Introduction
Extramedullary plasmacytoma is a relatively rare
disease, characterized by a localized monoclonal plasma cell
proliferation, in the absence of demonstrable systemic involvement.
It comprises 5–10% of all plasma cell neoplasms. The most common
sites of involvement are in the head and neck, particularly the
upper respiratory tract (including the nasal cavity and the
nasopharynx, which by itself is a rare occurrence) (1). To date, the origin of this type of tumor
in chronic nasopharyngitis has not been described. Chronic
nasopharyngitis has resulted in increased populations of
eosinophils and has been associated with nasal polyps, allergic
rhinitis, asthma and/or aspirin sensitivity (2). Paraimmunoblastic transformation rarely
develops in chronic lymphocytic leukemia/small lymphocytic lymphoma
(CLL/SLL) (3).
The present study describes the simultaneous
occurrence of a nasopharyngeal extramedullary plasmacytoma with the
paraimmunoblastic transformation of a newly diagnosed small
lymphocytic lymphoma. An association between the two malignant
tumors is discussed.
Case report
A 78-year-old male was admitted to the emergency
room at the Soroka University Medical Center (Beer-Sheva, Israel)
in August, 2015, with dyspnea, dysarthria and nasal congestion. An
ear, nose and throat examination associated the symptoms with a
narrowing of the nasopharynx by a mass, bilateral tonsillar
enlargement and cervical and axillary lymphadenopathy. In addition,
a total body computed tomography (CT) scan revealed generalized
lymphadenopathy without hepatosplenomegaly. A nasopharyngeal biopsy
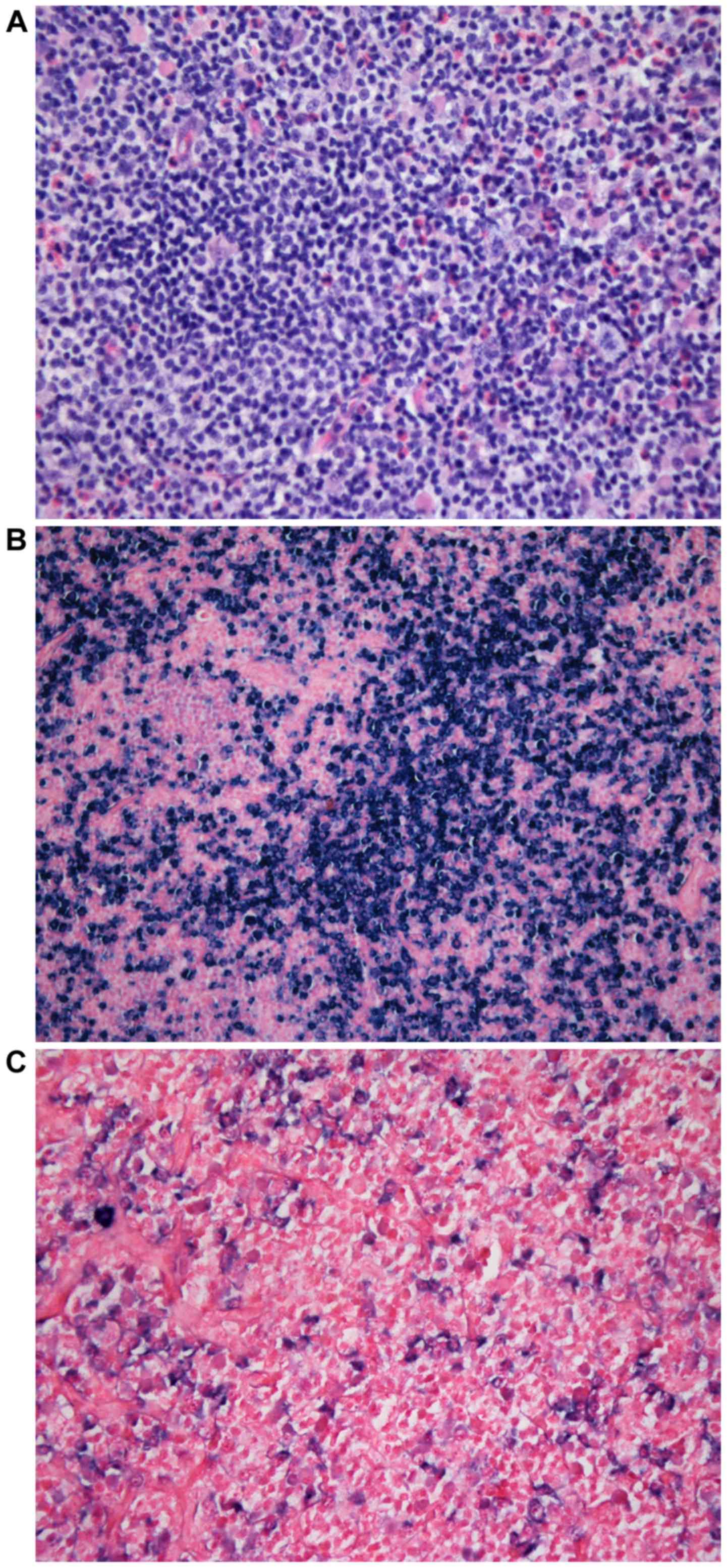
was performed under endoscopy in August, 2015. The tissue diagnosis
of a κ-light chain plasmacytoma, rich in eosinophils, was
established, as illustrated in Fig.
1A-C. Serum protein electrophoresis and immunofixation revealed
a monoclonal spike of Immunoglobulin (Ig)G-κ. A bone marrow
aspiration suggested a lymphoproliferative disorder, but no plasma
cells were present. Mild to moderate peripheral blood eosinophilia
had been present since 2003, but no allergic rhinitis, asthma,
nasal polyposis or aspirin sensitivity were detected. As an
immediate diagnosis of the nasopharyngeal lesion could not able be
made, a left axillary lymph node excision was performed in October
2015.
The clinical diagnosis of the nasopharyngeal mass
was based on an endoscopic examination of the nasopharynx and on a
CT scan. From the nasopharyngeal biopsy, two fragments of tissue
were obtained and the largest was 1.2×1 cm in size.
The histopathological diagnoses were based on
hematoxylin and eosin 5-µm-thick stained sections of formalin-fixed
paraffin-embedded tissue, according to standard protocols and
immunohistochemistry using a Ventana BenchMark XT (Ventana Medical
Systems, Tucson, AZ, USA). Immunostaining included cluster of
differentiation (CD) 45 (Dako; Agilent Technologies, Inc., Santa
Clara, CA, USA), CD20 (DakoAgilent Technologies, Inc), CD3 (Thermo
Fisher Scientific, Inc., Waltham, MA, USA), CD5 (Novocastra; Leica
Microsystems GmbH, Wetzlar, Germany), CD30 (DakoAgilent
Technologies, Inc), CD15 (DakoAgilent Technologies, Inc.), CD23
(Novocastra; Leica Microsystems GmbH), and Ki-67 (Thermo Fisher
Scientific, Inc.), alongside δ-(Cell Marque; Sigma-Aldrich; Merck
KGaA, Darmstadt, Germany) and κ-(Cell Marque; Sigma-Aldrich; Merck
KGaA) Ig light chains. In addition, Ig light chain RNA was studied
by in situ hybridization.
Histological examination using the Olympus BX41
microscope (Olympus, Tokyo, Japan) revealed that the tissue was
hypercellular with prominent plasma cells, a majority of which were
Mott cells. In addition, small to medium-sized lymphocytes,
numerous eosinophils and a number of scattered large lymphoid
cells, most probably immunoblasts, were identified.
The Mott cells and additional plasma cells were
κ-light chain monotypic: CD138 moderate (++) and CD20 negative (−).
The immunoblast immunostaining demonstrated a CD30 weak (+),
CD15−, melanoma-associated antigen (mutated) 1
(MUM1)+, B-cell-specific activator protein+
faint, Epstein-Barr virus (EBV)/latent membrane protein
1−, EBV-encoded small RNAs+ in a small number
of cells, fascin+, CD20+ and CD3−
profile. A nasopharyngeal extramedullary plasmacytoma was
diagnosed.
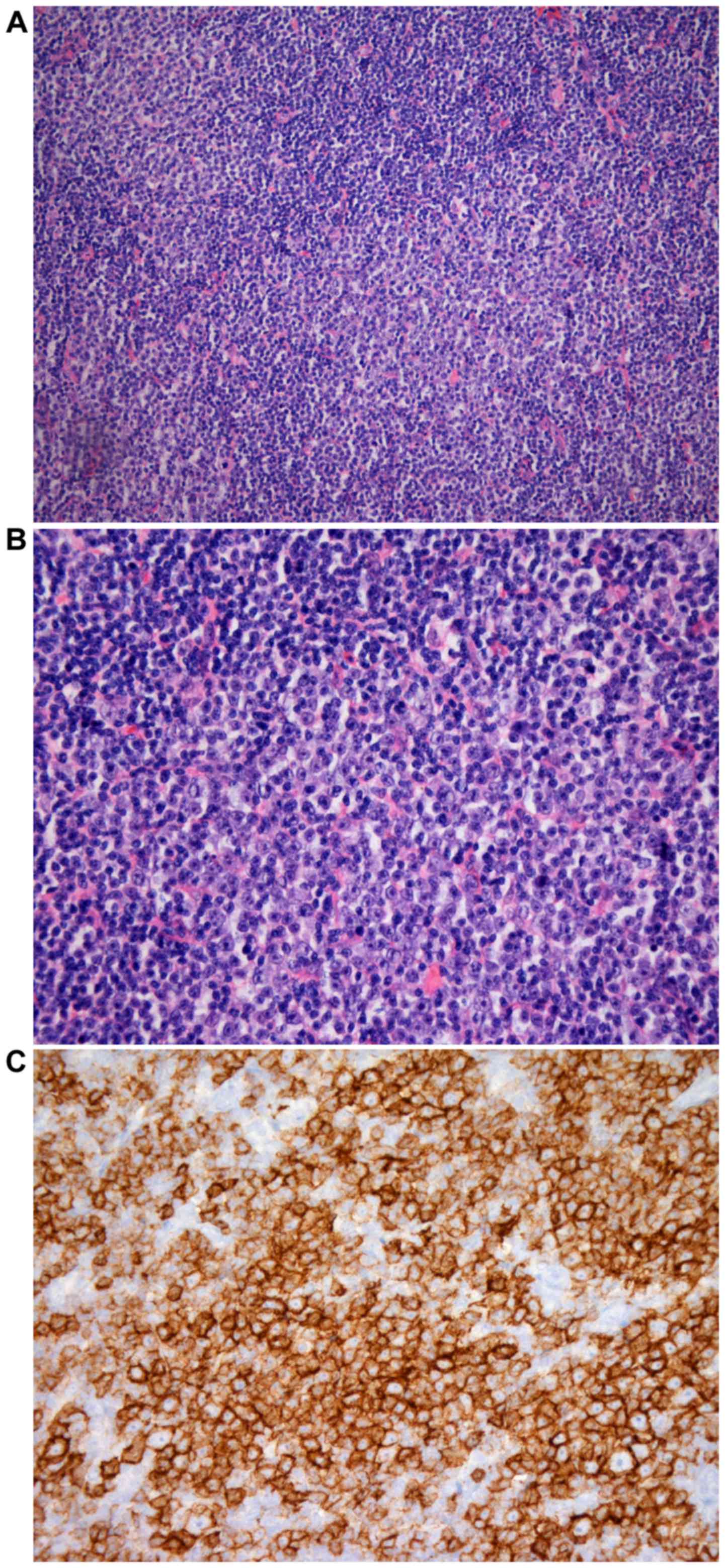
The lymph node biopsy suggested areas consistent
with the diagnosis of CLL/SLL with small round lymphocytes,
CD20+expression; CD5+ expression that was
>CD3+ expression levels and CD23++
expression levels. Proliferation centers were prominent and often
confluent. These areas contained almost exclusively a population of
medium to large-sized lymphoid cells with clear cytoplasm, a
vesicular and irregular nucleus and a small central eosinophilic
nucleolus with several admixed eosinophils. The larger lymphoid
cells exhibited strong (+++) expression levels of
LCA+++, CD20+++, CD23+++ and
CD5+++, which were >CD3+ expression, weak
and cellular expression of CD21+ and weak expression of
B-cell lymphoma 6+ and MUM1+. The
proliferation fraction of the proliferation centers (Ki-67) was
70%. The diagnosis of a variant paraimmunoblastic transformation of
CLL/SLL of the lymph node was made, as demonstrated in Fig. 2A-C. However, no clinical evidence for
CLL was present.
The bone marrow biopsy was normocellular for the age
of the patient. A near normal maturation of the hematopoietic
elements was evident. A small lymphocytic aggregate, with small
round lymphocytes, was isolated but was insufficient for the
diagnosis of CLL/SLL. No plasmacytosis was observed, which
confirmed the extramedullary nature of the plasmacytoma.
As the surgical resection was incomplete, the role
of adjuvant radiotherapy for the nasopharyngeal tumor was not
clear. However, radiotherapy was deemed necessary for the present
patient (4,5). The frequency and extent of the follow up
assessment in these types of cases depends on the patient and the
attending physician. During the visits, besides a physical
examination, serum protein electrophoresis and immunofixation, a
fiber optic endoscopy is recommended. Positron emission tomography
(PET)/CT or magnetic resonance imaging scans should be performed
twice a year.
Discussion
The present study describes the unusual report of an
elderly male patient who suffered simultaneously from a
nasopharyngeal extramedullary plasmacytoma, rich in Mott cells and
in eosinophils, synchronous with an axillary lymph node small
lymphocytic lymphoma with a variant paraimmunoblastic
transformation. No clinical or pathological evidence of multiple
myeloma, or clinical features of CLL were identified.
The lack of attention to the mild to moderate
peripheral blood eosinophilia diagnosed 12 years prior to admission
in the present patient may have delayed a diagnosis of chronic
nasopharyngitis. To this extent, the diagnoses of allergic
rhinitis, nasal polyps and aspirin hypersensitivity, individually
or in combination, may have been missed. Any of these diagnoses may
be associated with nasopharyngitis and are often rich in
eosinophils, and anyone of these disorders may have preceded the
extramedullary plasmacytoma at this unusual location (6–8).
The present patient had never previously presented
with symptoms of CLL, nor were signs of this condition detected.
The findings in the axillary lymph node were diagnostic of atypical
SLL, however the diagnosis of a transformation into
paraimmunoblastic lymphoma was favored due to the cytological
features of the larger cells, mainly located in the large
proliferation centers. This is an unusual form of progression of
SLL, particularly since the lymphoma was diagnosed for the first
time during the patients second admission. Additionally, the
nasopharyngeal plasmacytoma was identified shortly prior to the
lymph node biopsy, complicating the issue further. This occurrence
has been described in a small number of cases (9–11). In one
of these case reports, a patient with chronic lymphocytic leukemia
(CLL) revealed lymphadenopathy with evidence of an extramedullary
plasmacytoma. In a second case, CLL was complicated by a
plasmacytoma. A molecular study demonstrated that the plasmacytoma
was clonally different from the CLL. The authors of the third case
considered the composite tumor as transformation of CLL into
plasmacytoma. Notably, CLL/SLL with paraimmunoblastic
transformation has been reported previously (12), and has been retained as a provisional
entity of low-grade B-cell lymphoma (13).
An elderly patient is presented who initially
developed an extramedullary nasopharyngeal plasmacytoma rich in
eosinophils. Although no previous biopsy of this tissue was
performed, nor were allergic rhinitis or asthma diagnosed, this may
suggest chronic nasopharyngitis as the background of this
plasmacytoma. The rare occurrence of a synchronous
paraimmunoblastic transformation of small lymphocytic lymphoma was
diagnosed two weeks subsequent to this in an axillary lymph
node.
Acknowledgements
The authors would like to thank Kibbutz Sde-Boker,
Israel, for hosting them during the preparation of the
manuscript.
References
|
1
|
Chang YL, Chen PY and Hung SH:
Extramedullary plasmacytoma of the nasopharynx: A case report and
review of the literature. Oncol Lett. 7:458–460. 2014.PubMed/NCBI
|
|
2
|
Ichimura K, Sugimura H, Naito A and Maeda
Y: How to manage patients with hard to recognize postnasal drip?
Rhinology. 37:164–167. 1999.PubMed/NCBI
|
|
3
|
Kroft SH, Dawson DB and McKenna RW: Large
cell lymphoma transformation of chronic lymphocytic leukemia/small
lymphocytic lymphoma. A flow cytometry analysis of seven cases. Am
J ClinPathol. 115:385–395. 2001.
|
|
4
|
Creach KM, Foote RL, Neben-Wittich MA and
Kyle RA: Radiotherapy for extramedullary plasmacytoma of the head
and neck. Int J Radiat Oncol Biol Phys. 73:789–794. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tournier-Rangeard L, Lapeyre M,
Graff-Caillaud P, Mege A, Dolivet G, Toussaint B, Charra-Brunaud C,
Hoffstetter S, Marchal C and Peiffert D: Radiotherapy for solitary
extramedullary plasmacytoma in the head and neck region: A dose
greater than 45 Gy to the target volume improves the local control.
Int J Radiat Oncol Biol Phys. 64:1013–1017. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Horiguti S: Asthma and nasopharyngitis.
Allerg Immunol (Leipz). 20-21:1–425. 1975.
|
|
7
|
Obtulowicz K, Chlap Z and Olszewski E:
Bronchial asthma and pathological processes of the nasopharynx. I
Clinical analysis during remission and attack. Ann Allergy.
42:44–48. 1979.PubMed/NCBI
|
|
8
|
Rebhun J: A new approach to the treatment
of allergic nasopharyngitis. Ann Allergy. 39:175–178.
1977.PubMed/NCBI
|
|
9
|
Chantepie SP, Cabrera Q, Mear JB, Salaun
V, Lechapt-Zalcman E and Macro M: Unusual extramedullary
plasmacytoma: A rare but possible cause of lymphadenopathy in
chronic lymphocytic leukemia. Case Rep Med. 2015:6570492015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yahata N, Iwase O, Iwama H, Tauchi T,
Kawanishi Y, Serizawa H and Ohyashiki K: Chronic lymphocytic
leukemia complicated by plasmacytoma originating from different
clones. Leuk Lymphoma. 39:203–207. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pines A, Ben-Bassat I, Selzer G and Ramot
B: Transformation of chronic lymphocytic leukemia to plasmacytoma.
Cancer. 54:1904–1907. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chuang SS, Liao YL, Liou CP, Wiggins ML,
Ye H, Du MQ, Isaacson PG and Chang CC: Chronic lymphocytic leukemia
with paraimmunoblastic transformation - with comparative genomic
hybridization and review of the literature. Pathol Res Pract.
206:276–281. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sakata S, Tsuyama N and Takeuchi K:
Pathology of indolent B-cell neoplasms other than follicular
lymphoma. J Clin Exp Hematop. 54:11–22. 2014. View Article : Google Scholar : PubMed/NCBI
|