Introduction
Neuroblastoma (NB) is the most common type of
extracranial solid tumor in children, with a high prevalence in
toddlers (1). At diagnosis, a high
proportion of patients have stage IV metastatic disease (2). Intensive treatments for this type of
cancer improved the long-term survival rate, including in children
with high-risk NB (3). However, since
dividing cells are the target of chemo- and radiotherapy, these
treatments act not only on cancer cells but also on germ cells.
Therefore, they may affect reproductive function, exposing patients
to a high risk of infertility (4).
Therefore, fertility preservation for boys with NB is currently
recommended (5,6). For childhood cancer survivors,
preservation of reproductive potential is an important issue for
quality of life (7).
When spermatogenesis is effective in pubertal males,
sperm cryopreservation should be proposed (8). In pre-pubertal males, since
spermatogenesis has not yet started, the preferred strategy is
cryopreservation of testicular tissue (9–11). To
date, no restoration of human fertility has been reported by the
use of frozen/thawed testicular tissue. However, the animal data
are promising, and births have been reported following
spermatogonial stem cell transplantation or testicular tissue
grafting in rodents or pigs (12–14).
Furthermore, in vitro culture of testicular stem cells has
been studied in mice for its potential to generate post-meiotic
male gametes (15,16). These preliminary results may offer the
potential for fertility restoration in young males in the future.
However, fertility restoration using cryopreserved testicular
samples needs to be safe, without any risk of reintroducing cancer
cells.
As a number of cases of metastatic testicular NB
have previously been reported (17–19), the
possible presence of malignant cells in cryopreserved testicular
tissue involves a risk of recurrence of the primary disease
following fertility restoration by germ cell transplantation. The
detection of NB minimal residual disease (MRD) in blood and bone
marrow of patients with metastatic NB was developed using reverse
transcription-quantitative polymerase chain reaction (RT-qPCR) for
tyrosine hydroxylase (TH), paired-like homeobox 2b
(PHOX2B) and doublecortin (DCX) transcripts (20–22). These
transcripts represent useful and clinically significant biomarkers
of MRD in the blood and bone marrow of metastatic NB cells.
However, these biomarkers have not been assessed for NB MRD
detection in testicular tissue. The optimization of NB MRD
detection in testicular tissue is crucial to evaluate the risk of
malignant cell reintroduction. This detection method needs to be
applicable for testicular samples frozen by slow freezing and for
testicular tissues immediately following surgical collection, which
could subsequently be frozen by snap freezing until RNA extraction
is performed. This would allow detection of MRD for previously
cryopreserved testicular tissues and for future testicular sample
collections.
Therefore, the first objective of the present study
was to assess the accuracy of NB MRD detection. This was performed
by quantification of TH, DCX and PHOX2B
transcripts in human testicular tissues, cryopreserved by slow or
snap freezing and contaminated in vitro with increasing
number of tumor cells from two NB cell lines. Once accuracy was
assessed in this in vitro model, the expression levels of
these three biomarkers were evaluated in frozen testicular samples
from pre-pubertal males with and without NB.
Materials and methods
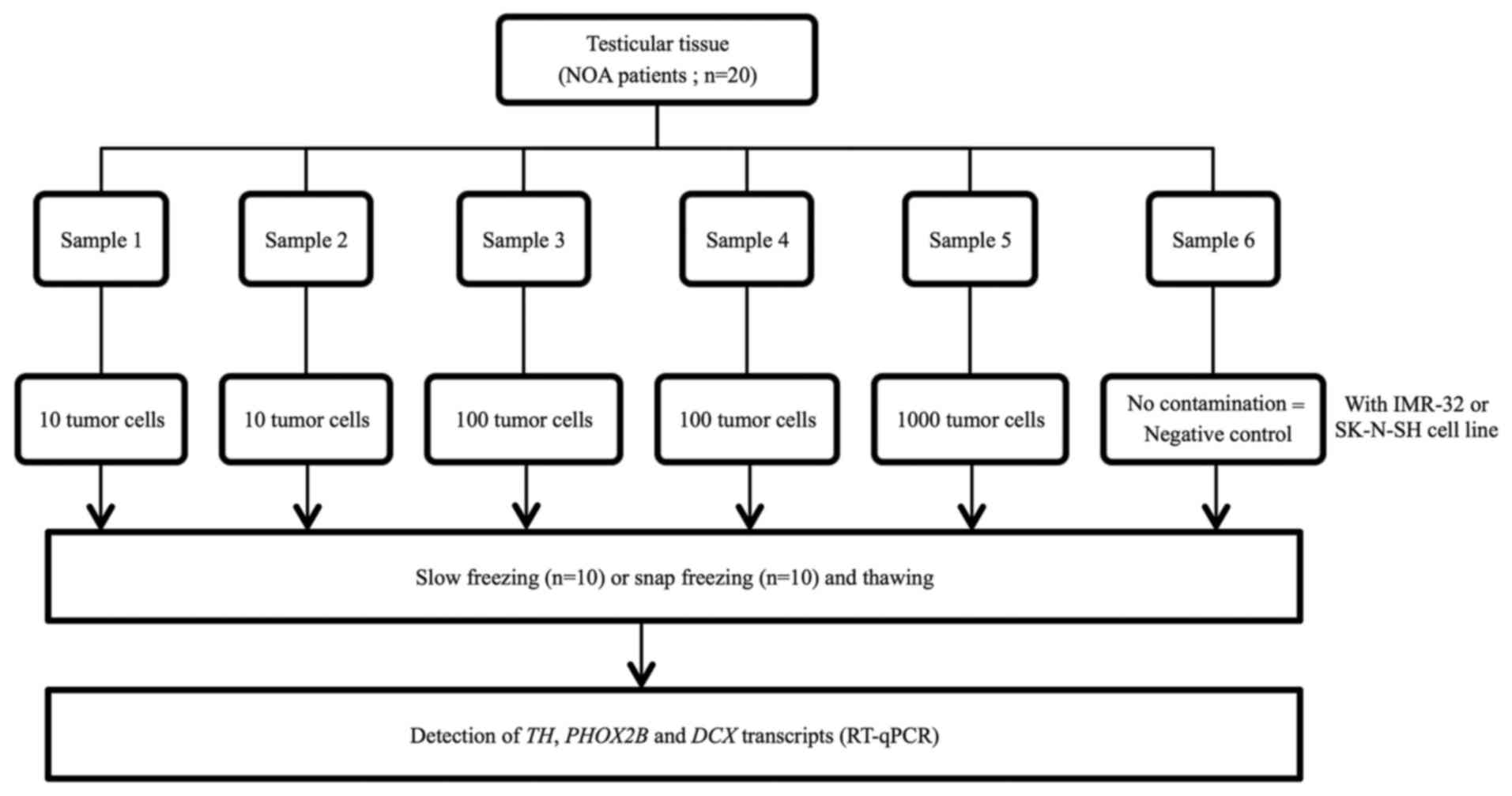
Experimental design
The specificity and sensitivity of NB MRD detection
were assessed by RT-qPCR quantification of TH, PHOX2B
and DCX mRNA expression in thawed testicular tissues that
were contaminated with IMR-32 and SK-N-SH human NB cell lines
(CCL-127 and HTB-11; American Type Culture Collection, Manassas,
VA, USA). Prior to these experiments, IMR-32 and SK-N-SH cells were
investigated for positivity and stability of TH,
PHOX2B and DCX mRNA expression in the subclones.
Subsequently, thawed testicular tissue from patients
with non-obstructive azoospermia (NOA) were contaminated with 0
(negative control), 10, 100 and 1,000 IMR-32 and SK-N-SH tumor
cells from human NB cell lines. The contamination procedure was
performed at room temperature and took ~20 min. RNA extraction was
performed immediately following contamination, without any
additional incubation of the samples. Experiments involving
contamination with 10 and 100 cells were performed in duplicate for
each sample (Fig. 1). Once
contamination was achieved, RNA extraction and RT-qPCR were
performed. Testicular tissues frozen either by snap or slow
freezing methods were used to investigate whether the freezing
method may interfere with RT-qPCR analysis.
Following assessment of MRD detection accuracy in
the in vitro model, thawed testicular samples obtained from
pre-pubertal males with stage IV NB and with non-NB malignancy
(Ewing tumor) were analyzed in order to expand the method to
include pre-pubertal testicular tissues.
Patients and samples
Testicular tissues were obtained from 20 males (mean
age, 32.4 years; range, 25–38 years) with NOA between November 2014
and September 2015 at the University Hospital of Clermont-Ferrand
(Clermont-Ferrand, France). The patients underwent testicular sperm
extraction for intra-cytoplasmic sperm injection. Following sperm
retrieval and freezing, the remaining testicular tissue sample
would usually be destroyed, but in this instance it was used for
the present study.
In addition, testicular tissues obtained from 2
pre-pubertal patients with stage IV NB in January 2012 (patient A,
aged 3 years) and in April 2014 (patient B, aged 2 years) and 2
pre-pubertal patients with Ewing sarcoma in January 2016 (patients
C and D, aged 6 years) were analyzed. Sample A was obtained at the
University Hospital of Rouen (Rouen, France). Samples B, C and D
were obtained at the University Hospital of Clermont-Ferrand
(Clermont-Ferrand, France). Bilateral testis samples from patients
A, B and C were evaluated. For patient D, only one sample of the
right testis was available and evaluated. The median weight of the
testicular samples for these 4 patients was 12 mg.
The present study was approved by the Committee for
Personal Protection (DC 2008 558). Written informed consent was
obtained from all patients prior to enrollment in the present study
and for inclusion of the testicular samples in the GERMETHEQUE
biobank (NFS 96900, www.chu-toulouse.fr/germetheque-centre-de-ressources-biologiques).
In the case of two males with NB who succumbed to disease prior to
the study, informed and written consent was obtained from their
parents. The study was declared on the clinicaltrial.gov website (no. NCT02400970).
Freezing and thawing
For the testicular tissues obtained from adult
patients with NOA, the samples were first cut into 6 thin fragments
of equal size (~1 mm3) following weighing. Subsequently,
the testicular fragments (equally sized samples) were frozen by
using the slow (n=10 patients) or snap (n=10 patients) freezing
method. The testicular tissues obtained from pre-pubertal males had
been previously frozen by slow freezing for the two males with NB
and by snap freezing for the males with Ewing sarcoma.
The slow freezing method was performed as previously
described and validated by Rives et al (10). For the snap freezing method,
testicular samples were put in cryogenic vials and immediately
frozen by immersion in liquid nitrogen. For both freezing
procedures, the samples were stored in cryogenic vials (CRYO BIO
SYSTEM, L'Aigle, France). The same thawing procedure was used for
testicular tissues frozen by slow or snap freezing. The cryogenic
vials were thawed at 37°C for 3 min and placed into three baths of
Leibovitz's L-15 medium (Eurobio, Courtaboeuf, France) for 5 min
for each step at room temperature.
Culture of IMR-32 and SK-N-SH
subclones
IMR-32 and SK-N-SH are well-established subclones of
human cell NB. The IMR-32 cell line was maintained in Dulbecco's
modified Eagle's medium (PAN-Biotech, Aidenbach, Germany),
supplemented with 10% fetal calf serum (PAN-Biotech), 4 mmol/l
L-glutamine, 10 UI/ml penicillin and 10 µg/ml streptomycin
(PAN-Biotech) (23). The SK-N-SH cell
line was maintained in Iscove's modified Dulbecco's Medium
(PAN-Biotech), supplemented with 10% fetal calf serum, 4 mmol/l
L-glutamine, 10 UI/ml penicillin and 10 µg/ml streptomycin. Cell
counting analysis was performed twice prior to each contamination
using the Malassez cell counting chamber. Blue trypan staining
(diluted 1/20 with phosphate buffered saline) for 10 min at room
temperature was used to assess cell viability. For IMR-32 and
SK-N-SH cell lines, the viability was always ≥85%. The cell
counting analysis and cell viability test were performed with a
light microscope by an experienced observer prior to each
contamination test.
Detection of TH, DCX and PHOX2B mRNA
expression by RT-qPCR
RNA was extracted using TRIzol® reagent
(Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA),
according to the manufacturer's instructions. RNA was treated with
DNAse I (Roche Diagnostics, Meylan, France) to remove any
contaminating DNA. A total of 1 µg RNA was reverse-transcribed
using SuperScript II (Invitrogen; Thermo Fisher Scientific, Inc.).
The target TH, DCX and PHOX2B gene transcripts
and the reference β-2-microglobulin (β2M) housekeeping gene
transcript were measured using the LightCycler 480 RT-PCR system
(Roche Diagnostics), using previously reported primers and probes
(24). The sequences are provided in
supplementary methods of the publication (24). The cycling conditions were as follows:
10 min at 95°C, followed by 40 cycles of 95°C for 15 sec and 60°C
for 1 min. Absolute quantification analysis with the LightCycler
software was performed to determine transcripts numbers, as
described previously (20). Briefly,
standard curves were generated using serial dilutions of plasmid
containing a known number of molecules of each transcript and used
to calculate the number of transcripts in the samples. The number
of the reference β2M gene transcripts was used for the
normalization of data. Normalized data were expressed as the copy
numbers of target transcripts per 106 copies of
β2M transcripts. The PCR reactions were performed in
triplicate.
Statistical analysis
Statistical analysis was performed using Stata
software (version 13; StataCorp LP, College Station, TX, US). The
results for quantitative parameters were presented as the mean ±
standard deviation, according to statistical distribution
(assumption of normality assessed by Shapiro-Wilk's test). The
investigation of associations between quantitative parameters was
based on the estimation of correlation coefficients (Pearson's or
Spearman's rho according to statistical distribution, noted r).
Subsequently, in order to take into account differences between and
within subject variability (due to several measurements for a given
patient), random-effects for correlated measures were performed
instead of the usual statistical tests, which would not be
appropriate as the hypothesis of independence of data was not
possible. The assumption of normality of residuals was studied
using the Shapiro-Wilk test. When appropriate (data not exhibiting
normal distributions), a logarithmic transformation was performed
in order to achieve normality assumption and to ensure the correct
use of previous analyses. Finally, receiver operating
characteristic curve analysis was performed to evaluate sensitivity
and specificity of RT-qPCR to detect the expression of TH,
PHOX2B and DCX mRNAs in testicular tissue. All tests
described in this section are two-sided, with a type I error set at
α=0.05: P<0.05 was considered to indicate a statistically
significant difference.
Results
Yield of RNA extraction from
testicular tissue frozen using snap and slow freezing methods
The median weight of testicular samples from 20 men
with NOA was 96 mg (33–210 mg). Each testicular sample was
sectioned into six equal size samples with a median weight of 14 mg
(6–46 mg). The median RNA yield from these samples was 15 µg
(0.6–36.6 µg). The amount of RNA obtained per mg of tissue did not
differ between the testicular samples frozen by snap (0.87 µg/mg)
or slow freezing (0.80 µg/mg) methods (P>0.05).
Expression of TH, PHOX2B and DCX
transcripts in IMR-32 and SK-N-SH cell lines
The expression levels of TH, PHOX2B
and DCX transcripts in IMR-32 and SK-N-SH cell lines were
evaluated for each artificial tumor contamination experiment
(Fig. 2). Overall, the cell lines
exhibited high levels of expression of the three markers, with the
mean normalized values of 3.3×105 for TH,
1.9×107 for PHOX2B and 3.1×107 for
DCX in IMR-32 cells and 3.0×105 for TH,
9.5×106 for PHOX2B and 3.6×107 for
DCX in SK-N-SH cells. The levels of transcripts indicated
minimal variations between different experiments, which were
<1.3 fold. The average fold changes in transcript levels in
IMR-32 and SK-N-SH cells were 1.26 and 1.22 for TH, 1.26 and
1.25 for PHOX2B and 1.28 and 1.27 for DCX,
respectively. These data indicated the high reproducibility of the
cell line models in terms of marker mRNA expression.
Detection of TH, PHOX2B and DCX
transcripts in frozen testicular samples contaminated with IMR-32
and SK-N-SH NB cells
In the present study, expression of TH
transcripts was observed in negative control testicular samples
(n=10). Expression of TH transcripts was detected in samples
frozen by snap freezing (IMR-32, 537 copy number/106
β2M copy number; SK-N-SH, 475 copy number/106
β2M copy number) and by slow freezing (IMR-32, 363 copy
number/106 β2M copy number; SK-N-SH, 490 copy
number/106 β2M copy number; Fig. 3A). Compared with the negative control
(uncontaminated testicular samples), the level of TH mRNA
was significantly higher in testicular samples contaminated with
100 and 1,000 NB cells from IMR-32 and SK-N-SH cell lines,
respectively (P<0.001). There was no significant difference
between the levels of TH mRNA detected in testicular samples
contaminated with 10 NB cells and uncontaminated samples (IMR-32,
P=0.18; SK-N-SH, P=0.24). For determination of TH
expression, the specificity and sensitivity rates were 100% when
100 NB cells were used for contamination.
 | Figure 3.Relative expression of (A) TH,
(B) PHOX2B and (C) DCX in thawed testicular tissues
following contamination by neuroblastoma cell lines (0, 10, 100 and
1,000 cells). Each symbol represents one testicular tissue
fragment. Blue, IMR-32 cells; red, SK-N-SH cells. ns, no
significant; TH, tyrosine hydroxylase; PHOX2B, paired-like homeobox
2b; DCX, doublecortin. |
PHOX2B mRNA was not detected in the
uncontaminated testicular samples (Fig.
3B) frozen either by the snap or slow freezing method (n=10).
PHOX2B transcripts were detected at significantly different
levels following contamination of testicular samples with 10, 100
and 1,000 NB cells (P<0.001 for IMR-32 and SK-N-SH).
Furthermore, there was a strong linear correlation between the
number of NB cells used for contamination (10, 100 and 1,000 NB
cells) and the levels of PHOX2B mRNA (r=0.96 for IMR-32 and
SK-N-SH). The specificity and sensitivity rates for PHOX2B
mRNA detection were 100% following contamination by 10 NB IMR-32 or
SK-N-SH cells.
High expression levels of DCX mRNA were
detected in negative controls (n=10) frozen by snap freezing
(IMR-32, 73,231 copy number/106 β2M copy number;
SK-N-SH, 68,386 copy number/106 β2M copy number)
and by slow freezing (IMR-32, 64,811 copy number/106
β2M copy number; SK-N-SH, 78,810 copy number/106
β2M copy number) methods (Fig.
3C). Furthermore, there was no significant difference in
DCX mRNA levels between the negative controls and samples
contaminated with 10, 100 and 1,000 NB cells.
Analysis of TH, DCX and PHOX2B mRNA
expression levels in testicular tissues of pre-pubertal males
In the testicular samples obtained from two
pre-pubertal NB stage IV males, the levels of TH mRNA were
similar in the right (patient A, 431 copy number/106
β2M copy number; patient B, 469 copy number/106
β2M copy number) and left (patient A, 420 copy
number/106 β2M; patient B, 371 copy
number/106 β2M copy number) testis tissue
samples. PHOX2B mRNA was undetectable in the testis samples
of patient A and B. Similar high levels of DCX mRNA were
observed in the right (patient A, 58,700 copy number/106
β2M; patient B: 48,297 copy number/106
β2M) and left (patient A: 51,280 copy number/106
β2M; patient B: 44,738 copy number/106
β2M) testis samples.
In the samples obtained from two pre-pubertal males
with no-NB malignancy (Ewing sarcoma; patients C and D), mRNA
TH levels were similar in the right (patient C, 684 copy
number/106 β2M; patient D, 500 copy
number/106 β2M) and left (patient C, 736 copy
number/106 β2M copy number) testis. PHOX2B
mRNA was not detected in testis samples obtained from either male.
High levels of DCX mRNA were observed in the right (patient
C, 53,690 copy number/106 β2M; patient D, 59,380
copy number/106 β2M copy number) and left
(patient C, 59,380 copy number/106 β2M copy
number) testis samples.
High expression levels of TH and DCX
observed in the testicular tissues of the four pre-pubertal males
were similar to the high expression levels detected in
uncontaminated testicular samples (negative controls) in the in
vitro model described previously in the results section.
Discussion
Given the increased survival rate of patients with
NB and the cytotoxic effects of therapies used for treatment of
this cancer (25), fertility
preservation is highly recommended for these children. Therefore,
for a pre-pubertal male facing sterilizing chemotherapy, testicular
biopsy may be performed as a preventive strategy. Freezing
testicular tissue allows subsequent transplantation either by
infusion of a testicular cell suspension into the seminiferous
tubules (26) or intra-testicular
grafting of tissue (27). However,
>60% of children with metastatic NB have circulating tumor cells
at the time of diagnosis (28).
Although testis is not the most frequent NB invasion site, numerous
cases of testicular NB metastasis have been described previously.
Simon et al (19) reported
testicular metastasis in 10/1,076 male patients with NB using the
data of the Cooperative German Neuroblastoma trials. Kushner et
al (29) demonstrated 11 positive
cases in a series of 289 male NB autopsies. Nistal et al
(30) also reported two cases of
testicular metastases confirmed by histological examination in a
total of 216 NB patients. Therefore, the possible presence of NB
cells in testicular tissue collected from NB males should be taken
into account to avoid reintroducing cancer cells when the thawed
testicular sample is used to restore fertility. However, in all of
the previous studies mentioned, only histological analyses were
performed. As the sensitivity of MRD detection by histological
analysis is lower compared with RT-qPCR, the actual frequency of NB
infiltration in testis may be higher.
In the present study, sufficient amounts of RNA were
extracted from small testicular samples to perform RT-qPCR in
optimal conditions and to analyze the level of three transcripts
associated with NB. The use of a small quantity of testicular
tissue to detect NB MRD ensures that a sufficient amount of sample
remains for fertility preservation in pre-pubertal males, in whom
large surgical retrieval is not always possible due to age and
small testis size. The present study did not observe any effect of
the freezing method on the yield of RNA extracted. Therefore, the
RT-qPCR method may be performed on testis samples that have already
been cryopreserved using slow freezing and on samples, which are
cryopreserved by snap freezing at the time of surgical retrieval
for subsequent analysis.
In the present study, an in vitro model of NB
dissemination in human testicular tissue was established to
evaluate the sensitivity and specificity for the detection of NB
mRNAs. The SK-N-SH and IMR-32 tumor cell lines used for
contaminations are well known and were established from human NB.
SK-N-SH cells were established from the bone marrow metastasis from
a 4 year-old Caucasian child (31).
IMR-32 cells were obtained from a metastatic site in an abdominal
mass in a 13 month-old Caucasian male with NB. The tumor was
diagnosed as NB with rare areas of organoid differentiation
(32). Therefore, SK-N-SH and IMR-32
human cell lines are highly representative of metastatic NB. In the
present study, TH, DCX and PHOX2B mRNAs were
expressed at high levels in SK-N-SH and IMR-32 cell lines. The
testicular samples that were used to validate the in vitro
contamination model were obtained from adult males with NOA, as it
was unethical to perform these preclinical tests with healthy
pre-pubertal testicular samples. Similar to pre-pubertal patients,
testicular biopsies from patients with NOA contain low numbers or
absence of mature germ cells.
In children with NB, metastatic tumor cells were
previously detected in the bone marrow and peripheral blood by
RT-qPCR for NB-specific target genes, including TH,
DCX and PHOX2B (24,33,34). To
the best of our knowledge, this is the first study to quantify the
expression level of these transcripts in human testicular tissues
to detect MRD. TH encodes for the key enzyme involved in the
synthesis of catecholamines, which serves a functional role in the
testis. A previous study provided evidence that Leydig cells
exhibited close similarity to cathecholaminergic nerve cells with
high expression of TH (35).
This may be explained by a developmental arrest of Leydig cells at
the immature state (36). In
addition, Leydig cells are characterized as non-dividing cells with
characteristics of early stem cell-like progenitors with endocrine,
neuronal and glial cell features (37). Although TH is one of the most
commonly used targets for MRD detection in peripheral blood and
bone marrow of patients with NB (20,21), the
use of this transcript as an MRD marker in testicular samples is
hindered by its background expression detected in uncontaminated
samples of patients with NOA and pre-pubertal males with and
without NB. Therefore, it is hypothesized that the background
expression of TH may be due to the presence of Leydig cells
(35,37). Furthermore, 100% sensitivity and
specificity rates of TH detection were only observed when
100 NB cells were used for contamination, which may suggest that
the accuracy of this marker for NB MRD detection is insufficient
for detection in human testicular samples.
Previously, the expression level of other
transcripts, including DCX and PHOX2B, were
demonstrated to be useful for NB MRD detection in bone marrow and
peripheral blood from patients with metastasis (24). DCX is involved in the signaling
pathway that regulates microtubule in migrating neurons (38). A previous study reported a high
expression of a DCX homolog, DCD1, in human testis
(39). This may explain the lack of
sensitivity and specificity that was observed for analysis of
DCX expression in the in vitro model in the present
study, and the high expression of DCX in pre-pubertal males
with or without NB. PHOX2B encodes a transcription factor
involved in the development of the autonomous nervous system
(34,40). It was previously revealed that
PHOX2B is a highly specific marker for sensitive MRD
detection of NB in the bone marrow, peripheral blood and harvested
hematopoietic stem cells (40). To
the best of our knowledge, the present study demonstrated for the
first time a high sensitivity and specificity of RT-qPCR analysis
for PHOX2B mRNA, enabling the detection of as few as 10 NB
cells in a testis sample. The absence of background PHOX2B
expression in uncontaminated testicular samples underlines the high
specificity of this marker. Furthermore, PHOX2B expression
was not detected in testicular samples of pre-pubertal males
without NB in the present study. The present study demonstrated
that NB MRD assessment in human testicular tissue by the detection
of PHOX2B by RT-qPCR is highly accurate. It is unknown
whether MRD marker genes of NB are up- or downregulated during
treatment (23,24), so a panel of PCR targets may be
required to overcome tumor heterogeneity (41). Since TH and DCX
transcripts are not sensitive and specific NB markers in testicular
tissues, it will be necessary to continue the evaluation of other
known NB-specific transcripts. Analysis of NB mRNA is able to
detect the presence of malignant cells but cannot predict their
vitality or invasive potential. Therefore, further studies are
required to investigate the risk of tumor dissemination on
MRD-positive pre-pubertal testicular samples by xenotransplantation
in rete testis of nude or severe combined immunodeficiency (SCID)
mice.
In conclusion, the present study provides evidence
that among the established NB markers for MRD analysis of blood and
bone marrow using RT-qPCR, PHOX2B mRNA may provide an
accurate assessment of MRD in testicular tissues for males that
require fertility preservation. These preliminary results require
confirmation by a further study of testicular tissues from a large
cohort of pre-pubertal males with NB and additional studies are
warranted to evaluate the safety threshold by xenotransplantation
in nude or SCID mice.
Acknowledgments
The present authors would like to thank the Ligue
contre le Cancer for supporting the project. The authors also thank
Mrs. Camille Meindre and Mrs. Lucie Vivier (Centre de Biothérapie
d'Auvergne, CHU Clermont-Ferrand, Clermont-Ferrand, France), Mrs.
Sandra Carlet-Dollet and Mr. Cyril Bouche (Assistance Médicale à la
Procréation, CECOS, CHU Clermont-Ferrand, Clermont-Ferrand,
France), Mrs. Marine Nervi and Mrs. Farida Godeau (Cytogénétique
Médicale, CHU Clermont-Ferrand, Clermont-Ferrand, France) and Mrs.
Alexandra Usclade (Unité CRECHE, INSERM-CIC 1405, Université
Clermont Auvergne, Clermont-Ferrand, France) for their excellent
technical assistance.
References
|
1
|
Kaatsch P: Epidemiology of childhood
cancer. Cancer Treat Rev. 36:277–285. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Haase GM, Perez C and Atkinson JB: Current
aspects of biology, risk assessment, and treatment of
neuroblastoma. Semin Surg Oncol. 16:91–104. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Oberthuer A, Hero B, Berthold F, Juraeva
D, Faldum A, Kahlert Y, Asgharzadeh S, Seeger R, Scaruffi P, Tonini
GP, et al: Prognostic impact of gene expression-based
classification for neuroblastoma. J Clin Oncol. 28:3506–3515. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Brougham MF and Wallace WH: Subfertility
in children and young people treated for solid and haematological
malignancies. Br J Haematol. 131:143–155. 2005.PubMed/NCBI
|
|
5
|
Lee SJ, Schover LR, Partridge AH, Patrizio
P, Wallace WH, Hagerty K, Beck LN, Brennan LV and Oktay K: American
Society of Clinical Oncology: American Society of Clinical Oncology
recommendations on fertility preservation in cancer patients. J
Clin Oncol. 24:2917–2931. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Loren AW, Mangu PB, Beck LN, Brennan L,
Magdalinski AJ, Partridge AH, Quinn G, Wallace WH and Oktay K;
American Society of Clinical Oncology, : Fertility preservation for
patients with cancer: American Society of Clinical Oncology
clinical practice guideline update. J Clin Oncol. 31:2500–2510.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sudour-Bonnange H, Tabone MD,
Thomas-Teinturier C, Pacquement H, Oberlin O, Marec-Berard P,
Laurence V, Aubier F, Duranteau L, Bernier-Chastagner V, et al:
Fertility preservation in children and teenagers with cancer. Bull
Cancer. 100:727–735. 2013.(In French). PubMed/NCBI
|
|
8
|
Daudin M, Rives N, Walschaerts M,
Drouineaud V, Szerman E, Koscinski I, Eustache F, Saïas-Magnan J,
Papaxanthos-Roche A, Cabry-Goubet R, et al: Sperm cryopreservation
in adolescents and young adults with cancer: Results of the French
national sperm banking network (CECOS). Fertil Steril.
103:478–486.e1. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wyns C, Curaba M, Vanabelle B, Van
Langendonckt A and Donnez J: Options for fertility preservation in
prepubertal boys. Hum Reprod Update. 16:312–328. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rives N, Milazzo JP, Travers A, Arkoun B,
Bironneau A, Sibert L, Liard-Zmuda A, Marie-Cardine A, Schneider P,
Vannier JP and Macé B: Cryopreservation of testicular tissue in
children. Bull Acad Natl Med. 197:877–886. 2013.(In French).
PubMed/NCBI
|
|
11
|
Goossens E, Van Saen D and Tournaye H:
Spermatogonial stem cell preservation and transplantation: From
research to clinic. Hum Reprod. 28:897–907. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shinohara T, Inoue K, Ogonuki N,
Kanatsu-Shinohara M, Miki H, Nakata K, Kurome M, Nagashima H,
Toyokuni S, Kogishi K, et al: Birth of offspring following
transplantation of cryopreserved immature testicular pieces and
in-vitro microinsemination. Hum Reprod. 17:3039–3045. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kanatsu-Shinohara M, Ogonuki N, Inoue K,
Ogura A, Toyokuni S and Shinohara T: Restoration of fertility in
infertile mice by transplantation of cryopreserved male germline
stem cells. Hum Reprod. 18:2660–2667. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nakai M, Kaneko H, Somfai T, Maedomari N,
Ozawa M, Noguchi J, Ito J, Kashiwazaki N and Kikuchi K: Production
of viable piglets for the first time using sperm derived from
ectopic testicular xenografts. Reproduction. 139:331–335. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Stukenborg JB, Schlatt S, Simoni M, Yeung
CH, Elhija MA, Luetjens CM, Huleihel M and Wistuba J: New horizons
for in vitro spermatogenesis? An update on novel three-dimensional
culture systems as tools for meiotic and post-meiotic
differentiation of testicular germ cells. Mol Hum Reprod.
15:521–529. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Reuter K, Ehmcke J, Stukenborg JB, Simoni
M, Damm OS, Redmann K, Schlatt S and Wistuba J: Reassembly of
somatic cells and testicular organogenesis in vitro. Tissue Cell.
46:86–96. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kumari PK, Surendran N, Chellam VG, Pillai
GR and Ramachandran K: Neuroblastoma with testicular metastasis.
Review of literature and report of a case. Indian J Cancer.
31:52–55. 1994.PubMed/NCBI
|
|
18
|
Casola G, Scheible W and Leopold GR:
Neuroblastoma metastatic to the testis: ultrasonographic screening
as an aid to clinical staging. Radiology. 151:475–476. 1984.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Simon T, Hero B and Berthold F: Testicular
and paratesticular involvement by metastatic neuroblastoma. Cancer.
88:2636–2641. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tchirkov A, Paillard C, Halle P, Bernard
F, Bordigoni P, Vago P, Deméocq F and Kanold J: Significance of
molecular quantification of minimal residual disease in metastatic
neuroblastoma. J Hematother Stem Cell Res. 12:435–442. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Burchill SA, Lewis IJ, Abrams KR, Riley R,
Imeson J, Pearson AD, Pinkerton R and Selby P: Circulating
neuroblastoma cells detected by reverse transcriptase polymerase
chain reaction for tyrosine hydroxylase mRNA are an independent
poor prognostic indicator in stage 4 neuroblastoma in children over
1 year. J Clin Oncol. 19:1795–1801. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chambon F, Tchirkov A, Pereira B, Rochette
E, Deméocq F and Kanold J: Molecular assessment of minimal residual
disease in PBSC harvests provides prognostic information in
neuroblastoma. Pediatr Blood Cancer. 60:E109–E112. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Stutterheim J, Zappeij-Kannegieter L, Ora
I, van Sluis PG, Bras J, den Ouden E, Versteeg R, Caron HN, van der
Schoot CE and Tytgat GA: Stability of PCR targets for monitoring
minimal residual disease in neuroblastoma. J Mol Diagn. 14:168–175.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Viprey VF, Gregory WM, Corrias MV,
Tchirkov A, Swerts K, Vicha A, Dallorso S, Brock P, Luksch R,
Valteau-Couanet D, et al: Neuroblastoma mRNAs predict outcome in
children with stage 4 neuroblastoma: A European HR-NBL1/SIOPEN
study. J Clin Oncol. 32:1074–1083. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Pinto NR, Applebaum MA, Volchenboum SL,
Matthay KK, London WB, Ambros PF, Nakagawara A, Berthold F,
Schleiermacher G, Park JR, et al: Advances in risk classification
and treatment strategies for neuroblastoma. J Clin Oncol.
33:3008–3017. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Brünsten RL and Zimmermann JW:
Spermatogenesis following male germ-cell transplantation. Proc Natl
Acad Sci USA. 91:pp. 11298–11302. 1994; PubMed/NCBI
|
|
27
|
Baert Y, van Saen D, Haentjens P, In't
Veld P, Tournaye H and Goossens E: What is the best
cryopreservation protocol for human testicular tissue banking? Hum
Reprod. 28:1816–1826. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yáñez Y, Hervás D, Grau E, Oltra S, Pérez
G, Palanca S, Bermúdez M, Márquez C, Cañete A and Castel V: TH and
DCX mRNAs in peripheral blood and bone marrow predict outcome in
metastatic neuroblastoma patients. J Cancer Res Clin Oncol.
142:573–580. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kushner BH, Vogel R, Hajdu SI and Helson
L: Metastatic neuroblastoma and testicular involvement. Cancer.
56:1730–1732. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nistal M, González-Peramato P and Paniagua
R: Secondary testicular tumors. Eur Urol. 16:185–188.
1989.PubMed/NCBI
|
|
31
|
Gilbert LC and Wachsman JT:
Characterization and partial purification of the plasminogen
activator from human neuroblastoma cell line, SK-N-SH. A comparison
with human urokinase. Biochim Biophys Acta. 704:450–460. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tumilowicz JJ, Nichols WW, Cholon JJ and
Greene AE: Definition of a continuous human cell line derived from
neuroblastoma. Cancer Res. 30:2110–2118. 1970.PubMed/NCBI
|
|
33
|
Viprey VF, Corrias MV, Kagedal B, Oltra S,
Swerts K, Vicha A, Ladenstein R and Burchill SA: Standardisation of
operating procedures for the detection of minimal disease by
QRT-PCR in children with neuroblastoma: Quality assurance on behalf
of SIOPEN-R-NET. Eur J Cancer. 43:341–350. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Viprey VF, Lastowska MA, Corrias MV,
Swerts K, Jackson MS and Burchill SA: Minimal disease monitoring by
QRT-PCR: Guidelines for identification and systematic validation of
molecular markers prior to evaluation in prospective clinical
trials. J Pathol. 216:245–252. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Davidoff MS, Ungefroren H, Middendorff R,
Koeva Y, Bakalska M, Atanassova N, Holstein AF, Jezek D, Pusch W
and Müller D: Catecholamine-synthesizing enzymes in the adult and
prenatal human testis. Histochem Cell Biol. 124:313–323. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Seil FJ, Johnson ML, Nishi R and Nilaver
G: Tyrosine hydroxylase expression in non-catecholaminergic cells
in cerebellar cultures. Brain Res. 569:164–168. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Schulze W, Davidoff MS and Holstein AF:
Are Leydig cells of neural origin? Substance P-like
immunoreactivity in human testicular tissue. Acta Endocrinol
(Copenh). 115:373–377. 1987.PubMed/NCBI
|
|
38
|
Oltra S, Martinez F, Orellana C, Grau E,
Fernandez JM, Cañete A and Castel V: The doublecortin gene, a new
molecular marker to detect minimal residual disease in
neuroblastoma. Diagn Mol Pathol. 14:53–57. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zeng L, Gu S, Li Y, Zhao E, Xu J, Ye X, Wu
Q, Wang L, Xie Y and Mao Y: Identification of a novel human
doublecortin-domain-containing gene (DCDC1) expressed mainly in
testis. J Hum Genet. 48:393–396. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Stutterheim J, Gerritsen A,
Zappeij-Kannegieter L, Kleijn I, Dee R, Hooft L, van Noesel MM,
Bierings M, Berthold F, Versteeg R, et al: PHOX2B is a novel and
specific marker for minimal residual disease testing in
neuroblastoma. J Clin Oncol. 26:5443–5449. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Corrias MV, Haupt R, Carlini B, Cappelli
E, Giardino S, Tripodi G, Tonini GP, Garaventa A, Pistoia V and
Pistorio A: Multiple target molecular monitoring of bone marrow and
peripheral blood samples from patients with localized neuroblastoma
and healthy donors. Pediatr Blood Cancer. 58:43–49. 2012.
View Article : Google Scholar : PubMed/NCBI
|