Introduction
Breast cancer is one of the most common malignant
tumors of females with high incidence and high mortality (1,2). It was
traditionally believed that tumor was originated from cell mutation
and could grow unlimitedly. However, theories on tumor stem cells
have extended knowledge on tumor cells, indicating that tumor
develops from tumor stem cells in tissues (3,4). The above
recent theory, not only explained biological behavior of breast
cancer cells, but also provided new research directions for tumor
treatment.
Radiotherapy involves X- or gamma-ray treatment onto
tumor region and is one of the main methods of treating tumor. The
rays interact with molecules (mainly water molecules) in tumor
cells to produce cytotoxic OH-free radical resulting in cell death
or apoptosis (5). However, during
conventional radiotherapy, resistance of cancer cells towards rays
is commonly observed (6,7). Therefore, seeking strategies to improve
breast cancer radiosensitivity is a recent hot spot in radiotherapy
research against tumor.
Targeting protein for Xenopus kinesin-like protein 2
(TPX2) gene, also called XKIP2-targeted protein, is
necessary for the microtubule structuring process of cell
kinetochore (8–10). Abundant research in recent years has
shown that TPX2 gene is closely related with the development
of cancer cells such as lung, colon and cervical cancer cells
(11). However, there are few studies
on the association between TPX2 gene and breast cancer
cells.
To the best of our knowledge, the present study
examined for the first time TPX2 expression in breast tumor
stem cells and investigated the association between TPX2
gene and breast tumor stem cells. The present study also involved
exploration of radiotherapy with various sensitizers on breast stem
cells by targeting the TPX2 gene.
Materials and methods
Experimental materials
Bcap37, MCF7, SKBR3 and MDAMB231 breast cancer cells
were purchased from the American Type Culture Collection (ATCC)
cell bank (Manassas, VA, USA). Tissue samples were collected from
55 cases of breast cancer cells removed during surgeries from March
2014 to June 2016 in the Hexian Memorial Hospital of Panyu
(Guangzhou, China). The samples were confirmed by biopsy. According
to clinical staging by International Federation of Gynecology and
Obstetrics (FIGO). There were 12, 13, 9 and 21 cases of I–IV
stages, respectively. The patients were aged 29–55 years with an
average of 38.4±3.9 years. Normal breast cells were collected for
comparison. Compounds with spectral sensitization such as
docetaxel, lovastatin and β-santalene were obtained.
Extraction of cell total proteins
Specific experimental methods were previously
described (12). Extracted proteins
were saved at −80°C.
Western blot analysis
Specific experimental methods were carried out as
previously described (13).
Extraction of total RNA, detection and
determination of purity
Experimental methods were conducted as in the
literature (14), with some
modifications. Extracted proteins were saved at −80°C.
Radiotherapy experiments on the
sensitizing compounds
Docetaxel, lovastatin and β-santalene of the same
concentration (20 mg/l) were prepared to function in Bcap37 breast
cancer cells. Sensitizing compounds of the same concentration (10,
15, 20, 25, 30, 40 and 50 mg/l) were prepared to investigate
effects of concentration on breast cancer cells (15).
Grouped processing of
sensitization
Two microliters of culture and buffer solutions were
added to group A for comparison. Different sensitizers at a rate of
20 mg/l were added to group B. In group C no sensitizer was given
and underwent radiotherapy only. After the experiment, the cell
apoptotic rate was recorded by flow cytometry (16).
Radiotherapy and flow cytometry
Specific experimental process was carried out as
published (15).
Immunohistochemistry experiment
For detection of TPX2 expression in breast tissues,
we performed inmmunohistochemical staining according to a previous
study (17).
Statistical analysis
Experimental data were analyzed by SPSS software
(Chicago, IL, USA). Differences among groups underwent homogeneity
test for variance and t-test; testing level was α=0.05. (P<0.05
was considered to indicate a statistically significant
difference).
Results
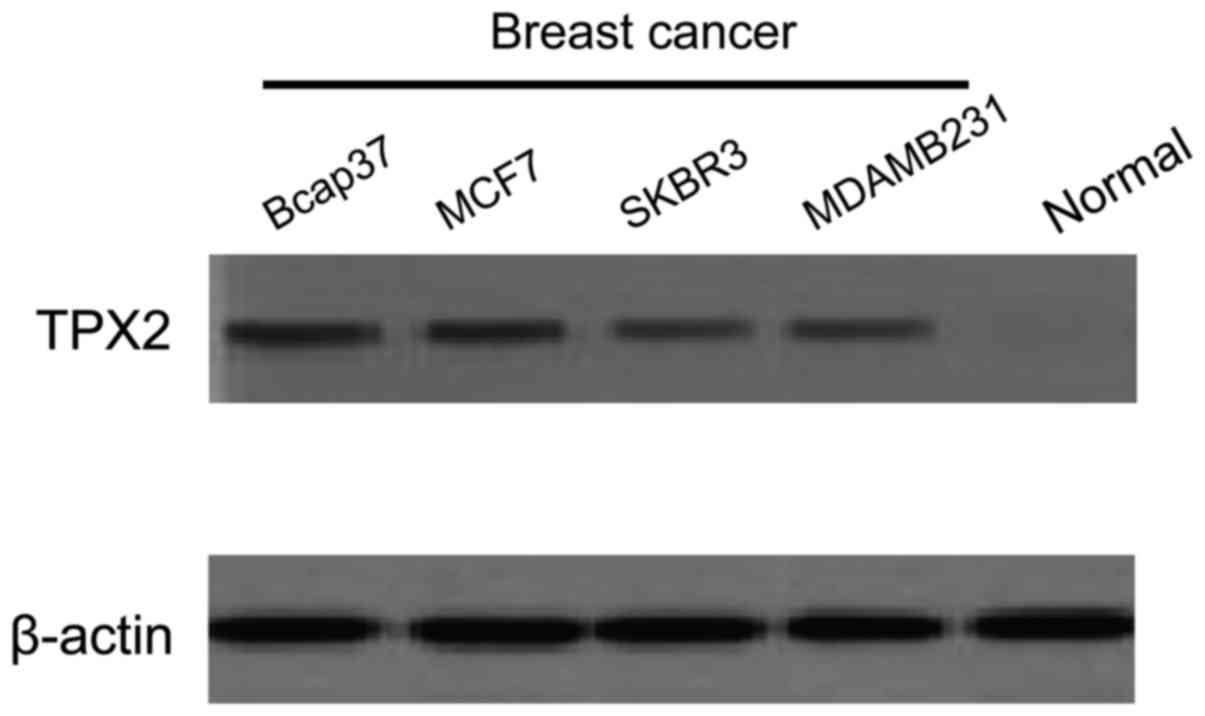
Detection of TPX2 protein expression
in different breast cancer cells by western blot analysis
TPX2 protein expression in four types of breast
cancer cells, Bcap37, MCF7, SKBR3 and MDAMB231 were detected by
western blot analysis. Normal breast cells were used for
comparison, and the OD value ratio of TPX2 and β-actin referred to
TPX2 protein relative expression. By combining markers, it was
confirmed that the bands between a molecular weight of 100 and 43
kDa were TPX2 protein and β-actin (Fig.
1). It was observed that TPX2 was expressed in the four types
of breast cancer cells but not expressed in the normal cells. This
experiment compared the detected OD values with image scanning and
analyzing software and conducted statistical processing. Table I shows that TPX2 protein expression in
four types of breast cancer cells was significantly higher than
that in normal cells (0.003±0.001), but TPX2 protein expression
between each pair of breast cancer cells had no statistical
significance (P>0.05).
 | Table I.TPX2 protein relative expression in
four types of breast cancer cells (mean ± SD). |
Table I.
TPX2 protein relative expression in
four types of breast cancer cells (mean ± SD).
| Variables | Normal cell | Bcap37 | MCF7 | SKBR3 | MDAMB231 |
|---|
| TPX2 (OD) | 0.028±0.012 | 0.318±0.023 | 0.377±0.019 | 0.373±0.018 | 0.374±0.022 |
| β-actin (OD) | 0.93±0.13 | 0.89±0.11 | 0.93±0.22 | 0.95±0.13 | 0.97±0.21 |
| Relative
expression |
0.003±0.001a |
0.357±0.043b |
0.406±0.093b |
0.393±0.025b |
0.386±0.036b |
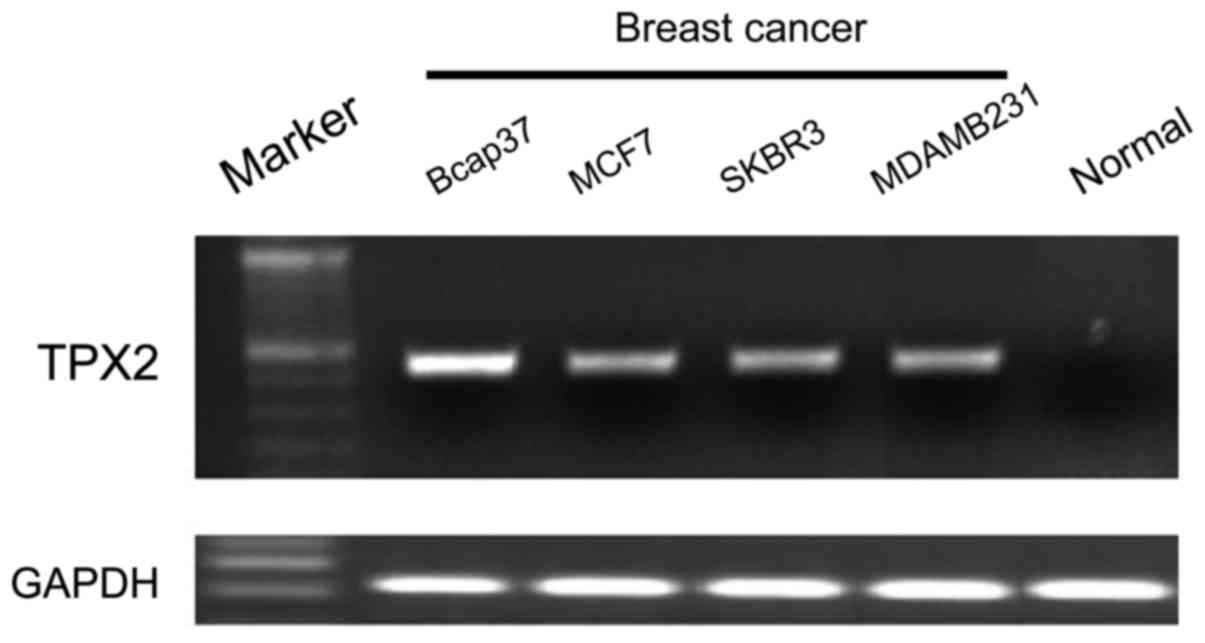
Detection of TPX2 mRNA expression in
different breast cancer cells by RT-PCR
TPX2 mRNA expression in Bcap37, MCF7, SKBR3 and
MDAMB231 was detected by RT-PCR. Normal breast cells were used for
comparison, and OD value ratio of TPX2 and GAPDH referred to TPX2
gene expression. It is clear from Fig.
2 that TPX2 mRNA expression was similar to its protein
expression in that it was expressed in the four types of breast
cancer cells but not expressed in the normal cells. This experiment
compared the detected OD values with image scanning and analyzing
software and statistical processing was conducted. The TPX2 mRNA
expression (Table II) in the four
types of breast cancer cells (0.536±0.039 on average) was
significantly higher than that in normal cells (0.005±0.002), but
TPX2 mRNA expression between each pair of breast cancer cells had
no statistical significance (P>0.05).
 | Table II.TPX mRNA expression in different
breast cancer cells (mean ± SD). |
Table II.
TPX mRNA expression in different
breast cancer cells (mean ± SD).
| Variables | Normal cells | Bcap37 | MCF7 | SKBR3 | MDAMB231 |
|---|
| TPX2 (OD) | 0.004±0.012 | 0.464±0.034 | 0.520±0.028 | 0.478±0.017 | 0.499±0.052 |
| GAPDH (OD) | 0.86±0.11 | 0.84±0.18 | 0.90±0.28 | 0.93±0.15 | 0.89±0.17 |
| Relative
expression |
0.005±0.002a |
0.553±0.023b |
0.578±0.091b |
0.514±0.033b |
0.561±0.062b |
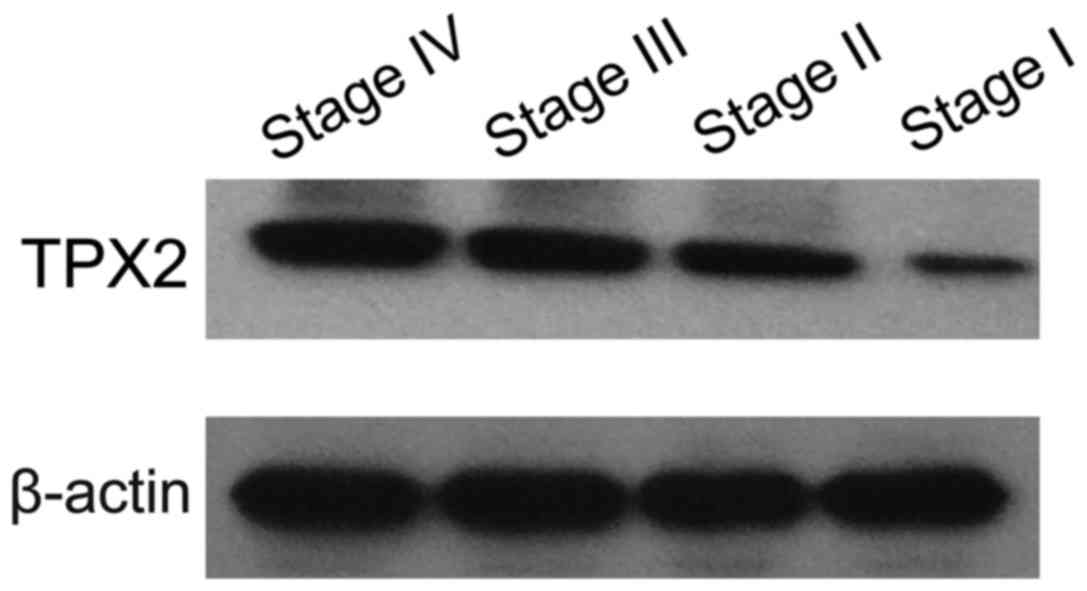
Detection of TPX2 expression in breast
cancer cells at various differentiation stages by western blot
analysis
TPX2 expression in breast cancer cells at the
various differentiation stages was detected by western blot
analysis to investigate TPX2 protein changes in the development of
breast cancer cells. Experimental results are shown in Fig. 3. The results showed that TPX2 protein
expression at stages I–IV was significantly increased along with
the increased of differentiation stages.
Investigation on radiotherapy effects
on three types of broad-spectrum sensitizers
In the present study, in comparison to the control
group, docetaxel and lovastatin produced less effect on breast
cancer cells confirming that cytotoxicity of the two compounds was
not strong. However, β-santalene between two groups had no
significant differences, reflecting its strong cytotoxicity.
Furthermore, lovastatin had the strongest effects. By comparing
three kinds of sensitizers, it was observed that lovastatin had
little cytotoxicity but obvious radiotherapy improving effects;
thus, it is a relatively reasonable radiotherapy sensitizer on
breast cancer cells. As a result, lovastatin was chosen to
investigate the effects of different concentration on breast cancer
cells (Tables III and IV).
 | Table III.Comparison of radiotherapy effects of
three types of broad-spectrum sensitizers on breast cancer stem
cells (cell apoptosis rate, %; mean ± SD). |
Table III.
Comparison of radiotherapy effects of
three types of broad-spectrum sensitizers on breast cancer stem
cells (cell apoptosis rate, %; mean ± SD).
| Groups | Docetaxel | Lovastatin | β-santalene |
|---|
| A (control) |
0.5±0.02 |
0.7±0.05 |
0.4±0.03 |
| B (adding
medicine) |
0.6±0.12 |
0.3±0.11 |
3.3±0.08 |
| C (radiotherapy) |
15.2±0.22a,b |
21.3±1.21a,b |
6.9±0.52a,b |
| D (radiotherapy and
adding medicine) |
18.5±1.11a–c |
33.2±2.10a–c |
11.3±1.15a–c |
 | Table IV.Comparison of radiotherapy effects of
lovastatin at different concentrations on breast cancer stem cells
(concentration, mg/l; cell apoptosis rate, %; mean ± SD). |
Table IV.
Comparison of radiotherapy effects of
lovastatin at different concentrations on breast cancer stem cells
(concentration, mg/l; cell apoptosis rate, %; mean ± SD).
|
| Concentrations
(mg/l) |
|---|
|
|
|
|---|
| Groups | 10 | 15 | 20 | 25 | 30 | 40 | 50 |
|---|
| C
(radiotherapy) | 21.5±1.21 | 19.6±1.42 | 22.8±1.11 | 18.1±1.32 | 19.4±1.47 | 20.8±2.01 | 20.2±1.96 |
| D (radiotherapy and
adding medicine) |
25.4±2.12a |
30.4±2.31a |
35.6±2.51a |
38.7±2.12a |
38.9±1.58a |
37.8±2.45a |
38.2±2.66a |
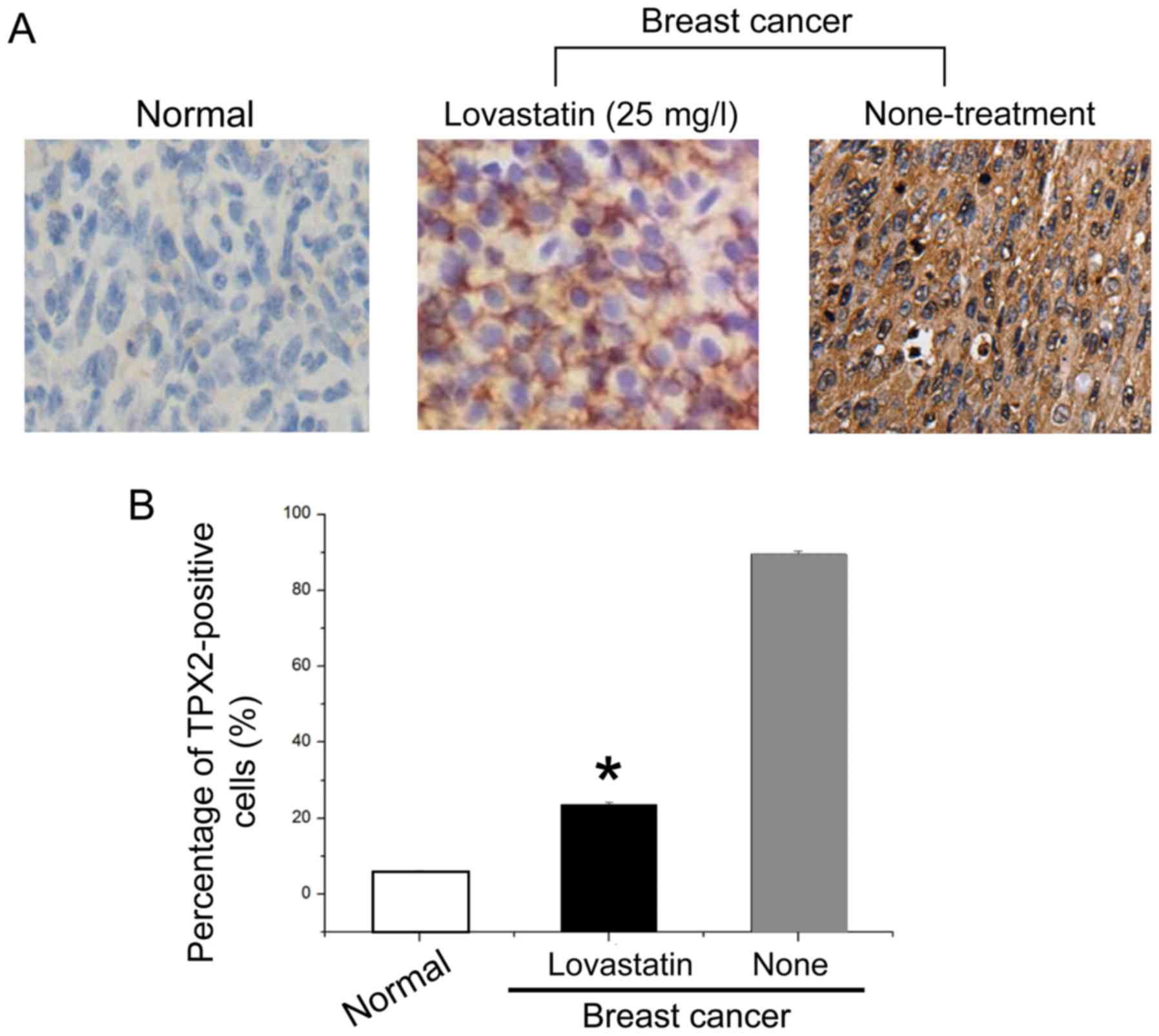
Immunohistochemical results of
different groups
Cells undergoing various processing were used as
research subjects, and TPX2 protein expression in the cells of
different groups were detected by immunohistochemistry. Fig. 4A shows that TPX2 protein-positive rate
of breast cancer cells processed by 25 mg/l lovastatin were
significantly lower than that of normal cancer cells. Counting
results of positive cells (Fig. 4B)
indicated that TPX2 protein positive rate of breast cancer cells
processed by 25 mg/l lovastatin was 23.6%, while TPX2
protein-positive rate of breast cancer cells in the control group
was 89.5%. Thus, processing with 25 mg/l lovastatin improved
radiotherapy sensitization significantly.
Discussion
As living standards improve and dietary habits
change, a significant rise in the incidence of breast cancer has
been recorded. Although theories on tumor stem cells have improved
knowledge on tumor cells, findings suggest new medical directions
(18). Breast cancer is a malignant
tumor and there is a possibility that incidence and cell migration
may occur following surgery. Therefore, treatment methods for
breast cancer have no obvious improvement yet, and it is imperative
that new treatment initiatives are identified. Advances in life
sciences with regard to treating cancer based on genetics has
gradually become a research focus (19).
TPX2 gene is a microtubule-associated
protein, and research in recent years has shown that it is closely
related with the development of multiple cancer cells (20) including breast cancer. Further,
radiotherapy has the ability to inhibit cancer cell proliferation
but is very cytotoxic. Therefore, seeking a TPX2
gene-targeted compound sensitizer for radiotherapy on breast cancer
may be an effective curative method that could alleviate associated
side effects. In the present study, we first explored the
relationship between TPX2 gene and breast cancer cells, then
used three broad-spectrum sensitizers to conduct radiotherapy in
vitro to identify the interactive relations between sensitizer
and TPX2 gene (21).
By analyzing the relationship between TPX2
gene and breast cancer cells, using western blot analysis and
RT-PCR, the present study revealed that TPX2 gene and
protein were hardly expressed in normal breast cells but were
expressed significantly more in all four types of breast cancer
cells. However, expressions in various breast cancer cells were not
significantly different. It showed that if TPX2 gene and
protein were detected in breast cells, malignant pathological
changes could probably exist. This experiment also investigated
TPX2 protein expression in breast cancer cells at various
differentiation stages and found that TPX2 protein expression
increased significantly along with the increase in differentiation
stages, which further indicated TPX2 gene is closely related
to the development and deteriorating severity of breast tumor
cells. Moreover, monitoring TPX2 gene expression in tumor
tissues could evaluate tumor severity and prove useful in the
prediction and prognostic treatment of the disease.
After confirming the relationship between
TPX2 gene and breast cancer stem cells, the present study
selected three kinds of broad-spectrum sensitizers, docetaxel,
lovastatin and β-santalene in threatment with breast cancer cells
by conducting radiotherapy in vitro. This experiment
compared three kinds of sensitizers and found that docetaxel and
lovastatin had little cytotoxicity when no radiotherapy was
conducted, while lovastatin had the strongest sensitizing effects
and the highest cell apoptotic rate. Therefore, lovastatin was
chosen as the sensitizer of radiotherapy for breast cancer. Further
effects of lovastatin at different concentrations on radiotherapy
were investigated and it was found that the cell apoptotic rate was
the highest at 25 mg/l concentration. Since association between
TPX2 gene and breast tumor stem cells have been confirmed
and lovastatin has significant sensitizing radiotherapy effects on
breast tumor stem cells, our research group suspected that
lovastatin affects TPX2 gene expression to increase the
death rate of cancer cells. However, further investigation is
required.
Acknowledgements
This study was supported by the Medical Science and
Technology Research of Guangdong Province (no. A2015033).
References
|
1
|
Sankaranarayanan R and Swaminathan R:
Cancer Survival in Africa, Asia, the Caribbean and Central America.
162. IARC Scientific Publications; Lyon: pp. 23–31. 2011
|
|
2
|
Li Y, Burns JA, Cheney CA, Zhang N,
Vitelli S, Wang F, Bett A, Chastain M, Audoly LP and Zhang ZQ:
Distinct expression profiles of Notch-1 protein in human solid
tumors: implications for development of targeted therapeutic
monoclonal antibodies. Biologics. 24:163–171. 2010.
|
|
3
|
Leong SP, Shen ZZ, Liu TJ, Agarwal G,
Tajima T, Paik NS, Sandelin K, Derossis A, Cody H and Foulkes WD:
Is breast cancer the same disease in Asian and Western countries?
World J Surg. 34:2308–2324. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Matsuda T, Marugame T, Kamo K, Katanoda K,
Ajiki W and Sobue T; Japan Cancer Surveillance Research Group, :
Cancer incidence and incidence rates in Japan in 2004: based on
data from 14 population-based cancer registries in the Monitoring
of Cancer Incidence in Japan (MCIJ) Project. Jpn J Clin Oncol.
40:1192–1200. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Matsuda T, Marugame T, Kamo K, Katanoda K,
Ajiki W and Sobue T; Japan Cancer Surveillance Research Group, :
Cancer incidence and incidence rates in Japan in 2005: based on
data from 12 population-based cancer registries in the Monitoring
of Cancer Incidence in Japan (MCIJ) project. Jpn J Clin Oncol.
41:139–147. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zorba A, Buosi V, Kutter S, Kern N,
Pontiggia F, Cho YJ and Kern D: Molecular mechanism of Aurora A
kinase autophosphorylation and its allosteric activation by TPX2.
eLife. 3:e026672014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Petry S, Groen AC, Ishihara K, Mitchison
TJ and Vale RD: Branching microtubule nucleation in Xenopus egg
extracts mediated by augmin and TPX2. Cell. 152:768–777. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Scholz C and Wagner E: Therapeutic plasmid
DNA versus siRNA delivery: common and different tasks for synthetic
carriers. J Control Release. 161:554–565. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Silva SM, Moreira HC and Canavarro MC:
Examining the links between perceived impact of breast cancer and
psychosocial adjustment: the buffering role of posttraumatic
growth. Psychooncology. 21:409–418. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cohen M and Numa M: Posttraumatic growth
in breast cancer survivors: a comparison of volunteers and
non-volunteers. Psychooncology. 20:69–76. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
O'Shaughnessy J, Osborne C, Pippen JE,
Yoffe M, Patt D, Rocha C, Koo IC, Sherman BM and Bradley C:
Iniparib plus chemotherapy in metastatic triple-negative breast
cancer. N Engl J Med. 36:205–214. 2011. View Article : Google Scholar
|
|
12
|
Shimura T, Takenaka Y, Fukumori T,
Tsutsumi S, Okada K, Hogan V, Kikuchi A, Kuwano H and Raz A:
Implication of galectin-3 in Wnt signaling. Cancer Res.
65:3535–3537. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gürtler A, Kunz N, Gomolka M, Hornhardt S,
Friedl AA, McDonald K, Kohn JE and Posch A: Stain-Free technology
as a normalization tool in Western blot analysis. Anal Biochem.
433:105–111. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Elbers A, Meiswinkel R, van Weezep E, van
Oldruitenborgh-Oosterbaan M Sloet and Kooi B: Schmallenberg virus
detected by RT-PCR in Culicoides biting midges captured during the
2011 epidemic in the Netherlands. Emerg Infect Diseases.
433:105–111. 2013.
|
|
15
|
Vollebergh MA, Jonkers J and Linn SC:
Genomic instability in breast and ovarian cancers: translation into
clinical predictive biomarkers. Cell Mol Life Sci. 69:223–245.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tutt A, Robson M, Garber JE, Domchek SM,
Audeh MW, Weitzel JN, Friedlander M, Arun B, Loman N, Schmutzler
RK, et al: Oral poly(ADP-ribose) polymerase inhibitor olaparib in
patients with BRCA1 or BRCA2 mutations and advanced breast cancer:
a proof-of-concept trial. Lancet. 376:235–244. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Blanco I, Kuchenbaecker K, Cuadras D, Wang
X, Barrowdale D, de Garibay GR, Librado P, Sánchez-Gracia A, Rozas
J, Bonifaci N, et al: Assessing associations between the
AURKA-HMMR-TPX2-TUBG1 functional module and breast cancer risk in
BRCA1/2 mutation carriers. PLoS One. 10:e1200202016.
|
|
18
|
Neumayer G, Belzil C, Gruss OJ and Nguyen
MD: TPX2: of spindle assembly, DNA damage response, and cancer.
Cell Mol Life Sci. 71:3027–3047. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hsu HT, Dodd MJ, Guo SE, Lee KA, Hwang SL
and Lai YH: Predictors of exercise frequency in breast cancer
survivors in Taiwan. J Clin Nurs. 20:1923–1935. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Newlaczyl AU and Yu LG: Galectin-3 - a
jack-of-all-trades in cancer. Cancer Lett. 313:123–128. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
McGuire R, Waltman N and Zimmerman L:
Intervention components promoting adherence to strength training
exercise in breast cancer survivors with bone loss. West J Nurs
Res. 33:671–689. 2011. View Article : Google Scholar : PubMed/NCBI
|