Introduction
Treatment of non-small cell lung cancer (NSCLC)
requires a complex regimen involving surgery, radiotherapy, and
systemic therapy. Molecular status of individual tumors is
considered as a predictive factor for response to chemo- or
biological therapy or as a prognostic marker for disease
progression (1–3). Driver mutations that are known to
promote carcinogenesis have been identified in certain
genes-mutations in EGFR (for epidermal growth factor
receptor; EGFR), PI3K (for phosphatidylinositol
3-kinase; PI3K), BRAF (for B-Raf), and KRAS (for
k-Ras) are considered to have a predictive value in NSCLC patients
(4) and the highest incidence of
mutations is observed in the EGFR and KRAS genes
(5,6).
Mutations in EGFR occur in exons 18–21 which
encode the tyrosine kinase domain of EGFR. These cause a loss in
autoinhibition of the tyrosine kinase and a continually activated
state of its kinase function. Deletion in exon 19 and a L858R
(leucine to arginine substitution at position 858) substitution in
exon 21 comprise approximately 90% of EGFR mutations found
in adenocarcinomas of the lung (7–16).
Patients with diagnosed mutations in EGFR are referred to as
EGFR-positive. The incidence of EGFR mutation in Caucasian
NSCLC patients in Europe is estimated to be 10% (7,9) and is
more common in women and non-smokers.
While platinum-based chemotherapy has been the
mainstay of NSCLC treatment, advances in molecular diagnostics and
targeted therapies have resulted in a paradigm shift with a focus
on individualized medicine based on histologic classification,
pathologic staging, prognostic markers of survival, and predictive
markers of therapeutic response (17). The discovery of EGFR mutations
in 2004 and subsequent therapeutic response in terms of response
rate (RR), progression-free survival (PFS), and quality of life
(QoL) elicited in EGFR-positive patients by targeted therapy with
EGFR tyrosine kinase inhibitors (TKIs) such as gefitinib and
erlotinib have been adequately documented in large-scale clinical
trials (12–15,18–24). These
results have led to a consensus that the presence of EGFR
mutations is a strong predictor of TKI treatment response and
various associations and working groups, internationally and in
Poland, now recommend screening newly diagnosed patients with
advanced NSCLC for specific mutations in order to customize the
modality of treatment (9,19–32).
Despite these, the incidence rates of EGFR mutations are
found to vary substantially between different regions and countries
(8,10,15).
Possible reasons for this discrepancy could be lack of clarity in
selection criteria for EGFR-positivity testing, differences in
molecular methods employed for screening, and issues with sampling
and tissue preservation. In addition, improper sample collection,
preparation, and storage techniques can render it unamenable for
molecular analysis. However, rapid advancement in diagnostics and
the use of modern methods such as quantitative polymerase chain
reaction (qPCR) allows for detection of EGFR mutation in
samples containing as low as 1% tumor cells (33) and the use of these techniques as a
standard screening procedure in NSCLC categorization could resolve
the issue of accurate detection and treatment optimization.
Despite developments in treatment of advanced NSCLC
and widely accepted guidelines in place, there is paucity in
real-life data on management of EGFR-positive NSCLC in the
Central/Eastern European (CEE) region. The main goal of the
ImplementatioN of perSonalized medicine In NSCLC in Central Europe:
EGFR testing, Histopathology, and clinical feaTures (INSIGHT)
registry was to address these shortcomings (34). In this sub-analysis of the INSIGHT
study, we report the real-life scenario in clinical management,
including diagnosis and treatment, of EGFR-positive advanced NSCLC
in Poland. Furthermore, we aimed at identifying predictors of
EGFR mutation as well as factors associated with the
clinical tumor stage at the time of diagnosis.
Patients and methods
Patient enrollment and data
collection
The INSIGHT study (34) was a multicenter, observational
registry of patients with NSCLC and tested for EGFR
mutation, conducted between November 2011 and March 2013 in five
CEE countries including Poland. Patients were ≥18 years of age,
were diagnosed with advanced and/or metastatic NSCLC and had biopsy
tissue available for EGFR testing, and provided an informed
consent to participation in the study. Also included were patients
who had already tested positive for EGFR mutation and had
either commenced or were scheduled to begin treatment with EGFR
TKIs.
Data collected included demographics, NSCLC
diagnosis, performance status, smoking status, histopathological
examination (including EGFR mutation), molecular method used
for determination of EGFR mutation, and prior and current
treatment regimens (including EGFR TKIs).
Performance status was assessed according to the
Eastern Cooperative Oncology Group (ECOG) scale (35): ECOG=0: Fully active, able to carry on
all pre-disease performance without restriction; ECOG=1: Restricted
in physically strenuous activity but ambulatory and able to carry
our work of a light or sedentary nature; ECOG=2: Ambulatory and
capable of all self-care but unable to carry out any work
activities; up and approximately more than 50% of waking hours;
ECOG=3: Capable of only limited self-care; confined to bed or chair
>50% of waking hours; ECOG=4: Completely disabled; cannot carry
on any self-care; totally confined to bed or chair; ECOG=5:
Dead.
The INSIGHT registry was approved by Ethics
Committees and followed all local laws and regulations.
Statistical analysis
Patient characteristics were summarized using
descriptive statistics. Categorical variables were compared using
Fisher's exact test.
Predictors of presence of EGFR mutation were
determined by logistic regression analysis. For each pre-chosen
parameter, a univariate model was first developed. Subsequently,
these were used to derive a multivariate model through backward
elimination. Odds ratio (OR), 95% confidence interval (95% CI) for
OR and Wald test P-value were reported.
Factors influencing clinical tumor stage at
diagnosis were identified with ordered logistic regression
analysis. Clinical tumor stage was divided into four
categories-I/II, IIIA, IIIB and IV. A multivariate model was
derived as described in the preceding paragraph. Proportional OR,
95% CI for proportional OR (proportional 95% CI) and Wald test
P-value were reported.
P<0.05 was considered to indicate a statistically
significant difference. Statistical analysis was performed using
the R software version 3.1.2 (36).
Results
Patient population
Data from 696 patients collected from four centers
in Poland were included in the analysis. The majority of the
patients were ≥60 years of age [median: 61.4 years, interquartile
range (IQR) 57.0–67.2 years], white Caucasian (n=696, 100%), and
male (n=417, 59.9%). Regarding smoking status, 196 (28.2%) patients
were currently smoking and 285 (40.9%) were ex-smokers.
Most of the NSCLC cases were advanced and metastases
were identified in 140 (20.1%) patients at diagnosis. Common sites
of metastases were supraclavicular lymph node (n=36, 25.7%), brain
(n=25, 17.9%), lung (n=7, 5.0%), and bone (n=5, 3.6%) and these are
classified and compared based on their EGFR mutation status
in Table I. The primary tumor was
identified in 571 (82.0%) patients.
 | Table I.Metastasis by presence of EGFR
mutation. |
Table I.
Metastasis by presence of EGFR
mutation.
| Variables | EGFR-positive | EGFR-negative | P-value |
|---|
| All metastasis, n
(%) | 20 (24.4) | 120 (19.5) | 0.378 |
| OR (95%
CI) of EGFR mutation in patients with all metastasis vs. no
metastasis | 1.33
(0.76–2.25) | 0.305 |
| Brain, n (%) | 2 (2.4) | 23 (3.7) | 0.757 |
| OR (95%
CI) of EGFR mutation in patients with brain metastasis vs.
no brain metastasis in whole group | 0.64
(0.10–2.28) | 0.553 |
| Subgroup with
metastasis, n (%) | 2 (10.0) | 23 (19.2) | 0.528 |
| OR (95%
CI) of EGFR mutation in patients with brain metastasis vs.
any but brain metastasis | 0.47
(0.07–1.78) | 0.332 |
| Bone, n (%) | 3 (3.7) | 2 (0.3) | 0.013 |
| OR (95%
CI) of EGFR mutation in patients with bone metastasis vs. no
bone metastasis in whole group | 11.62
(1.90–89.24) | 0.008 |
| Subgroup with
metastasis, n (%) | 3 (15.0) | 2 (1.7) | 0.021 |
| OR (95%
CI) of EGFR mutation in patients with bone metastasis vs.
any but bone metastasis | 10.41
(1.62–83.51) | 0.014 |
| Lung, n (%) | 1 (1.2) | 6 (1.0) | 0.586 |
| OR (95%
CI) of EGFR mutation in patients with lung metastasis vs. no
lung metastasis in whole group | 1.25
(0.07–7.45) | 0.837 |
| Subgroup
with metastasis, n (%) | 1 (5.0) | 6 (5.0) | >0.999 |
| OR (95%
CI) of EGFR mutation in patients with lung metastasis vs.
any but lung metastasis | 1.00
(0.05–6.32) | >0.999 |
| Liver, n (%) | 0 (0.0) | 1 (0.2) | >0.999 |
| OR (95%
CI) of EGFR mutation in patients with liver metastasis vs.
no liver metastasis in whole group | NAa | NAa |
| Subgroup with
metastasis, n (%) | 0 (0.0) | 1 (0.8) | >0.999 |
| OR (95%
CI) of EGFR mutation in patients with liver metastasis vs.
any but liver metastasis | NAa | NAa |
| Adrenal gland, n
(%) | 0 (0.0) | 1 (0.2) | >0.999 |
| OR (95%
CI) of EGFR mutation in patients with adrenal gland
metastasis vs. no adrenal gland metastasis in whole group | NAa | NAa |
| Subgroup
with metastasis, n (%) | 0 (0.0) | 1 (0.8) | >0.999 |
| OR (95%
CI) of EGFR mutation in patients with adrenal gland
metastasis vs. any but adrenal gland metastasis | NAa | NAa |
| SCL, n (%) | 3 (3.7) | 33 (5.4) | 0.789 |
| OR (95%
CI) of EGFR mutation in patients with SCL metastasis vs. no
SCL metastasis in whole group | 0.67
(0.16–1.92) | 0.512 |
| Subgroup with
metastasis, n (%) | 3 (15.0) | 33 (27.5) | 0.364 |
| OR (95%
CI) of EGFR mutation in patients with SCL metastasis vs. any
but SCL metastasis | 0.47
(0.10–1.50) | 0.245 |
| Other, n (%) | 2 (10.0) | 23 (19.2) | 0.528 |
| OR (95%
CI) of EGFR mutation in patients with other metastasis vs.
no other metastasis in whole group | 1.58
(0.75–3.04) | 0.199 |
| Subgroup with
metastasis, n (%) | 11 (55.0) | 55 (45.8) | 0.604 |
| OR (95%
CI) of EGFR mutation in patients with other metastasis vs.
any but other metastasis | 1.44
(0.56–3.83) | 0.449 |
Performance status at the time of diagnosis as
defined by ECOG rating was ‘good’ in a substantial proportion of
the patients [ECOG=0 in 16 (3.9%) patients; ECOG=1 in 308 (74.9%)
patients] and ‘moderate’ (ECOG=2) in 81 (19.7%) patients (Table II).
 | Table II.Performance status and clinical stage
of tumors by presence of EGFR mutation. |
Table II.
Performance status and clinical stage
of tumors by presence of EGFR mutation.
|
| n (%) |
|---|
|
|
|
|---|
| Variables | EGFR negative | EGFR positive | Total |
|---|
| ECOG score |
|
|
|
| 0 | 9 (2.5) | 7 (13.5) | 16 (3.9) |
| 1 | 275 (76.6) | 33 (63.5) | 308 (74.9) |
| 2 | 70 (19.5) | 11 (21.2) | 81 (19.7) |
| 3 | 5 (1.4) | 1 (1.9) | 6 (1.5) |
| 4 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Clinical tumor
stage |
|
|
|
|
I/II | 67 (13.6) | 5 (6.6) | 72 (12.7) |
|
IIIA | 64 (13.0) | 4 (5.3) | 68 (12.0) |
|
IIIB | 79 (16.0) | 6 (7.9) | 85 (14.9) |
| IV | 283 (57.4) | 61 (80.3) | 344 (60.5) |
Histopathological diagnosis
Diagnosis of NSCLC was based on evaluation of
histological specimen in 82.4% of the patients and of cytological
sample in 16.8% of the patients. The most commonly employed methods
of sample collection were surgical biopsy (32.1%), transbronchial
biopsy (25.8%), and endoscopic/endobronchial ultrasound guided
needle biopsy (15.5%). Other methods also used were computed
tomography guided transpareital biopsy (9.2%), intraluminal biopsy
(3.0%), fine needle biopsy without X-ray guidance (2.4%),
mediastinoscopy (2.4%), brush cytology (1.7%), computed tomography
guided bronchoscopic biopsy (0.9%), bronchial lavage (0.9%), and
others (6.0%).
Most of the NSCLC tumors in study patients were of
adenocarcinomatous (AC) origin-36.5% of the patients presenting
non-mucinous AC, 30.2% presenting non-specified AC, and 3.6% with
mucinous AC. A total of 1.3% patients presented with an
adenosquamous carcinoma, a tumor type with a mixed histology. A
majority of EGFR-TKI treated patients present with adenosquamous
carcinomas with a predominance of adenomas.
Clinical management of NSCLC
A substantial proportion of study patients (79.6%)
received systemic therapy-of these, 85.0% as palliative therapy,
11.3% in neoadjuvant setting, and 3.8% in adjuvant setting (data
not shown). In patients not considered for systemic therapy, low
performance status and poor compliance were the major individual
reasons for the decision. Surgery as a therapeutic intervention was
performed in 26.6% of the patients while 13.7% received radiation
therapy.
EGFR mutation
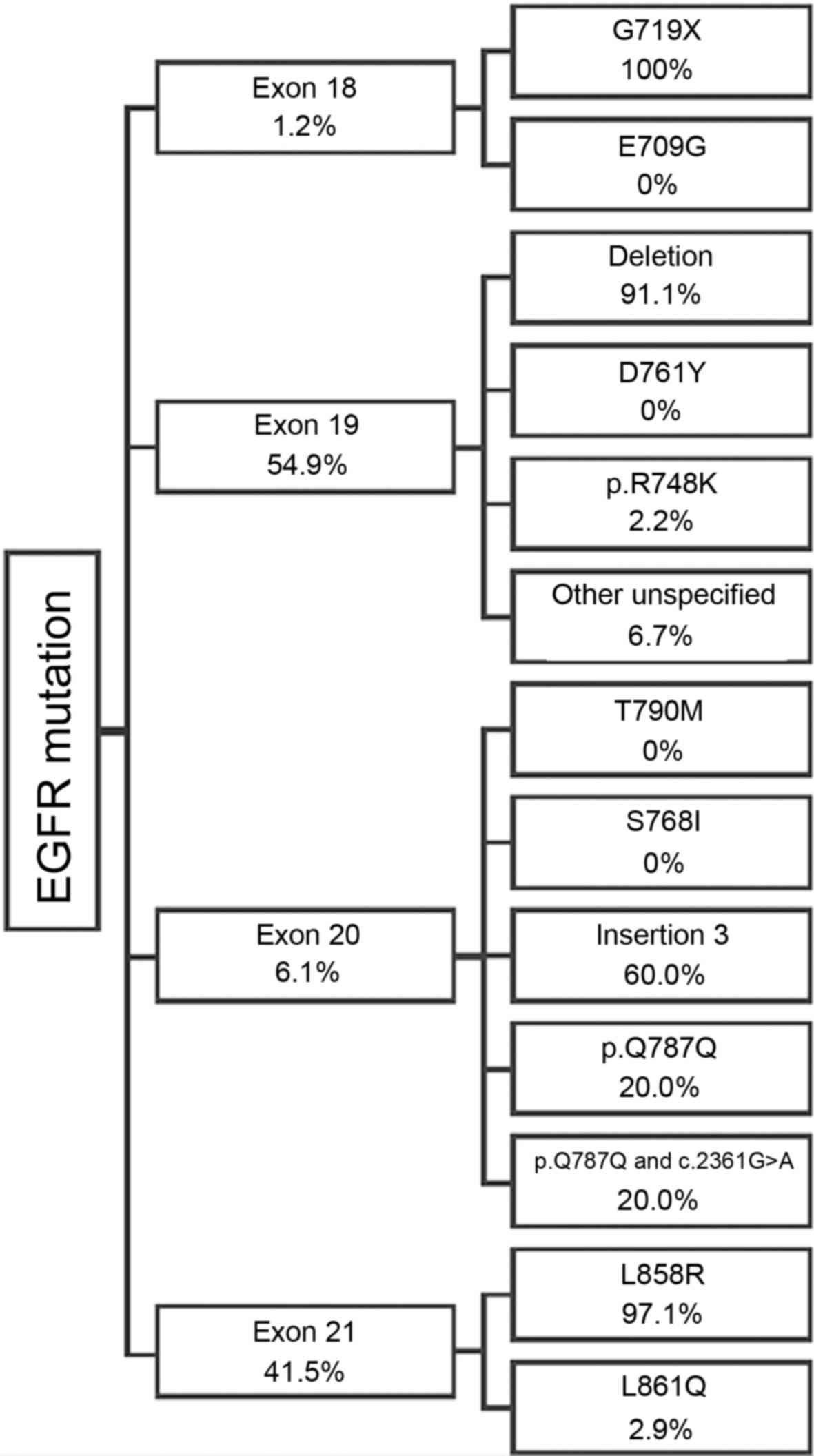
A total of 82 (11.8%) study patients were determined
to have EGFR mutations. Most commonly reported mutations
were deletion on exon 19 and L858R substitution on exon 21. Details
of distribution of EGFR mutations are given in Fig. 1.
Factors associated with presence of
EGFR mutation
Patients with EGFR mutation were
predominantly female [45 of 82 (54.9%) EGFR-positive patients] in
comparison to patients without such mutations (38.1% of
EGFR-negative patients) (P=0.005). An EGFR-positive status was
strongly associated with gender and males were less likely to be
EGFR-positive (male vs. female OR: 0.51; 95% CI: 0.32–0.80;
P=0.004). The proportion of never-smokers was higher in
EGFR-positive patients (26 of 69 patients, 37.7%; smoking status
unknown in 13 patients) than in EGFR-negative patients (6.8%)
(P<0.001) and the propensity for EGFR-positive status was lower
in patients who were current or past smokers (OR: 0.16; 95% CI:
0.09–0.28; P<0.001). Performance status at the time of diagnosis
had a wider distribution and proportion of patients in advanced
disease stage was higher in EGFR-positive patients (Table III). Moreover, EGFR-positive
patients had a higher predilection to be in clinical stage IV than
in stage I/II at the time of diagnosis (OR: 2.89; 95% CI:
1.22–8.50; P=0.029).
 | Table III.Factors associated with advanced
cancer stage identified by multivariate analysis. |
Table III.
Factors associated with advanced
cancer stage identified by multivariate analysis.
| Variables | Proportional OR
(95% CI) | P-value |
|---|
| EGFR
mutation status |
|
|
|
EGFR-positive vs.
EGFR-negative | 2.63
(1.31–5.26) | 0.006 |
| Performance on ECOG
scale |
|
|
| ECOG=1
vs. ECOG=0 | 2.26
(0.80–6.41) | 0.125 |
|
ECOG=2/3 vs. ECOG=0 | 5.87
(1.86–18.48) | 0.003 |
| Diagnosis |
|
|
| All
other tumour types except squamous cell carcinoma and
adenocarcinoma vs. adenocarcinoma | 1.92
(1.18–3.14) | 0.009 |
|
Squamous cell carcinoma vs.
adenocarcinoma | 2.43
(0.22–26.54) | 0.466 |
EGFR mutation and metastasis
With the exception of metastasis to the bone, no
association was observed between the EGFR status and metastatic
potential of primary tumors. Incidence of metastasis to the bone
was higher (3.7%) in patients with EGFR mutation in
comparison with EGFR-negative patients (0.3%; P=0.013). The odds of
EGFR mutation in patients with bone metastasis in comparison
to the patients without bone metastasis in the entire population or
those with any but bone metastasis was also significantly higher
(bone metastasis vs. no bone metastasis in the entire group
OR=11.62; 95% CI: 1.90–89.23; P=0.008 and bone metastasis vs. any
but bone metastasis in metastasis group OR=10.41; 95% CI:
1.62–83.51; P=0.014).
EGFR mutation and histopathological
tumor staging
An association between histopathological diagnoses
of NSCLC and presence of EGFR mutation is given in Table IV. The most striking observation is
decreased probability of EGFR mutation in not otherwise
specified (NOS) type NSCLC in comparison to adenocarcinoma
(OR=0.23; 95% CI: 0.06–0.64; P=0.015). Patients without EGFR
mutation were noted to undergo surgical treatment more frequently
than EGFR-positive patients but this difference could not be
statistically validated (27.9 vs. 19.5%; P=0.151). We also observed
that more patients with EGFR mutation received radiotherapy
in comparison to EGFR-negative patients (24.4 vs. 11.7%;
P=0.004).
 | Table IV.EGFR mutation and clinical
stage of tumor by histopathological diagnosis. |
Table IV.
EGFR mutation and clinical
stage of tumor by histopathological diagnosis.
| OR (95% CI) of
EGFR-positive status | P-value | Proportional OR
(95% CI) of clinical stage of tumor | P-value |
|---|
| Bronchoalveolar
carcinoma vs. adenocarcinoma |
|
|
|
| 3.51
(0.48–18.38) | 0.151 | 2.38
(0.25–22.21) | 0.446 |
| Large-cell
carcinoma vs. adenocarcinoma |
|
|
|
| 0.88
(0.05–4.90) | 0.904 | 1.18
(0.29–4.80) | 0.818 |
| Mixed cell
carcinoma vs. adenocarcinoma |
|
|
|
| 2.11
(0.46–7.11) | 0.266 | 0.13
(0.03–0.57) | 0.007 |
| NOS carcinoma vs.
adenocarcinoma |
|
|
|
| 0.23
(0.06–0.64) | 0.015 | 2.07
(1.25–3.42) | 0.005 |
| Other carcinoma vs.
adenocarcinoma |
|
|
|
| 2.64
(0.92–6.67) | 0.051 | 1.48
(0.60–3.65) | 0.399 |
| Squamous cell
carcinoma vs. adenocarcinoma |
|
|
|
| 1.08
(0.17–4.03) | 0.919 | 1.97
(0.40–9.82) | 0.406 |
Factors associated with presence of
EGFR mutation
As shown in Table V,
multivariate regression analysis revealed that NSCLC patients who
were past or current smokers or had lower performance as per ECOG
scale were less likely to carry a EGFR mutation.
 | Table V.Factors associated with presence of
EGFR mutation identified by multivariate analysis. |
Table V.
Factors associated with presence of
EGFR mutation identified by multivariate analysis.
| Factor | OR (95% CI) | P-value |
|---|
| Smoking status |
|
|
|
Ex/current smoker vs. never
smoked | 0.12
(0.05–0.25) | <0.001 |
| Performance on ECOG
scale |
|
|
| ECOG=1
vs. ECOG=0 | 0.19
(0.06–0.70) | 0.009 |
| ECOG=2
vs. ECOG=0 | 0.25
(0.06–1.01) | 0.048 |
| ECOG=3
vs. ECOG=0 | 0.54
(0.02–4.98) | 0.624 |
Factors associated with clinical tumor
stage at diagnosis
The proportional OR between stages I/II, IIIA, IIIB,
and IV for ECOG=1 vs. ECOG=0 was 1.515 (95% CI: 0.580–3.958;
P=0.397). In contrast, the proportional OR between stages when
comparing ECOG=2–3 and ECOG=0 was 4.076 (95% CI: 1.394–11.923;
P=0.010) thereby indicating that performance status substantially
diminished with progression in clinical stages.
The NOS type NSCLC was associated with greater odds
of more advanced clinical tumor than adenocarcinoma. Odds of more
advanced clinical tumor in bronchoalveolar carcinoma, large cell
carcinoma, mixed carcinoma, or squamous cell carcinoma did not
differ significantly from odds in adenocarcinoma diagnosis. In
contrast, the mixed type carcinoma had lower odds of more advance
clinical stage than adenocarcinoma.
The results of multivariate regression modelling
(Table III) confirm previous
findings that patients with poor ECOG scores, EGFR mutation,
and diagnosed with NSCLC of a histopathological type other than
adenocarcinoma or squamous cell carcinoma have a higher likelihood
of being diagnosed with advanced clinical tumors.
Discussion
We found that the incidence of EGFR mutation
in the Polish subpopulation of the INSIGHT study is similar that
reported for the general European population (5). We also reiterate previous findings that
EGFR-positive status is associated with female gender and
never-smoker status. The clinical stage of NSCLC at the time of
diagnosis was usually more advanced in EGFR-positive patients
thereby precluding radical surgery and promoting radiotherapy and
systemic therapy in these patients. However, one must take note
that the presentation of advanced stage in NSCLC patients with
EGFR mutations is not always associated with an increased
probability of bearing such a mutation; the late diagnosis could
simply be because patients in Stage I or II are not routinely
tested for mutations. We also discovered that the propensity to
develop bone metastasis, usually associated with a poor prognosis
(37), was almost 12-fold higher in
EGFR-positive NSCLC patients in comparison to their EGFR-negative
counterparts. However, this statistic may not be an accurate
reflection of the actual risk when we take in consideration the
small patient number in the reported study.
The choice of appropriate molecular methods is
important for reliable detection of EGFR mutations,
especially in samples with low tumor cell count. The effectiveness
of these methods could be jeopardized by suboptimal procedures of
tumor sampling and preservation techniques. Nevertheless, results
from a multicenter, retrospective study designed to evaluate
effectiveness of various methods for EGFR mutation testing
showed no substantial difference in detected frequency of mutations
between cytological and histological samples (33). This implies that the low tumor
cellularity evidenced with cytological and small biopsy samples did
not hinder the sensitivity of the real-time PCR assay employed in
the study for detecting EGFR mutations. This offers a
substantial benefit in screening NSCLC patients with poorer
performance status or those in whom invasive procedures are
contraindicated. Despite the demonstrated benefits of TKI therapy
in EGFR-positive NSCLC and guidelines recommending timely screening
and treating at-risk patients with TKI as first-line chemotherapy
(38), these are not widely applied
in clinical practice in Poland. While we cannot identify any
particular reason for this, it has been demonstrated that routine
nationwide molecular profiling of NSCLC patients is feasible and
provides immense benefit in terms of frequency of driver mutations
and their specific type (39). Of
special interest are NSCLC with uncommon EGFR mutations that
occur in approximately 1.0% of NSCLC cases (40), or those with poor prognosis such as
adenosquamous carcinoma (41),
detected in 1.3% of our study patients, and EGFR-positive NSCLC
metastasizing to the bone (42). The
heterogeneous molecular profiles presented in these types need to
be studied in detail in order to not only study the occurrence and
pathological differences arising from various mutations but also to
design specific therapies aimed at molecular targets (40).
The database of the INSIGHT registry is the first of
its kind for Poland in our knowledge and it provides robust data on
sampling methods, molecular testing, frequency and types of
EGFR mutations, treatment modalities, and prognostic factors
related to Polish patients with EGFR-positive NSCLC. In comparison
to conventional chemotherapy, EGFR TKI therapy has been
demonstrated to be more effective and safer in NSCLC patients with
EGFR mutations. A notable conclusion of a meta-analysis of
13 phase III trials was that targeted therapy with EGFR TKIs
noticeably improved PFS [Hazard ratio (HR): 0.43; 95% CI:
0.38–0.49] but had no such effect on overall survival (OS) (HR:
1.01; 95% CI: 0.87–1.18) (43). A
plausible reason for this lack of improvement in OS could be that
EGFR TKIs were used as second or further lines of therapy, once
conventional chemotherapy was found to lack therapeutic effect.
Results from the OPTIMAL study have shown that erlotinib as a
first-line treatment enhances PFS and has a better safety profile
in comparison with conventional chemotherapy (24). Similar beneficial effects on PFS have
been reported from two landmark phase III trials on the
irreversible EGFR TKI, afatinib (21,22). In
addition, while no statistically significant differences were
evident in these studies between afatinib and cisplatin (latter in
combination with either permetrexed or gemcitabine) as first-line
treatment in EGFR-positive stage IIIB and IV lung adenocarcinoma
patients, subgroup analysis has shown that OS of patients with
del19 EGFR mutation who were administered afatinib was
substantially improved (23). In the
LUX-Lung 3 trial, afatinib-treated patients presenting del 19
mutation had median OS of 33.3 months (95% CI: 26.8–41.5) in
comparison to 21.1 months (95% CI: 16.3–30.7) in those who received
conventional chemotherapy (HR: 0.54; 95% CI: 0.36–0.79; P=0.0015).
Similarly, in the LUX-Lung 6 trial, patients with del 19 mutations
who received afatinib had median OS of 31.4 months (95% CI:
24.2–35.3) vs. OS of 18.4 months (95% CI: 14.6–25.6) in those on
conventional therapy (HR: 0.64; 95% CI: 0.44–0.94; P=0.020).
Despite being the first of its kind disease registry
that gathered information on clinical management of EGFR-positive
NSCLC in the CEE region, the INSIGHT study and our sub-analysis
have some inherent limitations. Being an observational study, we
could only capture a snapshot of current practices at predetermined
locations in Poland and the nationwide situation could differ. One
way to rectify this could be drafting and implementing guidelines
that would require participation from all tertiary cancer centers
in Poland in a national NSCLC registry. Another drawback of the
INSIGHT registry is that since it was not prospective by nature, we
could not assess the long-term benefits and effectiveness of
current strategies in the therapeutics of EGFR-positive NSCLC in
Poland and the CEE region. These questions can only be answered by
elaborate prospective studies and we hope that our registry serves
as an impetus to such investigations.
In conclusion, EGFR TKIs are effective agents
against EGFR-positive NSCLC and should be routinely considered as
first-line treatment in these patients; therefore EGFR
testing should be performed at the earliest. Data from the INSIGHT
registry could be used to improve guidelines, standardize screening
techniques, as well as create a predictor algorithm for example a
nomogram (44). Such an approach that
will integrate individual risk factor analysis and improve
EGFR-targeted therapies could lead to personalized gene-directed
therapies for EGFR-positive NSCLC patients.
Acknowledgements
The editorial help with this manuscript was provided
by Mateusz Spalek, Satyen Shenoy and Agnieszka
Linkiewicz-Zegan.
References
|
1
|
Coate LE, John T, Tsao MS and Shepherd FA:
Molecular predictive and prognostic markers in non-small-cell lung
cancer. Lancet Oncol. 10:1001–1010. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kerr KM, Bubendorf L, Edelman MJ,
Marchetti A, Mok T, Novello S, O'Byrne K, Stahel R, Peters S, Felip
E, et al: Second ESMO consensus conference on lung cancer:
Pathology and molecular biomarkers for non-small-cell lung cancer.
Ann Oncol. 25:1681–1690. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
O'Byrne KJ, Gatzemeier U, Bondarenko I,
Barrios C, Eschbach C, Martens UM, Hotko Y, Kortsik C, Paz-Ares L,
Pereira JR, et al: Molecular biomarkers in non-small-cell lung
cancer: A retrospective analysis of data from the phase 3 FLEX
study. Lancet Oncol. 12:795–805. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chatziandreou I, Tsioli P, Sakellariou S,
Mourkioti I, Giannopoulou I, Levidou G, Korkolopoulou P, Patsouris
E and Saetta AA: Comprehensive molecular analysis of NSCLC;
Clinicopathological Associations. PLoS One. 10:e01338592015.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dearden S, Stevens J, Wu YL and Blowers D:
Mutation incidence and coincidence in non small-cell lung cancer:
Meta-analyses by ethnicity and histology (mutMap). Ann Oncol.
24:2371–2376. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
D'Arcangelo M and Cappuzzo F: K-Ras
mutations in non-small-cell lung cancer: Prognostic and predictive
value. ISRN Mol Biol. 2012:8373062012.PubMed/NCBI
|
|
7
|
Aisner DL and Marshall CB: Molecular
pathology of non-small cell lung cancer: A practical guide. Am J
Clin Pathol. 138:332–346. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Boch C, Kollmeier J, Roth A,
Stephan-Falkenau S, Misch D, Grüning W, Bauer TT and Mairinger T:
The frequency of EGFR and KRAS mutations in non-small cell lung
cancer (NSCLC): Routine screening data for central Europe from a
cohort study. BMJ Open. 3:pii:e0025602013. View Article : Google Scholar
|
|
9
|
Eberhard DA, Giaccone G and Johnson BE:
Non-Small-Cell lung Cancer Working Group: Biomarkers of response to
epidermal growth factor receptor inhibitors in Non-Small-Cell Lung
Cancer Working Group: Standardization for use in the clinical trial
setting. J Clin Oncol. 26:983–994. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gahr S, Stoehr R, Geissinger E, Ficker JH,
Brueckl WM, Gschwendtner A, Gattenloehner S, Fuchs FS, Schulz C,
Rieker RJ, et al: EGFR mutational status in a large series of
Caucasian European NSCLC patients: Data from daily practice. Br J
Cancer. 109:1821–1828. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kosaka T, Yatabe Y, Endoh H, Kuwano H,
Takahashi T and Mitsudomi T: Mutations of the epidermal growth
factor receptor gene in lung cancer: Biological and clinical
implications. Cancer Res. 64:8919–8923. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lynch TJ, Bell DW, Sordella R,
Gurubhagavatula S, Okimoto RA, Brannigan BW, Harris PL, Haserlat
SM, Supko JG, Haluska FG, et al: Activating mutations in the
epidermal growth factor receptor underlying responsiveness of
non-small-cell lung cancer to gefitinib. N Eng J Med.
350:2129–2139. 2004. View Article : Google Scholar
|
|
13
|
Paez JG, Jänne PA, Lee JC, Tracy S,
Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, et
al: EGFR mutations in lung cancer: Correlation with clinical
response to gefitinib therapy. Science. 304:1497–1500. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pao W, Miller V, Zakowski M, Doherty J,
Politi K, Sarkaria I, Singh B, Heelan R, Rusch V, Fulton L, et al:
EGF receptor gene mutations are common in lung cancers from ‘never
smokers’ and are associated with sensitivity of tumors to gefitinib
and erlotinib. Proc Natl Acad Sci USA. 101:13306–13311. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Rosell R, Carcereny E, Gervais R,
Vergnenegre A, Massuti B, Felip E, Palmero R, Garcia-Gomez R,
Pallares C, Sanchez JM, et al: Erlotinib versus standard
chemotherapy as first-line treatment for European patients with
advanced EGFR mutation-positive non-small-cell lung cancer
(EURTAC): A multicentre, open-label, randomised phase 3 trial.
Lancet Oncol. 13:239–246. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shigematsu H, Lin L, Takahashi T, Nomura
M, Suzuki M, Wistuba II, Fong KM, Lee H, Toyooka S, Shimizu N, et
al: Clinical and biological features associated with epidermal
growth factor receptor gene mutations in lung cancers. J Natl
Cancer Inst. 97:339–346. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Souglakos J: Customizing chemotherapy in
non-small cell lung cancer: The promise is still unmet. Trans Lung
Cancer Res. 4:653–655. 2015.
|
|
18
|
Maemondo M, Inoue A, Kobayashi K, Sugawara
S, Oizumi S, Isobe H, Gemma A, Harada M, Yoshizawa H, Kinoshita I,
et al: Gefitinib or chemotherapy for non-small-cell lung cancer
with mutated EGFR. N Eng J Med. 362:2380–2388. 2010. View Article : Google Scholar
|
|
19
|
Mitsudomi T, Morita S, Yatabe Y, Negoro S,
Okamoto I, Tsurutani J, Seto T, Satouchi M, Tada H, Hirashima T, et
al: Gefitinib versus cisplatin plus docetaxel in patients with
non-small-cell lung cancer harbouring mutations of the epidermal
growth factor receptor (WJTOG3405): An open label, randomised phase
3 trial. Lancet Oncol. 11:121–128. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mok TS, Wu YL, Thongprasert S, Yang CH,
Chu DT, Saijo N, Sunpaweravong P, Han B, Margono B, Ichinose Y, et
al: Gefitinib or carboplatin-paclitaxel in pulmonary
adenocarcinoma. N Eng J Med. 361:947–957. 2009. View Article : Google Scholar
|
|
21
|
Sequist LV, Yang JC, Yamamoto N, O'Byrne
K, Hirsh V, Mok T, Geater SL, Orlov S, Tsai CM, Boyer M, et al:
Phase III study of afatinib or cisplatin plus pemetrexed in
patients with metastatic lung adenocarcinoma with EGFR mutations. J
Clin Oncol. 31:3327–3334. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wu YL, Zhou C, Hu CP, Feng J, Lu S, Huang
Y, Li W, Hou M, Shi JH, Lee KY, et al: Afatinib versus cisplatin
plus gemcitabine for first-line treatment of Asian patients with
advanced non-small-cell lung cancer harbouring EGFR mutations
(LUX-Lung 6): An open-label, randomised phase 3 trial. Lancet
Oncol. 15:213–222. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yang JC, Wu YL, Schuler M, Sebastian M,
Popat S, Yamamoto N, Zhou C, Hu CP, O'Byrne K, Feng J, et al:
Afatinib versus cisplatin-based chemotherapy for EGFR
mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6):
Analysis of overall survival data from two randomised, phase 3
trials. Lancet Oncol. 16:141–151. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhou C, Wu YL, Chen G, Feng J, Liu XQ,
Wang C, Zhang S, Wang J, Zhou S, Ren S, et al: Erlotinib versus
chemotherapy as first-line treatment for patients with advanced
EGFR mutation-positive non-small-cell lung cancer (OPTIMAL,
CTONG-0802): A multicentre, open-label, randomised, phase 3 study.
Lancet Oncol. 12:735–742. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ettinger DS, Akerley W, Bepler G, Blum MG,
Chang A, Cheney RT, Chirieac LR, D'Amico TA, Demmy TL, Ganti AK, et
al: Non-small cell lung cancer. J Natl Compr Canc Netw. 8:740–801.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lindeman NI, Cagle PT, Beasley MB, Chitale
DA, Dacic S, Giaccone G, Jenkins RB, Kwiatkowski DJ, Saldivar JS,
Squire J, et al: Molecular testing guideline for selection of lung
cancer patients for EGFR and ALK tyrosine kinase inhibitors:
Guideline from the College of American pathologists, international
association for the study of lung cancer and Association for
Molecular Pathology. Arch Pathol Lab Med. 137:828–860. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Marchetti A, Normanno N AIOM-SIAPEC-IAP,
Pinto C, Taddei GL, Adamo V, Ardizzoni A, Botti G, Bardelli A,
Comin C, et al: Recommendations for mutational analysis of EGFR in
lung carcinoma. Pathologica. 102:119–126. 2010.(In English,
Italian). PubMed/NCBI
|
|
28
|
Pirker R, Herth FJ, Kerr KM, Filipits M,
Taron M, Gandara D, Hirsch FR, Grunenwald D, Popper H, Smit E, et
al: Consensus for EGFR mutation testing in non-small cell lung
cancer: Results from a European workshop. J Thorac Oncol.
5:1706–1713. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Travis WD, Brambilla E, Noguchi M,
Nicholson AG, Geisinger KR, Yatabe Y, Beer DG, Powell CA, Riely GJ,
Van Schil PE, et al: International association for the study of
lung cancer/American thoracic society/European respiratory society
international multidisciplinary classification of lung
adenocarcinoma. J Thorac Oncol. 6:244–285. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Westwood M, Joore M, Whiting P, van Asselt
T, Ramaekers B, Armstrong N, Misso K, Severens J and Kleijnen J:
Epidermal growth factor receptor tyrosine kinase (EGFR-TK) mutation
testing in adults with locally advanced or metastatic non-small
cell lung cancer: A systematic review and cost-effectiveness
analysis. Health Technol Assess. 18:1–166. 2014. View Article : Google Scholar
|
|
31
|
Keedy VL, Temin S, Somerfield MR, Beasley
MB, Johnson DH, McShane LM, Milton DT, Strawn JR, Wakelee HA and
Giaccone G: American Society of Clinical Oncology provisional
clinical opinion: Epidermal growth factor receptor (EGFR) Mutation
testing for patients with advanced non-small-cell lung cancer
considering first-line EGFR tyrosine kinase inhibitor therapy. J
Clin Oncol. 29:2121–2127. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Krawczyk P, Chorostowska-Wynimko J,
Dziadziuszko R, Jassem J, Krzakowski M, Langfort R, Puacz E, Wasąg
B and Wojas-Krawczyk K: Methodological recommendations for the
diagnostics of EGFR gene mutations and ALK gene rearrangement in
the selection of non-small-cell lung cancer patients to molecularly
targeted therapies. Pneumonol Alergol Pol. 82:437–444. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Krawczyk P, Ramlau R, Chorostowska-Wynimko
J, Powrózek T, Lewandowska MA, Limon J, Wasąg B, Pankowski J,
Kozielski J, Kalinka-Warzocha E, et al: The efficacy of EGFR gene
mutation testing in various samples from non-small cell lung cancer
patients: A multicenter retrospective study. J Cancer Res Clin
Oncol. 141:61–68. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ramlau R, Cufer T, Berzinec P,
Dziadziuszko R, Olszewski W, Popper H, Bajcic P, Dušek L,
Zbozinkova Z and Pirker R: INSIGHT study team: Epidermal growth
factor receptor mutation-positive non-small-cell lung cancer in the
real-world setting in central Europe: The INSIGHT Study. J Thorac
Oncol. 10:1370–1374. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Oken MM, Creech RH, Tormey DC, Horton J,
Davis TE, McFadden ET and Carbone PP: Toxicity and response
criteria of the Eastern Cooperative Oncology Group. Am J Clin
Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
R Development Core Team: R: A language and
environment for statistical computingR Foundation for Statistical
Computing. Vienna: 2014
|
|
37
|
Santini D, Barni S, Intagliata S, Falcone
A, Ferraù F, Galetta D, Moscetti L, La Verde N, Ibrahim T, Petrelli
F, et al: Natural history of non-small-cell lung cancer with bone
metastases. Sci Rep. 5:186702015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Petrelli F, Borgonovo K, Cabiddu M and
Barni S: Efficacy of EGFR tyrosine kinase inhibitors in patients
with EGFR-mutated non-small-cell lung cancer: A meta-analysis of 13
randomized trials. Clin Lung Cancer. 13:107–114. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Barlesi F, Mazieres J, Merlio JP,
Debieuvre D, Mosser J, Lena H, Ouafik L, Besse B, Rouquette I,
Westeel V, et al: Routine molecular profiling of patients with
advanced non-small-cell lung cancer: Results of a 1-year nationwide
programme of the French Cooperative Thoracic Intergroup (IFCT).
Lancet. 387:1415–1426. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Beau-Faller M, Prim N, Ruppert AM,
Nanni-Metéllus I, Lacave R, Lacroix L, Escande F, Lizard S, Pretet
JL, Rouquette I, et al: Rare EGFR exon 18 and exon 20 mutations in
non-small-cell lung cancer on 10 117 patients: A multicentre
observational study by the French ERMETIC-IFCT network. Ann Oncol.
25:126–131. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Powrózek T, Krawczyk P, Ramlau R, Sura S,
Wojas-Krawczyk K, Kucharczyk T, Walczyna B, Szumiło J,
Szyszka-Barth K, Milecki P, et al: EGFR gene mutations in patients
with adenosquamous lung carcinoma. Asia Pac J Clin Oncol.
10:340–345. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Krawczyk P, Nicoś M, Ramlau R, Powrózek T,
Wojas-Krawczyk K, Sura S, Jarosz B, Szumiło J, Warda E,
Mazurkiewicz T, et al: The incidence of EGFR-activating mutations
in bone metastases of lung adenocarcinoma. Pathol Oncol Res.
20:107–112. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lee CK, Brown C, Gralla RJ, Hirsh V,
Thongprasert S, Tsai CM, Tan EH, Ho JC, da Chu T, Zaatar A, et al:
Impact of EGFR inhibitor in non-small cell lung cancer on
progression-free and overall survival: A meta-analysis. J Natl
Cancer Inst. 105:595–605. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Girard N, Sima CS, Jackman DM, Sequist LV,
Chen H, Yang JC, Ji H, Waltman B, Rosell R, Taron M, et al:
Nomogram to predict the presence of EGFR activating mutation in
lung adenocarcinoma. Eur Respir J. 39:366–372. 2012. View Article : Google Scholar : PubMed/NCBI
|