Introduction
Paragangliomas occur along the human body's
sympathetic and parasympathetic chains, and this type of neoplasm
may develop in various anatomical locations, with the head and neck
region being the primary site. Carotid body tumors (CBTs) derive
from the neural crest and are a relatively rare type of neck tumor
(1). A CBT located in the upper
cervical region is typically considered to be benign and develops
slowly (2); however, CBTs are
challenging for surgeons due to the spatial locations and abundant
blood supply of this type of neoplasm (3). The occurrence of CBT exhibits sporadic
or familial traits. Between 5 and 10% of bilateral CBT cases have
been reported to be of the sporadic type (4), and ≤30% of bilateral CBT cases are of
the familial form (5); however, the
specific etiology of CBT remains unknown. Previous studies have
described a mutation in six specific genes (including RET
proto-oncogene, von Hippel-Lindau tumor suppressor, neurofibromin 1
and mitochondrial complex II: Succinate dehydrogenase subunits)
(6,7)
which is associated with CBT.
Between January 2009 and May 2015, 37 patients
presenting to The First Affiliated Hospital of Zhengzhou University
(Zhengzhou, China) were diagnosed with CBT (Table I). The present case report describes a
typical patient with bilateral CBT which was surgically removed
with minimal blood loss and temporary neurological loss. In
addition, the clinical manifestations and the imaging and
pathological features of CBT were summarized. The present case
report revealed that preoperative preparation and proper surgical
technique are required to improve treatment outcome.
 | Table I.Clinical parameters of carotid body
tumors (n=37). |
Table I.
Clinical parameters of carotid body
tumors (n=37).
| Characteristic | Patients, n (%) |
|---|
| Age, years |
|
| ≥60 | 3 (8.2) |
|
<60 | 34 (91.8) |
| Sex |
|
| Male | 17 (45.9) |
|
Female | 20 (54.1) |
| Treatment method |
|
|
Observation | 13 (35.1) |
|
Surgery | 21 (56.8) |
| External
carotid artery ligation | 7 (33.3) |
| Internal
carotid artery ligation | 3 (14.3) |
| Common
artery ligation | 3 (14.3) |
| CBT
completely resection | 8 (28.1) |
|
Missing | 3 (8.1) |
| Site |
|
| Left side
of neck | 15 (40.6) |
| Right
side of neck | 16 (43.2) |
| Bilateral
of neck | 3 (8.1) |
|
Missing | 3 (8.1) |
| Smoking
history |
|
|
Non-smoker | 29 (78.4) |
|
Smoker | 3 (8.1) |
|
Missing | 5 (13.5) |
| Alcohol
consumption |
|
|
Non-drinker | 30 (81.1) |
|
Drinker | 2 (5.4) |
|
Missing | 5 (13.5) |
Case report
Materials and methods
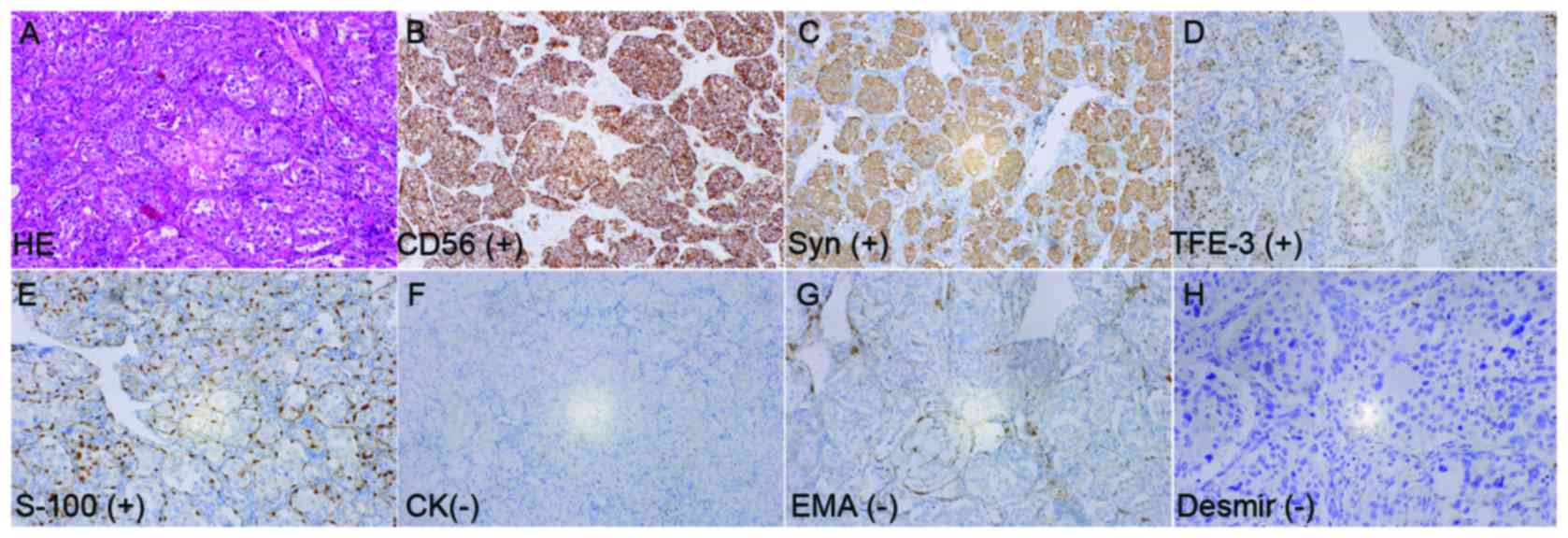
Formalin-fixed paraffin-embedded tissues were cut
into sections of 4 µm thickness. The avidin-biotin complex (ABC)
technique was used, according to the Vectastain Elite ABC kit
(Vector Laboratories, Inc., Burlingame, CA, USA). Tissue sections
were deparaffinized in xylene, rehydrated in graded ethanol,
treated with Tris-EDTA buffer for antigen retrieval and quenched in
H2O2. Tissue sections were blocked with 2.5%
normal serum at room temperature for 1 h and incubated overnight at
4°C with the following primary antibodies: Cluster of
differentiation (CD)56 (dilution, 1:400; cat. no. 3576; Cell
Signaling Technology, Inc., Danvers, MA, USA) Syn (dilution, 1:400;
cat. no. ab32127; Abcam, Cambridge, MA, USA), transcription factor
E3 (TFE3; dilution, 1:250; cat. no. ab179804; Abcam), S-100
(dilution, 1:500; cat. no. ab97051; Abcam), cytokeratin (CK;
dilution, 1:500; cat. no. ab97051; Abcam), epithelial membrane
antigen (EMA; dilution, 1:150; cat. no. ab156947; Abcam) and Demin
(dilution, 1:500; cat. no. ab97051; Abcam). Subsequently, sections
were incubated at room temperature for 1 h with biotinylated
secondary antibody (dilution, 1:400; cat. no. 8125; Cell Signaling
Technology, Inc.) and with ABC reagent. Diaminobenzidine was used
as chromogen and counterstained with Mayer's hematoxylin
(Sigma-Aldrich; Merck KGaA, Darmstadt, Germany), the results were
observed using a light microscope (magnification, ×200). The
present study was approved by the Institutional Ethics Committee
Office of The First Affiliated Hospital of Zhengzhou University.
Written informed consent was obtained from the patient for the
publication of the present case report and accompanying images.
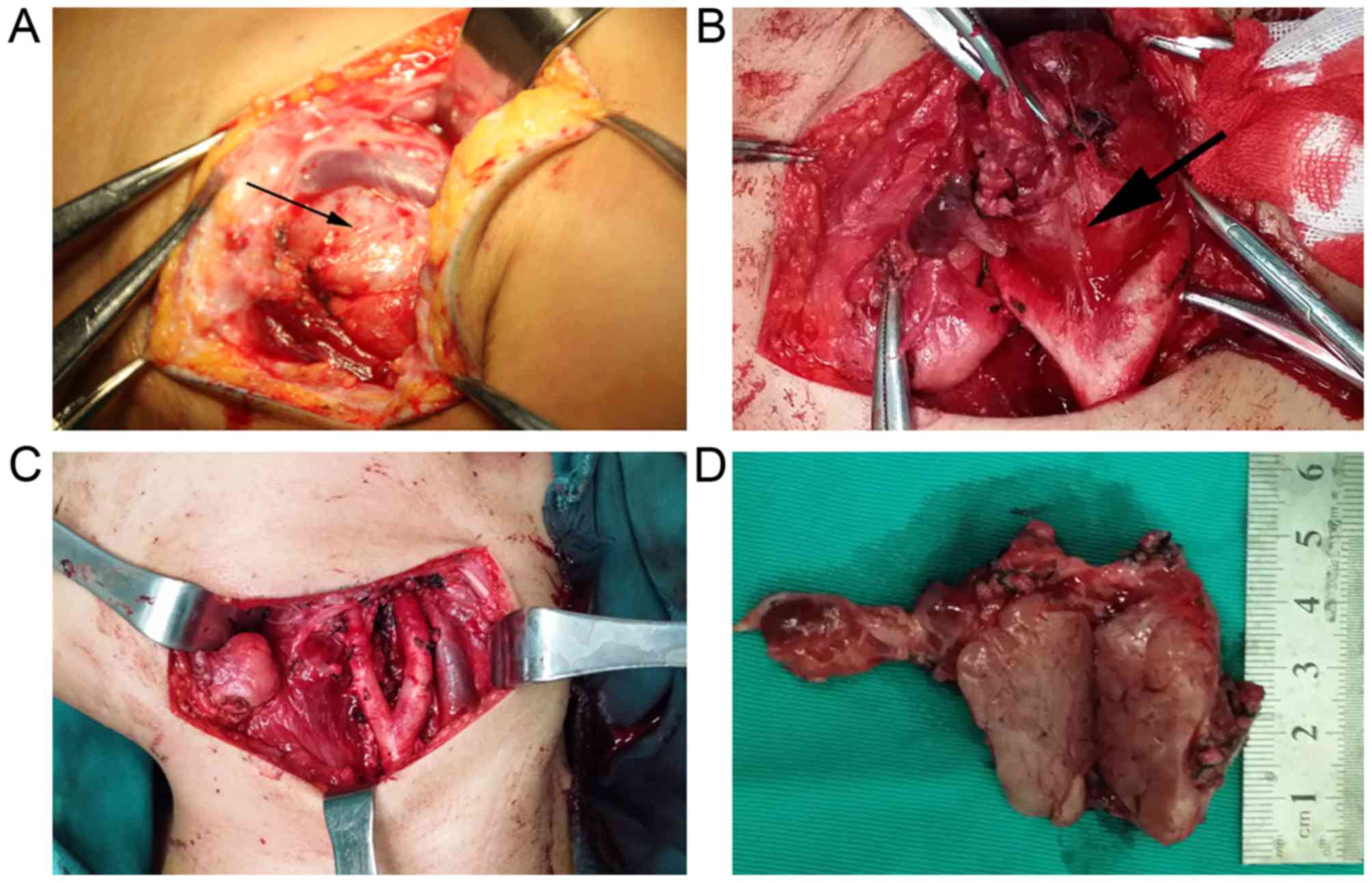
Patient case
A 22-year-old female presented with a 4-year history
of a left side neck tumor and occasional pain when cold. The skin
of the upper neck was free of the tumor. Type-B ultrasonic revealed
a 40×25 mm solid nodule in the upper neck area with a clear
boundary, irregular shape and an uneven internal echo, and the
Type-B ultrasonic imaging identified the abundant blood flow
signals. Enhanced computed tomography (CT) revealed two irregular
solid nodules on the left and right carotid artery bifurcation. The
patient described that the foreign body sensation had recently
become serious and therefore surgery was decided upon following the
patient's first visit to oral and maxillofacial surgery. The border
of the tumor was relatively evident and the tumor had an intact
envelope that bled easily, so no biopsy was performed. On the basis
of these clinical characteristics and radiographic results, the
tumor was identified as a benign CBT, although the possibility of
metastatic cancer was not excluded. The tumor occupied the overall
carotid artery bifurcation which oppressed the internal carotid
artery, therefore it was decided that the tumor was resectable by
transverse incision. There was no obvious connection between the
tumor and surrounding tissue, and the tumor was resected
completely. The common carotid artery, internal carotid artery and
external carotid artery remained intact (Fig. 1).
Imaging characteristics
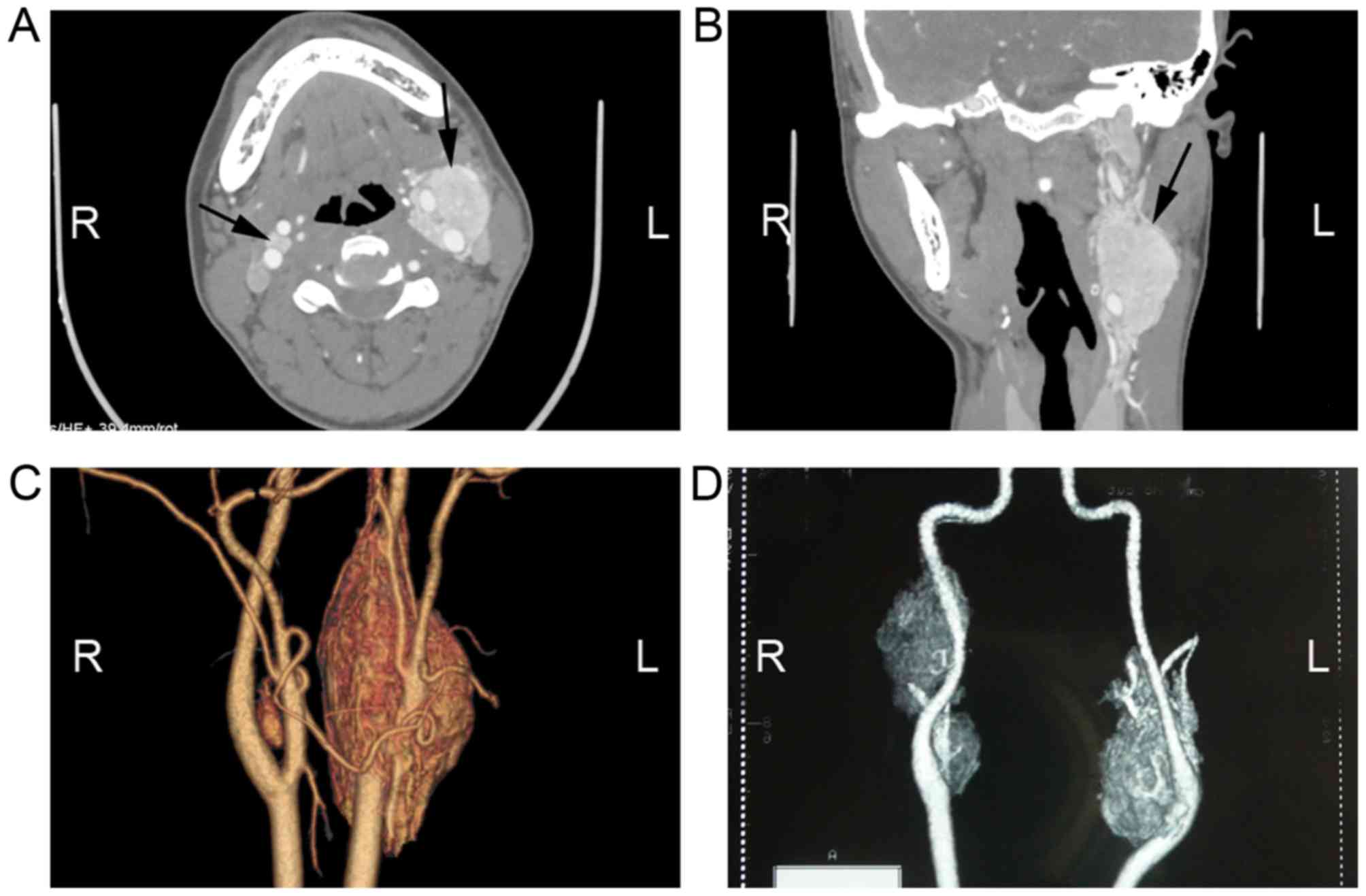
Enhanced CT revealed two irregular solid nodules,
consisting of 5.7×2.4×2 and 1×0.8×0.7 cm soft tissue density
located in the left and right carotid artery bifurcation,
respectively. Additionally, CT demonstrated heterogeneous
reinforcement. The left mass surrounded the internal carotid artery
and external carotid artery; however, the boundary between the CBT
and carotid artery was clear. The CBT was demonstrated to be rich
in blood vessels (Fig. 2). These were
identified to be possible bilateral CBTs.
Surgical specimens and pathological
features
The size of surgical specimens were 5.5×2×1.5 cm
which was identified as solid and pinkish-gray, following cutting
through the mass. The mass was soft and coated by an envelope. The
first pathology report indicated that the tumor may be a
paraganglioma, which required validation by immunohistochemical
tests. The immunohistochemical report indicated that the tumor
cells were strongly positive to CD56, Syn and protein S-100,
moderately positive to TFE3, negative to CK and EMA, and partial
cells were weakly positive to Desmir (<5%). This confirmed
diagnosis of paraganglioma of the carotid body (Fig. 3).
Discussion
The carotid body tumor is located at the common
carotid artery bifurcation and was reported by Kapoor et al
(7). The carotid body contains
chemoreceptors that are sensitive to hypoxia, hypercapnia and
acidosis, and functions to maintain homeostasis and blood pressure
in the human body. In the present case report, CBT primarily
occurred in individuals <60 years old, and whether a history of
smoking and consumption of alcohol are associated with CBT remains
unknown. CBT is a type of paraganglioma arising from the carotid
body and is located at the carotid bifurcation (8). Chronic hypoxia is considered to be one
of the reasons for CBTs; however, in the present case report, the
patient lived in low altitude area where there was no hypoxia and
the hypoxia cannot explain the pathogenesis of the case. In the
present case report, the majority of CBTs were benign and
slow-growing tumors; therefore, the CBTs may have been misdiagnosed
as lymph nodes. Owing to the rarity and lack of clinical features
of CBTs, diagnosis may be difficult and clinicians may be
mistakenly diagnosed as branchial cleft cyst (9), vascular malformation (10), lymph node and arterial aneurysm
(11), when the mass is small.
Ultrasonography and CT scans may be enable preoperative diagnosis
and treatment plan. Ultrasonography may identify whether the mass
is solid and exhibits a rich blood flow, whereas CT scans or
magnetic resonance imaging are improved methods for the diagnosis
of CBTs (12,13). In the present case report, the CT
angiograph (CTA) was required for preoperative diagnosis, which may
improve the identification of the dimensions and anatomical
association with important blood vessels, including the internal
carotid, external carotid artery and common carotid artery.
Furthermore, the CTA may indicate the ‘feeding artery’ which may
supply important information for surgery. Fine needle aspiration
has been used to improve the diagnosis accuracy of CBT (1), but this technique poses risks.
For patients with bilateral CBTs, surgery may not be
performed all at once in order to avoid serious complications,
including vascular or cranial nerve lesions. There are a number of
patients who are not suitable for surgery, for instance clinically
unstable patients, including elderly patients or those with a
certainty of stroke. Conservative treatment, including chemotherapy
and radiotherapy is ineffective for CBT (14–17).
Embolization is one effective palliative treatment, but the
vascular complications and cranial nerve deficits may occur in ~33%
of the patients (3,18).
Surgical treatment is considered to be the optimal
treatment choice for CBTs. Of those patients who underwent surgery
at The First Affiliated Hospital of Zhengzhou University, only 1
case exhibited recurrence 2 months after surgery. The tumors may be
dissected in the sub-adventitial avascular plane of the artery
(19). Shamblin CBT groups II and III
may require removal with arteriectomy or internal carotid artery
ligation (8). Occasionally,
anastomosis may be required between the internal and common carotid
arteries or vascular reconstruction with grafts may be required
(18,20). Occurrences of technical complications
in anastomoses between the common and internal carotid arteries
following resection of the carotid body have been reported in a
previous study (21). These cases
evolved with a number of hematomas and, in a limited number of
cases, with cerebral ischemia-reperfusion (21). Of those patients who underwent surgery
at The First Affiliated Hospital of Zhengzhou University, only 1
case required vascular repair, and in order to improve and assess
the tolerance of unilateral carotid blood supply, the Matas test
and the balloon test occlusion of internal carotid artery are
required prior to surgery (22). If
the vascular compensatory function exhibited is satisfactory in the
total cerebral angiogram and BOT, surgery may be performed. During
surgery, the tumor is stripped away from the surface of the blood
vessel and damage to the artery walls is avoided. If the walls of
the internal carotid and common carotid artery are damaged during
surgery, ligation of the internal carotid or common carotid artery
may be performed, to avoid postoperative complications.
Improved diagnostic methods are useful for the
treatment of CBT. The CTA and Digital Subtraction Angiography may
identify the border and the supply artery. Ligation of the supply
artery may markedly decrease during the surgery. The Matas test and
the BOT of internal carotid artery are required to evaluate the
surgery indication. Refined surgical technologies or skills may
provide security of safety resection and decrease the occurrence of
complications.
Acknowledgements
The present case report was supported by the
National Natural Science Foundation of China (grant no. 81402231),
the Basic and Frontier Technology Research Projects by Science and
Technology Department of Henan (grant no. 142300410315) and the
Youth Foundation of The First Affiliated Hospital of Zhengzhou
University, and the Oral and Maxillofacial Surgery Academician
Workstation of Zhengzhou (grant no. 152PYSGZ040).
References
|
1
|
Casarim AL, Tincani AJ, Del Negro A,
Aguiar CG, Fanni RV and Martins AS: Carotid body tumor:
Retrospective analysis on 22 patients. Sao Paulo Med J.
132:133–139. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nora JD, Hallett JW Jr, O'Brien PC,
Naessens JM, Cherry KJ Jr and Pairolero PC: Surgical resection of
carotid body tumors: Long-term survival, recurrence, and
metastasis. Mayo Clin Proc. 63:348–352. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wieneke JA and Smith A: Paraganglioma:
Carotid body tumor. Head Neck Pathol. 3:303–306. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sanghvi VD and Chandawarkar RY: Carotid
body tumors. J Surg Oncol. 54:190–192. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Brown JS: Glomus jugulare tumors
revisited: A ten-year statistical follow-up of 231 cases.
Laryngoscope. 95:284–288. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Offergeld C, Brase C, Yaremchuk S, Mader
I, Rischke HC, Gläsker S, Schmid KW, Wiech T, Preuss SF, Suárez C,
et al: Head and neck paragangliomas: Clinical and molecular genetic
classification. Clinics (Sao Paulo). 67 Suppl 1:S19–S28. 2012.
View Article : Google Scholar
|
|
7
|
Kapoor R, Saha MM, Das DK, Gupta AK and
Tyagi S: Carotid body tumor initially diagnosed by fine needle
aspiration cytology. Acta Cytol. 33:682–683. 1989.PubMed/NCBI
|
|
8
|
Lim JY, Kim J, Kim SH, Lee S, Lim YC, Kim
JW and Choi EC: Surgical treatment of carotid body paragangliomas:
Outcomes and complications according to the shamblin
classification. Clin Exp Otorhinolaryngol. 3:91–95. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Williams MD, Phillips MJ, Nelson WR and
Rainer WG: Carotid body tumor. Arch Surg. 127:963–968. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhao FY, Gao Y, Wu MJ, Luo QF, Liu Y and
Xu ZQ: Diagnosis and therapy on hemangiomas and vascular
malformation in view of the new classification. Beijing Da Xue Xue
Bao. 41:21–27. 2009.(In Chinese). PubMed/NCBI
|
|
11
|
Muhm M, Polterauer P, Gstöttner W, Temmel
A, Losert H, Richling B, Undt G, Niederle B, Staudacher M,
Kretschmer G and Ehringer H: Glomus caroticum chemodectoma. Review
on current diagnosis and therapy. Wien Klin Wochenschr.
112:115–120. 2000.(In German). PubMed/NCBI
|
|
12
|
Demattè S, Di Sarra D, Schiavi F, Casadei
A and Opocher G: Role of ultrasound and color Doppler imaging in
the detection of carotid paragangliomas. J Ultrasound. 15:158–163.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Arya S, Rao V, Juvekar S and Dcruz AK:
Carotid body tumors: Objective criteria to predict the Shamblin
group on MR imaging. AJNR Am J Neuroradiol. 29:1349–1354. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ruby R, Gullane PJ and Mintz D:
Chemodectomas of the head and neck. J Otolaryngol. 10:126–136.
1981.PubMed/NCBI
|
|
15
|
Liapis C, Gougoulakis A, Karydakis V,
Verikokos C, Doussaitou B, Skandalakis P, Gogas J and Sechas M:
Changing trends in management of carotid body tumors. Am Surg.
61:989–993. 1995.PubMed/NCBI
|
|
16
|
Pellitteri PK, Rinaldo A, Myssiorek D,
Jackson Gary C, Bradley PJ, Devaney KO, Shaha AR, Netterville JL,
Manni JJ and Ferlito A: Paragangliomas of the head and neck. Oral
Oncol. 40:563–575. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kasper GC, Welling RE, Wladis AR, CaJacob
DE, Grisham AD, Tomsick TA, Gluckman JL and Muck PE: A
multidisciplinary approach to carotid paragangliomas. Vasc
Endovascular Surg. 40:467–474. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lack EE, Cubilla AL and Woodruff JM:
Paragangliomas of the head and neck region. A pathologic study of
tumors from 71 patients. Hum Pathol. 10:191–218. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Anand VK, Alemar GO and Sanders TS:
Management of the internal carotid artery during carotid body tumor
surgery. Laryngoscope. 105:231–235. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gardner P, Dalsing M, Weisberger E,
Sawchuk A and Miyamoto R: Carotid body tumors, inheritance, and a
high incidence of associated cervical paragangliomas. Am J Surg.
172:196–199. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mitchell RO, Richardson JD and Lambert GE:
Characteristics, surgical management, and outcome in 17 carotid
body tumors. Am Surg. 62:1034–1037. 1996.PubMed/NCBI
|
|
22
|
Qin RF, Shi LF, Liu YP, Lei DL, Hu KJ,
Feng XH, Nie X and Mao TQ: Diagnosis and surgical treatment of
carotid body tumors: 25 years' experience in China. Int J Oral
Maxillofac Surg. 38:713–718. 2009. View Article : Google Scholar : PubMed/NCBI
|