Introduction
Dislocation of the temporomandibular joint (TMJ) is
defined as an excessive forward movement of the condyle beyond the
articular eminence with complete separation of the articular
surfaces and fixation in that position (1). Although dislocation or subdislocation of
the TMJ is typically bilateral, it may be unilateral and cause
occlusal abnormality (2). TMJ
dislocation is typically associated with hypermobility of the
mandible and poor development of the articular fossa (1,2). The
differential diagnosis for diseases leading to malocclusion and/or
dislocation in this region includes dental malocclusion without
skeletal anomalies, skeletal malocclusion, articular disc
displacement, thickness of the retrodiscal tissue, trauma,
infection, arthritis, tumor or tumor-like lesions, and
neuromuscular diseases (3,4). TMJ dislocation is rarely associated with
tumor or tumor-like lesions, and cases of metastasis-induced TMJ
dislocation are extremely rare (5).
The 5-year survival rate of pancreatic cancer (PC)
was reported to be no more than 5% in China (6) and the USA (7). Patients with PC often exhibit no
symptoms in the early stage, and the early clinical symptoms of PC
that are present are typically non-specific, including back and
shoulder pain, dyspepsia, dysphagia, changes in bowel habits and
lethargy (8). Therefore, patients
with PC are often diagnosed at an advanced stage and distant
metastases are occasionally detected at the initial diagnosis
(8). The most frequent metastatic
sites are the liver and peritoneum, followed by the lungs (9). PC rarely metastasizes to the head and
neck region, and there are few reports in the English literature of
PC metastasizing to the mandibular condyle (10).
The current report presents a case of TMJ
dislocation caused by PC metastasis, and discusses this in the
context of literature on occlusal abnormality and/or TMJ
dislocation due to metastasis.
Case report
An 85-year-old female was referred to the Department
of Dentistry and Oral Surgery, the University of Fukui Hospital
(Fukui, Japan) in January 2012 presenting with trismus, mandibular
deviation toward the left side, and spontaneous pain in the right
auricular and buccal region for 3 months. Physical examination
revealed trismus and facial asymmetry due to mandibular deviation
toward the left side and right preauricular depression. Panoramic
radiography and lateral oblique transcranial projection revealed
anterior displacement of the right mandibular condyle, whereas the
left condyle was located in the mandibular fossa (Figs. 1 and 2).
The patient was diagnosed with right temporomandibular dislocation
upon presentation to the Department of Dentistry and Oral Surgery,
the University of Fukui Hospital, and reduction of the dislocation
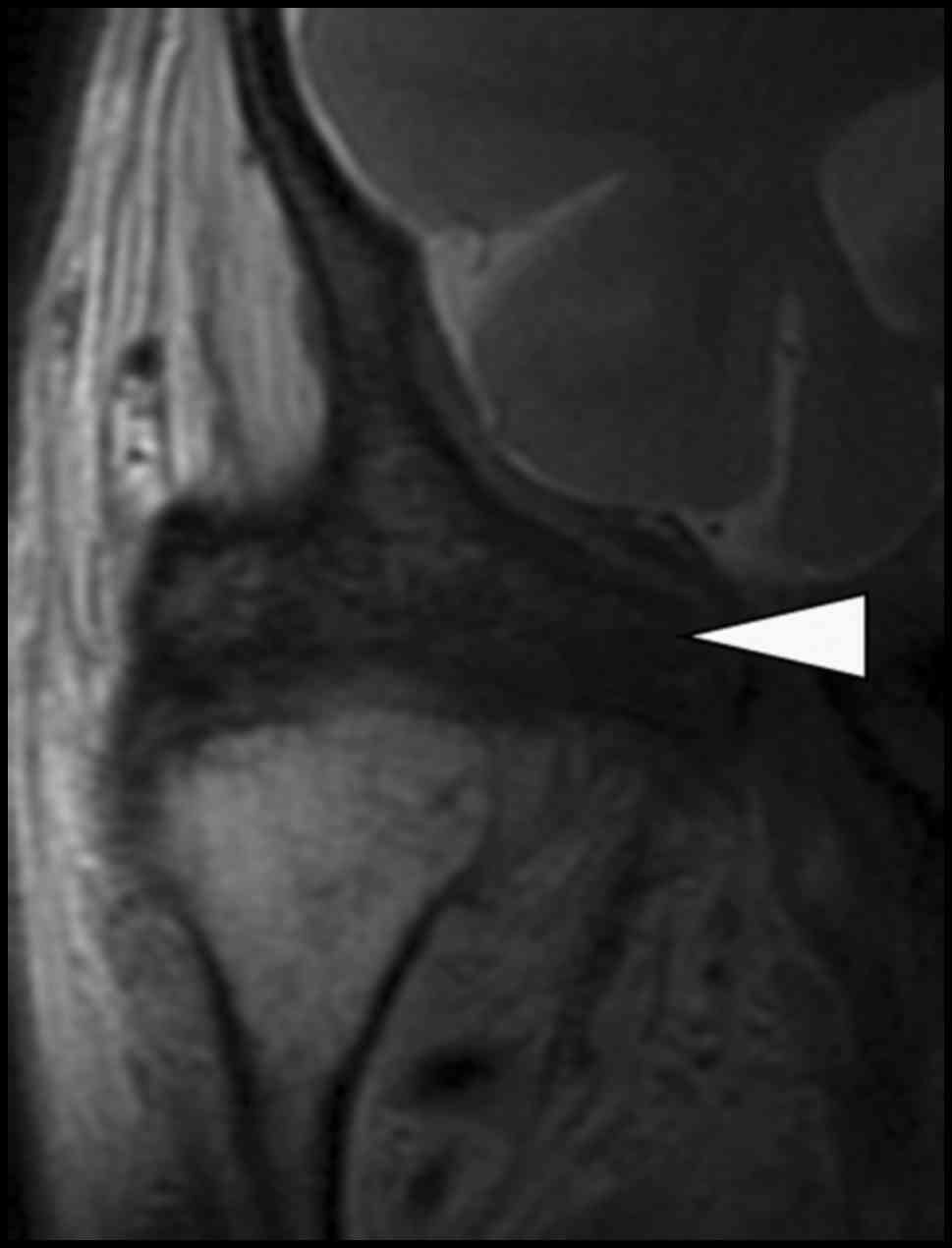
was unsuccessfully attempted. Magnetic resonance imaging (MRI)
revealed a tumorous lesion extending from the right temporal muscle
to the right sphenoid bone, right temporomandibular dislocation and
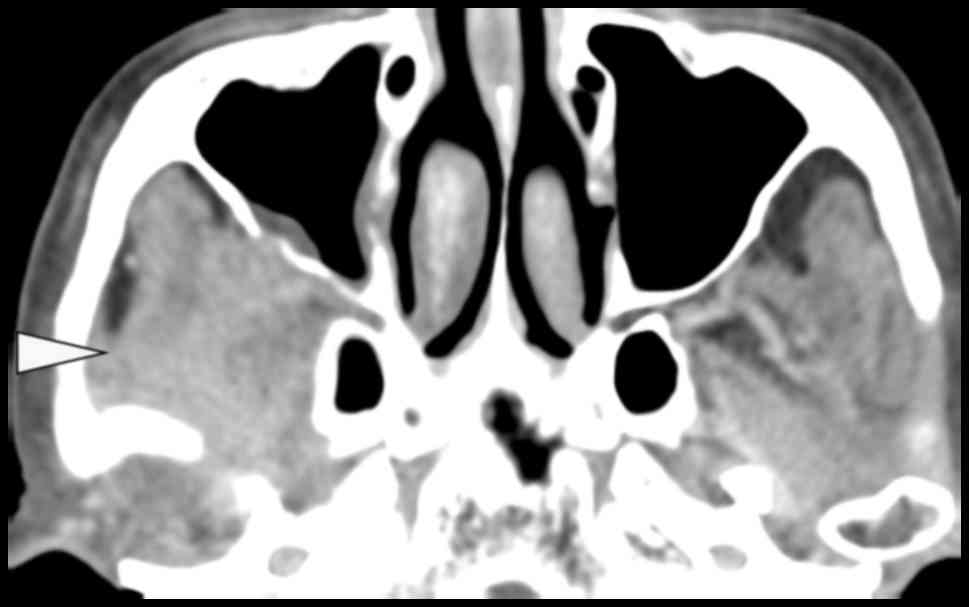
anterior displacement of the right articular disc (Fig. 3). Enhanced computed tomography (CT)
revealed a tumorous lesion from the right temporal muscle to the
right pterygoid muscles, and intracranial and orbital extension was
observed (Fig. 4). Three-dimensional
CT using the OsiriX program (version 4.1.2; Pixmeo SARL, Geneva,
Switzerland) demonstrated dislocation of the right TMJ (Fig. 5) (11).
Technetium-99 m methylene diphosphonate and gallium-67 citrate
scintigraphy showed abnormally increased uptake in the right
temporal and sphenoidal regions and multiple sites throughout the
body, including the skull bones, upper and lower jaw, vertebrae,
ribs, scapula, sternum and pelvic bone, and in each femur (Fig. 6). An enhanced CT scan of the chest and
abdomen revealed a 4-cm nodule in the tail of the pancreas and a
hypoenhanced mass in the liver (Fig.
7). Laboratory examination revealed increased C-reactive
protein (0.89 mg/dl; normal range, <0.32 mg/dl),
carcinoembryonic antigen (CEA; 83.5 ng/ml; normal range, <5.0
ng/ml), carbohydrate antigen 19-9 (CA19-9; 52,541.7 U/ml; normal
range, <37.0 U/ml) and DUPAN-2 (2,660 U/ml; normal range, 0–150
U/ml), which are tumor markers of gastrointestinal cancer and PC.
Therefore, the patient was diagnosed with PC with multiple
metastases by a gastroenterologist in the Department of
Gastroenterology, the University of Fukui Hospital. In addition,
the patient was diagnosed with PC metastasis-associated dislocation
of the TMJ. The patient and the patient's family chose not to
undergo further examinations, including biopsy. Chemotherapy and
palliative therapy were proposed instead of surgery due to the age
and general condition of the patient and the progression of the
lesion. The patient opted for palliative therapy and was discharged
from hospital and succumbed to cachexia 2 months after initially
presenting with disease.
Written informed consent for the publication of this
case report and associated images was obtained from the patient's
family.
Discussion
Kolokythas et al (10) reported in their review article that
metastasis to the oral cavity is rare in PC, with an incidence of
1–8%, and metastasis to the TMJ is extremely rare. Approximately
33% of cases of previously undiscovered primary tumor presented
with oral metastasis as the first indication (10). According to the literature on 796
cases of oral and maxillofacial metastases, the most common
metastatic site was the mandible (283/796 cases, 35.6%), and only
39/796 cases (4.9%) were of metastasis to the mandibular condyle
(12). A review of the literature
from between 1954 and 2013 identified 66 cases of metastasis to the
TMJ (29 males, 35 females and 2 of unknown gender; age range, 32–85
years; mean age ± standard deviation, 59.0±11.4 years); pain and/or
swelling were common clinical symptoms in these patients (13).
Rubin et al (14) reported that symptoms of TMJ
dysfunction, including pain, trismus and mandibular deviation,
coupled with swelling and radiographic evidence of a destructive
lesion or pathological fracture, may suggest the presence of a
malignancy, either primary or metastatic. A tumor occurring in the
TMJ often obstructs the opening of the jaws; however, in the
present study, the tumor in the mandibular fossa caused TMJ
dislocation by pushing the condyle out of the fossa (3). The literature review revealed 11 cases
of occlusal abnormality and/or TMJ dislocation due to metastasis (5
males and 6 females; age range, 49–85 years; mean age ± standard
deviation, 63.7±9.6 years), 4 of which were cases of TMJ
dislocation (Table I) (5,14–23). Condylar destruction, including
pathological fracture, was often observed using conventional
radiography in cases of occlusal abnormality, whereas it was not
observed in cases of TMJ dislocation (16–18,22).
Smolka et al (20) reported a
case of TMJ dislocation due to synovial metastasis without
destructive bone changes, in which a tumorous lesion was revealed
using MRI. In the present study, unilateral TMJ dislocation was
suspected when the patient initially presented, since destructive
bone changes were not observed using conventional radiography and
MRI revealed a tumorous lesion. The present study highlights the
importance of considering whether a malignant disease is present in
cases of occlusal abnormality and/or dislocation of the TMJ, and
suggests that, in patients with TMJ dislocation that cannot easily
be repositioned, additional imaging examinations, including MRI,
should be performed as soon as possible, regardless of whether
destructive bone changes are observed.
 | Table I.Cases of OA and/or TMJ dislocation due
to metastasis. |
Table I.
Cases of OA and/or TMJ dislocation due
to metastasis.
| Authors | Year | Patient sex | Patient age,
years | Primary lesion
site | Pathological
diagnosis | OA | Dislocation of
TMJ | Condylar destruction
on conventional radiographs | Additional imaging
examination | (Refs.) |
|---|
| Butler | 1975 | F | 49 | N.A. | N.A. | (+) | N.A. | N.A. | N.A. | (15) |
| Jagger et
al | 1978 | M | 63 | N.A. | Multiple myeloma | (+) | N.A. | (+), pathological
fracture | N.A. | (16) |
| Giles and
McDonald | 1982 | F | 55 | Rectum | Adenocarcinoma | (+) | N.A. | (+), pathological
fracture | Scintigraphy | (17) |
| Rubin et
al | 1989 | F | 67 | N.A. | Adenocarcinoma | N.A. | (+) | (−) | CT, scintigraphy | (14) |
| Stavropoulos and
Ord | 1993 | F | 55 | Breast | Adenocarcinoma | (+) | N.A. | (+), pathological
fracture | CT | (18) |
| Meneghini et
al | 2002 | F | 63 | Sacrococcygeal
region | Chordoma | (+) | N.A. | (+) | CT | (19) |
| Smolka et
al | 2004 | M | 67 | Stomach | Adenocarcinoma | N.A. | (+) | (−) | CT, MRI | (20) |
| Sari et
al | 2006 | M | 65 | Lung | Squamous cell
carcinoma | N.A. | (+) | N.A. | CT, MRI | (21) |
| Boniello et
al | 2008 | M | 60 | Lung | Adenocarcinoma | N.A. | (+) | N.A. | N.A. | (5) |
| Kruse et
al | 2010 | M | 85 | Thyroid
glanda | N.A. | (+) | N.A. | (+), pathological
fracture | PET-CT | (22) |
| Scolozzi et
al | 2012 | F | 72 | Lung | Large cell
carcinoma | (+) | N.A. | (+) | CT, MRI,
PET-CT | (23) |
| Present study |
| F | 85 | Pancreasa | N.A. | N.A. | (+) | (−) | CT, MRI,
scintigraphy | – |
In cases of metastasis to the TMJ, the most common
primary site was the breast and the most common histological type
of tumor was adenocarcinoma (13).
Metastasis to the TMJ was typically associated with generalized
skeletal metastasis in the final stage of malignancy, and mortality
occurred in the majority of patients within 1 year after the
diagnosis of metastasis (24). The
mechanism underlying metastasis to the mandible is considered to be
hematogenous spread, since there is no lymphatic system in the jaw
bone (10,24). Metastases are more likely to occur in
regions with increased red marrow concentration since malignant
cells become lodged in red marrow as the initial site for skeletal
metastasis, or occur in regions with abrupt angulation of the
vessel due to the decelerated blood flow, which aids the deposition
of malignant cells (25,26). In previous studies, the majority of
mandibular metastases (53%) occurred in the molar and premolar
regions where red marrow was present and blood flow was decelerated
(12,26). By contrast, metastasis to the
mandibular condyle rarely occurs due to a lack of substantial
hematopoietic marrow and limited local blood supply (10). In addition, synovial metastases, among
which the knee is the most common site, appear to be rare (27). The normal synovium contains blood and
lymphatic vessels. Therefore, this tissue could be associated with
metastasis (27). However, the
majority of synovial metastases are reportedly the direct extension
of bone metastases into the adjacent joint, while hematogenous
metastasis is rare (27). McConnell
et al (27) reported that
synovial metastases occurred following knee arthroplasty in 2
patients with gastrointestinal cancer. Hematogenous metastasis to
the mandible and synovial membrane may occur through the Batson
venous plexus (28).
CEA, CA19-9 and DUPAN-2 are recognized markers for
PC (29,30). Ni et al (29) reported that the sensitivity of CA19-9
alone was 80%, and that the specificity of CEA combined with CA19-9
was 84% in the diagnosis of PC. Furthermore, the median survival
time of patients with a CA19-9 serum level ≥1,000 U/ml was 6 months
(29). Goonetilleke and Siriwardena
(30) reported that the sensitivity
and specificity of CA19-9 for diagnosing PC were 79 and 82%,
respectively, and those of DUPAN-2 were 65 and 80%, respectively.
Furthermore, a CA19-9 serum level >40 U/ml with positive or
equivocal radiological findings was highly suggestive of a
diagnosis of PC (30). In the present
study, the serum levels of tumor markers specific for PC (CEA,
CA19-9 and DUPAN-2) were increased beyond the normal range. These
results were consistent with those of the imaging examinations, and
suggested that PC was present.
To conclude, the present study suggested that
healthcare professionals should consider whether a malignancy is
present in cases of occlusal abnormality and/or TMJ dislocation,
and that, in patients with TMJ dislocation that cannot easily be
repositioned, additional imaging examinations, including MRI,
should be performed as soon as possible, regardless of whether
there are destructive bone changes. Metastasis to the TMJ is
typically associated with generalized skeletal metastasis in the
final stage of malignancy (24); in
the present case, destructive changes to the cervical spine due to
metastasis was observed on the CT scan shortly before the patient
succumbed to the disease. Therefore, it is necessary to consider
the possibility of cervical spine metastasis in order to decrease
the risk of cervical fracture when attempting reduction of a TMJ
dislocation, particularly in patients with a history of cancer.
References
|
1
|
Vasconcelos BC and Porto GG: Treatment of
chronic mandibular dislocations: A comparison between eminectomy
and miniplates. J Oral Maxillofac Surg. 67:2599–2604. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cardoso AB, Vasconcelos BC and Oliveira
DM: Comparative study of eminectomy and use of bone miniplate in
the articular eminence for the treatment of recurrent
temporomandibular joint dislocation. Braz J Otorhinolaryngol.
71:32–37. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Brustowicz KA and Padwa BL: Malocclusion
in children caused by temporomandibular joint effusion. Int J Oral
Maxillofac Surg. 42:1034–1063. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hasegawa T, Shibuya Y, Minamikawa T and
Komori T: Two cases of posterior open bite caused by the thickness
of retrodiscal tissue in the temporomandibular joint. Int J Oral
Maxillofac Surg. 43:1104–1107. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Boniello R, Gasparini G, D'Amato G, Di
Petrillo A and Pelo S: TMJ metastasis: A unusual case report. Head
Face Med. 4:82008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Luo J, Xiao L, Wu C, Zheng Y and Zhao N:
The incidence and survival rate of population-based pancreatic
cancer patients: Shanghai Cancer Registry 2004–2009. PLoS One.
8:e760522013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jemal A, Siegel R, Ward E, Hao Y, Xu J and
Thun MJ: Cancer statistics, 2009. CA Cancer J Clin. 59:225–249.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Keane MG, Horsfall L, Rait G and Pereira
SP: A case-control study comparing the incidence of early symptoms
in pancreatic and biliary tract cancer. BMJ Open. 4:e0057202014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rao R, Sadashiv SK, Goday S and Monga D:
An extremely rare case of pancreatic cancer presenting with
leptomeningeal carcinomatosis and synchronous intraparenchymal
brain metastasis. Gastrointest Cancer Res. 6:90–92. 2013.PubMed/NCBI
|
|
10
|
Kolokythas A, Miloro MB, Olsson AB and
Miloro M: Metastatic pancreatic adenocarcinoma to the mandibular
condyle: A rare clinical presentation. J Oral Maxillofac Surg.
72:83–88. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Osman R and Antoine R: Open-source
software in medical imaging: Development of OsiriX. Int J CARS.
1:187–196. 2006. View Article : Google Scholar
|
|
12
|
Shen ML, Kang J, Wen YL, Ying WM, Yi J,
Hua CG, Tang XF and Wen YM: Metastatic tumors to the oral and
maxillofacial region: A retrospective study of 19 cases in West
China and review of the Chinese and English literature. J Oral
Maxillofac Surg. 67:718–737. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pretzl C, Lübbers HT, Grätz KW and Kruse
AL: Metastases in the temporomandibular joint: A review from 1954
to 2013. Rare causes for temporomandibular disorders. Swiss Dent J.
124:1067–1083. 2014.(In French, German).
|
|
14
|
Rubin MM, Jui V and Cozzi GM: Metastatic
carcinoma of the mandibular condyle presenting as temporomandibular
syndrome. J Oral Maxillofac Surg. 47:507–510. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Butler JH: Myofascial pain dysfunction
syndrome involving tumor metastasis. Case report. J Periodontol.
46:309–311. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jagger RG, Helkimo M and Carlsson GE:
Multiple myeloma involving the temporomandibular joint: Report of
case. J Oral Surg. 36:557–559. 1978.PubMed/NCBI
|
|
17
|
Giles DL and McDonald PJ: Pathologic
fracture of mandibular condyle due to carcinoma of the rectum. Oral
Surg Oral Med Oral Pathol. 53:247–249. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Stavropoulos MF and Ord RA: Lobular
adenocarcinoma of breast metastatic to the mandibular condyle.
Report of a case and review of the literature. Oral Surg Oral Med
Oral Pathol. 75:575–578. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Meneghini F, Castellani A, Camelin N and
Zanetti U: Metastatic chordoma to the mandibular condyle: An
anterior surgical approach. J Oral Maxillofac Surg. 60:1489–1493.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Smolka W, Brekenfeld C, Büchel P and
Iizuku T: Metastatic adenocarcinoma of the temporomandibular joint
from the cardia of the stomach: A case report. Int J Oral
Maxillofac Surg. 33:713–715. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sari M, Serin GM, Inanli S and Kaya H:
Condylar metastasis involoving TMJ and TMJ dislocation presenting
as the initial manifestation of squamous lung cancer. Oral Oncol
Extra. 42:224–226. 2006. View Article : Google Scholar
|
|
22
|
Kruse AL, Luebbers HT, Obwegeser JA,
Edelmann L and Graetz KW: Temporomandibular disorders associated
with metastases to the temporomandibular joint: a review of the
literature and 3 additional cases. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 110:e21–e28. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Scolozzi P, Becker M and Lombardi T:
Mandibular condylar metastasis mimicking acute internal derangement
of the temporomandibular joint. J Can Dent Assoc.
78:c772012.PubMed/NCBI
|
|
24
|
Zachariades N: Neoplasms metastatic to the
mouth, jaws and surrounding tissues. J Craniomaxillofac Surg.
17:283–290. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Basu S and Alavi A: Bone marrow and not
bone is the primary site for skeletal metastasis: Critical role of
[18F]fluorodeoxyglucose positron emission tomography in this
setting. J Clin Oncol. 25:12972007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Banerjee SC: Metastasis to the mandible.
Oral Surg Oral Med Oral Pathol. 23:71–77. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
McConnell M, Kumar R, Amini B, Lin PP and
Wang WL: Calcified synovial metastasis in the knee from renal cell
carcinoma: A case report. Skeletal Radiol. 46:123–127. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Batson OV: The function of the vertebral
veins and their role in the spread of metastases. Ann Surg.
112:138–149. 1940. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ni XG, Bai XF, Mao YL, Shao YF, Wu JX,
Shan Y, Wang CF, Wang J, Tian YT, Liu Q, et al: The clinical value
of serum CEA, CA19-9, and CA242 in the diagnosis and prognosis of
pancreatic cancer. Eur J Surg Oncol. 31:164–169. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Goonetilleke KS and Siriwardena AK:
Systematic review of carbohydrate antigen (CA 19-9) as a
biochemical marker in the diagnosis of pancreatic cancer. Eur J
Surg Oncol. 33:266–270. 2007. View Article : Google Scholar : PubMed/NCBI
|