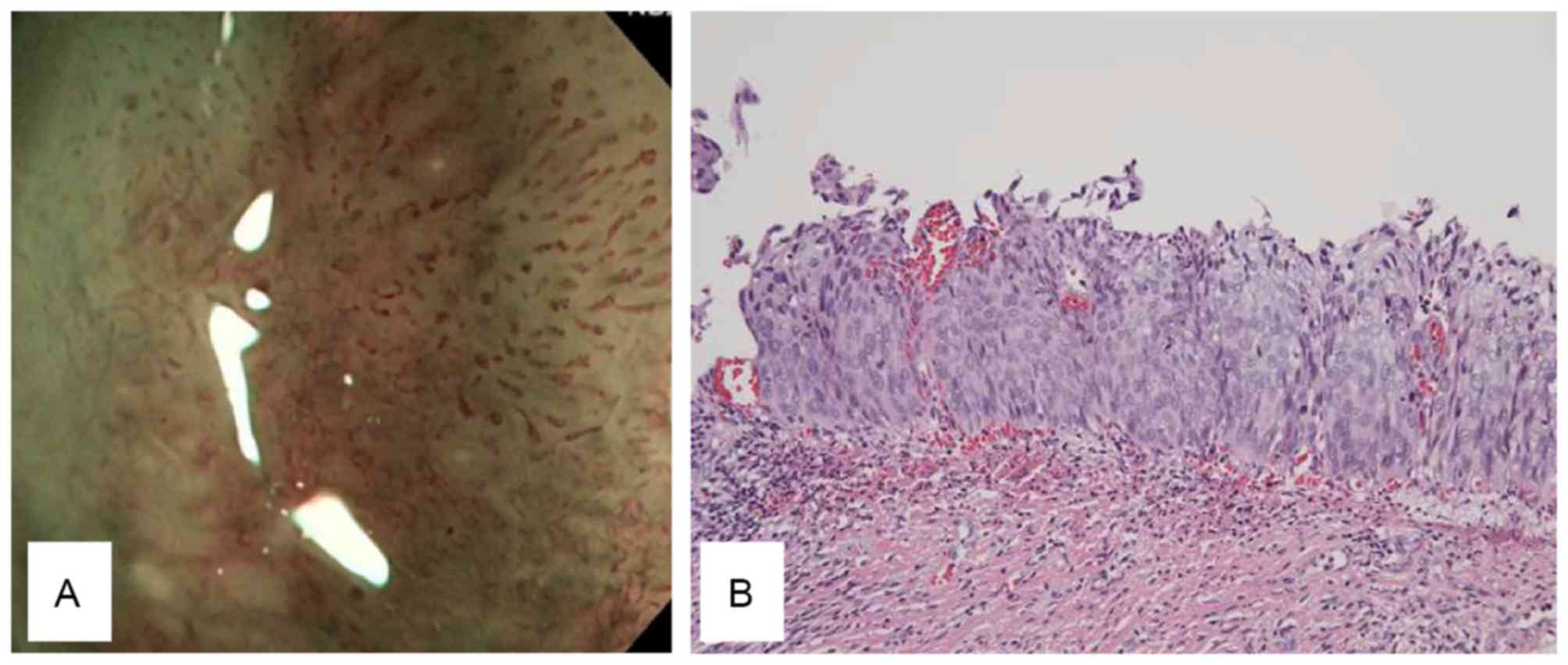
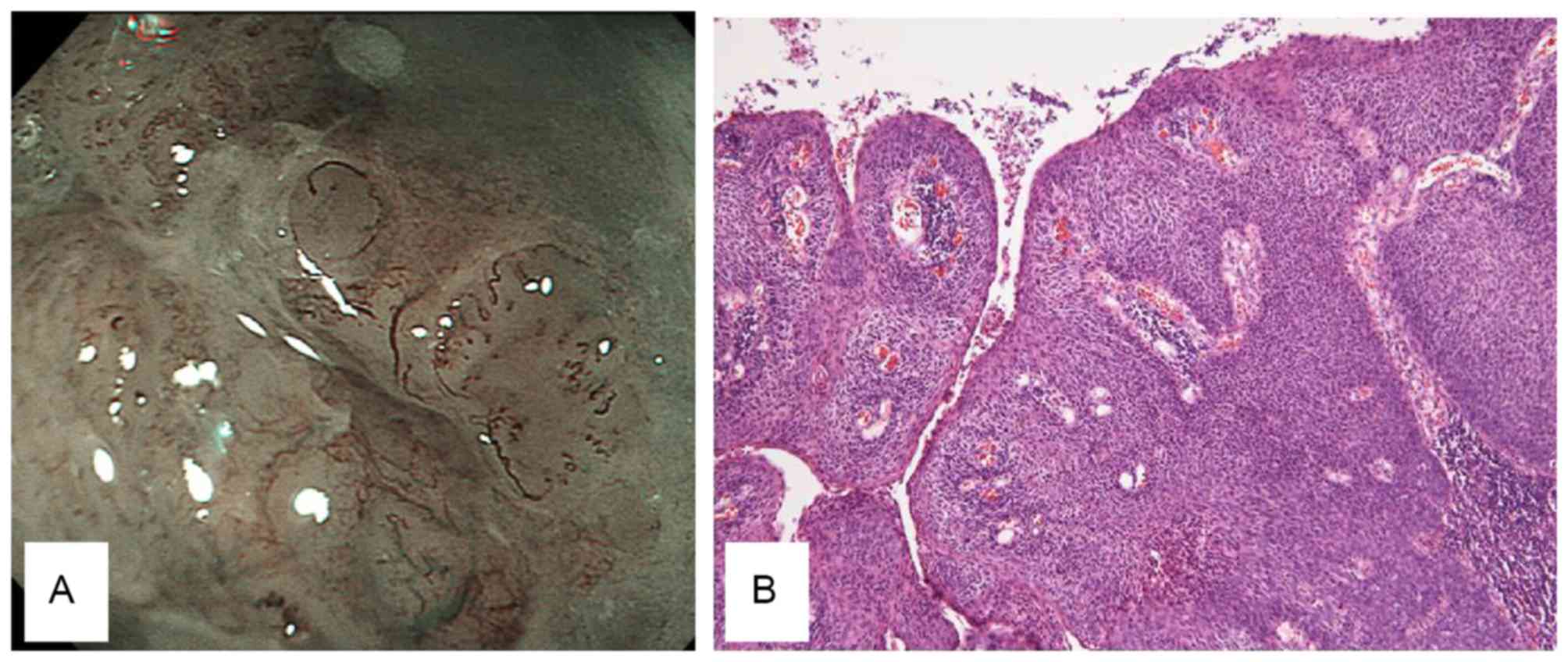
(Fig. 5). MIC was defined as the
presence of crawling vessels with irregular arrangements, high
densities and caliber changes (Fig.
6). IC was defined as the presence of irregular, high density
willow branch vessels and new tumor vessels (Fig. 7). Histological findings of the
different stages were demonstrated in Figs. 2–7,
respectively (hematoxylin and eosin staining; magnification, ×20).
A novel classification system (Table
III) was proposed based on the data from the present study.
 | Table II.Microvascular findings via NBI-ME in
10 patients. |
Table II.
Microvascular findings via NBI-ME in
10 patients.
| Parameters | Normal | CIN1 | CIN2 | CIN3 | CIS | MIC | IC |
|---|
| Total number of
patients | 1 | 2 | 2 | 1 | 2 | 1 | 1 |
| Characteristics of
NBI-ME findings |
|
|
|
|
|
|
|
|
|
|
|
Presence of dots | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 |
|
Irregular arrangement of
dots | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 |
| High
density of dots | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 |
| Caliber
change of vessels | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| New
tumor vessels | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
 | Table III.Proposed microvascular classification
system via NBI-ME for uterine cervical neoplasms. |
Table III.
Proposed microvascular classification
system via NBI-ME for uterine cervical neoplasms.
| Classification | Normal | CIN1 | CIN2 | CIN3 | CIS | MIC | IC |
|---|
| Values |
|
|
|
|
|
|
|
|
Vascular change | No vascular
dilatation | Presence of
dots | Presence of
dots | Elongation of
dots | Elongation of
dots | Multi-caliber
vessel changes | New tumor vessels
(2x dilated vessels, like IPCL) |
| Arrangement | Regular | Regular | Regular | Irregular
(slight) | Irregular
(severe) | Irregular
(severe) | Irregular
(severe) |
| Density
Postscript | Regular | Slight | Mild | High | High | High Crawling
vessel | High Willow
branch |
Discussion
An NBI system has been proposed to be valuable for
the diagnosis of early GI neoplasm (6–12). The NBI
system is currently utilized in the gynecological field. It has
previously been demonstrated that colposcopy with the NBI system is
effective for the diagnosis of cervical adenocarcinoma (14) and that flexible hysteroscopy with NBI
may be useful for the diagnosis of malignant endometrial lesions
(15). However, it is difficult to
evaluate the microvascular pattern of tumors in detail, because the
NBI mode does not have a high magnification function. Inoue et
al (6) demonstrated that it is
possible to classify the micro-vascular pattern of intrapapillary
capillary loops in squamous esophageal neoplasms by NBI-ME.
Furthermore, Yao et al (7,8) described
a micro-vascular and micro-surface classification system for
tubular epithelium that is useful for distinguishing early gastric
neoplasms from other lesions.
In accordance with these results, NBI-ME was
expected to be an excellent tool for the diagnosis of uterine
cervical neoplasms, similar to the diagnoses of epithelial
neoplasms of the GI tract. In the present study, NBI-ME was
demonstrated to reveal different characteristics of tumors of
different stages, as listed in Table
III. This is the first report of the potential diagnostic value
of NBI-ME for uterine cervical tumors.
GI endoscopists currently serve an important role in
other areas in addition to gastroenterology. The first-ever
application of endoscopic hemostatic forceps for active cervical
bleeding was previously reported by our group (16). This idea was based on the advances
made in endoscopic skills and devices. Endoscopic submucosal
dissection (ESD) for malignant epithelial tumors has been well
established in the field of gastroenterology. ESD facilitates
technical maneuvers under direct vision. Novel modalities,
including NBI-ME, and minimally invasive endoscopic treatments,
including ESD, may have multiple benefits compared with
conventional procedures. For example, NBI-ME is able to detect
early pharyngeal carcinomas (17),
and ESD endoscopists are able to perform curative resection of
pharyngeal epithelial carcinomas (18). The collaboration of
gastro-endoscopists and physicians in other fields is now an option
for overcoming conventional issues. Laparoscopic and endoscopic
cooperative surgery has been introduced clinically for local
resection of intraluminal type GI stromal tumors (19). Endoscopists are able to perform
endoscopic full-thickness resection (20) with an accurately set marginal line and
controlled bleeding. As one method of natural orifice transluminal
endoscopic surgery, gastro-endoscopists, surgeons, and
gynecologists act cooperatively when performing cholecystectomy via
the vagina (21).
Therefore, the introduction of NBI-ME for uterine
cervical lesions in patients treated collaboratively by GI
endoscopists and gynecologists is reasonable and represents a
novel, team approach. NBI-ME has certain advantages over
colposcopy. First, endoscopy (×80 magnification) has a higher
magnification power than colposcopy (×23.7 magnification). Second,
it is possible to accurately acquire the target lesion with biopsy
forceps, and spray acetic acid under direct vision through the
scope. Third, it is possible to observe the cervix by endoscopy in
a left lateral decubitus position instead of the lithotomy
position. However, the present study was a single-center,
preliminary study with a small sample size. In addition, the
limitation of the present study is that, in our experience, only
squamous cell lesions are involved except for columnar lesions. A
large prospective study is required to confirm the diagnostic value
of this novel method. A comparative prospective study with a large
number of cases is now being performed at Kagawa University
Hospital.
In conclusion, the present study demonstrated that
NBI-ME may be a valuable option for the diagnosis of uterine
cervical epithelial tumors, may result in the establishment of a
novel classification system, and may contribute to further
developments in the gynecologic field.
Glossary
Abbreviations
Abbreviations:
|
NBI-ME
|
narrow band imaging with magnification
endoscopy
|
|
GI
|
gastrointestinal
|
|
CIN
|
cervical intraepithelial neoplasia
|
|
CIS
|
carcinoma in situ
|
|
MIC
|
microinvasive cancer
|
|
IC
|
invasive cancer
|
|
ESD
|
endoscopic submucosal dissection
|
References
|
1
|
Arbyn M, Autier P and Ferlay J: Burden of
cervical cancer in the 27 member states of the European Union:
Estimates for 2004. Ann Oncol. 18:1423–1425. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Boutas I, Sofoudis C, Kalampokas E,
Anastasopoulos C, Kalampokas T and Salakos N: Fertility
preservation in women with early stage cervical cancer. Review of
the literature. Eur J Gyneacol Oncol. 35:373–377. 2014.
|
|
3
|
Coronado PJ and Fasero M: Correlating the
accuracy of colposcopy with practitioner experience when diagnosing
cervical pathology using the dynamic spectral imaging system.
Gynecol Obstet Invest. 78:224–229. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wentzensen N, Walker JL, Gold MA, Smith
KM, Zuna RE, Mathews C, Dunn ST, Zhang R, Moxley K, Bishop E, et
al: Multiple biopsies and detection of cervical cancer precursors
as colposcopy. J Clin Oncol. 33:83–89. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Duggan MA and Nation J: An audit of the
cervical cancer screening histories of 246 women with carcinoma. J
Low Genit Tract Dis. 16:263–270. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Inoue H, Kaga M, Ikeda H, Sato C, Sato H,
Minami H, Santi EG, Hayee B and Eleftheriadis N: Magnification
endoscopy in esophageal squamous cell carcinoma: A review of the
intrapapillary capillary loop classification. Ann Gastroenterol.
28:41–48. 2015.PubMed/NCBI
|
|
7
|
Yao K: How is the VS (vessel plus surface)
classification system applicable to magnifying narrow-band imaging
examinations of gastric neoplasias initially diagnosed as low-grade
adenomas? Gastric Cancer. 15:118–120. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yao K, Oishi T, Matsui T, Yao T and
Iwashita A: Novel magnified endoscopic findings of microvascular
architecture in intramucosal gastric cancer. Gastrointest Endosc.
56:279–284. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Goda K, Dobashi A and Tajiri H:
Perspectives on narrow-band imaging endoscopy for superficial
squamous neoplasms of the orohypopharynx and esophagus. Dig Endosc.
26 Suppl 1:1–11. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yamada S, Doyama H, Yao K, Uedo N, Ezoe Y,
Oda I, Kaneko K, Kawahara Y, Yokoi C, Sugiura Y, et al: An
efficient diagnostic strategy for small, depressed early gastric
cancer with magnifying narrow-band imaging: A post-hoc analysis of
a prospective randomized controlled trial. Gastrointest Endosc.
79:55–63. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ezoe Y, Muto M, Uedo N, Doyama H, Yao K,
Oda I, Kaneko K, Kawahara Y, Yokoi C, Sugiura Y, et al: Magnifying
narrowband imaging is more accurate than conventional white-light
imaging in diagnosis of gastric mucosal cancer. Gastoroentelrology.
141:2017–2025.e3. 2011. View Article : Google Scholar
|
|
12
|
Tanaka S and Sano Y: Aim to unify the
narrow band imaging (NBI) magnifying classification for colorectal
tumors: Current status in Japan from a summary of the consensus
symposium in the 79th annual meeting of the Japan
gastroenterological endoscopy society. Dig Endosc. 23 Suppl
1:131–139. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gono K, Obi T, Yamaguchi M, Ohyama N,
Machida H, Sano Y, Yoshida S, Hamamoto Y and Endo T: Appearance of
enhanced tissue features in narrow-band endoscopic imaging. J
Biomed Opt. 9:568–577. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fujii T, Nakamura M, Kameyama K, Saito M,
Nishio H, Ohno A, Hirao N, Iwata T, Tsukazaki K and Aoki D: Digital
colposcopy for the diagnosis of cervical adenocarcinoma using a
narrow band imaging system. Int J Gynecol Cancer. 20:605–610. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kisu J, Banno K, Kobayashi Y, Ono A,
Masuda K, Ueki A, Nomura H, Hirasawa A, Abe T, Kouyama K, et al:
Flexible hysteroscopy with narrow band imaging (NBI) for endoscopic
diagnosis of malignant endometrial lesions. Int J Oncol.
38:613–618. 2011.PubMed/NCBI
|
|
16
|
Kobara H, Mori H, Rafiq K, Fujihara S,
Nishiyama N, Morishita A, Goda Y, Kanenishi K, Hata T and Masaki T:
Application of endoscopic hemostatic forceps for uterine cervical
bleeding. Gastrointest Endosc. 81:234–235. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nakanishi H, Doyama H, Takemura K, Yoshida
N, Tsuji K, Takeda Y, Asahina Y, Kito Y, Ito R, Hayashi T, et al:
Detection of pharyngeal cancer in the overall population undergoing
upper GI endoscopy by using narrow-band imaging: A single-center
experience, 2009–2012. Gastrointest Endosc. 79:558–564. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Okada K, Tsuchida T, Ishiyama A, Taniguchi
T, Suzuki S, Horiuchi Y, Matsuo Y, Yoshizawa N, Suganuma T, Omae M,
et al: Endoscopic mucosal resection and endoscopic submucosal
dissection for en bloc resection of superficial pharyngeal
carcinomas. Endoscopy. 44:556–564. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hiki N, Nunobe S, Matsuda T, Hirasawa T,
Yamamoto Y and Yamaguchi T: Laparoscopic endoscopic cooperative
surgery. Dig Endosc. 27:197–204. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mori H, Kobara H, Fujihara S, Nishiyama N,
Ayagi M, Matsunaga T, Yachida T and Masaki T: Establishment of the
hybrid endoscopic full-thickness resection of gastric
gastrointestinal stromal tumors. Mol Clin Oncol. 3:18–22.
2015.PubMed/NCBI
|
|
21
|
Federlein M, Borchert D, Müller V, Atas Y,
Fritze F, Burghardt J, Elling D and Gellert K: Transvaginal
video-assisted cholecystectomy in clinical practice. Surg Endosc.
24:2444–2452. 2010. View Article : Google Scholar : PubMed/NCBI
|