Introduction
Breast cancer is the most common type of malignancy
in women and the second most prevalent cause of tumor-associated
mortality worldwide. It is estimated that there were 234,190 new
cases and 40,730 mortalities due to breast cancer in 2015 (1–3). A number
of factors have been verified to contribute to the carcinogenesis
of breast cancer, including genetic alterations, epigenetic
alterations and environmental factors (4,5). The
progression of breast cancer is characterized by aggressive local
invasion, early metastasis, and a low sensitivity to chemotherapy
(6,7).
Metastasis is the complication that may occur the most often during
cancer and is the most prevalent cause of breast cancer-associated
mortality (8). Subsequent to surgery
and adjuvant treatment, 30–75% of breast cancer patients will
develop metastatic disease. Patients with metastatic breast cancer
have a median survival time of ~2 years following the diagnosis of
metastasis (9). The
invasion-metastasis cascade of breast cancer comprises multiple
steps, including local invasion, entry into the circulation,
arrival at distant secondary sites, extravasation and colonization
in distant organs (10–12). Therefore, further elucidation of the
molecular signaling cascades that control the metastasis of breast
cancer is urgent, and may provide new strategies to prevent breast
cancer metastasis.
MicroRNAs (miRNAs) are a group of small, non-coding
and endogenous RNAs of ~22 nucleotides that negatively regulate
gene expression in eukaryotes (13).
miRNAs exert their functions by binding to the 3′-untranslated
region (3′-UTR) of the targeted mRNAs, promoting mRNA degradation,
inhibiting mRNA translation, and affecting transcription (14,15). It
has been previously demonstrated that miRNAs control a wide range
of biological functions, participating in the processes of cell
differentiation, proliferation, apoptosis, cell cycle,
angiogenesis, metabolism, invasion and metastasis (16–18).
miRNAs are differentially expressed in a variety of tissues and
cells; therefore, they are important biomarkers and therapeutic
targets for numerous types of disease (19). Increasing evidence supports the
hypothesis that the alteration of miRNA expression may serve a
pivotal role in carcinogenesis and progression in numerous human
cancer types, including breast cancer (20–22). In
breast cancer, miRNAs may function as oncogenes (which are
expressed at higher levels in cancer and decrease the expression of
tumor suppressor genes) or as tumor suppressors (which are
downregulated in cancer and decrease the expression of oncogenes)
(23). Therefore, miRNAs may be novel
therapeutic targets for the treatment of breast cancer.
miR-452 has been reported to be abnormally expressed
in numerous types of human cancer (24–26).
However, no specific studies have been performed to reveal the
expression and biological roles underlying miR-452 in breast
cancer. The aim of the present study was to investigate the
expression level, biological roles and its underlying mechanism in
breast cancer. In the present study, significantly lower levels of
miR-452 were identified in breast cancer tissues compared with
paired normal breast tissues. In addition, the miR-452 expression
level was lower in breast cancer tissues from patients with
metastasis compared with the breast cancer tissue from patients
without metastasis. miR-452 was also downregulated in all examined
breast cancer lines. Induction of miR-452 expression suppressed
migration and invasion abilities in the cell lines. Further
analysis revealed that miR-452 decreased breast cancer cell
metastasis by directly targeting RAB11A.
Patients and methods
Patients and tissue samples
A total of 61 pairs of breast cancer tissues and
adjacent normal tissues were obtained from 3201 Hospital (Hanzhong,
Shaanxi, China). All patients included in the study had not
received chemotherapy or any other treatment prior to the surgery.
All tissues were snap frozen in liquid nitrogen immediately
following surgery, and stored in a −80°C freezer until they were
used. The present study was approved by the Ethics Committee of San
Er Ling Yi Hospital. Written informed consent was also obtained
from all patients enrolled in the present study.
Cell culture
Human breast cancer cells (MCF-7, BT-474,
MDA-MB-453, MDA-MB-231, SKBR3) and HEK293T cells were purchased
from American Type Culture Collection (Manassas, VA, USA). A normal
mammary epithelial cell line (MCF-10A) was purchased from the
Shanghai Institute of Biochemistry and Cell Biology (Shanghai,
China). All cell lines were cultured in RPMI-1640 medium (MCF-7,
BT-474 and SKBR3; Gibco; Thermo Fisher Scientific Inc., Waltham,
MA, USA) or Dulbecco's modified Eagle's medium (DMEM; MDA-MB-453,
MDA-MB-231, HEK293T and MCF-10A) with 10% (v/v) fetal bovine serum
(FBS) and penicillin/streptomycin (Gibco; Thermo Fisher Scientific,
Inc.).
Oligonucleotide transfection
The miR-452 mimic, negative control mimic (miR-NC),
RAB11A siRNA and negative control siRNA (siR-NC) were all obtained
from Guangzhou RiboBio Co., Ltd. (Guangzhou, China). Cells were
transfected with miR-452 mimics (50 pmol/ml), miR-NC (50 pmol/ml),
RAB11A siRNA (50 pmol/ml), siR-NC (50 pmol/ml), using Lipofectamine
2000 (Invitrogen; Thermo Fisher Scientific Inc.), following the
manufacturer's protocol.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was extracted from the tissues and cells
using TRIzol (Invitrogen; Thermo Fisher Scientific, Inc.) according
to the manufacturer's protocol. The relative expression level of
miR-452 were determined using a SYBR PrimeScript miRNA RT-PCR kit
(Takara Bio, Inc., Otsu, Japan), and normalized to U6. The reaction
system contained 12.5 µl 2X One Step SYBR® RT-PCR Buffer 4, 1.5 µl
TaKaRa Ex Taq™ HS Mix, 0.5 µl PrimeScript™
PLUS RTase Mix, 1 µl forward primer and 1 µl reverse primer, 2 µl
cDNA and 6.5 µl double distilled water. The cycling conditions were
as follows: 42°C for 5 min; 95°C for 10 sec; and 40 cycles of 95°C
for 5 sec, 55°C for 30 sec and 70°C for 30 sec. For detection of
mRNA expression, total RNA was quantified and cDNA was generated by
RT using M-MLV Reverse Transcriptase (Promega Corporation, Madison,
WI USA). RT-qPCR was performed using SYBR Green Real-time PCR
Master Mix (Toyobo Co., Ltd., Osaka, Japan) on an Applied
Biosystems 7500 Sequence Detection system (Thermo Fisher
Scientific, Inc.), with GADPH as an internal control. The reaction
system contained 10 µl SYBR Green PCR master mix, 2 µl forward
primer and 2 µl reverse primer, 2 µl cDNA and double distilled
water. The thermocycling conditions were as follows: 95°C for 10
min, then 40 cycles of 95°C for 15 sec and 60°C for 1 min. The
primer sequences used were as follows: miR-452 forward,
5′-GCGAACTGTTTGCAGAGG-3′ and reverse, 5′-CAGTGCGTGTCGTGGAGT-3′; U6
forward, 5′-TGCGGGTGCTCGCTTCGGCAGC-3′ and reverse,
5′-CCAGTGCAGGGTCCGAGGT-3′; RAB11A forward,
5′-ATCTTCTCCTCGCTTCTGG-3′ and reverse, 5′-GCCTGCTGGCTGGTTATCA-3′;
and GAPDH forward, 5′-TGTGGGCATCAATGGATTTGG-3′ and reverse,
5′-ACACCATGTATTCCGGGTCAAT-3′. Each sample was analyzed in
triplicate, and data were analyzed using the 2−ΔΔCq
method (27).
Transwell migration assay
Transwell chambers (8.0-µm pores; BD Biosciences,
San Jose, CA, USA) were used to evaluate the migration abilities of
cells. At 48 h after transfection, as previously described,
5×104 cells were suspended in FBS-free DMEM medium and
added to the upper chamber, and 500 µl medium with 20% FBS was
placed into the lower compartment. After incubating for 24 h at
37°C with 5% CO2, the non-migrated cells in the upper
chamber were removed with a cotton swab. The migrated cells were
fixed with 100% methanol, stained with 0.5% crystal violet and
washed with PBS (Gibco; Thermo Fisher Scientific, Inc.). The
membranes were observed under a light microscope (Olympus
Corporation, Tokyo, Japan) and five fields were randomly selected
to represent each membrane.
Transwell invasion assay
Transwell chambers pre-coated with Matrigel (BD
Biosciences) were used to evaluate the invasion abilities of cells.
Cells and medium were inserted into the chambers as described for
the Transwell migration assay. After incubating for 48 h at 37°C
with 5% CO2, the cells remaining in the upper chamber
were removed with a cotton swab. The invading cells were fixed and
analyzed as described in the Transwell migration assay section.
Western blotting
Cells were harvested, and lysed with
radioimmunoprecipitation assay lysis buffer. Bulk protein
concentration was determined with a Pierce BCA Protein Assay kit
(Thermo Fisher Scientific, Inc.). Equal amounts of protein (20 µg)
were electrophoresed on an 10% SDS-PAGE gel and transferred to
polyvinylidene fluoride membranes (EMD Millipore, Billerica, MA,
USA). Membranes were blocked with 5% skimmed milk powder in
Tris-buffered saline (TBS) for 1 h, then probed with the primary
antibodies (Abcam, Cambridge, UK) at 4°C overnight. The primary
antibodies were a monoclonal mouse anti-human RAB11A antibody
(ab170134; dilution, 1:1,000) and a monoclonal mouse anti-human
GADPH antibody (ab9484; dilution, 1:1,000). The membranes were
washed with TBS containing 0.1% Tween-20, and incubated with a
corresponding horseradish peroxidase-conjugated secondary antibody
(ab6789; 1:3,000; Abcam) for 1 h at 37°C. Subsequent to washing,
the membranes were visualized using a Pierce Enhanced
Chemiluminescence Detection System (Thermo Fisher Scientific,
Inc.). The densitometry was analyzed by Quantity One software
(version 4.6.2; Bio-Rad Laboratories, Inc., Hercules, CA, USA). For
bioinformatic analysis, the potential target genes of miR-452 were
analyzed using miRanda (http://www.microrna.org) and TargetScan (http://www.targetscan.org/).
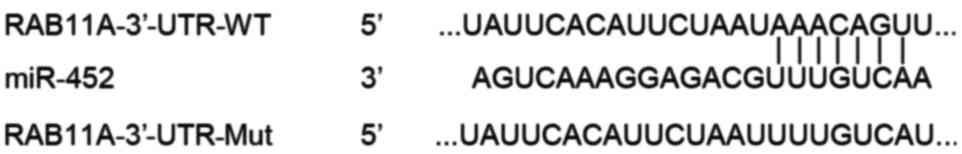
Luciferase reporter assay
Plasmids containing the wild-type RAB11A 3′-UTR
(PmirGLO-RAB11A-3′-UTR-WT) or a mutant RAB11A 3′-UTR
(PmirGLO-RAB11A-3′-UTR-Mut; Fig. 1)
were obtained from Shanghai GenePharma Co., Ltd. (Shanghai, China).
HEK293T cells were co-transfected with PmirGLO-RAB11A-3′-UTR-WT or
PmirGLO-RAB11A-3′-UTR-Mut together with a miR-452 mimic or miR-NC.
At 48 h after transfection, luciferase activity was measured with
the Dual-Luciferase Reporter Assay System (Promega Corporation),
following the manufacturer's protocol. Firefly luciferase
activities were normalized to Renilla luciferase activities.
Statistical analysis
Each assay was repeated three times. Data are
presented as the mean ± standard deviation. Statistical analysis
was performed using two-tailed Student's t-test or one-way analysis
of variance using SPSS software (version 16; SPSS, Inc., Chicago,
IL, USA). SNK was used to compare between two groups in multiple
groups. P<0.05 was considered to indicate a statistically
significant difference.
Results
Expression levels of miR-452 are
downregulated in breast cancer tissues
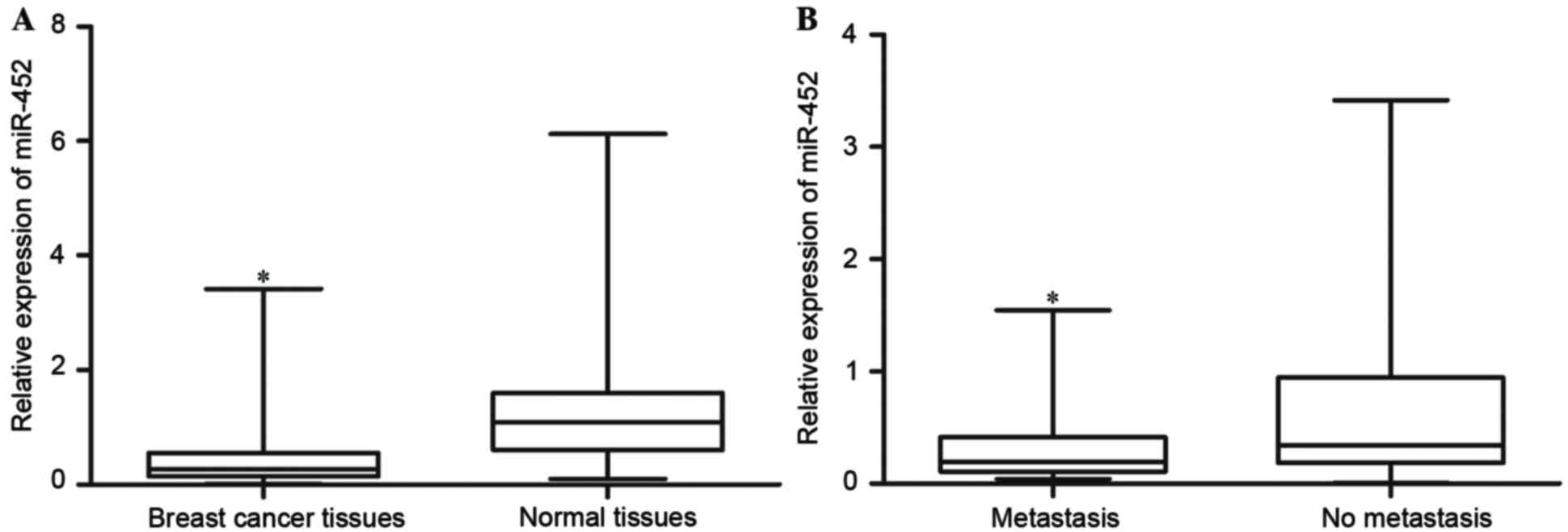
Initially, the expression levels of miR-452 in
breast cancer tissues and matched adjacent normal tissues were
quantified with RT-qPCR. The results revealed that miR-452
expression levels in breast cancer tissues were significantly lower
compared with those in the matched normal tissues (P<0.05;
Fig. 2A).
miR-452 expression levels were additionally compared
between breast cancer tissues in patients with and without
metastatic breast cancer. It was identified that the levels of
miR-452 in breast cancer with metastasis were significantly lower
than those in breast cancer without metastasis (P<0.05; Fig. 2B). These results indicated that
miR-452 was downregulated in breast cancer tissues, and may be
associated with breast cancer metastasis.
Expression levels of miR-452 are
decreased in breast cancer cell lines
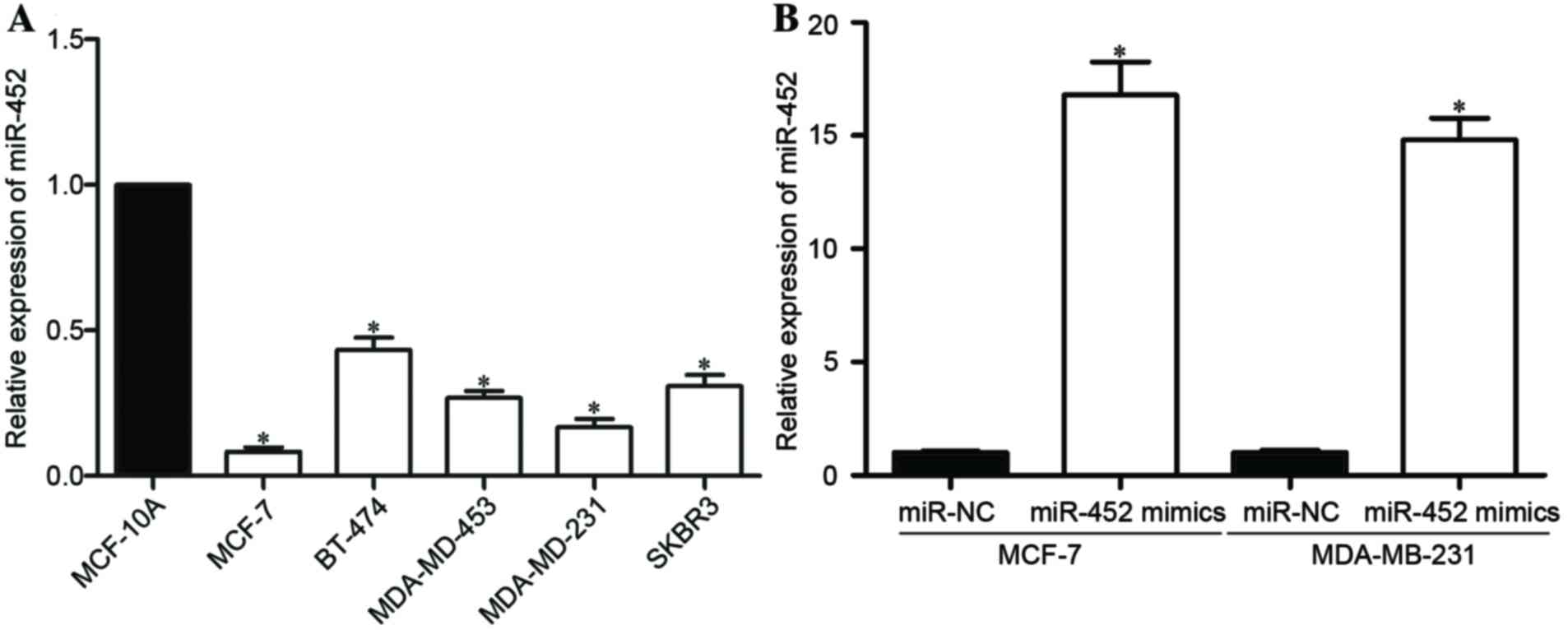
miR-452 expression levels were quantified for a
number of breast cancer cell lines. The miR-452 expression levels
were revealed to be significantly downregulated in all the assessed
breast cancer cell lines (MCF-7, BT-474, MDA-MB-453, MDA-MB-231,
SKBR3) compared with that in MCF-10A, a normal human breast
epithelial cell line (P<0.05; Fig.
3A).
For further studies, MCF-7 and MDA-MB-231 cells were
selected, as these had the lowest miR-452 expression level. An
miR-452 mimic was introduced into MCF-7 and MDA-MB-231 cells to
increase the miR-452 expression level, and miR-NC was used as a
control. The RT-qPCR results demonstrated that miR-452 levels were
significantly higher in MCF-7 and MDA-MB-231 cells following
transfection with the miR-452 mimic than with the miR-NC
(P<0.05; Fig. 3B).
miR-452 inhibits the migration and
invasion capacities of breast cancer cells
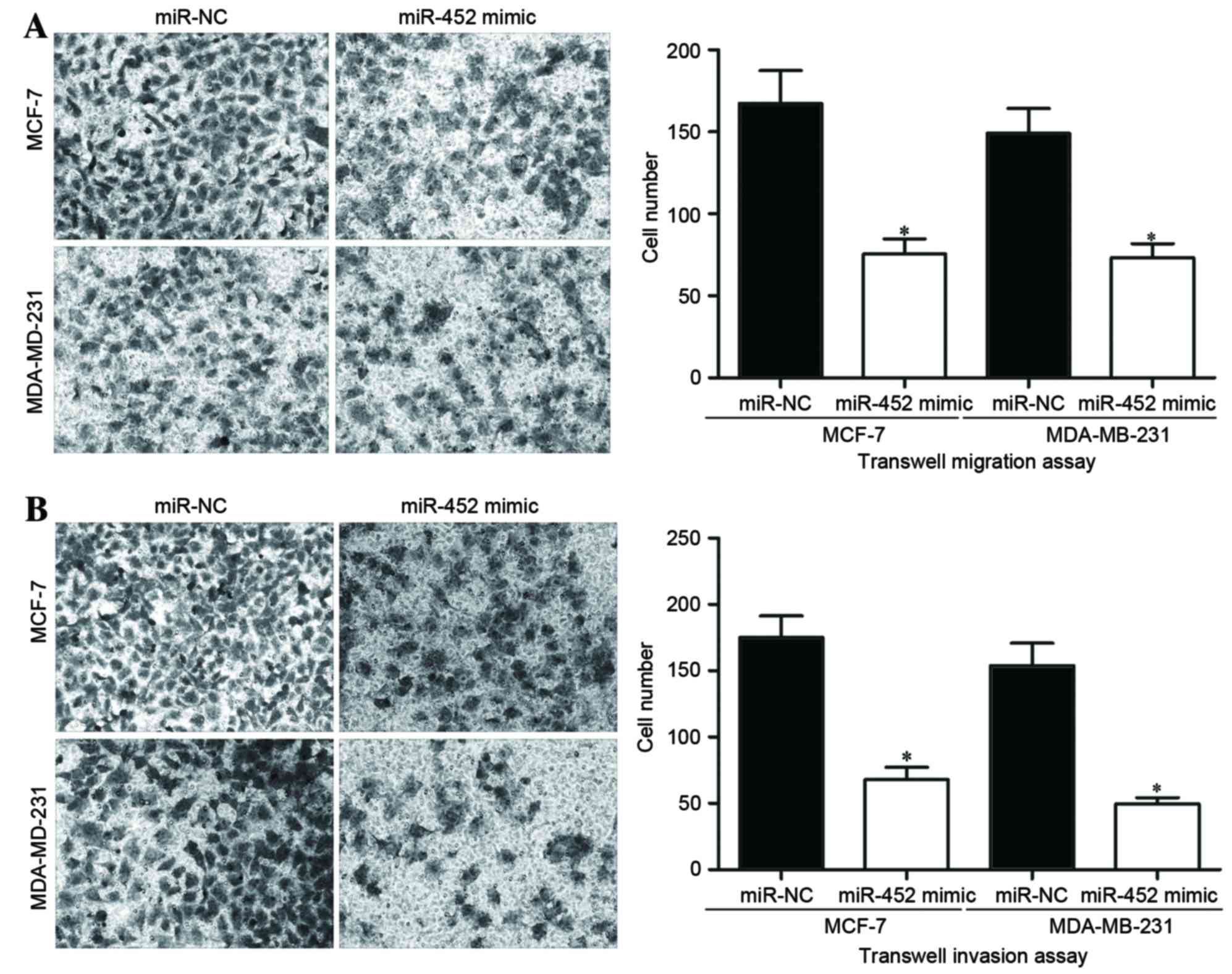
As the expression level of miR-452 had been
associated with metastatic breast cancer in previous results,
Transwell migration and invasion assays were performed to assess
the effect of miR-452 on the migration and invasion capacities of
breast cancer cells. The Transwell migration assay results
demonstrated that miR-452 overexpression significantly inhibited
the migration capacities of MCF-7 and MDA-MB-231 cells (P<0.05;
Fig. 4A). Similarly, the invasion
capacities of MCF-7 and MDA-MB-231 cells were also significantly
inhibited, as demonstrated by the Transwell invasion assays
(P<0.05; Fig. 4B). These results
suggested that miR-452 may be associated with the regulation of
metastasis in breast cancer cells.
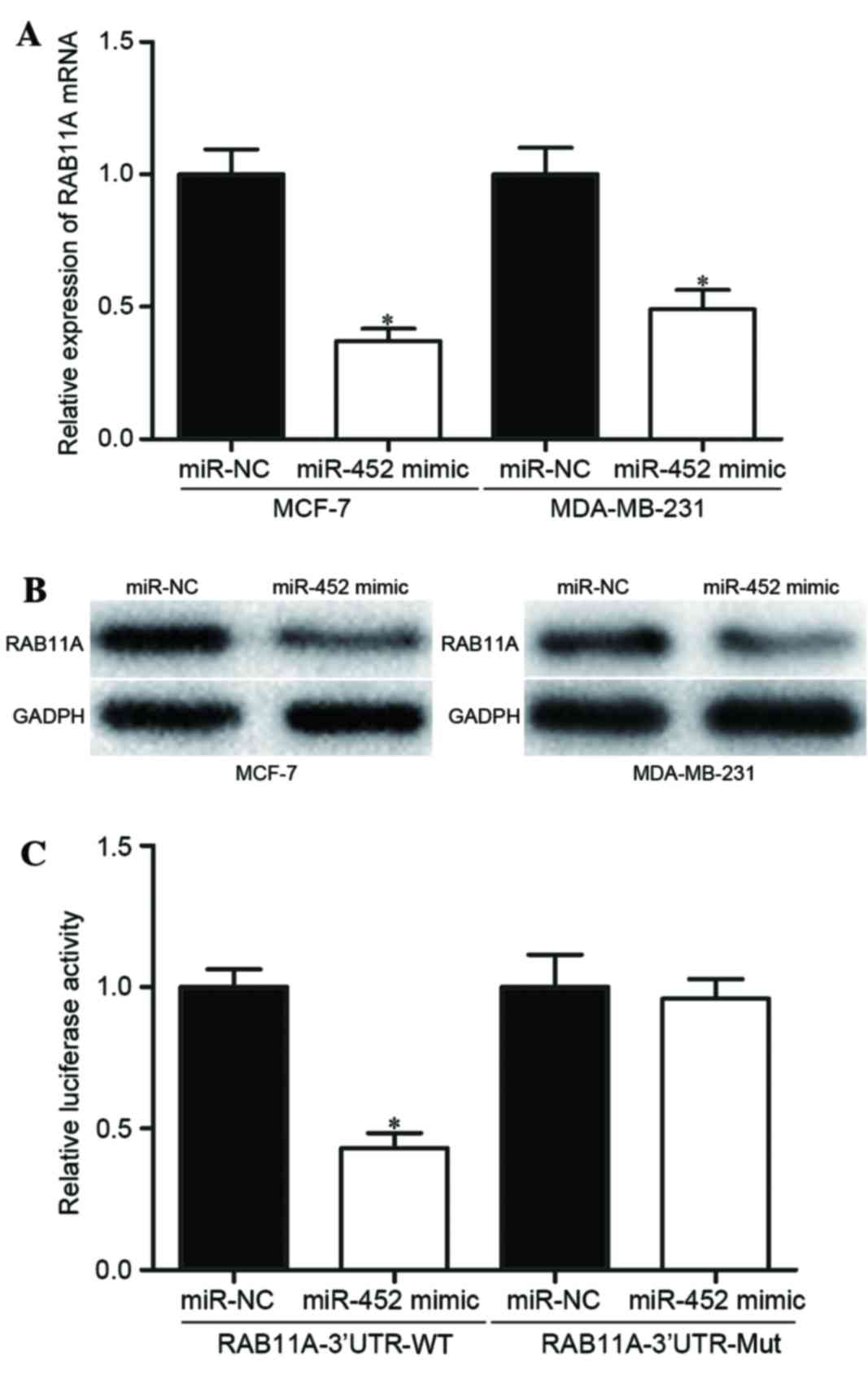
miR-452 directly targets RAB11A in
breast cancer cells
To explore the molecular mechanisms by which miR-452
may inhibit the migration and invasion of breast cancer cells,
bioinformatics analysis was performed with two miRNA algorithms:
miRanda (www.microrna.org) and TargetScan
(www.targetscan.org). The analysis
revealed that RAB11A was a likely target gene of miR-452 (Fig. 1). To confirm whether miR-452
negatively regulated RAB11A expression, the expression of RAB11A at
the mRNA and protein levels was measured by RT-qPCR and western
blot analyses. RAB11A expression was significantly reduced at the
mRNA (P<0.05; Fig. 5A) and protein
(P<0.05; Fig. 5B) levels in the
MCF-7 and MDA-MB-231 cells transfected with an miR-452 mimic,
compared with the cells transfected with miR-NC.
Luciferase reporter assays were performed to explore
whether miR-452 regulated RAB11A expression directly through
binding to the 3′-UTR of RAB11A mRNA. The luciferase activity
significantly decreased following co-transfection with
PmirGLO-RAB11A-3′-UTR-WT and an miR-452 mimic, compared with
co-transfection with PmirGLO-RAB11A-3′-UTR-Mut and the miR-452
mimic (P<0.05; Fig. 5C),
indicating that miR-452 specifically binds to the 3′-UTR of RAB11A
mRNA. Taken together, the results demonstrated that miR-452
negatively regulates RAB11A expression directly through binding the
3′-UTR of RAB11A mRNA.
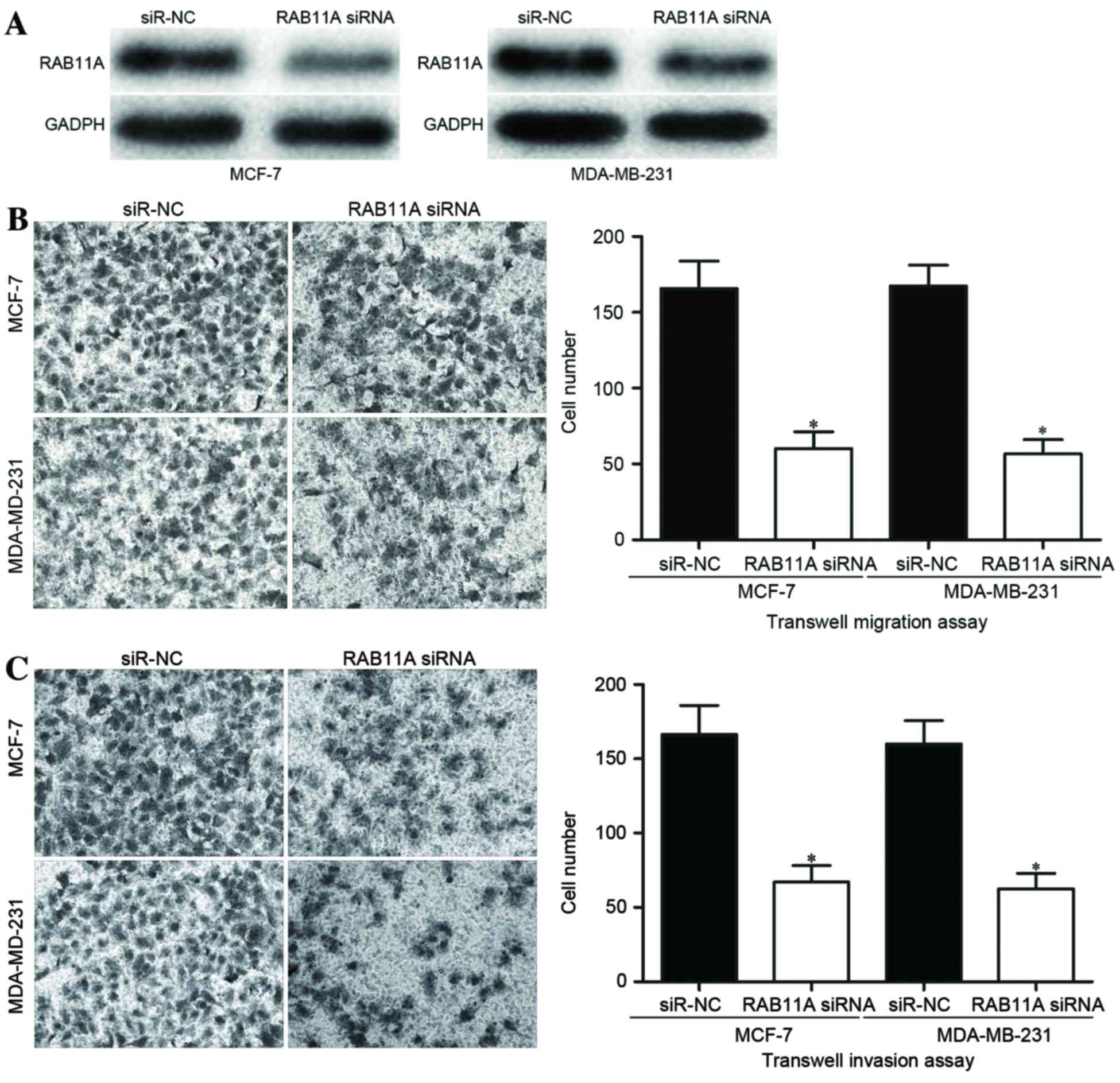
Inhibition of RAB11A protein levels by
RAB11A siRNA inhibits breast cancer cell migration and
invasion
To explore whether miR-452 inhibited breast cancer
cell migration and invasion through negative regulation of RAB11A,
siRNA was used to knockdown the RAB11A expression level in breast
cancer cells. The migration and invasion abilities of these cells
were then evaluated. Following transfection, western blot analysis
measured the expression of RAB11A protein. The results confirmed
that RAB11A was significantly downregulated in MCF-7 and MDA-MB-231
cells subsequent to transfection with RAB11A siRNA, compared with
transfection with an siR-NC (P<0.05; Fig. 6A). Transwell migration and invasion
assays revealed that the numbers of migrating (P<0.05; Fig. 6B) and invading (P<0.05; Fig. 6C) cells were significantly decreased
in the MCF-7 and MDA-MB-231 cells transfected with RAB11A siRNA
compared with in the cells transfected with siR-NC. These results
demonstrated that miR-452 may decrease the migration and invasion
capacities of breast cancer cells via the downregulation of
RAB11A.
Discussion
Breast cancer is the most common type of malignant
tumor in women. The main therapy options for patients with breast
cancer are surgery, radiotherapy and chemotherapy (28). However, patients with metastatic
breast cancer do not respond well to these treatments. Metastasis
is the predominant cause of breast cancer-associated mortality
(29). Thus, it is important to
explore the prevention of metastasis in breast cancer. Studies have
recently identified that miRNAs may inhibit (30,31) or
enhance the metastasis of breast cancer cells (32) or prostate cancer cells (33). The pivotal role of miRNAs in
metastasis via the modulation of various target genes has promoted
intensive research into miRNAs as a novel perspective on the
metastatic process.
In the present study, miR-452 expression levels in
breast cancer tissues and matched adjacent normal tissues were
quantified with RT-qPCR. The result indicated that miR-452 was
significantly downregulated in breast cancer tissues compared with
that in matched adjacent normal tissues, and the level of miR-452
in breast cancer with metastasis was significantly lower than in
breast cancer without metastasis. In addition, the expression
levels of miR-452 were lower in all examined breast cancer cell
lines than in the human breast epithelial cell line MCF-10A.
Similar results have been reported for non-small cell lung cancer
(24), prostate cancer (25) and glioma (26). These findings suggest that the low
expression of miR-452 may be a common event in human cancer, and
may be associated with metastasis of breast cancer.
To investigate the effect of miR-452 on metastasis
of breast cancer, an miR-452 mimic was transfected into breast
cancer cells to enhance its expression. The restoration of miR-452
expression inhibited the migration and invasion capacities of
breast cancer cells, as determined by Transwell migration and
invasion assays, respectively. In non-small cell lung cancer,
overexpression of miR-452 has been shown to decrease the invasion
ability of cancer cells (24).
Furthermore, Liu et al (26)
reported that downregulation of miR-452 serves an important
function in glioma carcinogenesis. Collectively, these findings
indicate that miR-452 may act as a tumor suppressor, and may be a
potential therapeutic target in these types of cancer.
However, the expression level and function of
miR-452 is tissue-specific. miR-452 was identified as upregulated
in various types of human cancer, including hepatocellular
carcinoma (34), esophageal cancer
(22) and urothelial carcinoma
(23). miR-452 enhanced
proliferation, migration and invasion, induced cell cycle G1 to S
transition, and inhibited apoptosis in hepatocellular carcinoma
cells. The difference between cancer types may be explained by the
distinct context of various tissue microenvironments, and the
‘imperfect complementarity’ of the interactions between miRNAs and
target mRNAs (24).
In previous studies, the genes BMI1 proto-oncogene
(24), insulin-like growth factor-1
receptor (35), lymphoid enhanced
binding factor 1 (26), transcription
factor 4 (26), and cyclin-dependent
kinase inhibitor 1B (34) were
demonstrated to be direct targets of miR-452. To understand the
mechanisms by which miR-452 inhibited metastasis in breast cancer,
predicted targets of miR-452 were identified using the TargetScan
and miRanda search tools. The tools predicted that RAB11A was a
target of miR-452. To assess the regulatory association between
miR-452 and RAB11A, RT-qPCR and western blot analyses were adopted
to detect RAB11A expression at the mRNA and protein level in breast
cancer cells following transfection with an miR-452 mimic. The
results revealed that RAB11A mRNA and protein levels were
significantly reduced in miR-452-transfected breast cancer cells.
Additionally, a luciferase reporter assay indicated that miR-452
binds directly to the 3′-UTR of the RAB11A mRNA. The inhibition of
RAB11A protein expression by RAB11A siRNA inhibited breast cancer
cell migration and invasion, thus further verifying that RAB11A is
a direct, functional target gene of miR-452 in breast cancer.
RAB11A is a member of the Rab family, which also
includes RAB11B and RAB25. Rab proteins are small (21–25 kDa),
monomeric GTPases that constitute the largest branch of the Ras
superfamily and are evolutionarily conserved between yeast and
humans (36). It has been reported
that Rab proteins exert an important function in various types of
human cancer, including breast, colon, lung, ovarian and bladder
cancer (37). RAB11A has previously
been demonstrated to be involved in breast cancer carcinogenesis
and progression (38–40). Wang et al (41) reported that RAB11A was a direct target
of miR-320a in breast cancer, and contributed to the growth and
invasion of cancer cells. All these findings support the results of
the present study in implicating RAB11A as a direct functional
target of miR-452 in breast cancer.
In conclusion, the present study revealed that
miR-452 is a novel tumor suppressor gene in breast cancer. miR-452
was significantly downregulated in breast cancer, and its
downregulation was also correlated with metastasis in patients with
breast cancer. Forced miR-452 expression decreased breast cancer
cell metastasis through the direct targeting of RAB11A. Therefore,
these findings provide a potential prognostic target for breast
cancer patients.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Xue J, Chen Z, Gu X, Zhang Y and Zhang W:
MicroRNA-148a inhibits migration of breast cancer cells by
targeting MMP-13. Tumour Biol. 37:1581–1590. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sharma S, Kelly TK and Jones PA:
Epigenetics in cancer. Carcinogenesis. 31:27–36. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Beckmann MW, Niederacher D, Schnurch HG,
Gusterson BA and Bender HG: Multistep carcinogenesis of breast
cancer and tumour heterogeneity. J Mol Med (Berl). 75:429–439.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gradishar WJ: Treatment of metastatic
breast cancer. J Natl Compr Canc Netw. 12 5 Suppl:S759–S761. 2014.
View Article : Google Scholar
|
|
7
|
Martin HL, Smith L and Tomlinson DC:
Multidrug-resistant breast cancer: Current perspectives. Breast
Cancer (Dove Med Press). 6:1–13. 2014.PubMed/NCBI
|
|
8
|
Takahashi RU, Miyazaki H and Ochiya T: The
roles of MicroRNAs in breast cancer. Cancers (Basel). 7:598–616.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gamucci T, D'Ottavio AM, Magnolfi E,
Barduagni M, Vaccaro A, Sperduti I, Moscetti L, Belli F and Meliffi
L: Weekly epirubicin plus docetaxel as first-line treatment in
metastatic breast cancer. Br J Cancer. 97:1040–1045. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chaffer CL and Weinberg RA: A perspective
on cancer cell metastasis. Science. 331:1559–1564. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wan L, Pantel K and Kang Y: Tumor
metastasis: Moving new biological insights into the clinic. Nat
Med. 19:1450–1464. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang Z and Ouyang G: Periostin: A bridge
between cancer stem cells and their metastatic niche. Cell Stem
Cell. 10:111–112. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Teng G and Papavasiliou FN: Shhh!
Silencing by microRNA-155. Philos Trans R Soc Lond B Biol Sci.
364:631–637. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hydbring P and Badalian-Very G: Clinical
applications of microRNAs. F1000Res. 2:1362013.PubMed/NCBI
|
|
15
|
Gromak N: Intronic microRNAs: A crossroad
in gene regulation. Biochem Soc Trans. 40:759–761. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bartel DP: MicroRNAs: Target recognition
and regulatory functions. Cell. 136:215–233. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hwang HW and Mendell JT: MicroRNAs in cell
proliferation, cell death, and tumorigenesis. Br J Cancer. 96
Suppl:R40–R44. 2007.PubMed/NCBI
|
|
18
|
Ryan BM, Robles AI and Harris CC: Genetic
variation in microRNA networks: The implications for cancer
research. Nat Rev Cancer. 10:389–402. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shukla GC, Singh J and Barik S: MicroRNAs:
Processing, maturation, target recognition and regulatory
functions. Mol Cell Pharmacol. 3:83–92. 2011.PubMed/NCBI
|
|
20
|
Wu D, Zhou Y, Pan H, Zhou J, Fan Y and Qu
P: microRNA-99a inhibiting cell proliferation, migration and
invasion by targeting fibroblast growth factor receptor 3 in
bladder cancer. Oncol Lett. 7:1219–1224. 2014.PubMed/NCBI
|
|
21
|
Wu D, Pan H, Zhou Y, Zhang Z, Qu P, Zhou J
and Wang W: Upregulation of microRNA-204 inhibits cell
proliferation, migration and invasion in human renal cell carcinoma
cells by downregulating SOX4. Mol Med Rep. 12:7059–7064.
2015.PubMed/NCBI
|
|
22
|
Wang CZ, Yuan P and Li Y: MiR-126
regulated breast cancer cell invasion by targeting ADAM9. Int J
Clin Exp Pathol. 8:6547–6553. 2015.PubMed/NCBI
|
|
23
|
van Schooneveld E, Wildiers H, Vergote I,
Vermeulen PB, Dirix LY and Van Laere SJ: Dysregulation of microRNAs
in breast cancer and their potential role as prognostic and
predictive biomarkers in patient management. Breast Cancer Res.
17:212015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
He Z, Xia Y, Pan C, Ma T, Liu B, Wang J,
Chen L and Chen Y: Up-Regulation of MiR-452 inhibits metastasis of
non-small cell lung cancer by regulating BMI1. Cell Physiol
Biochem. 37:387–398. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kristensen H, Haldrup C, Strand S,
Mundbjerg K, Mortensen MM, Thorsen K, Ostenfeld MS, Wild PJ, Arsov
C, Goering W, et al: Hypermethylation of the GABRE~miR-452~miR-224
promoter in prostate cancer predicts biochemical recurrence after
radical prostatectomy. Clin Cancer Res. 20:2169–2181. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liu L, Chen K, Wu J, Shi L, Hu B, Cheng S,
Li M and Song L: Downregulation of miR-452 promotes stem-like
traits and tumorigenicity of gliomas. Clin Cancer Res.
19:3429–3438. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wei C, Luo Q, Sun X, Li D, Song H, Li X,
Song J, Hua K and Fang L: MicroRNA-497 induces cell apoptosis by
negatively regulating Bcl-2 protein expression at the
posttranscriptional level in human breast cancer. Int J Clin Exp
Pathol. 8:7729–7739. 2015.PubMed/NCBI
|
|
29
|
Hong W and Dong E: The past, present and
future of breast cancer research in China. Cancer Lett. 351:1–5.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Bockhorn J, Prat A, Chang YF, Liu X, Huang
S, Shang M, Nwachukwu C, Gomez-Vega MJ, Harrell JC, Olopade OI, et
al: Differentiation and loss of malignant character of spontaneous
pulmonary metastases in patient-derived breast cancer models.
Cancer Res. 74:7406–7417. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Erturk E, Cecener G, Polatkan V, Gokgoz S,
Egeli U, Tunca B, Tezcan G, Demirdogen E, Ak S and Tasdelen I:
Evaluation of genetic variations in miRNA-binding sites of BRCA1
and BRCA2 genes as risk factors for the development of early-onset
and/or familial breast cancer. Asian Pac J Cancer Prev.
15:8319–8324. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sun EH, Zhou Q, Liu KS, Wei W, Wang CM,
Liu XF, Lu C and Ma DY: Screening miRNAs related to different
subtypes of breast cancer with miRNAs microarray. Eur Rev Med
Pharmacol Sci. 18:2783–2788. 2014.PubMed/NCBI
|
|
33
|
Cai ZK, Chen Q, Chen YB, Gu M, Zheng DC,
Zhou J and Wang Z: microRNA-155 promotes the proliferation of
prostate cancer cells by targeting annexin 7. Mol Med Rep.
11:533–538. 2015.PubMed/NCBI
|
|
34
|
Zheng Q, Sheng Q, Jiang C, Shu J, Chen J,
Nie Z, Lv Z and Zhang Y: MicroRNA-452 promotes tumorigenesis in
hepatocellular carcinoma by targeting cyclin-dependent kinase
inhibitor 1B. Mol Cell Biochem. 389:187–195. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hu Q, Gong JP, Li J, Zhong SL, Chen WX,
Zhang JY, Ma TF, Ji H, Lv MM, Zhao JH and Tang JH: Down-regulation
of miRNA-452 is associated with adriamycin-resistance in breast
cancer cells. Asian Pac J Cancer Prev. 15:5137–5142. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bhuin T and Roy JK: Rab11 in disease
progression. Int J Mol Cell Med. 4:1–8. 2015.PubMed/NCBI
|
|
37
|
Mosesson Y, Mills GB and Yarden Y:
Derailed endocytosis: An emerging feature of cancer. Nat Rev
Cancer. 8:835–850. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
38
|
Gelsi-Boyer V, Orsetti B, Cervera N,
Finetti P, Sircoulomb F, Rougé C, Lasorsa L, Letessier A, Ginestier
C, Monville F, et al: Comprehensive profiling of 8p11-12
amplification in breast cancer. Mol Cancer Res. 3:655–667. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Caswell PT, Chan M, Lindsay AJ, McCaffrey
MW, Boettiger D and Norman JC: Rab-coupling protein coordinates
recycling of alpha5beta1 integrin and EGFR1 to promote cell
migration in 3D microenvironments. J Cell Biol. 183:143–155. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zhang J, Liu X, Datta A, Govindarajan K,
Tam WL, Han J, George J, Wong C, Ramnarayanan K, Phua TY, et al:
RCP is a human breast cancer-promoting gene with Ras-activating
function. J Clin Invest. 119:2171–2183. 2009.PubMed/NCBI
|
|
41
|
Wang B, Yang Z, Wang H, Cao Z, Zhao Y,
Gong C, Ma L, Wang X, Hu X and Chen S: MicroRNA-320a inhibits
proliferation and invasion of breast cancer cells by targeting
RAB11A. Am J Cancer Res. 5:2719–2729. 2015. View Article : Google Scholar : PubMed/NCBI
|