Introduction
Although parathyroid neoplasms are common and often
cause primary hyperparathyroidism (pHPT), parathyroid carcinoma
(PC) isa rare endocrine malignancy, and accounts for <1% of
cases of pHPT (1). To date, >1,000
cases of PC have been identified in the English literature
(2–4);
however, there have been no nation-wide large-sample studies in
China, and the majority of the available studies are case reports
and literature reviews.
The histopathological distinction between benign and
malignant parathyroid tumors is often difficult, with up to 50% of
patients presenting with metastases following an initial diagnosis
of benign disease (5,6). It is of great importance to raise
awareness of PC in order to reduce its misdiagnosis and to improve
its cure rate and prognosis. In the present study, a systematic
review of Chinese language literature on PC was performed, and 8
cases of PC diagnosed and treated at the Department of Thyroid
Surgery of The First Hospital of Jilin University (Changchun,
China) were included.
As PC is resistant to radiotherapy and chemotherapy,
en bloc resection of the tumor is usually recommended; however,
there is dispute over whether the prophylactic removal of the
ipsilateral central compartment lymph nodes and other regional
tissues or organs should be performed (3,6–8). Therefore, clinical evaluation, including
preoperative examination and intraoperative judgement by the
surgeon, are key factors on which the clinical outcome relies.
Adjuvant therapy, including chemo-, radio- or anti-parathyroid
hormone (PTH) immunotherapy has also been investigated, but the
data are limited (3,7,9–11). Therefore, radical resection remains
the standard regimen. For recurrent disease, surgery is also
recommended as the primary treatment strategy, and the majority of
patients with PC require multiple surgeries (3,7).
Throughout the English literature, >1,000 cases
of PC have been identified (2–4). However,
a systematic study on a large Chinese cohort is not available,
despite the fact that a large number of cases have been described
(12–17). Due to a lack of histopathological
markers that differentiate malignant from benign parathyroid
tumors, up to 50% of patients with metastases have been
misdiagnosed initially with benign disease (5,6).
Therefore, it is necessary to raise awareness and improve general
understanding of PC.
In the present study, 234 cases of PC archived in
three commonly used databases in China, or diagnosed and treated in
the Department of Thyroid Surgery of The First Hospital of Jilin
University, were reviewed in order to summarize the
clinicopathological features relevant to the diagnosis and
prognosis of this disease, and the current optimal treatment
strategy.
Materials and methods
Patient selection
A total of three major databases in China, VIP
Journal Integration Platform (qikan.cqvip.com), China Knowledge Resource Integrated
Database (www.cnki.net), and Wanfang Data
(www.wanfangdata.com.cn), were searched
(2 December 2015) using the key words ‘parathyroid cancer’ and
‘parathyroid tumor’. Subsequent to removing duplicate records or
those with incomplete information, a final list of archived cases
(n=226) from across China, and which contained detailed
information, were obtained. These cases were then combined with the
8 cases of PC that had been diagnosed and managed in The First
Hospital of Jilin University, and analyzed in the present
retrospective study. All cases included in the present study were
in one of the following categories: i) Patients who were diagnosed
with parathyroid cancer (18)
[including patients who exhibited macroscopic evidence of a
parathyroid tumor with a fibrotic capsule and surrounding
adhesions, and for whom the histopathological criteria for
parathyroid cancer (trabecular pattern, thick fibrous trabeculae,
mitotic figures, capsular or vascular invasion and/or lymph node
invasion) were subsequently confirmed; patients with a locally
invasive tumor; and/or patients with distant metastasis]; or ii)
patients who developed local recurrence or nodal and/or distant
metastases, and who were initially classified as having benign
disease on histology during follow-up (5,6). All the
identified cases were from large teaching hospitals affiliated to
medical universities in China.
Data extraction
The physical and clinicopathological features that
were retrieved for the patients included sex, age, preoperative
symptoms and their duration, clinical classification, correct
diagnosis vs. incorrect diagnosis, tumor location, type of initial
surgery, intraoperative diagnosis, recurrence, follow-up (using
patient records), reoperation and outcome. Surgical treatments for
primary and recurrent tumors included parathyroidectomy and radical
resection. Parathyroidectomy was undertaken to remove the primary
tumor, and radical resection also included the ipsilateral
parathyroid glands with the surrounding hemithyroid and lymphatic
tissues, the unilateral/ipsilateral central compartment and the
involved surrounding structures.
Statistical analysis
Data analyses were performed using SPSS software,
version 21.0 (IBM Corp., Armonk, NY, USA). Patients who succumbed
without PC recurrence were censored for the disease-specific
survival analysis.
The 5- and 10-year disease-free and disease-specific
survival rates were estimated using the Kaplan-Meier method, and
univariate comparisons of survival time by covariate patterns were
evaluated using a log-rank test. Cox proportional hazards analysis
was used to study the effects of prognostic factors on the
disease-free and disease-specific survival times. P<0.05 was
considered to indicate a statistically significant difference.
Results
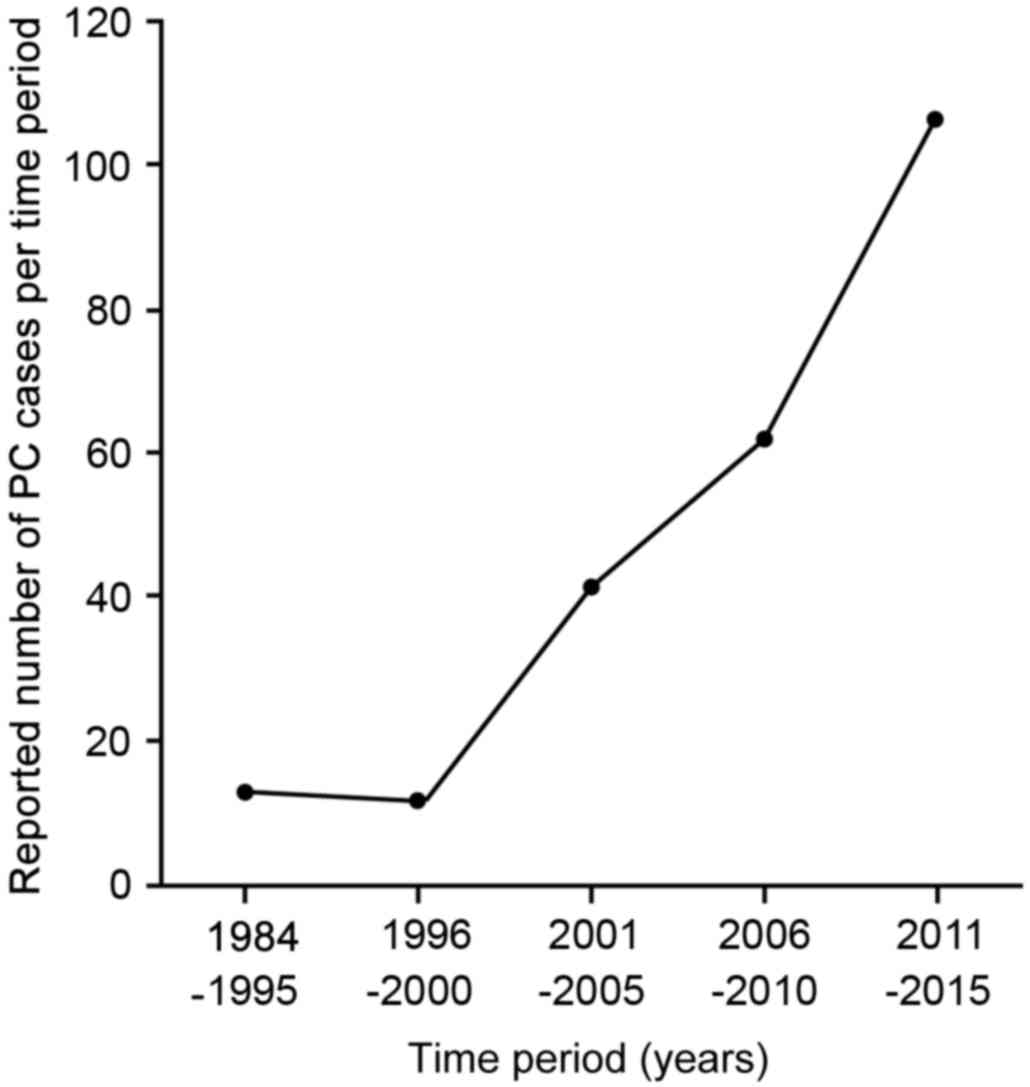
PC incidence exhibits a temporally
increasing trend
From the three databases in China, 61 PC-relevant
medical publications, including 42 case reports and 19 short
original articles from between 1984 and 2015, were identified.
These publications, in addition to the 8 cases treated at our
hospital, included a total of 234 cases of PC from 60 large
teaching hospitals affiliated to medical universities in China
(Table I). To study the diagnosis and
management of PC in China during the past 32 years, the 234 cases
were divided into 5 subgroups based on the date of diagnosis
(Fig. 1). Patients diagnosed prior to
1995 were pooled, and then those diagnosed during each subsequent
5-year interval (between 1996 and 2015) were grouped. The data
indicated an apparent increase in the number of diagnosed PC cases,
from 13 cases between 1996 and 2000 to >100 cases between 2011
and 2015 (Fig. 1).
 | Table I.Clinicopathological characteristics
of patients with parathyroid carcinoma. |
Table I.
Clinicopathological characteristics
of patients with parathyroid carcinoma.
| Variable | Value |
|---|
| Total patients,
n | 234 |
| Sex, n |
|
|
Male | 120 |
|
Female | 114 |
| Age, years |
|
|
Median | 45.5 |
|
Range | 18–78 |
| Site of primary
tumor, n |
|
| Left
upper | 10 |
| Right
upper | 19 |
| Left
lower | 91 |
| Right
lower | 114 |
| Pre-diagnosis
duration |
|
|
Mean | 19.58 months |
|
Longest | 9 years |
| Clinical
classification, n (%) |
|
| Bone
type | 93 (39.74) |
| Renal
type | 16 (6.84) |
|
Mixed | 84 (34.62) |
|
Others | 41 (17.52) |
| Cases of distant
metastasis, n (%)a | 35 |
|
Lung | 14 (40.00) |
|
Bone | 9 (25.71) |
|
Mediastinum | 1 (2.86) |
|
Multiple organs | 11 (31.43) |
| Initial surgery,
number of cases (%) |
|
| Radical
resection | 141 (60.26) |
|
Parathyroidectomy | 93 (39.74) |
| Recurrence |
|
| Total,
n | 91 |
|
Following radical
resection |
|
|
Number of
cases | 37 |
|
Disease-free
period | 36
monthsb |
|
Following
parathyroidectomy |
|
|
Number of
cases | 54 |
|
Disease-free
period | 24
monthsb |
Clinical features
Among the patients, 120 were males and 114 were
females, and the male/female ratio was ~1:1. The median age at
diagnosis was 45.5 years (range, 18–78 years). The average diameter
of the tumors was 3.21±1.16 cm, and the average disease course was
19.58 months in duration, with a maximum time prior to diagnosis of
9 years. There were various subtypes among the study population,
which included bone, renal, mixed or other subtypes, and were
defined according to the signs and symptoms of pHPT caused by PC
(18). ‘Bone subtype’ refers to
bone-associated complications, among which the most common type of
bone disease in pHPT is osteitis fibrosacystica (19), which results in pain and occasionally
pathological fractures. Other bone diseases associated with pHPT
include osteoporosis, osteomalacia and arthritis. ‘Renal subtype’
refers to kidney stones, nephrocalcinosis and diabetes insipidus
(polyuria and polydipsia); these may ultimately lead to renal
failure. The ‘mixed’ subtype consists of both the bone and renal
subtypes. Finally, the ‘other’ subtype consists of nonspecific
gastrointestinal, cardiovascular and neuromuscular dysfunction and
asymptomatic pHPT. In the present study, various clinical
classifications were identified, with the bone and mixed subtypes
accounting for 39.74 and 34.62% of cases, respectively, while 16
cases were recorded as renal and 41 cases as other subtypes. The
majority of the 234 PCs were observed in the bilateral lower
parathyroid regions, with 114 in the lower right and 91 in the
lower left, whereas there were only 29 cases exhibiting tumors in
the upper parathyroid region.
Of the 234 patients with PC, a large proportion (191
cases) were misdiagnosed prior to surgery; misdiagnoses included
rheumatoid arthritis, urinary stones, bone tumors, pathological
fractures, osteoporosis, gout, myeloma, ankylosing spondylitis,
osteomyelitis, gastroenteritis, bone tuberculosis, neurosis,
weakness, menopausal syndrome, thyroid cancer or pancreatitis.
Intraoperative diagnosis performed on the frozen sections did not
improve the diagnosis, with only 17 out of the 113 examined being
correctly diagnosed. The use of fine-needle aspirate for cytology
was prohibited in order to avoid seeding the tumor (5).
Distant metastasis occurred in 35 cases, including
10 patients who exhibited metastatic tumors prior to the first
surgery, and did not demonstrate a decrease in serum calcium
following the surgery. Metastatic tumors were identified in the
lungs (14 cases), bone (9 cases), mediastinum (1 case) and multiple
organs (11 cases).
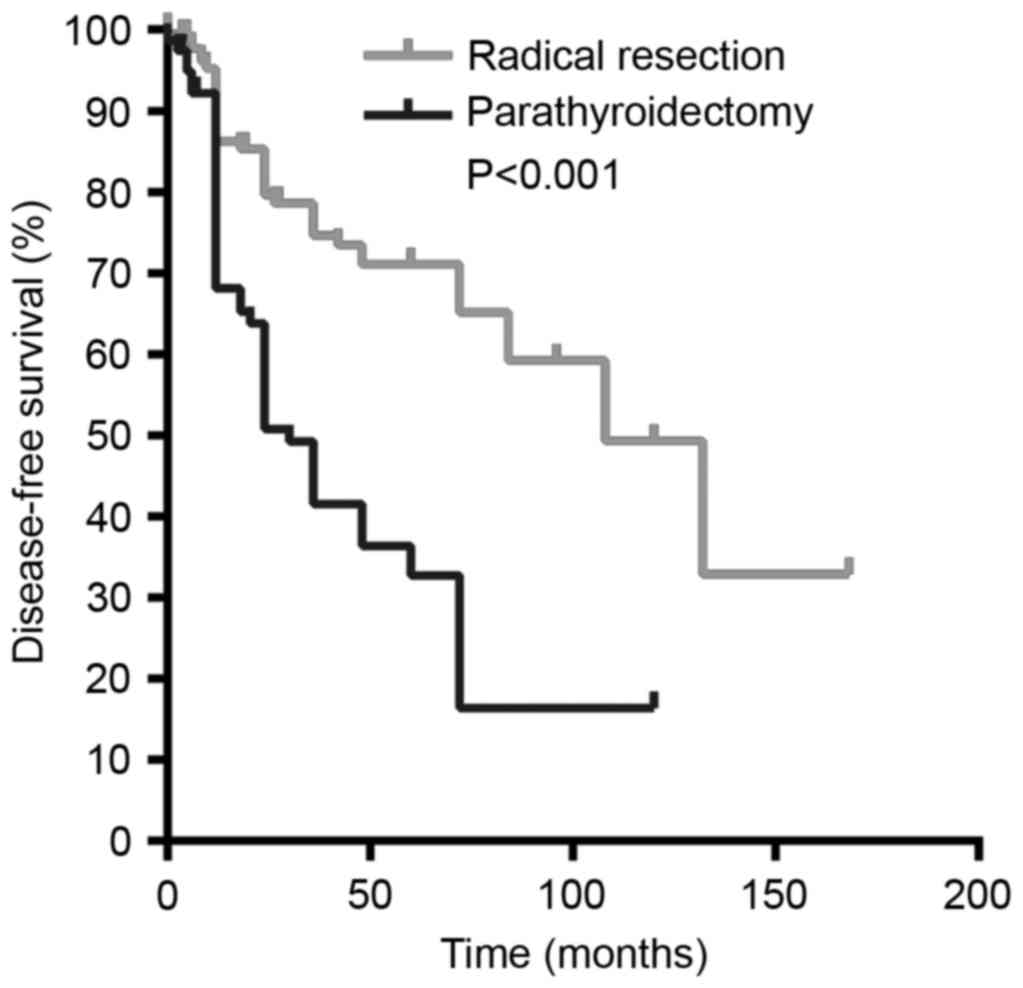
Radical resection reduces recurrence
and metastasis
Surgery was performed as the first-line therapy in
all 234 patients; 141 of them were treated by radical resection, in
which the primary tumor, ipsilateral thyroid, surrounding lymph
nodes and involved structures were completely removed. The other 93
patients were managed by parathyroidectomy or palliative resection.
The advantages of radical resection in reducing the probability of
recurrence and prolonging patient survival over other surgical
strategies were significant (log-rank, 20.956; P<0.001); the
median disease-free survival time was increased in patients treated
by radical resection compared with those treated by
parathyroidectomy (132 vs. 36 months, respectively; Fig. 2; Table
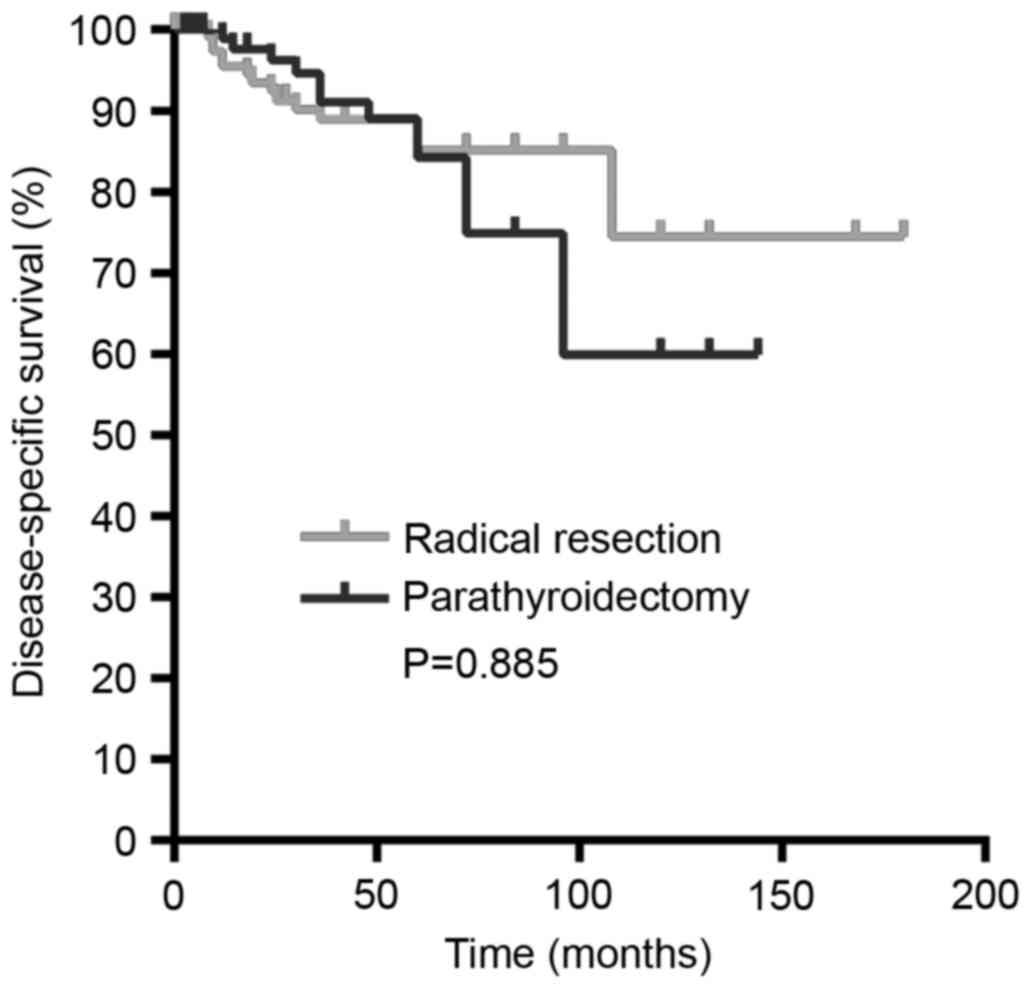
II). However, no significant variation in the disease-specific
survival between the two surgical strategies was observed
(log-rank, 0.021; P=0.885; Fig. 3;
Table III).
 | Table II.Effect of initial surgery on the
probability of recurrence. |
Table II.
Effect of initial surgery on the
probability of recurrence.
| Surgery type | Total patients,
n | Cases of
recurrence, n (%) | Pearson's
χ2 | P-value |
|---|
|
Parathyroidectomy | 87 | 54 (62.07) | 23.33 | <0.001 |
| Radical
resection | 128 | 37 (28.91) |
|
|
 | Table III.Effect of initial surgeries on the
disease-specific survival. |
Table III.
Effect of initial surgeries on the
disease-specific survival.
| Surgery type | Total patients,
n | Mortalities, n
(%) | Pearson's
χ2 | P-value |
|---|
|
Parathyroidectomy | 87 | 9 (10.34) | 0.23 | 0.885 |
| Radical
resection | 128 | 16 (12.50) |
|
|
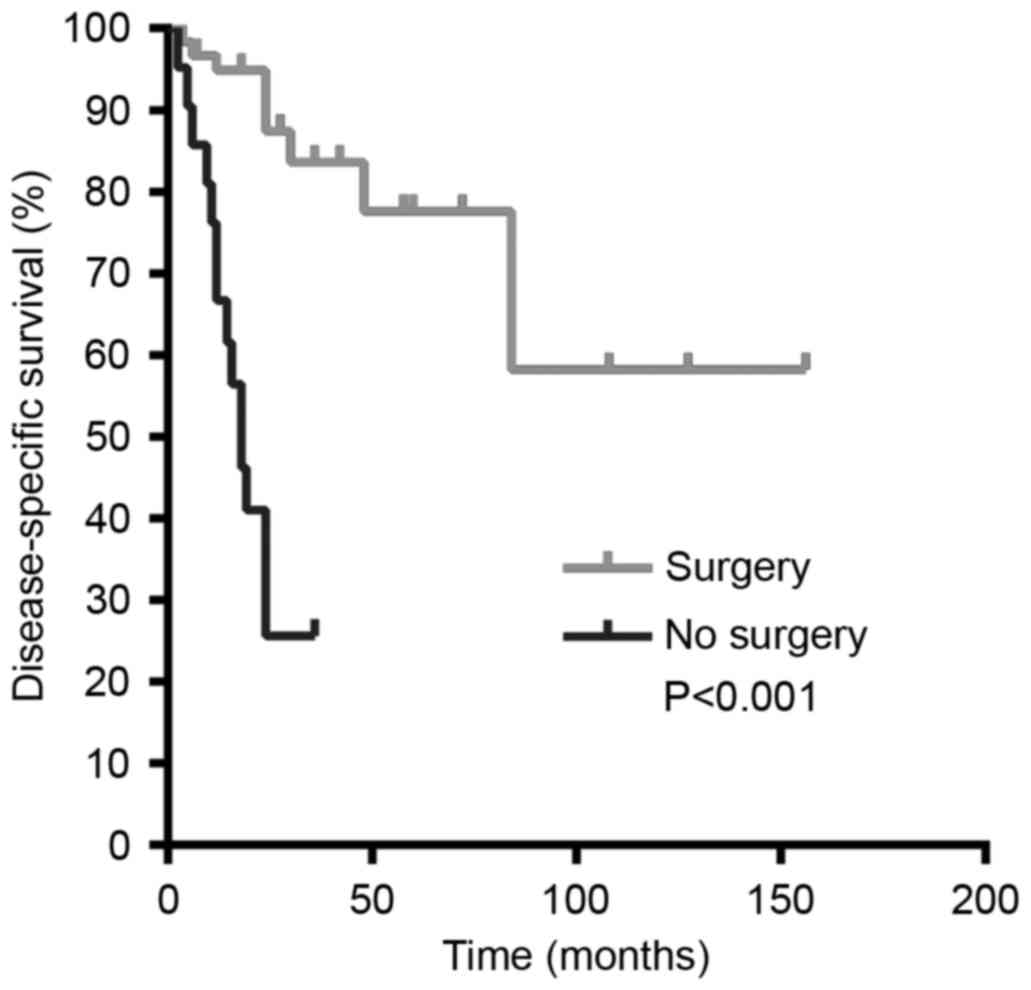
Reoperation increases survival
subsequent to PC recurrence
Of all the patients, 91 experienced recurrent PC,
with frequent involvement of the surrounding thyroid gland,
trachea, esophagus and strap muscles. Relapse occurred, on average,
at 12 months following surgery, but the longest period of time
prior to relapse was 132 months. A total of 65 patients among the
91 cases of recurrence underwent additional surgeries (8 times in
one particular case), and 46 patients responded (hypercalcemia and
elevated PTH returned to normal levels). Among all 91 cases of
recurrence, 25 patients succumbed to PC, including 11/65 in the
surgical group and 14/26 in the non-surgical group (Table IV). The data indicated that multiple
surgeries on patients with disease recurrence significantly
increased their disease-specific survival time (Fig. 4; log-rank, 35.322; P<0.001).
 | Table IV.Effects of surgical treatment
following recurrence (n=91) on patient outcomes. |
Table IV.
Effects of surgical treatment
following recurrence (n=91) on patient outcomes.
| Treatment | Total patients,
n | Mortalities, n
(%) | Pearson's
χ2 | P-value |
|---|
| Surgical | 65 | 11 (16.92) | 12.71 | <0.001 |
| Non-surgical | 26 | 14 (53.85) |
|
|
Other factors affecting recurrence and
survival following PC surgery
The effects of other factors on the disease-free
survival were assessed by log-rank test, but no statistically
significant associations were identified for age (log-rank, 0.280;
P=0.596), sex (log-rank, 3.233; P=0.072) or duration of the
preoperative period (log-rank, 0.070; P=0.792). In addition, no
significant association was observed between the disease-specific
survival and age (log-rank, 0.012; P=0.912), sex (log-rank 0.074;
P=0.786) or preoperative duration of disease (log-rank, 3.438;
P=0.064; data not shown).
To further confirm these results, sex, age,
preoperative duration, recurrence, reoperation, distant metastasis
and radical surgery were assessed for their association with PC
recurrence and survival using a multivariate Cox proportional
hazards analysis. Radical resection was found to be an independent
factor associated with decreased PC recurrence (P=0.030). Notably,
male sex was associated with an increased mortality rate compared
with female sex (P=0.040), while reoperation was associated with an
increased survival rate (P=0.030; Table
V).
 | Table V.Multivariate Cox proportional hazards
analysis. |
Table V.
Multivariate Cox proportional hazards
analysis.
|
|
|
|
|
|
| 95% CI for Exp
(B) |
|---|
|
|
|
|
|
|
|
|
|---|
| Variable | B | SE | Wald | P-value | Exp(B) | Lower | Upper |
|---|
| Survival |
|
|
|
|
|
|
|
|
Sex | −1.61 | 0.81 | 3.99 | 0.04 | 0.20 | 0.04 | 0.96 |
|
Age | 0.01 | 0.03 | 0.08 | 0.77 | 1.01 | 0.95 | 1.07 |
|
Preoperative duration | −0.25 | 0.18 | 1.88 | 0.17 | 0.78 | 0.55 | 1.11 |
|
Recurrence status | −2.44 | 131.41 | 0.00 | 0.98 | 0.08 | 0.00 | 184.90 |
|
Reoperation | −2.64 | 1.25 | 4.46 | 0.03 | 0.07 | 0.01 | 0.826 |
| Distant
metastasis | 12.27 | 100.78 | 0.02 | 0.90 | 316.12 | 0.00 | 325.28 |
| Radical
surgery | −0.09 | 0.67 | 0.02 | 0.88 | 0.90 | 0.24 | 3.38 |
| Recurrence |
|
Sex | −0.27 | 0.36 | 0.59 | 0.44 | 0.76 | 0.37 | 1.52 |
|
Age | 0.01 | 0.01 | 0.04 | 0.84 | 1.00 | 0.97 | 1.03 |
|
Preoperative duration | −0.14 | 0.13 | 1.23 | 0.26 | 0.86 | 0.67 | 1.11 |
| Radical
surgery | −0.74 | 0.35 | 4.66 | 0.03 | 0.47 | 0.23 | 0.93 |
Prognosis
Follow-up information was available for 215 cases.
The patients were followed up for ≤15 years (mean, 3.73 years), and
25 succumbed to PC. The cumulative 5- and 10-year disease-specific
survival rates were 83 and 67%, respectively.
Discussion
The rate of parathyroid cancer misdiagnosis remains
high. Since the first study investigating PC (de Quervain, 1904)
(19), >1,000 cases of this rare
cancer have been identified in the literature (2,3,8,20,21). However, the knowledge of this
malignancy remains limited, and additional studies are required to
improve understanding and increase awareness of this disease. In
the present study, 234 cases of PC that were diagnosed and managed
in 60 hospitals across China were collectively analyzed to screen
for clinicopathological features that may potentially assist in the
diagnosis and treatment of this malignancy, and to identify optimal
therapeutic strategies.
The data obtained from the present study indicated a
marked increase in the number of PC cases identified in China over
32 years (Fig. 1). This may suggest
the rising incidence of PC with industrialization, as documented
for other types of cancer (22,23), but
may be due to advances in diagnosis. The routinization of blood
calcium testing allows incidental and symptom-independent diagnosis
of hyperparathyroidism (24). Apart
from an excessive secretion of parathyroid hormone and
hypercalcemia, that clinical features that are indicative of PC
include the following: A palpable neck mass (>3 cm);
hyperparathyroidism concomitant with jaw tumor; hoarseness and/or
neck pain; an albumin-corrected calcium level >3 mmol/l;
infiltration and/or calcification visible on neck ultrasound; PTH
levels >3 times the upper limit of normal; local invasion and
metastasis observed intraoperatively or on sestamibi parathyroid
scintigraphy and/or computed tomography scans; significant bone and
kidney involvement; and a family history of hyperparathyroidism-jaw
tumor syndrome (24). The data from
the present study suggested that intraoperative diagnosis on frozen
sections did not assist in distinguishing benign from malignant
disease, which was consistent with a previous study (25). A definitive diagnosis requires
evidence of vascular invasion, perineural invasion, capsular
penetration into the adjacent structures, and metastases (26,27).
As the genetic features of the 234 patients in the
present study were not recorded and not available in the databases,
the molecular mechanisms driving tumorigenesis remain unclear. In
previous studies, >70% of cases of sporadic PC were identified
to have mutations in the cell division cycle 73 (CDC73) gene
(13,14,28).
Immunohistochemically, the loss of the expression of parafibromin
(encoded by CDC73), retinoblastoma protein, p27, Bcl-2-α,
mouse double minute 2 homolog and adenomatous polyposis coli gene,
and elevation of galectin-3, tumor protein 53 and proliferation
marker protein Ki-67 (>5%) have been demonstrated (24). In particular, parafibromin, galectin-3
and Bcl-2-α are the most useful ancillary biomarkers (29).
The present study indicates that initial radical
resection is essential to reduce the recurrence of PC. Due to the
difficulties in the diagnosis of PC, the intraoperative assessment
by the surgeon of the local invasion of surrounding structures
determines whether the lesion is malignant, and what the optimal
surgical procedure is. Therefore, the adjacent structures such as
the ipsilateral thyroid lobe and thymus, paratracheal alveolar
tissue and lymph nodes, require careful inspection and removal, if
necessary, to minimize the chance of tumor cells remaining within
the body (7,24,30). In
general, radical resection of the tumor with safe margins is the
first-line therapy of choice (31).
Among the 234 patients in the present study, 60.26% underwent
radical resection, and these patients experienced a lower rate of
recurrence compared with those who underwent parathyroidectomy only
(Table II; Fig. 2). Failure to perform radical resection
was an independent risk factor for PC recurrence (Table V). However, radical resection did not
confer an overall survival advantage for the patients compared with
parathyroidectomy (Table III;
Fig. 3). This is consistent with
previous results in which no difference in survival was observed
between simple excision and en bloc resection (7,32).
However, local resection becomes problematic when tumor spillage
and parathyromatosis are involved (30). Similarly, Koea and Shaw (6) demonstrated that en bloc resection of the
tumor at first presentation was associated with an improved local
disease control, and their data also indicated that radical
resection significantly improved long-term survival.
Recurrence of PC often occurs around 3 years after
the first surgery (7,30). Although the resection of metastatic
tumors rarely offers the possibility of cure, removal of the
recurrent or metastatic tumors relieves suffering. Patients with PC
undergo, on average, two to three surgeries during the course of
their disease (33), and extensive
neck and mediastinal exploration are recommended in cases of local
recurrence. Surgical resection is also recommended to control
hypercalcemia, particularly for those with local recurrence or
limited distant metastases (34).
Lung metastasis is common in PC, and the resection
of pulmonary metastases can result in long-term remission of PC
(1,30,35,36). When
metastasis is identified toward the lateral neck lymph nodes,
dissection of the level II–V lymph nodes should be performed. In
cases of mediastinal lymph node or limited lung involvement,
laparoscopic or open surgery should be considered (7,24,30). In the present study, a total of 329
parathyroid surgeries were performed on the 234 patients with PC
(an average of 1.41 surgeries per patient). Reoperation
significantly prolonged the survival of the patients with
recurrence (Table IV; Fig. 4). Male sex and lack of reoperation
following recurrence were independent negative risk factors for
patient survival (Table V).
In summary, in the present study, 234 PC cases
during a 32-year period in China were collected, and their
diagnosis, treatment and clinical outcomes were analyzed. The data
suggested that PC has primarily been misdiagnosed in China due to
its sporadic occurrence and the lack of awareness. Radical
resection as the first-line therapy significantly reduced the
chance of tumor recurrence. Following recurrence, reoperation
represents an ideal approach to inhibit cancer progression and
improve the clinical outcome.
Acknowledgements
The present study was financially supported by the
Department of Health, Jilin Province, China, awarded to Guang Chen
(grant no. 2010Z100).
References
|
1
|
Shane E: Clinical review 122: Parathyroid
carcinoma. J Clin Endocrinol Metab. 86:485–493. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mori H, Okada Y, Arao T and Tanaka Y: Case
of parathyroid carcinoma with a highly aggressive clinical course.
J UOEH. 36:243–249. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sadler C, Gow KW, Beierle EA, Doski JJ,
Langer M, Nuchtern JG, Vasudevan SA and Goldfarb M: Parathyroid
carcinoma in more than 1,000 patients: A population-level analysis.
Surgery. 156:1622–1630. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Asare EA, Sturgeon C, Winchester DJ, Liu
L, Palis B, Perrier ND, Evans DB, Winchester DP and Wang TS:
Parathyroid carcinoma: An update on treatment outcomes and
prognostic factors from the national cancer data base (NCDB). Ann
Surg Oncol. 22:3990–3995. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Marcocci C, Cetani F, Rubin MR, Silverberg
SJ, Pinchera A and Bilezikian JP: Parathyroid carcinoma. J Bone
Miner Res. 23:1869–1880. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Koea JB and Shaw JH: Parathyroid cancer:
Biology and management. Surg Oncol. 8:155–165. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Busaidy NL, Jimenez C, Habra MA, Schultz
PN, El-Naggar AK, Clayman GL, Asper JA, Diaz EM Jr, Evans DB, Gagel
RF, et al: Parathyroid carcinoma: A 22-year experience. Head Neck.
26:716–726. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Givi B and Shah JP: Parathyroid carcinoma.
Clin Oncol (R Coll Radiol). 22:498–507. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mohebati A, Shaha A and Shah J:
Parathyroid carcinoma: Challenges in diagnosis and treatment.
Hematol Oncol Clin North Am. 26:1221–1238. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Schott M, Feldkamp J, Schattenberg D,
Krueger T, Dotzenrath C, Seissler J and Scherbaum WA: Induction of
cellular immunity in a parathyroid carcinoma treated withtumor
lysate-pulsed dendritic cells. Eur J Endocrinol. 142:300–306. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bradwell AR and Harvey TC: Control of
hypercalcaemia of parathyroid carcinoma by immunisation. Lancet.
353:370–373. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang L, Han D, Chen W, Zhang S, Wang Z, Li
K, Gao Y, Zou S and Yang A: Non-functional parathyroid carcinoma: A
case report and review of the literature. Cancer Biol Ther.
16:1569–1576. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang J, Tong F, Zhong W and Li S: A case
report of anti-parathyroid hormone immunotherapy for parathyroid
carcinoma. J Diabetes Endocrinol. 2:36–40. 2011.
|
|
14
|
Siu WK, Law CY, Lam CW, Mak CM, Wong GW,
Ho AY, Ho KY, Loo KT, Chiu SC, Chow LT, et al: Novel nonsense CDC73
mutations in Chinese patients with parathyroid tumors. Fam Cancer.
10:695–699. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhao J, Hu Y, Liao Q, Niu Z, Xing X, Xia W
and Zhao Y: Gene identification of potential malignant parathyroid
tumors phenotype in Chinese population. Endocr J. 61:597–605. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cao J, Chen C, Wang QL, Xu JJ and Ge MH:
Parathyroid carcinoma: A report of six cases with a brief review of
the literature. Oncol Lett. 10:3363–3368. 2015.PubMed/NCBI
|
|
17
|
McClenaghan F and Qureshi YA: Parathyroid
cancer. Gland Surg. 4:329–338. 2015.PubMed/NCBI
|
|
18
|
Harari A, Waring A, Fernandez-Ranvier G,
Hwang J, Suh I, Mitmaker E, Shen W, Gosnell J, Duh QY and Clark O:
Parathyroid carcinoma: A 43-year outcome and survival analysis. J
Clin Endocrinol Metab. 96:3679–3686. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dąbrowska A, Tarach J and Zwolak A:
Primary hyperparathyroidism due to parathyroid cancer-a diagnostic
and management challenge. Endokrynol Pol. 66(150): 157–167.
2015.
|
|
20
|
Talat N and Schulte KM: Clinical
presentation, staging and long-term evolution of parathyroid
cancer. Ann Surg Oncol. 17:2156–2174. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Villar-del-Moral J, Jiménez-García A,
Salvador-Egea P, Martos-Martínez JM, Nuño-Vázquez-Garza JM,
Serradilla-Martín M, Gómez-Palacios A, Moreno-Llorente P,
Ortega-Serrano J and de la Quintana-Basarrate A: Prognostic factors
and staging systems in parathyroid cancer: A multicenter cohort
study. Surgery. 156:1132–1144. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Schwartz GG and Sahmoun AE: Ovarian cancer
incidence in the United States in relation to manufacturing
industry. Int J Gynecol Cancer. 24:247–251. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Stevens RG: Working against our endogenous
circadian clock: Breast cancer and electric lighting in the modern
world. Mutat Res. 680:106–108. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Duan K and Mete Ö: Parathyroid Carcinoma:
Diagnosis and Clinical Implications. Turk Patoloji Derg. 31 Suppl
1:S80–S97. 2015.
|
|
25
|
Kassahun WT and Jonas S: Focus on
parathyroid carcinoma. Int J Surg. 9:13–19. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
DeLellis RA: Parathyroid carcinoma: An
overview. Adv Anat Pathol. 12:53–61. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Okamoto T, Iihara M, Obara T and Tsukada
T: Parathyroid carcinoma: Etiology, diagnosis, and treatment. World
J Surg. 33:2343–2354. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gill AJ: Understanding the genetic basis
of parathyroid carcinoma. Endocr Pathol. 25:30–34. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Erovic BM, Harris L, Jamali M, Goldstein
DP, Irish JC, Asa SL and Mete O: Biomarkers of parathyroid
carcinoma. Endocr Pathol. 23:221–231. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kebebew E, Arici C, Duh QY and Clark OH:
Localization and reoperation results for persistent and recurrent
parathyroid carcinoma. Arch Surg. 136:878–885. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Munson ND, Foote RL, Northcutt RC, Tiegs
RD, Fitzpatrick LA, Grant CS, van Heerden JA, Thompson GB and Lloyd
RV: Parathyroid carcinoma: Is there a role for adjuvant radiation
therapy? Cancer. 98:2378–2384. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Owen RP, Silver CE, Pellitteri PK, Shaha
AR, Devaney KO, Werner JA, Rinaldo A and Ferlito A: Parathyroid
carcinoma: A review. Head Neck. 33:429–436. 2011.PubMed/NCBI
|
|
33
|
Obara T and Fujimoto Y: Diagnosis and
treatment of patients with parathyroid carcinoma: An update and
review. World J Surg. 15:738–744. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Qiu ZL, Wu CG, Zhu RS, Xue YL and Luo QY:
Unusual case of solitary functioning bone metastasis from a
‘parathyroid adenoma’: Imagiologic diagnosis and treatment with
percutaneous vertebroplasty-case report and literature review. J
Clin Endocrinol Metab. 98:3555–3561. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hundley JC, Albertson DA, Bradley RF and
Levine EA: Resection of pulmonary metastasis from parathyroid
carcinoma. Am Surg. 69:779–783. 2003.PubMed/NCBI
|
|
36
|
Iihara M, Okamoto T, Suzuki R, Kawamata A,
Nishikawa T, Kobayashi M and Obara T: Functional parathyroid
carcinoma: Long-term treatment outcome and risk factor analysis.
Surgery. 142:936–943.e1. 2007. View Article : Google Scholar : PubMed/NCBI
|