Introduction
Granulocyte-colony stimulating factor (G-CSF) is a
cytokine produced mainly by macrophages, fibroblasts and
endothelial cells, which functions to induce maturation and
proliferation of the precursor of neutrophils in the bone marrow
and recruit them into the periphery (1). Production of G-CSF by non-hematological
malignant cells is rarely observed. G-CSF-producing cancers have
been reported in the lung, digestive organs and urinary bladder
(2). The histological types of
G-CSF-producing gastric cancers are often poorly differentiated
carcinoma and undifferentiated carcinoma (3). In addition, G-CSF-producing tumors
generally show an aggressive clinical course and poor
prognosis.
Neoplasms of the various organs with neuroendocrine
features have been recognized as neuroendocrine tumors (NETs), and
their annual age-adjusted incidence was reported to be ~5 per
100,000 individuals (4).
Neuroendocrine carcinoma (NEC) is a type of NET, which shows a
pathologically high proliferation rate. NEC encompasses small cell
NEC and large cell NEC (5). Small
cell lung carcinoma (SCLC) is the most frequently identified type
of NEC, and 33% of extrapulmonary small cell carcinomas have been
reported to be of gastrointestinal origin (6). Since the standard treatment of
extrapulmonary NECs (EPNECs) including gastric NECs has not been
established, platinum-based combination chemotherapies are commonly
selected, since the clinicopathological features of EPNECs are
similar to those of SCLC (7).
However, treatment effectiveness is limited, and the prognosis of
EPNEC is poor. The median survival of patients with
gastrointestinal NEC has been reported to be ~13 months (8).
There are a limited number of studies describing
G-CSF-producing NECs (9,10), and to the best of our knowledge, no
G-CSF-producing advanced gastric NECs have been reported. Since the
chemotherapy regimen for NEC may be affected by a high serum G-CSF
concentration, careful supportive therapy is required. The present
study presents the case of a male with a G-CSF-producing advanced
gastric NEC, which was expected to have an aggressive clinical
course. The patient was successfully treated with chemotherapy
along with an appropriate supportive therapy.
Case presentation
A 67-year-old male with bloody emesis and black
stools was referred by a physician to the Department of Hematology
and Oncology, Kyushu University Hospital (Fukuoka, Japan) in April
2015. The patient had a history of smoking for 47 years and
hypertension. The patient's temperature was 37.0°C when he was
referred. The other vital signs of the patient were within normal
limits, and his Eastern Cooperative Oncology Group (ECOG)
performance status was 1. Upon physical examination, the bulbar
conjunctiva appeared anemic. The laboratory results were as
follows: White blood cells (WBC), 25,190/µl (neutrophils 90.8%,
lymphocytes 3.3%, monocytes 4.9%, eosinophils 0.3% and basophils of
0.3%; normal levels: WBC 3300-8600/ml, neutrophils 40–70%,
lymphocytes 18–53%, monocytes 2–12%, eosinophils 1–4%, and
basophils 0–1%); hemoglobin, 9.3 g/dl (normal level 13.7–16.8
g/dl); platelets, 23.5×104/µl (normal level
15.8–34.8×104/µl); C-reactive protein (CRP), 11.21 mg/ml
(normal level <0.14 mg/ml); lactate dehydrogenase, 348 IU/l
(normal level 124–222 IU/l); neuron specific enolase (NSE), 75.3
ng/ml (normal level <15.1 ng/ml); pro-gastrin-releasing peptide
(Pro-GRP), 54.4 pg/ml (normal level <81.0 pg/ml); and
carcinoembryonic antigen 15.9 ng/ml (normal level <3.2 ng/ml).
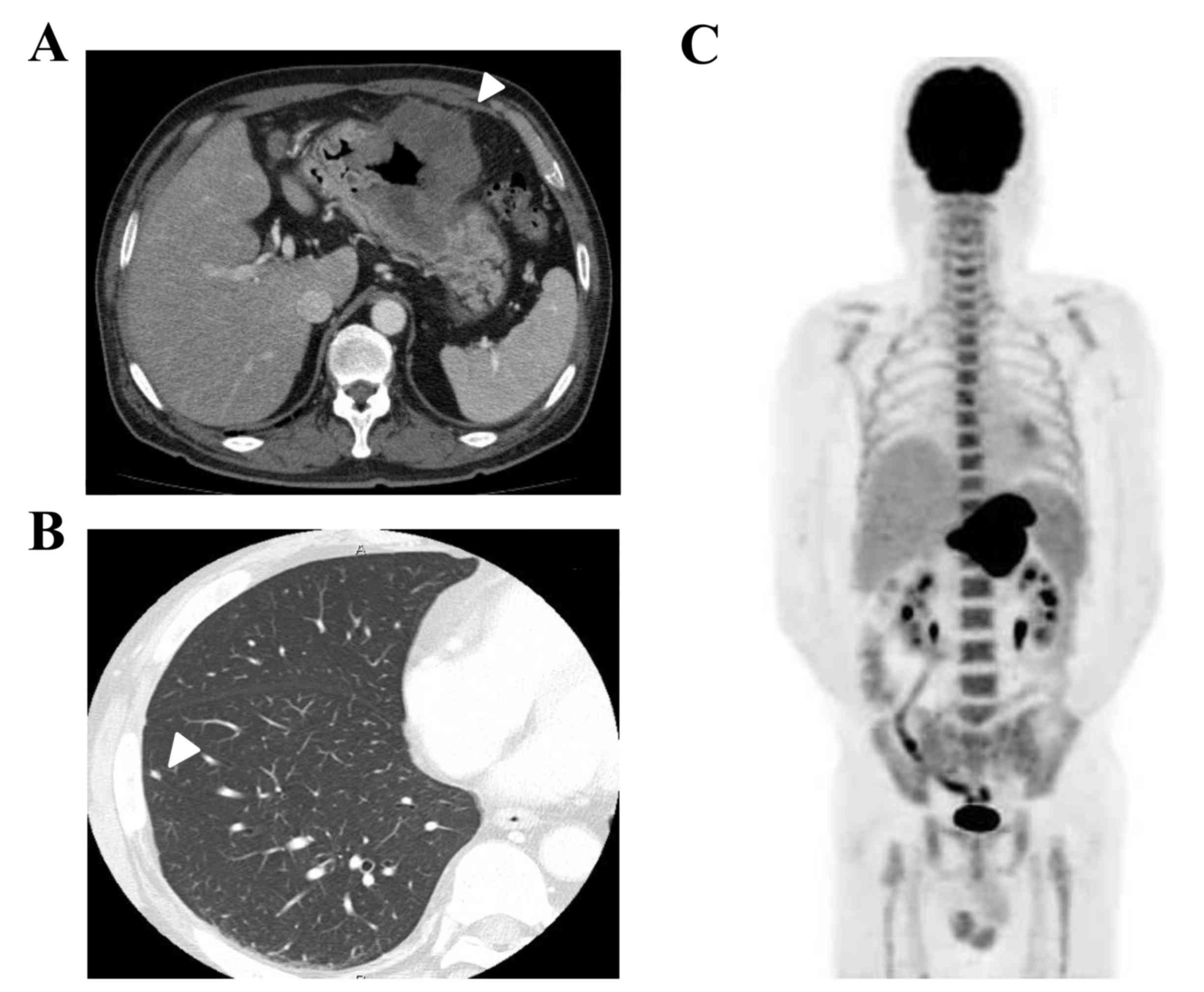
Liver and renal function was within normal limits. Computed
tomography (CT) demonstrated that the gastric tumor had directly
invaded the transverse colon, and perigastric lymph node swelling
was also observed (Fig. 1A). Several
small nodules in the lungs were also identified, which were
suggested to be metastatic tumors rather than primary lung tumors
(Fig. 1B).
Fluorodeoxyglucose-positron emission tomography (FDG-PET)/CT
scanning also revealed metabolically active lesions in the stomach
and lymph nodes, and bones of the spine, scapulae, ribs, pelvis and
femur, however it was negative for the multiple lung nodules
(Fig. 1C). Bone marrow aspiration
revealed hypercellular bone marrow with no malignant features. The
WBC count increased gradually, but neither symptom nor medical
finding suggesting infectious diseases was observed. Elevation of
the serum G-CSF concentration (105 pg/ml; normal level <38
pg/ml) was thought to be the possible cause of the leukocytosis and
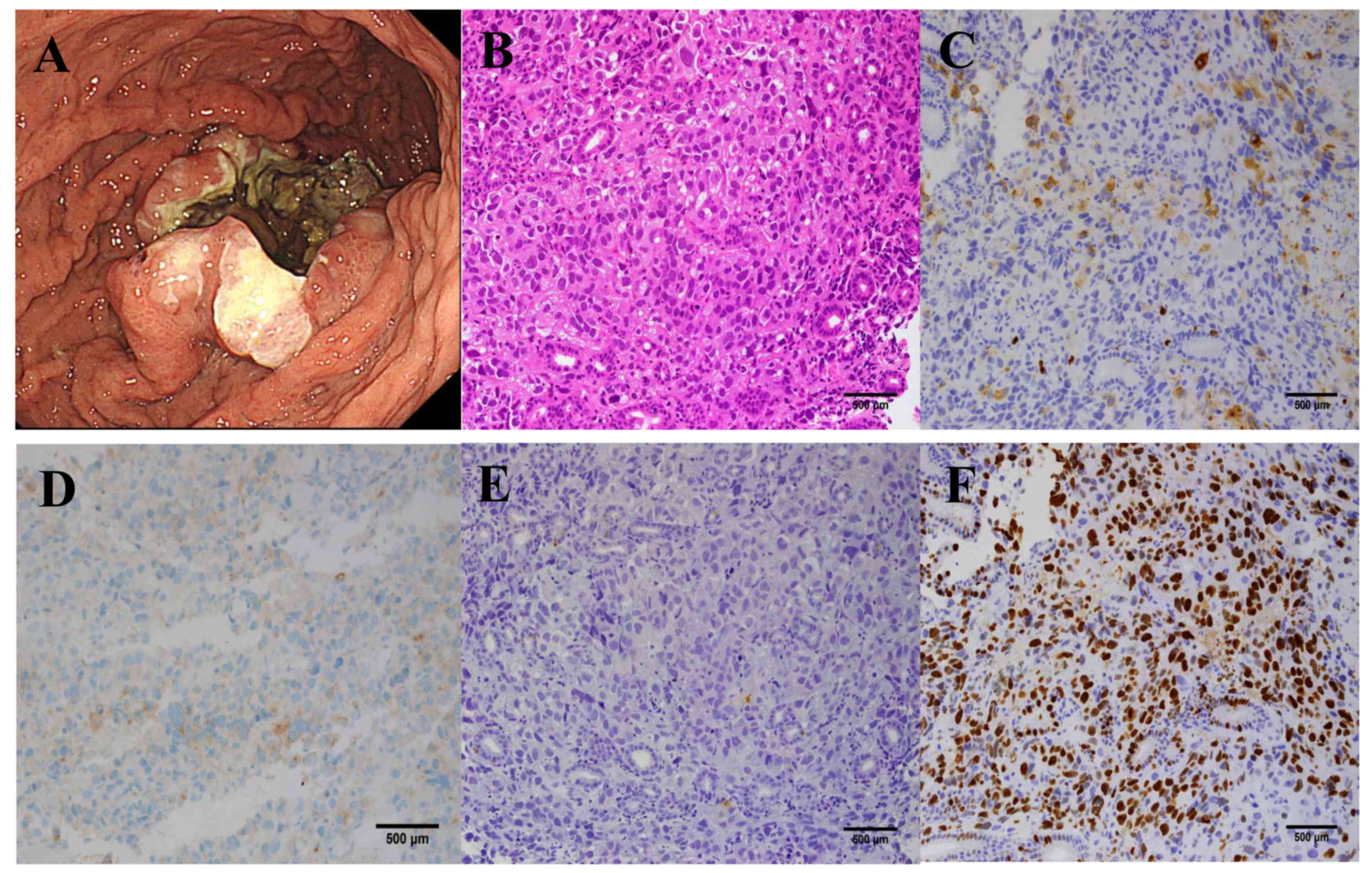
serum CRP elevation. Upper gastrointestinal endoscopy revealed an
ulcerating tumor in the middle of the stomach, which was similar to
a primary epithelial tumor (Fig. 2A).
Light microscopic examination of the endoscopic biopsy specimen
from the gastric tumor was fixed by 10% formalin neutral buffer for
24 h at room temperature and stained with hematoxylin and eosin
that revealed proliferation of carcinoma cells arranged in a
sheet-like pattern (Fig. 2B).
Immunohistochemical analyses demonstrated that these tumor cells
were positive for synaptophysin (Fig.
2C) and CD56, focally positive for G-CSF (Fig. 2D), but negative for chromogranin A
(Fig. 2E), indicating the presence of
a neuroendocrine tumor. The MIB-1 labeling index was 70% (Fig. 2F). The final diagnosis was a
G-CSF-producing neuroendocrine carcinoma (NEC) (T4bN2M1PUL,
clinical stage IV).
Since the tumors were unlikely to be curatively
resectable, systemic chemotherapy consisting of cisplatin (60
mg/m2, day 1, every 28 days) and irinotecan (60
mg/m2, days 1, 8 and 15, every 28 days) was started in
May 2015. Tumor lysis syndrome (TLS) of common terminology criteria
for adverse events (CTCAE) grade 3 in association with hyperkalemia
and hyperuricemia appeared 4 days subsequent to the initiation of
chemotherapy. TLS improved with a large infusion of normal saline.
Grade 4 neutropenia appeared on day 7 and agranulocytosis appeared
on day 11. Grade 4 neutropenia lasted for 10 days even with
intensive G-CSF administration. Grade 3 febrile neutropenia was
also observed, and the patient was treated with antibiotic and
antimycotic drugs. Other severe adverse events experienced were
grade 3 anemia, thrombocytopenia, fatigue and loss of appetite. Due
to these adverse events, the administration of cisplatin and
irinotecan on day 8 and 15 was stopped. The method of dose
reduction followed the standard therapy for small cell lung cancer
(11). The WBC count (2,610/µl) and
serum G-CSF concentration (13.7 pg/ml) decreased to within normal
limits prior to the beginning of the second cycle of
chemotherapy.
The doses of cisplatin and irinotecan in the second
cycles were decreased to 50 mg/m2, and were not
administered on day 15. Grade 4 neutropenia appeared on day 21,
however it recovered immediately. No tumor lysis syndrome occurred,
however grade 2 vomiting was observed. The doses of cisplatin and
irinotecan in the third cycles were decreased additionally to 40
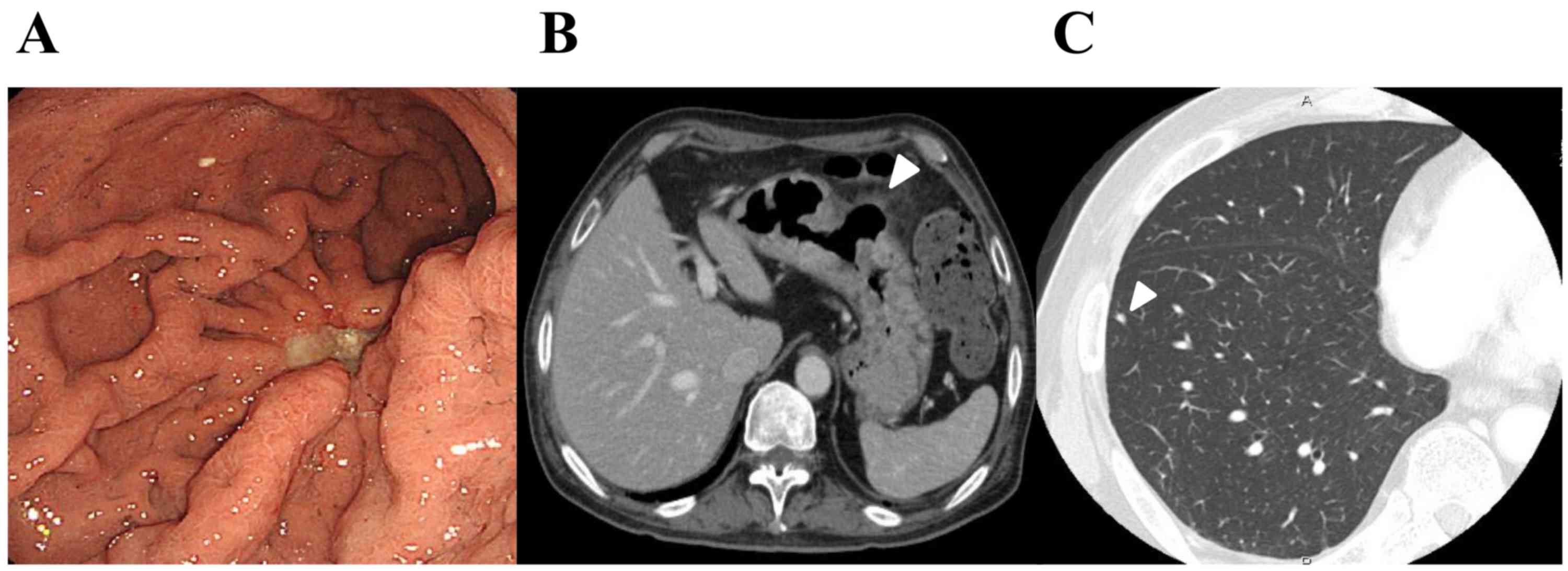
mg/m2. Subsequent to 3 cycles of chemotherapy, the
general condition of the patient improved markedly, and
gastrointestinal endoscopy (Fig. 3A)
and CT (Fig. 3B) demonstrated
remarkable shrinkage of the primary gastric tumor in association
with the penetration of the gastric wall at the ulcerative tumor.
Lymph nodes were also reduced in size, however no marked change was
observed in the lung nodules, suggesting that these were
non-tumorous lesions (Fig. 3C). The
patient underwent laparoscopic total gastrectomy with regional
lymph adenectomy and partial resection of the transverse colon for
curative intent in September 2015. Histological examination of the
resected specimens revealed that the ulcerative residual tumor was
composed of proliferating viable carcinoma cells with transmural
fibrosis, necrosis and clear-cell degeneration, involving the whole
thickness of gastric wall and invading around the adipose tissue,
accompanied by a healed ulcer. Subsequent to recovery from the
surgery, adjuvant chemotherapy with the same regimen is planned. A
chest CT scan performed 3 months subsequent to total gastrectomy
revealed no significant differences in the sizes of lung
nodules.
Discussion
G-CSF-producing malignant solid tumors are not
common, however G-CSF-producing tumors originating from lung,
digestive organs and other organs have been reported (2). Leukocytosis, increased serum G-CSF
concentrations, decreased leukocytes subsequent to surgery for the
primary tumor, and positivity for G-CSF on immunohistochemical
examination of tumor cells have been used as criteria for
G-CSF-producing tumors (12). The
present patient also exhibited some of these features and was
diagnosed as an advanced G-CSF-producing gastric NEC.
The prognosis of G-CSF-producing tumors has
generally been thought to be poor, however the reasons for this are
unclear. One possible explanation is the autocrine loop of
G-CSF/G-CSF receptors on the tumor cells. G-CSF-producing tumor
cells may be stimulated via their own G-CSF receptors, and can also
produce several types of cytokines including interleukin (IL)-6
(13), IL-1β, and TNF-α, which
function to enhance tumor cell growth (14). Additionally, G-CSF can promote tumor
growth by enhancing angiogenesis (15). Since a G-CSF-producing nature tended
to be observed in poorly differentiated cancers, this histological
feature may be associated with the poor prognosis of
G-CSF-producing tumors.
Tumors with neuroendocrine features with a
gastrointestinal origin have been diagnosed based on various
nomenclatures. Since the World Health Organization (WHO)
nomenclature published in 2010 is widely used, the present case was
diagnosed according to it (5). NECs,
including those of gastrointestinal origin, have been thought to be
relatively sensitive to systemic chemotherapies (16). Yamaguchi et al (8) examined 154 patients with advanced
gastrointestinal NECs treated with first-line chemotherapy, and
demonstrated that each treatment, irinotecan plus cisplatin (IP)
and etoposide plus cisplatin, demonstrated equivalent efficacy with
respect to the response rate (51 vs. 75%), median PFS (5.4 vs. 4.9
months), and median OS (13.4 vs. 14.0 months) (8).
The present study identified four reports of
G-CSF-producing neuroendocrine tumors in the literature (Table I). All cases demonstrated leukocytosis
and high serum G-CSF concentrations. Immunohistochemical
examinations were performed in two patients (with esophageal and
cervical cancer), whereas the other two patients were diagnosed
without immunohistochemical analyses as having large cell lung
cancer (9,10,17,18).
Multidisciplinary therapy for these patients was tried, however
long-term survival data were not provided. No severe adverse events
in association with the systemic chemotherapies were reported,
including severe neutropenia and tumor lysis syndrome. Since there
are no reports of G-CSF-producing advanced gastric NECs, the
present report is the first to demonstrate the effect of systemic
chemotherapy for this disease. The patient was treated with the
same IP regimen as for extended disease of small cell lung cancer
(11). A favorable response was
achieved, and the patient underwent surgery for curative
intent.
 | Table I.G-CSF-producing neuroendocrine tumors
in the literature. |
Table I.
G-CSF-producing neuroendocrine tumors
in the literature.
| Age/sex | Primary site | Stage | Histology | WBC (/ul) | G-CSF (ng/ml) | Treatment | Chemotherapy
regimen | (Refs.) |
|---|
| 79 M | Esophagus | T3N2M0, Stage
III | Small cell
carcinoma | 15,180 | 52.4 | CRT | VP-16+CDDP | (9) |
| 70 F | Uterine cervix | Stage IVb | Small cell
carcinoma | 17,100 | 268 | CTx, RTx | CAJ, 5-FU | (10) |
| 41 M | Lung | T3N0M0, Stage
IIIA | Large cell
carcinoma | 38,400 | 105 | CTx, Surgery | CDDP+VDS | (17) |
| 46 M | Lung | T2N0M0, Stage IB | Large cell
carcinoma | 40,400 | 318 | Surgery, Adjuvant
CTx | CBDCA+PTX,
Gefitinib | (18) |
| 67 M | Stomach | T4bN2M1, Stage
IV | Small cell
carcinoma | 25,190 | 105 | CTx, Surgery | CPT-11+CDDP | Present case |
TLS is common in hematological malignancies, however
is rare in patients with solid tumors. Among solid tumors, TLS has
been reported in association with small cell lung cancer. However,
TLS cases are rare in patients who are diagnosed with
extrapulmonary NEC (EPNEC) or extrapulmonary small cell carcinoma.
Therefore, differences of the incidence and the clinical features
of TLS between small cell lung cancer and EPNEC remain unclear.
Tumors with susceptibility to TLS are thought to be those with
rapid growth, a large tumor and sensitivity to chemotherapy.
Elevation of serum uric acids, phosphate and creatinine,
dehydration, hypotension and drugs affecting renal function are
also risk factors of TLS (19). In
the present case, specific features of the tumor may influence the
occurrence of TLS. The increased concentration of G-CSF produced by
tumor cells induces over-proliferation of granulocytes in the bone
marrow and peripheral leukocytosis. Systemic chemotherapy during
the condition in which neutrophils are greatly increased by G-CSF
has been theoretically recognized to enhance bone marrow
suppression due to damaging myeloid progenitor cells (20). Therapeutic use of G-CSF products is
required within 24 h after the chemotherapy to avoid enhanced bone
marrow suppression (21). However, it
was unclear whether chemotherapy for patients with continuously
increased serum G-CSF concentrations could induce similar effects
(20). No reports of G-CSF-producing
tumor patients who suffered from severe neutropenia were
identified. Notably, the present case demonstrated prominent
adverse events induced by the systemic chemotherapy and required
intensive supportive therapies. One of the possible reasons for the
severe adverse events in the patient in the present case report may
be a feature of the IP regimen, which tended to induce bone marrow
suppression. A phase III clinical study for small cell lung cancer
revealed that 25% of patients treated with the IP regimen exhibited
CTCAE grade 4 neutropenia (11). The
timing of chemotherapy in the condition of enhanced hematopoiesis
by tumor-producing G-CSF and this feature of the IP regimen may be
associated with the occurrence of serious adverse events in this
patient.
At the onset of the severe neutropenia, C-GSF was
intensively administered for therapeutic use. Since the serum G-CSF
concentration at the point was not measured, it is not clear
whether enough amount of intrinsic G-CSF remained to improve the
neutropenia and the administered G-CSF was actually effective.
The gastric tumor of the present patient was
resected subsequent to chemotherapy since the lung nodules were
finally suggested to be non-tumorous lesions. Efficacy of
conversion surgery may theoretically be expected in cases which
demonstrate a high response rate of chemotherapy and possess
limited metastatic sites. Additionally, efficacy of this strategy
differs between the types of tumor. While conversion surgery could
be one of the therapeutic strategies in colorectal cancer, the
clinical meaning of it was not recognized in gastric cancer. Since
favorable data of conversion surgery for gastric cancer has been
accumulated, clinical studies assessing the efficacy of conversion
surgery are ongoing (22). It remains
unclear whether conversion surgery can be a standard therapy of
EPNEC.
The present study demonstrated clear adverse events
and favorable efficacy of systemic chemotherapy in a
G-CSF-producing advanced gastric NEC patient. Since certain
G-CSF-producing tumor patients may exhibit profound bone marrow
suppression, as in the present case, careful observation and
intensive supportive therapy are required.
References
|
1
|
Demetri GD and Griffin JD: Granulocyte
colony-stimulating factor and its receptor. Blood. 78:2791–2808.
1991.PubMed/NCBI
|
|
2
|
Kojima K, Nakashima F, Boku A, Muroishi Y,
Nakanishi I and Oda Y: Clinicopathological study of involvement of
granulocyte colony stimulating factor and granulocyte-macrophage
colony stimulating factor in non-lymphohematopoietic malignant
tumors accompanied by leukocytosis. Histol Histopathol.
17:1005–1016. 2002.PubMed/NCBI
|
|
3
|
Kawaguchi M, Asada Y, Terada T, Takehara
A, Munemoto Y, Fujisawa K, Mitsui T, Iida Y, Miura S and Sudo Y:
Aggressive recurrence of gastric cancer as a granulocyte-colony
stimulating factor-producing tumor. Int J Clin Oncol. 15:191–195.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yao JC, Hassan M, Phan A, Dagohoy C, Leary
C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A and Evans
DB: One hundred years after ‘carcinoid’: epidemiology of and
prognostic factors for neuroendocrine tumors in 35,825 cases in the
United States. J Clin Oncol. 26:3063–3072. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bosman FT, Cameiro F, Hruban RH and Theise
ND: WHO classification of tumors of the digestive system. 4th. WHO
Press; Geneva: pp. 13–14. 2010
|
|
6
|
Wong YN, Jack RH, Mak V, Henrik M and
Davies EA: The epidemiology and survival of extrapulmonary small
cell carcinoma in South East England, 1970–2004. BMC Cancer.
9:2092009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kulke MH, Shah MH, Benson AB III,
Bergsland E, Berlin JD, Blaszkowsky LS, Emerson L, Engstrom PF,
Fanta P, Giordano T, et al: Neuroendocrine tumors, version 1.2015.
J Natl Compr Canc Netw. 13:78–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yamaguchi T, Machida N, Morizane C, Kasuga
A, Takahashi H, Sudo K, Nishina T, Tobimatsu K, Ishido K, Furuse J,
et al: Multicenter retrospective analysis of systemic chemotherapy
for advanced neuroendocrine carcinoma of the digestive system.
Cancer Sci. 105:1176–1181. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sato Y, Takahashi Y, Nishiie K, Okubo S,
Fujikaw K, Shintani N, Takada K, Sato Y, Takimoto R, Kato J and
Niitsu Y: A case of granulocyte-colony stimulating factor producing
small cell carcinoma of esophagus. Nihon Shokakibyo Gakkai Zasshi.
102:888–893. 2005.(In Japanese). PubMed/NCBI
|
|
10
|
Watanabe A, Wachi T, Omi H, Nishii H,
Ochiai K, Tanaka T and Endo Y: Granulocyte colony-stimulating
factor-producing small-cell carcinoma of the uterine cervix: Report
of a case. Diaqn Cytopathol. 23:269–274. 2000. View Article : Google Scholar
|
|
11
|
Noda K, Nishiwaki Y, Kawahara M, Negoro S,
Sugiura T, Yokoyama A, Fukuoka M, Mori K, Watanabe K, Tamura T, et
al: Irinotecan plus cisplatin compared with etoposide plus
cisplatin for extensive small-cell lung cancer. N Engl J Med.
346:85–91. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Asano S, Urabe A, Okabe T, Sato N and
Kondo Y: Demonstration of granulopoietic factor(s) in the plasma of
nude mice transplanted with a human lung cancer and in the tumor
tissue. Blood. 49:845–852. 1977.PubMed/NCBI
|
|
13
|
Tsuyuoka R, Takahashi T, Sasaki Y,
Taniguchi Y, Fukumoto M, Suzuki A, Nakamura K, Kobayashi S, Kudo T
and Nakao K: Colony-stimulating factor-producing tumours:
Production of granulocyte colony-stimulating factor and
interleukin-6 is secondary to interleukin-1 production. Eur J
Cancer. 30A:2130–2136. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Matsumoto M, Nakayama T, Inoue D,
Takamatsu K, Itotani R, Ishitoko M, Suzuki S, Sakuramoto M, Yuba Y,
Yoshie O, et al: A pleomorphic carcinoma of the lung producing
multiple cytokines and forming a rapidly progressive mass-like
opacity. BMC Cancer. 14:5882014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Morales-Arias J, Meyers PA, Bolontrade MF,
Rodriguez N, Zhou Z, Reddy K, Chou AJ, Koshkina NV and Kleinerman
ES: Expression of granulocyte-colony-stimulating factor and its
receptor in human Ewing sarcoma cells and patient tumor specimens:
Potential consequences of granulocyte-colony-stimulating factor
administration. Cancer. 110:1568–1577. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Moertel CG, Kvols LK, O'Connell MJ and
Rubin J: Treatment of neuroendocrine carcinomas with combined
etoposide and cisplatin. Evidence of major therapeutic activity in
the anaplastic variants of these neoplasms. Cancer. 68:227–232.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Teramachi M, Miyamoto N, Yamamoto Y,
Sasaka T, Nakamura T and Kitamura F: A case of large cell carcinoma
of the lung which is suspected of producing granulocyte
colony-stimulating factor. Nihon Kyobu Shikkan Gakkai Zasshi.
30:1327–1332. 1992.(In Japanese). PubMed/NCBI
|
|
18
|
Hasegawa S, Suda T, Negi K and Hattori Y:
Lung large cell carcinoma producing granulocyte-colony-stimulating
factor. Ann Thorac Surg. 83:308–310. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gemici C: Tumor lysis syndrome in solid
tumors. Clin Oncol (R Coll Radiol). 18:773–780. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Amadori S, Suciu S, Jehn U, Stasi R,
Thomas X, Marie JP, Muus P, Lefrère F, Berneman Z, Fillet G, et al:
Use of glycosylated recombinant human G-CSF (lenograstim) during
and/or after induction chemotherapy in patients 61 years of age and
older with acute myeloid leukemia: Final results of AML-13, A
randomized phase-3 study. Blood. 106:27–34. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Burris HA, Belani CP, Kaufman PA, Gordon
AN, Schwartzberg LS, Paroly WS, Shahin S, Dreiling L and Saven A:
Pegfilgrastim on the same day versus next day of chemotherapy in
patients with breast cancer, non-small-cell lung cancer, ovarian
cancer, and non-hodgkin's lymphoma: Results of four multicenter,
double-blind, randomized phase ii studies. J Oncol Pract.
6:133–140. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yoshida K, Yamaguchi K, Okumura N,
Tanahashi T and Kodera Y: Is conversion therapy possible in stage
IV gastric cancer: The proposal of new biological categories of
classification. Gastric Cancer. 19:329–338. 2016. View Article : Google Scholar : PubMed/NCBI
|