Introduction
Pancreatic cancer is a highly aggressive cancer,
with a 5-year overall survival (OS) rate of <1.0%, and is one of
the most frequent causes of cancer-associated mortality worldwide
(1). The poor outcome for patients
with pancreatic cancer is associated with its late diagnosis due to
the paucity of symptoms, rapid tumor progression and
unresponsiveness to chemotherapy or radiotherapy. These parameters
result in low resectability rates following diagnosis, early
recurrence subsequent to resection and an overall poor survival
rate (2). Therefore, pancreatic
cancer is the object of extensive study, to obtain an improved
understanding of the development and progression of the disease,
and to improve the survival and quality of life of patients.
In total, >90% of pancreatic cancer cases arise
from the ductal epithelium of the pancreas and are termed
pancreatic ductal adenocarcinoma (PDAC). Extensive efforts have
been made to identify potential biomarkers that may be used to
develop anti-metastatic treatments and improve prognostic
evaluation (3). Unlike PDACs, solid
pseudopapillary neoplasms (SPNs) of the pancreas are distinctive
tumors that exhibit a low malignancy potential and are associated
with a favorable prognosis following resection (4).
Autophagy, which is known as type II programmed cell
death, is an important pathway for the degradation and recycling of
cellular components and the response to stress (5). At basal levels, autophagy controls
cellular homeostasis by removing potential intrinsic toxic
components and enables cells to perform structural remodeling,
which serves an essential role in cellular differentiation,
development and survival in response to starvation conditions
(6,7).
The aberrant regulation of these mechanisms contributes to the
pathogenesis of a variety of diseases, including cancer (6,8).
The Beclin 1 gene was the first mammalian autophagy
gene identified, and it is located on chromosome 17q21 (6). Beclin 1 has received special attention
in studies investigating autophagy, as it is the first autophagy
protein demonstrated to be a haploinsufficient tumor suppressor in
cancer cell experiments (9,10). However, studies associating Beclin 1
with the pathogenesis of human cancer are limited, and the
correlation is controversial. Decreased expression of Beclin 1 has
been detected in glioblastoma (11),
hepatocellular carcinoma (12),
esophageal cancer (13), non-small
cell lung cancer (14), bladder
urothelial tumors (15) and breast
cancer (16), whilst increased
expression of Beclin 1 has been identified in ovarian cancer
(17), colorectal cancer (18) and gastric cancer (19).
The BCL2, apoptosis regulator (BCL2) gene,
located on chromosome 18q21, is a member of the Bcl-2 family, which
serves an important role in apoptosis suppression (20,21). The
anti-apoptotic function extends cell survival in normal and tumor
cells by inhibiting different cell death mechanisms (22). Bcl-2 is involved in cellular
morphogenesis and differentiation; it functions as an oncogenic and
anti-death molecule by modulating various homeostatic,
developmental and disease processes (23–25).
Although overexpression of Bcl-2 confers a survival advantage to
the cell that may lead to rapid and uncontrolled cellular
proliferation, which characterizes the development of cancer,
differences in the expression of Bcl-2 in numerous types of human
cancer have been identified, similar to that found for Beclin 1.
Bcl-2 downregulation has been revealed in breast cancer and
pancreatic cancer (26,27), whereas increased expression of Bcl-2
upregulation has also been demonstrated (16,28). The
significance of Bcl-2 expression for cancer prognosis remains
unclear.
Beclin 1 was originally identified in a yeast two
hybrid screen as a Bcl-2 family-interacting protein that serves a
pivotal role in the process of autophagy (29). The binding between Beclin 1 and Bcl-2
is regulated by a variety of proteins and compounds that enhance or
inhibit the Bcl-2/Beclin 1 interaction to repress or activate
autophagy, and serve important roles in the crosstalk between
autophagy and apoptosis (30,31). The cooperation between Beclin 1 and
Bcl-2 may additionally affect tumorigenesis and progression.
Studies suggest that Beclin1 and Bcl-2 expression in
tumor cells varies according to tumor and tissue type, which
requires additional investigation (11–19,26–28).
There is a study that assesses Beclin 1 and Bcl-2 expression levels
in pancreatic tumors, their interactions, and the correlation
between their expression and patient survival (32). The aim of the present study was to
examine the expression of Beclin 1 and Bcl-2 by
immunohistochemistry in pancreatic neoplasms, including PDACs, SPNs
and chronic pancreatitis (CP) tissues as the controls for PDAC. The
expression of Beclin 1 and Bcl-2 was evaluated in correlation with
clinicopathological parameters and the survival of patients to
assess their value as markers of tumor development and
prognosis.
Patients and methods
Patients and tissue samples
Formalin-fixed and paraffin-embedded tissue samples
from 117 patients with PDAC, 43 patients with SPN and 32 patients
with CP were selected from the archived materials of the Department
of Pathology of Shengjing Hospital of China Medical University
(Shenyang, China). The PDAC group consisted of 70 men and 47 women,
the age of which ranged between 37 and 77 years (mean age ±
standard deviation, 58.89±9.27). The SPN group consisted of 5 men
and 38 women, the age of which ranged between 9 and 65 years (mean
age ± standard deviation, 32.77±13.72). Patients diagnosed with
PDAC, SPN or CP underwent pancreaticoduodenectomy or distal
pancreatectomy between January 2011 and May 2014. Sufficient
clinical and survival information of the PDAC and SPN patients was
available.
Patients without complete survival information or
those who succumbed to surgical complications were excluded from
the study. No patients had received any neoadjuvant chemotherapy or
chemoradiotherapy prior to the surgical resection. All patients
were followed up by interview in the clinic or by phone call. Data
on chemotherapy following surgery, disease-free survival (DFS) time
and OS time were collected for each patient. Cases with distant
metastasis or R1 resection were excluded from DFS evaluation. The
total period of follow-up was 18–57 months.
All samples were initially stained with Mayer's
hematoxylin for 5 min and 2% eosin for 1 min at room temperature;
two independent investigators evaluated each section to confirm the
foci and the differentiation of PDAC microscopically, and the most
representative section from each case was used for
immunohistochemical staining.
The present study was approved by the Clinical
Ethics Committee of Shengjing Hospital of China Medical
University.
Immunohistochemistry
Immunohistochemical staining was performed using the
biotin-free polymer detection system. The formalin-fixed,
paraffin-embedded sections (4-µm thick) were deparaffinized and
dehydrated via dimethylbenzene and a graded alcohol series,
respectively.
Microwave antigen retrieval was achieved in sodium
citrate buffer (pH 6.0) for Beclin 1, and in Tris-EDTA buffer (pH
9.0) for Bcl-2, each for 20 min at 100°C. Endogenous peroxidase
activity was blocked by incubation with 0.3% hydrogen peroxidase at
37°C for 15 min. Sections were then incubated with primary mouse
monoclonal antibodies against Beclin 1 (1:400; cat. no. ab114071;
Abcam, Cambridge, UK) and rabbit monoclonal antibodies against
Bcl-2 (1:350; cat. no. ab32124; Abcam) at 4°C overnight. A two-step
immunohistochemical staining kit was used for expression analysis
(cat. no. PV-9000; Zhongshan Jinqiao Biotechnology Co. Ltd.,
Beijing, China). Tissue sections were then incubated with a polymer
auxiliary for 15 min at 37°C and a biotin-free polymeric
horseradish peroxidase-linked antibody-conjugate agent from the kit
for 25 min at 37°C. Following incubation, the reaction product was
detected using diaminobenzidine (ZLI-9018; Zhongshan Jinqiao
Biotechnology Co. Ltd., Beijing, China). Finally, the sections were
counterstained with Mayer's hematoxylin as aforementioned,
dehydrated, and mounted.
The normal ductal epithelium in breast tissue
obtained from Pathology Department of Shengjing Hospital of China
Medical University and the lymphocytes in the pancreatic stroma of
the included pancreatic samples were used as positive controls for
Beclin 1 and Bcl-2, respectively. The negative controls were
obtained by replacing the primary antibodies with 0.01 mol/l
phosphate-buffered saline.
Images were captured with a light microscope and
NIS-Elements F3.0 software (Nikon Corporation, Tokyo, Japan).
Evaluation of immunohistochemical
staining
Immunohistochemical sections were independently
evaluated by two investigators in a blinded manner. At least five
fields at a magnification, ×400 were randomly chosen per section.
Cytoplasmic or membranous staining for Beclin 1 and Bcl-2 was
considered to represent a positive immunoreaction. Beclin 1 and
Bcl-2 expression levels were estimated semiquantitatively based on
the combination of staining intensity and the percentage of
positively stained cells (proportion score). The staining intensity
was scored as follows: 0, negative; 1, weak; 2, moderate; and 3,
strong. According to the percentage of positively stained cells in
whole foci, the staining extent was categorized into 5 grades as
follows: 0, negative; 1, 0–25%; 2, 26–50%; 3, 51–75%; and 4,
76–100%. The intensity score and proportion score were multiplied
together for a final score. Final scores were as follows for Beclin
1 and Bcl-2: <6, low expression; and ≥6, high expression.
Clinical outcome assessment
DFS was calculated from the date of surgery to the
date of detection of local recurrence/distant metastasis or to the
date of mortality due to PDAC. DFS was only calculated in patients
with R0 resection (free resection margins). Patients with R1
resection (resection margins invaded) were considered to have
failure at time zero. OS was defined as the time from the date of
surgery to the date of mortality or to the date of last follow-up
if patients remained alive. The DFS of patients with PDAC was
acquired in 97 cases with R0 resection; the mean DFS was 10.9
months (median, 6.0 months; range, 0.8–32.7 months). The OS of
patients with PDAC was acquired in 117 cases; the mean OS was 13.6
months (median, 10.4 months; range, 1.37–42.0 months). None of the
patients with SPN exhibited local recurrence/distant metastasis or
had succumbed by the date of last follow-up.
Statistical analysis
Statistical analysis was performed using SPSS v.18.0
software (SPSS, Inc., Chicago, IL, USA). Pearson's χ2
test and Fisher's exact test were used to evaluate the association
between Beclin 1 and Bcl-2 expression and several
clinicopathological variables, and the difference between the
Beclin 1 and Bcl-2 expression in PDAC and CP cases. The correlation
coefficients (r and P-values) between Beclin 1 and Bcl-2 among
PDAC, SPN and CP tissues were obtained using the Spearman's test.
Survival curves of DFS and OS were analyzed by the Kaplan-Meier
method and compared with the log-rank test. Multivariate analysis
of prognostic factors was tested with the Cox proportional hazards
model. P<0.05 was considered to indicate a statistically
significant difference.
Results
Beclin 1 expression in pancreatic
neoplasms
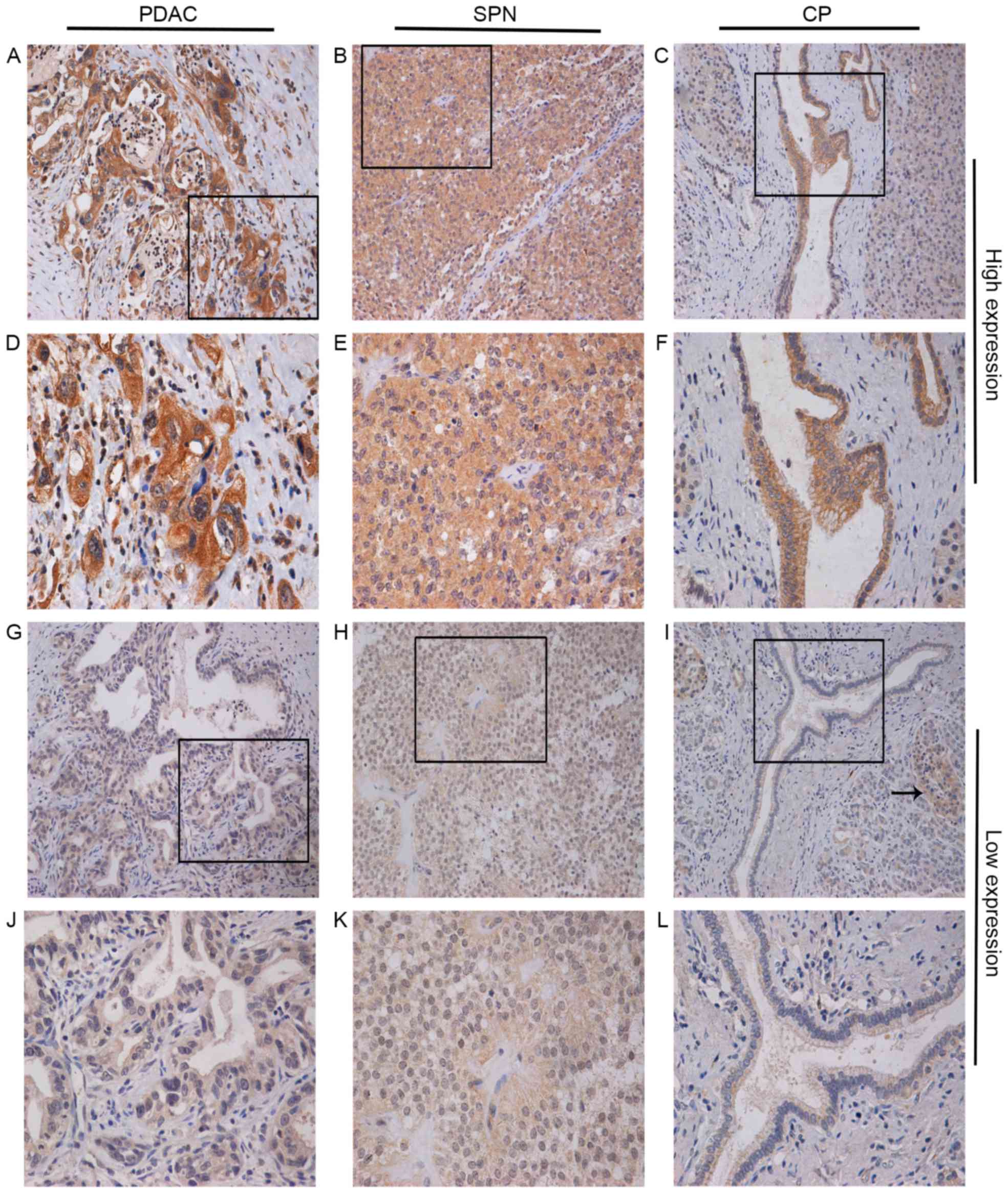
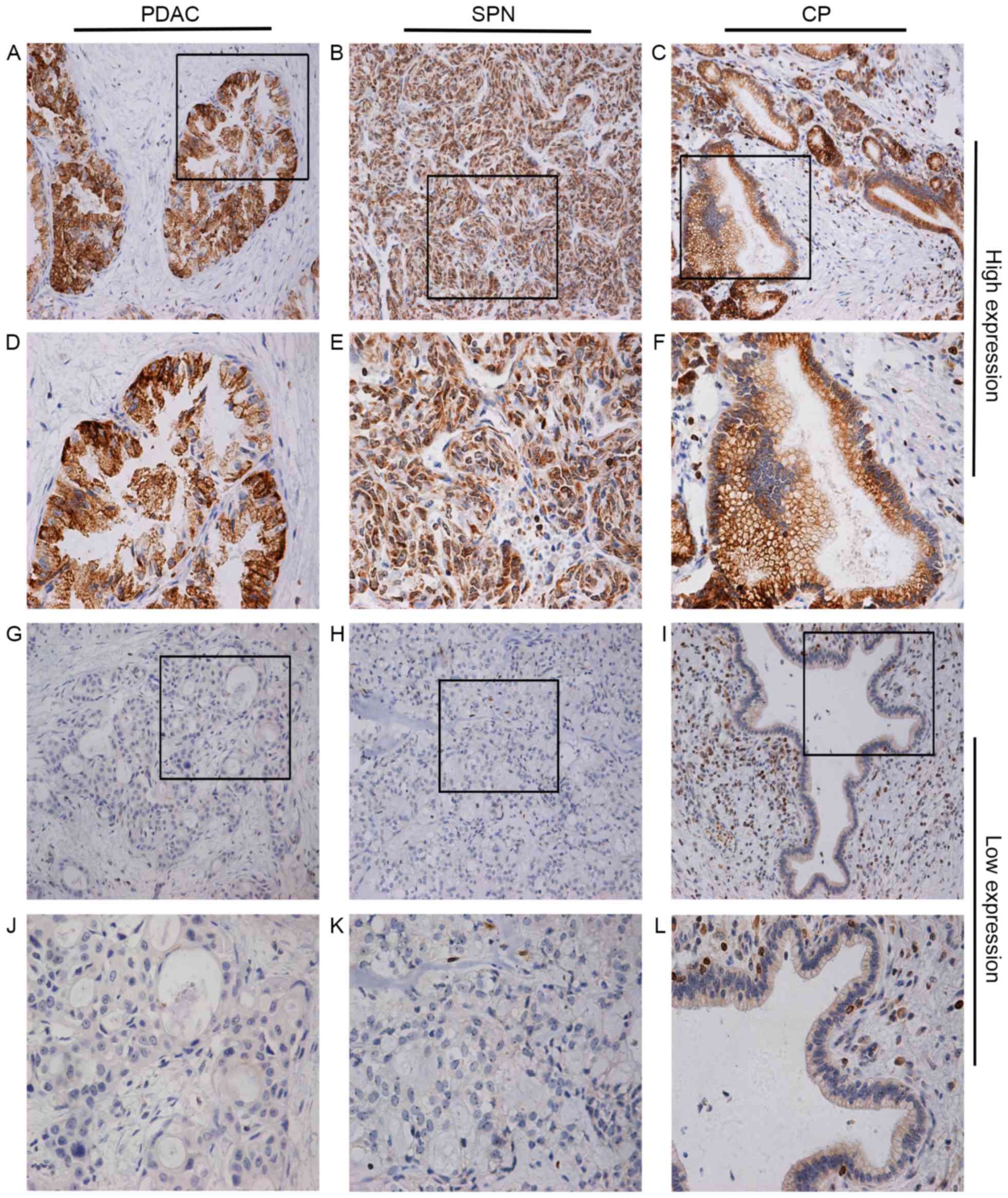
Assessment of Beclin 1 expression in pancreatic
tissues demonstrated positive staining in cancerous foci, SPN foci
and normal epithelium in CP tissues, and in the cytoplasm of
intralobular ductal epithelial cells, acinar cells and pancreatic
islet cells (Fig. 1). Pancreatic
islet cells stained positive for Beclin 1, and were used as the
positive control for Beclin 1 immunostaining in subsequent
experiments. High Beclin 1 expression was observed in 74 (63.2%)
PDAC cases, while 43 (36.8%) PDAC cases demonstrated low
expression. PDAC tissues exhibited significantly higher Beclin 1
expression compared with the normal ductal epithelium in CP tissues
(P=0.047) (Table I).
 | Figure 1.Immunohistochemical staining for high
Beclin 1 expression in PDAC tissues at (A) magnification, ×200 and
(D) ×400, in SPN tissues at (B) magnification, ×200 and (E) ×400,
and in normal ductal epithelium in CP tissues at (C) magnification,
×200 and (F) ×400. Low Beclin 1 expression in PDAC tissues at (G)
magnification, ×200 and (J) ×400, in SPN tissues at (H)
magnification, ×200 and (K) ×400, and in normal ductal epithelium
in CP tissues at (I) magnification, ×200 and (L) ×400. Pancreatic
islet cells were positively stained with Beclin 1 in each sample
(arrow). PDAC, pancreatic ductal adenocarcinoma; SPN,
solid-pseudopapillary neoplasm; CP, chronic pancreatitis. |
 | Table I.Expression of Beclin 1 and Bcl-2 in
PDAC and CP tissues. |
Table I.
Expression of Beclin 1 and Bcl-2 in
PDAC and CP tissues.
|
|
| Beclin 1 |
| Bcl-2 |
|
|---|
|
|
|
|
|
|
|
|---|
| Tissue type | Cases, n | Low, n (%) | High, n (%) | P-value | Low, n (%) | High, n (%) | P-value |
|---|
| PDAC | 117 | 43 (36.8) | 74 (63.2) | 0.047a | 79 (67.5) | 38 (32.5) |
<0.001a |
| CP | 32 | 18 (56.3) | 14 (43.8) |
| 8
(25.0) | 24 (75.0) |
|
The association between Beclin 1 expression and the
clinicopathological characteristics of patients with PDAC is
described in Table II. High Beclin 1
expression was correlated with poor histological differentiation
(P=0.001) and distant metastasis (P=0.021).
 | Table II.Association of Beclin 1 and Bcl-2
expression with clinicopathological characteristics in pancreatic
ductal adenocarcinoma. |
Table II.
Association of Beclin 1 and Bcl-2
expression with clinicopathological characteristics in pancreatic
ductal adenocarcinoma.
|
|
| Beclin 1 |
| Bcl-2 |
|
|---|
|
|
|
|
|
|
|
|---|
|
Characteristics | Cases, n | Low, n (%) | High, n (%) | P-value | Low, n (%) | High, n (%) | P-value |
|---|
| Age, years
(mean=58.98) |
|
|
| 0.518 |
|
| 0.646 |
|
<58.98 | 59 | 20 (33.9) | 39 (66.1) |
| 41 (69.5) | 18 (30.5) |
|
|
≥58.98 | 58 | 23 (39.7) | 35 (60.3) |
| 38 (65.5) | 20 (34.5) |
|
| Sex |
|
|
| 0.064 |
|
| 0.485 |
|
Female | 47 | 22 (46.8) | 25 (53.2) |
| 30 (63.8) | 17 (36.2) |
|
|
Male | 70 | 21 (30.0) | 49 (70.0) |
| 49 (70.0) | 21 (30.0) |
|
| Smoker |
|
|
| 0.170 |
|
| 0.332 |
| No | 75 | 31 (41.3) | 44 (58.7) |
| 53 (70.7) | 22 (29.3) |
|
|
Yes | 42 | 12 (28.6) | 30 (71.4) |
| 26 (61.9) | 16 (38.1) |
|
| Diabetes |
|
|
| 0.631 |
|
| 0.629 |
| No | 104 | 39 (37.5) | 65 (62.5) |
| 71 (68.3) | 33 (31.7) |
|
|
Yes | 13 | 4 (30.8) | 9 (69.2) |
| 8 (61.5) | 5 (38.5) |
|
| CA19-9,
U/mlb |
|
|
| 0.585 |
|
| 0.871 |
|
≤37 | 27 | 9 (33.3) | 18 (66.7) |
| 18 (66.7) | 9 (33.3) |
|
|
>37 | 79 | 31 (39.2) | 48 (60.8) |
| 54 (68.4) | 25 (31.6) |
|
| CEA,
ng/mlb |
|
|
| 0.915 |
|
| 0.996 |
| ≤5 | 78 | 29 (37.2) | 49 (62.8) |
| 53 (67.9) | 25 (32.1) |
|
|
>5 | 25 | 9 (36.0) | 16 (64.0) |
|
|
|
|
| Location |
|
|
| 0.235 |
|
| 0.017a |
|
Head | 85 | 34 (40.0) | 51 (60.0) |
| 52 (61.2) | 33 (38.8) |
|
|
Body/Tail | 32 | 9 (28.1) | 23 (71.9) |
| 27 (84.4) | 5 (15.6) |
|
|
Differentiation |
|
|
| 0.001a |
|
| 0.002a |
|
Well | 21 | 12 (57.1) | 9 (42.9) |
| 11 (52.4) | 10 (47.6) |
|
|
Moderate | 71 | 29 (40.8) | 42 (59.2) |
| 44 (62.0) | 27 (38.0) |
|
|
Poor | 25 | 2 (8.0) | 23 (92.0) |
| 24 (96.0) | 1 (4.0) |
|
| T stage |
|
|
| 0.786 |
|
| 0.577 |
|
T1/T2 | 39 | 15 (38.5) | 24 (61.5) |
| 25 (64.1) | 14 (35.9) |
|
|
T3/T4 | 78 | 28 (35.9) | 50 (64.1) |
| 54 (69.2) | 24 (30.8) |
|
| N stage |
|
|
| 0.390 |
|
| 0.351 |
| N0 | 73 | 29 (39.7) | 44 (60.3) |
| 47 (64.4) | 26 (35.6) |
|
| N1 | 44 | 14 (31.8) | 30 (68.2) |
| 32 (72.7) | 12 (27.3) |
|
| M stage |
|
|
| 0.021a |
|
| 0.049a |
| M0 | 100 | 41 (41.0) | 59 (59.0) |
| 64 (64.0) | 36 (36.0) |
|
| M1 | 17 | 2 (11.8) | 15 (88.2) |
| 15 (88.2) | 2 (11.8) |
|
| TNM stage |
|
|
| 0.235 |
|
| 0.017a |
|
I/II | 85 | 34 (40.0) | 51 (60.0) |
| 52 (61.2) | 33 (38.8) |
|
|
III/IV | 32 | 9 (28.1) | 23 (71.9) |
| 27 (84.4) | 5 (15.6) |
|
High Beclin 1 expression was detected in 26 (60.5%)
patients with SPN and was correlated with pancreatic body or tail
location (P=0.018) and the presence of nuclear pleomorphism
(P=0.031). There was no significant correlation between Beclin 1
expression and other clinicopathological features (Table III).
 | Table III.Association of Beclin 1 and Bcl-2
expression with clinicopathological characteristics in
solid-pseudopapillary neoplasms. |
Table III.
Association of Beclin 1 and Bcl-2
expression with clinicopathological characteristics in
solid-pseudopapillary neoplasms.
|
|
| Beclin 1 |
| Bcl-2 |
|
|---|
|
|
|
|
|
|
|
|---|
|
Characteristics | Cases, n | Low, n (%) | High, n (%) | P-value | Low, n (%) | High, n (%) | P-value |
|---|
| Age, years
(mean=32.77) |
|
|
| 0.207 |
|
| 0.399 |
|
<32.77 | 28 | 13 (46.4) | 15 (53.6) |
| 22 (78.6) | 6 (21.4) |
|
|
≥32.77 | 15 | 4 (26.7) | 11 (73.3) |
| 10 (66.7) | 5 (33.3) |
|
| Sex |
|
|
| 0.633 |
|
| 0.096 |
|
Male | 5 | 1 (20.0) | 4 (80.0) |
| 2 (40.0) | 3 (60.0) |
|
|
Female | 38 | 16 (42.1) | 22 (57.9) |
| 30 (78.9) | 8 (21.1) |
|
| Location |
|
|
| 0.018a |
|
| 0.116 |
|
Head | 16 | 10 (62.5) | 6 (37.5) |
| 14 (87.5) | 2 (12.5) |
|
|
Body/Tail | 27 | 7 (25.9) | 20 (74.1) |
| 18 (66.7) | 9 (33.3) |
|
| Size, cm |
|
|
| 0.859 |
|
| 0.802 |
|
<6.75 | 26 | 10 (38.5) | 16 (61.5) |
| 19 (73.1) | 7 (26.9) |
|
|
≥6.75 | 17 | 7 (41.2) | 10 (58.8) |
| 13 (76.5) | 4 (23.5) |
|
| Tumor feature |
|
|
| 0.834 |
|
| 0.422 |
|
Solid | 16 | 6 (37.5) | 10 (62.5) |
| 13 (81.3) | 3 (18.8) |
|
| Cystic
and solid | 27 | 11 (40.7) | 16 (59.3) |
| 19 (70.4) | 8 (29.6) |
|
| Nuclear
pleomorphism, HPFs |
|
|
| 0.031a |
|
| 0.273 |
|
<10 | 36 | 17 (47.2) | 19 (52.8) |
| 28 (77.8) | 8 (22.2) |
|
|
≥10 | 7 | 0 (0.0) | 7 (100.0) |
| 4 (57.1) | 3 (42.9) |
|
| Peripancreatic
invasion |
|
|
| 0.446 |
|
| 0.967 |
|
Yes | 8 | 2 (25.0) | 6 (75.0) |
| 6 (75.0) | 2 (25.0) |
|
| No | 35 | 15 (42.9) | 20 (57.1) |
| 26 (74.3) | 9 (25.7) |
|
| Cytokeratin |
|
|
| 0.749 |
|
| 1.000 |
| + | 21 | 8 (38.1) | 13 (61.9) |
| 15 (71.4) | 6 (28.6) |
|
| − | 16 | 7 | 9 |
| 11 (68.8) | 5 (31.3) |
|
| Synaptophysin |
|
|
| 1.000 |
|
| 1.000 |
| + | 18 | 7 (38.9) | 11 (61.1) |
| 12 (66.7) | 6 (33.3) |
|
| − | 13 | 5 (38.5) | 8 (61.5) |
| 8 (61.5) | 5 (38.5) |
|
Bcl-2 expression in pancreatic
neoplasms
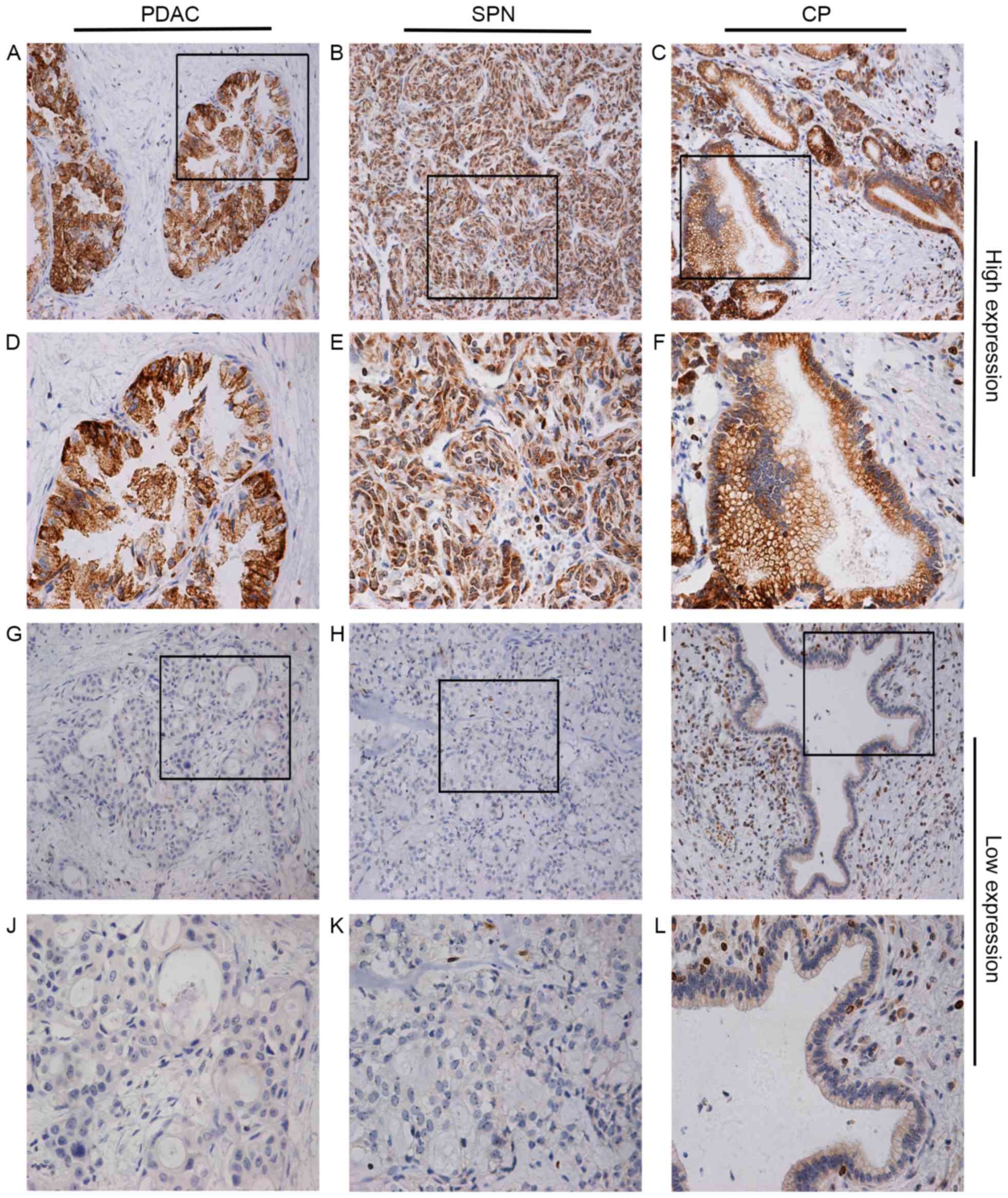
Cytoplasmic or membranous Bcl-2 immunostaining was
observed in the majority of the normal ductal (intralobular and
interlobular) cells and certain acinar compartments, whilst no
staining was observed in the endocrine component (Fig. 2).
 | Figure 2.Immunohistochemical staining for high
Bcl-2 expression in PDAC tissues at (A) magnification, ×200 and (D)
×400 in SPN tissues at (B) magnification, ×200 and (E) ×400 and in
normal ductal epithelium in CP tissues at (C) magnification, ×200
and (F) ×400. Low Bcl-2 expression in PDAC tissues at (G)
magnification, ×200 and (J) ×400 in SPN tissues at (H)
magnification, ×200 and (K) ×400 and in normal ductal epithelium in
CP tissues at (I) magnification, ×200 and (L) ×400. Lymphocytes in
the pancreatic stroma were used as the positive controls (arrow).
PDAC, pancreatic ductal adenocarcinoma; SPN, solid-pseudopapillary
neoplasm; CP, chronic pancreatitis; Bcl-2, B-cell lymphoma-2. |
Decreased Bcl-2 expression was detected in PDAC foci
compared with the normal ductal epithelium (Table I). High Bcl-2 expression was detected
in 38 (32.5%) PDAC cases, while 79 (67.5%) PDAC cases demonstrated
low expression. The correlation between Bcl-2 and the
clinicopathological characteristics of PDAC patients is summarized
in Table II. Decreased Bcl-2
expression was correlated with cancerous pancreatic body or tail
location (P=0.017), poor histological differentiation (P=0.002),
distant metastasis (P=0.049) and advanced Tumor-Node-Metastasis
(TNM) (33) stage (P=0.017).
High Bcl-2 expression was detected in 11 (25.6%)
patients with SPN. There was no significant correlation between
Bcl-2 expression and clinicopathological features in SPN (Table III).
Association between Beclin 1 and Bcl-2
expression
As demonstrated in Table
IV, Beclin 1 expression level was not associated with Bcl-2
expression in CP cases (P=0.629, r=0.073). However, there was a
statistically significant inverse correlation (P<0.001,
r=−0.342) between the level of Beclin 1 and Bcl-2 expression in
PDAC cases. A statistically significant direct correlation
(P=0.016, r=0.365) was detected between Beclin 1 and Bcl-2
expression in SPN cases.
 | Table IV.Association between Beclin 1 and
Bcl-2 expression. |
Table IV.
Association between Beclin 1 and
Bcl-2 expression.
|
| Bcl-2
expression |
|
|
|---|
|
|
|
|
|
|---|
| Beclin 1
expression | Low expression, n
(%) | High expression, n
(%) | r | P-value |
|---|
| PDAC |
|
| −0.342 |
<0.001a |
| Low
expression | 20 (17.1) | 23 (19.7) |
|
|
| High
expression | 59 (50.4) | 15 (12.8) |
|
|
| SPN |
|
| 0.365 | 0.016a |
| Low
expression | 16 (37.2) | 1 (2.3) |
|
|
| High
expression | 16 (37.2) | 10 (23.3) |
|
|
| CP |
|
| 0.073 | 0.692 |
| Low
expression | 5 (15.6) | 13 (40.6) |
|
|
| High
expression | 3 (9.4) | 11 (34.4) |
|
|
Association of clinicopathological
characteristics, Beclin 1/Bcl-2 expression and patient survival in
PDAC: A univariate survival analysis
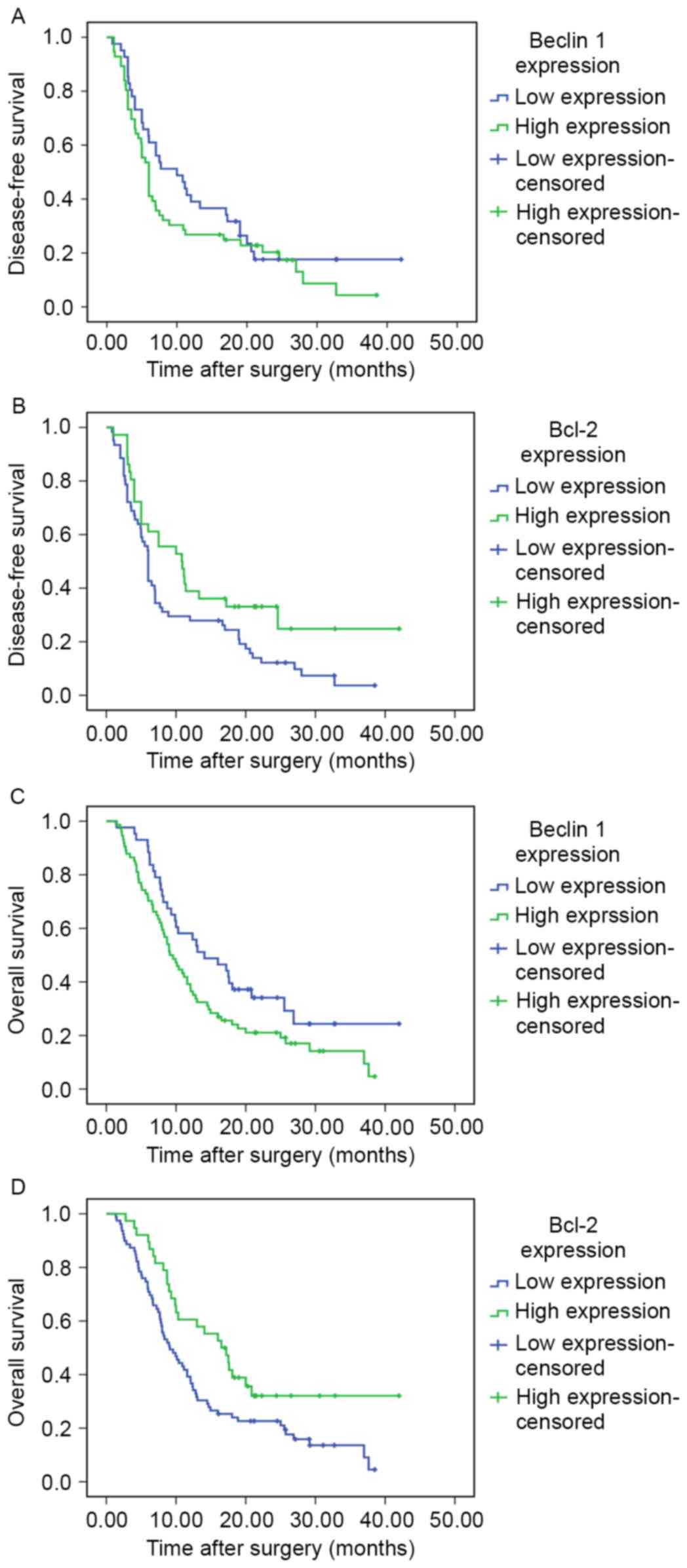
Univariate survival analysis with the Kaplan-Meier
method and log-rank test was used to calculate the effect of
well-established clinical prognostic factors and the levels of
Beclin 1 and Bcl-2 expression on the DFS and OS of patients with
PDAC (Table V). The outcomes
demonstrated that longer DFS was significantly correlated with head
location (P=0.001), improved differentiation (P<0.001), limited
tumor size and local invasion (T stage; P=0.003) and high
expression of Bcl-2 (P=0.030). The median DFS of patients with high
Beclin 1 expression was shorter compared with that of patients with
low expression, although the difference did not reach statistical
significance (Fig. 3A).
 | Table V.Univariate analysis and multivariate
analysis of DFS and OS in pancreatic ductal adenocarcinoma. |
Table V.
Univariate analysis and multivariate
analysis of DFS and OS in pancreatic ductal adenocarcinoma.
|
|
| DFS |
| OS |
|---|
|
|
|
|
|
|
|---|
|
|
| Univariate
analysis | Multivariate
analysis |
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|
|
|
|
|---|
| Variable | Cases, n | Median survival,
months | P-value | HR (95% CI) | P-value | Cases, n | Median survival,
months | P-value | HR (95% CI) | P-value |
|---|
| Age, years |
|
| 0.856 | 0.926
(0.558–1.534) | 0.764 |
|
| 0.567 | 1.071
(0.679–1.687) | 0.769 |
|
<58.98 | 46 | 6.0 |
|
|
| 59 | 9.9 |
|
|
|
|
≥58.98 | 51 | 6.5 |
|
|
| 58 | 11.1 |
|
|
|
| Sex |
|
| 0.292 | 0.913
(0.509–1.637) | 0.760 |
|
| 0.639 | 1.469
(0.871–2.478) | 0.149 |
|
Female | 37 | 7.5 |
|
|
| 47 | 12.1 |
|
|
|
|
Male | 60 | 5.9 |
|
|
| 70 | 10.0 |
|
|
|
| Smoker |
|
| 0.786 | 0.843
(0.482–1.475) | 0.550 |
|
| 0.451 | 0.546
(0.326–0.914) | 0.021a |
| No | 61 | 6.9 |
|
|
| 75 | 11.6 |
|
|
|
|
Yes | 36 | 5.9 |
|
|
| 42 | 8.7 |
|
|
|
| Diabetes |
|
| 0.421 | 1.722
(0.735–4.034) | 0.211 |
|
| 0.499 | 1.336
(0.638–2.798) | 0.443 |
| No | 87 | 6 |
|
|
| 104 | 10.4 |
|
|
|
|
Yes | 10 | 6 |
|
|
| 13 | 10.0 |
|
|
|
| Location |
|
| 0.001a | 0.576
(0.319–1.040) | 0.067 |
|
| 0.004a | 0.826
(0.495–1.379) | 0.465 |
|
Head | 74 | 7.5 |
|
|
| 85 | 12.1 |
|
|
|
|
Body/Tail | 23 | 4.5 |
|
|
| 32 | 7.2 |
|
|
|
|
Differentiation |
|
|
<0.001a | 0.399
(0.190–0.839) | 0.015a |
|
|
<0.001a | 0.394
(0.201–0.774) | 0.007a |
|
Well/Moderate | 86 | 7.0 |
|
|
| 92 | 12.9 |
|
|
|
|
Poor | 11 | 4.5 |
|
|
| 25 | 5.9 |
|
|
|
| T stage |
|
| 0.003a | 0.500
(0.287–0.871) | 0.014a |
|
|
<0.001a | 0.307
(0.175–0.539) |
<0.001a |
|
T1/T2 | 38 | 12.0 |
|
|
| 39 | 20.8 |
|
|
|
|
T3/T4 | 59 | 6.0 |
|
|
| 78 | 8.7 |
|
|
|
| N stage |
|
| 0.388 | 1.084
(0.628–1.870) | 0.773 |
|
| 0.022a | 1.154
(0.679–1.960) | 0.596 |
| N0 | 71 | 6.9 |
|
|
| 73 | 12.8 |
|
|
|
| N1 | 26 | 5.0 |
|
|
| 44 | 7.9 |
|
|
|
| M stage |
|
| – | – | – |
|
|
<0.001a | 0.380
(0.156–0.923) | 0.033a |
| M0 | 97 | 6.0 |
|
|
| 100 | 12.1 |
|
|
|
| M1 | 0 | – |
|
|
| 17 | 4.3 |
|
|
|
| TNM stage |
|
| 0.140 | 0.777
(0.349–1.731) | 0.537 |
|
|
<0.001a | 1.377
(0.647–2.930) | 0.406 |
|
I/II | 85 | 6.5 |
|
|
| 85 | 12.9 |
|
|
|
|
III/IV | 12 | 3.6 |
|
|
| 32 | 6.2 |
|
|
|
| Chemotherapy |
|
| 0.871 | 0.949
(0.515–1.748) | 0.866 |
|
| 0.235 | 2.415
(1.283–4.544) | 0.006a |
| No | 80 | 6.0 |
|
|
| 98 | 9.3 |
|
|
|
|
Yes | 17 | 7.0 |
|
|
| 19 | 13.1 |
|
|
|
| Beclin 1 |
|
| 0.238 | 0.870
(0.532–1.423) | 0.580 |
|
| 0.038a | 0.927
(0.557–1.543) | 0.771 |
| Low
expression | 41 | 10.0 |
|
|
| 43 | 14.1 |
|
|
|
| High
expression | 56 | 6.0 |
|
|
| 74 | 9.1 |
|
|
|
| Bcl-2 |
|
| 0.030a | 1.400
(0.810–2.421) | 0.228 |
|
| 0.017a | 1.850
(1.053–3.249) | 0.032a |
| Low
expression | 61 | 6.0 |
|
|
| 79 | 9.1 |
|
|
|
| High
expression | 36 | 10.8 |
|
|
| 38 | 16.5 |
|
|
|
The effects of prognostic factors on OS was next
analyzed. The results demonstrated that a longer OS was
significantly associated with pancreatic head location (P=0.004),
improved differentiation (P<0.001), limited tumor size and local
invasion (P<0.001), negative lymph node metastasis (P=0.022), no
distant metastasis (P<0.001) and lower TNM stage (P<0.001).
Low expression of Beclin 1 and high expression of Bcl-2 were
predictive factors of improved OS (P=0.038 and P=0.017,
respectively; Fig. 3C and D).
Independent prognostic factors of
PDAC: A multivariate survival analysis
To avoid the bias of univariate analysis, the
expression of Beclin 1, Bcl-2 and other characteristics were
examined by multivariate Cox analysis (Table V). In the multivariate analysis,
Beclin 1 and Bcl-2 were not independent prognostic parameters for
DFS [Beclin 1: Hazard ratio (HR), 0.870; 95% confidence interval
(CI), 0.532–1.423; P=0.580; Bcl-2: HR, 1.400; 95% CI, 0.810–2.421;
P=0.228]. DFS was affected by improved differentiation (HR, 0.399;
95% CI, 0.190–0.839; P=0.015) and limited tumor size and local
invasion (HR, 0.399; 95% CI, 0.190–0.839; P=0.014)
independently.
Bcl-2 was an independent prognostic biomarker for OS
(HR, 1.850; 95% CI, 1.053–3.249; P=0.032), whereas Beclin 1 was not
an independent prognostic parameter for OS (HR, 0.927; 95% CI,
0.557–1.543; P=0.771). No smoking (HR, 0.546; 95% CI, 0.326–0.914;
P=0.021), improved differentiation (HR, 0.394; 95% CI, 0.201–0.774;
P=0.007), limited tumor size and local invasion (HR, 0.307; 95% CI,
0.175–0.539; P<0.001) and chemotherapy following surgery (HR,
2.415; 95% CI, 1.218–4.544; P=0.006) were also associated with
improved OS.
Discussion
The burden of pancreatic cancer is increasing
worldwide, making it a serious health concern. Risk factors such as
older age, smoking and long-term diabetes mellitus have been
associated with pancreatic tumorigenesis (34). Surgical resection is considered the
best potentially curative treatment; however, the majority of
patients are diagnosed at an unresectable locally advanced or
distal metastatic stage due to the aggressiveness of the disease
(34). The effects of surgical
resection on OS remains minimal, and the local failure rate is as
high as 50–80% in patients who successfully undergo surgical
resection, resulting in poor quality of life (35). Pancreatic cancer is difficult to
prevent and diagnose early; it progresses rapidly and exhibits a
poor prognosis. Therefore, extensive studies have been conducted to
understand the mechanisms underlying pancreatic cancer development
at the biochemical, genomic and proteomic levels to inhibit the
progression of pancreatic cancer and to improve patient
prognosis.
Autophagy and apoptosis have been studied
extensively in association with tumor progression in previous
years, particularly Beclin 1 and Bcl-2 as the primary factors in
the 2 programmed cell death pathways. The correlation between
autophagy and apoptosis is complex and varies with cell type and
stress stages (31). Autophagy may
initiate or inhibit apoptosis depending on the cellular context and
stimulus, and the inhibition of autophagy may increase the
sensitivity of cells to apoptotic signals (6). The present study focused on analyzing
the correlation between Beclin 1 and Bcl-2 expression in pancreatic
tissues.
In previous studies, Beclin 1 downregulation was
detected in glioblastoma, hepatocellular carcinoma, esophageal
cancer, non-small cell lung cancer, bladder urothelial tumors and
breast cancer (11–16), whereas Beclin 1 upregulation was
identified in colorectal, ovarian and gastric cancer (17–19). The
correlation between Beclin 1 expression and clinicopathological
characteristics differs among different cancer tissues. Decreased
expression of Beclin 1 is correlated with poor differentiation or
advanced TNM stage, inducing early tumor relapse and causing low OS
in glioblastoma (11), hepatocellular
carcinoma (12), non-small cell lung
cancer (14), breast cancer (16), ovarian cancer (17) and gastric carcinoma (19). Han et al (18) performed a meta-analysis, including six
studies, to evaluate the prognostic significance of Beclin-1
expression in colorectal cancer, and revealed that Beclin 1
overexpression is associated with tumor metastasis and a poor
prognosis in affected patients. Therefore, the effects of Beclin 1
expression levels differ among malignant tissues.
In the present study, high Beclin 1 expression was
observed in 74 (63.2%) PDAC cases, while 43 (36,8%) PDAC cases
exhibited low expression. Compared with the normal ductal epithelia
in CP tissues, patients with PDAC demonstrated high Beclin 1
expression, and the difference was more apparent in poorly
differentiated tissues and patients with advanced TNM stage. In the
analysis of the correlations between Beclin 1 expression and
clinicopathological characteristics, high Beclin 1 expression was
associated with poor histological differentiation and distant
metastasis. The univariate analysis of survival indicated that,
despite a longer median DFS and OS in patients with low Beclin 1
expression compared with that in those patients with high
expression, the difference was not statistically significant. In
the multivariate Cox analysis, although low Beclin 1 expression was
associated with improved OS (P<0.05), it was not an independent
prognostic factor for PDAC. The significant prognostic factors
based on PDAC itself were the differentiation status, local
advancement and distal metastasis. Taken together, these results
suggest that Beclin 1 expression is upregulated in PDAC tissues,
and increased Beclin 1 levels serve a significant role in PDAC
progression. High Beclin 1 expression affects the survival of
patients with PDAC by affecting tumor differentiation, local
advancement and distal metastasis; however, it was not an
independent indicator of prognosis in patients with PDAC in the
present study.
To the best of our knowledge, there is only one
previous study analyzing Beclin 1 expression in patients with PDAC.
In that study, Kim et al (36)
evaluated Beclin 1 expression levels in 63 PDAC cases, with
positive expression in 14 (22.2%) cases and negative expression in
49 (77.8%) cases. The results of correlation and survival analyses
were different from those of the present study, and the
immunohistochemical pattern was also different. The opposite
outcomes may be attributed to differences in the methods used. In
the present study, the Power Vision two-step method was chosen to
perform the immunohistochemical staining, whereas Kim et al
(36) chose the
streptavidin-peroxidase three-step method in their study. In our
opinion, the streptavidin-peroxidase three-step method is not
suited to pancreatic tissue.
Bcl-2 protein is considered a carcinogenic protein,
as it contributes to apoptosis inhibition; its tumorigenic
potential has been demonstrated in animal models (37) and is supported by its overexpression
in a variety of tumors and in lymphomas, in which Bcl-2 acts as an
oncogene (38,39). However, in certain solid tumors, Bcl-2
paradoxically appears to exert a tumor suppressor effect, and its
expression is associated with favorable prognostic features.
Callagy et al (40) performed
a meta-analysis, including 17 studies and 5,892 breast cancer
cases, to determine whether Bcl-2 is an independent prognostic
marker in breast cancer. The meta-analysis clearly supported the
prognostic role of Bcl-2 expression in breast cancer, as assessed
by immunohistochemistry, and demonstrated that it is associated
with DFS and OS. The mechanisms by which Bcl-2 exerts its
protective effects remain unclear.
In the present study, it was demonstrated that Bcl-2
expression was lower in PDAC tissues compared with the normal
ductal epithelium in CP tissues, and that it was associated with
poor differentiation, positive distant metastasis, advanced TNM
stage and a poor prognosis. The outcomes revealed that Bcl-2 is
downregulated in PDAC tissues and that Bcl-2 downregulation
promotes PDAC progression, suggesting that Bcl-2 is an independent
prognostic indicator in PDAC. Consistent with the results of the
present study, previous studies demonstrated decreased Bcl-2
expression in PDAC cancerous foci, and low Bcl-2 expression was
associated with poor differentiation and high TNM stage cases
(26,41,42).
However, the prognostic significance of Bcl-2 expression in
patients with PDAC remains controversial, which may be attributed
to population differences.
Knowlton et al (43) analyzed cell cycle progression in
breast cancer cells and demonstrated a decreased S phase fraction
and an increased G1/G0 fraction in Bcl-2(−)
cells, suggesting that Bcl-2 prolongs the cell cycle. Additionally,
Bcl-2 also enhanced the G0 fraction and delayed
G0 to S transition (44).
Ke et al (45) revealed that
Bcl-2 upregulation serves a critical role in the regulation of cell
adhesion and migration via the formation of Bcl-2 and gelsolin
complexes, leading to the inhibition of cell diffusion, given the
established correlation of cell motility with cancer metastasis.
Despite the antiapoptotic effects favoring tumor survival, these
results may explain why the expression of Bcl-2 in certain tumor
cell types reduces the potential for metastasis and improves
patient prognosis.
Another notable reason for the high relapse and low
5-year OS of PDAC is the poor sensitivity to chemotherapy,
radiotherapy or immunotherapy. Therefore, a number of patients with
PDAC refuse adjuvant therapy subsequent to surgery. As an important
adjuvant therapy following tumor resection, chemotherapy serves an
essential role in preventing tumor relapse and prolonging OS.
Chemotherapy is the adjuvant therapy method considered to be
potentially effective in PDAC (2).
The modulation of cell apoptosis is one of the mechanisms of
chemotherapy. A meta-analysis performed by Yang et al
(46) revealed that Bcl-2 expression
is a predictive factor for chemotherapy sensitivity, and negative
Bcl-2 expression is associated with a good chemotherapy response in
patients with breast cancer. Therefore, the modulation of Bcl-2
expression may potentially benefit additional clinical treatment
for PDAC.
In the present study, Beclin 1 and Bcl-2 levels were
inversely correlated in PDAC tissues. The inverse correlation
between Beclin 1 and Bcl-2 expression has been demonstrated in
previous studies (16,27,28,47). Under
normal conditions, Bcl-2 inhibits Beclin 1, whereas under
conditions of stress, Beclin 1 dissociates from Bcl-2, allowing the
activation of Vps34 and the subsequent stimulation of autophagy
(48). Bcl-2 inhibits autophagy when
bound to Beclin 1 and downregulates Beclin 1, which is associated
with the outcomes of patients in the present study (48). Reduced Bcl-2 expression leads to
decreased interaction with Beclin 1, resulting in increased Beclin
1 levels and the stimulation of autophagy, primarily in patients
with PDAC with poor prognostic factors.
SPN was first described by Frantz in 1959 (4), and defined by the World Health
Organization as a ‘solid pseudopapillary neoplasm’, a low grade
malignant neoplasm of the exocrine pancreas in 2010 (49). SPNs primarily affect young women in
their 20 sec and 30 sec, and generally form a well-demarcated mass
with a mean diameter of 5–10 cm. Despite their large size, the
majority of these tumors behave indolently; complete surgical
resection of SPNs may lead to a favorable prognosis, with a 5-year
survival rate >95% (50).
The present study detected Beclin 1 and Bcl-2
expression in SPN tissues, and detected 26 (60.5%) cases with high
Beclin 1 expression and 11 (25.6%) cases with high Bcl-2
expression. High Beclin 1 expression was significantly correlated
with the presence of nuclear pleomorphism. This result confirmed
that increased Beclin 1 expression leads to poor tumor
differentiation. Unlike PDAC, a direct correlation was detected
between the levels of Beclin 1 and Bcl-2 expression in SPN cases.
Additionally, the expression levels of Beclin 1 and Bcl-2 in normal
ductal epithelium of CP tissues were not correlated. The
differences in expression patterns indicated the tissue specificity
of Beclin 1 and Bcl-2, suggesting that autophagy and apoptosis
exhibit separate regulatory mechanisms in SPN. None of the patients
exhibited tumor relapse, and all patients were alive by the date of
last follow-up.
The present study has several limitations. Firstly,
normalized chemotherapy for PDAC is generally performed based on
the guidelines for pancreatic cancer treatment; however, few
patients undergo chemotherapy due to the poor sensitivity of PDAC
to adjuvant therapy and the ineffectiveness of primary chemotherapy
strategies for PDAC. Therefore, the present study was unable to
collect a large sample size of PDAC cases to analyze the
association between the sensitivity to chemotherapy and Beclin 1
and Bcl-2 expression. Secondly, due to the unknown pathogenesis of
SPNs, the present study was unable to detect changes in Beclin 1
and Bcl-2 expression in comparison with those in normal pancreatic
tissues. Finally, due to the short follow-up time, none of the
patients with SPN exhibited tumor relapse and all patients were
alive by the date of last follow-up. Future studies with a larger
sample size are necessary to overcome these limitations.
To conclude, the results of the present study
suggest that Beclin 1 upregulation and Bcl-2 downregulation in PDAC
promotes cancer progression, and that their expression is inversely
correlated. High expression of Bcl-2 is a favorable prognostic
indicator in PDAC. Unlike the expression pattern in PDAC, Beclin 1
and Bcl-2 are positively correlated in SPN. High Beclin 1
expression may lead to poor progression of neoplasms.
Acknowledgements
The authors would like to thank the Science and
Technology Department of Liaoning Province for supporting the
present study (grant no. 2013225021).
References
|
1
|
Xiao AY, Tan ML, Wu LM, Asrani VM, Windsor
JA, Yadav D and Petrov MS: Global incidence and mortality of
pancreatic diseases: A systematic review, meta-analysis and
meta-regression of population-based cohort studies. Lancet
Gastroenterol Hepatol. 1:45–55. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Parker SL, Tong T, Bolden S and Wingo PA:
Cancer statistics, 1997. CA Cancer J Clin. 47:5–27. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Singh D, Upadhyay G, Srivastava RK and
Shankar S: Recent advances in pancreatic cancer: Biology, treatment
and prevention. Biochim Biophys Acta. 1856:13–27. 2015.PubMed/NCBI
|
|
4
|
Frantz VK: Atlas of tumor pathology,
Section VII, Fascicles 27 and 28. Tumors of the Pancreas.
Washington, D.C.: Armed forces institute of pathology. Brit J Surg.
47:334. 1959.
|
|
5
|
Levine B and Klionsky DJ: Development by
self-digestion: Molecular mechanisms and biological functions of
autophagy. Dev Cell. 6:463–477. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liang XH, Jackson S, Seaman M, Brown K,
Kempkes B, Hibshoosh H and Levine B: Induction of autophagy and
inhibition of tumorigenesis by beclin 1. Nature. 402:672–676. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang CW and Klionsky DJ: The molecular
mechanism of autophagy. Mol Med. 9:65–76. 2003.PubMed/NCBI
|
|
8
|
Shintani T and Klionsky DJ: Autophagy in
health and disease: A double-edged sword. Science. 306:990–995.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Qu X, Yu J, Bhagat G, Furuya N, Hibshoosh
H, Troxel A, Rosen J, Eskelinen EL, Mizushima N, Ohsumi Y, et al:
Promotion of tumorigenesis by heterozygous disruption of the beclin
1 autophagy gene. J Clin Invest. 112:1809–1820. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yue Z, Jin S, Yang C, Levine AJ and Heintz
N: Beclin 1, an autophagy gene essential for early embryonic
development, is a haploinsufficient tumor suppressor. Proc Natl
Acad Sci USA. 100:pp. 15077–15082. 2003, View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Miracco C, Cosci E, Oliveri G, Luzi P,
Pacenti L, Monciatti I, Mannucci S, De Nisi MC, Toscano M,
Malagnino V, et al: Protein and mRNA expression of autophagy gene
Beclin 1 in human brain tumours. Int J Oncol. 30:429–436.
2007.PubMed/NCBI
|
|
12
|
Qiu DM, Wang GL, Chen L, Xu YY, He S, Cao
XL, Qin J, Zhou JM and Zhang YXEQ: The expression of beclin-1, an
autophagic gene, in hepatocellular carcinoma associated with
clinical pathological and prognostic significance. BMC Cancer.
14:3272014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen Y, Lu Y, Lu C and Zhang L: Beclin-1
expression is a predictor of clinical outcome in patients with
esophageal squamous cell carcinoma and correlated to
hypoxia-inducible factor (HIF)-1alpha expression. Pathol Oncol Res.
15:487–493. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhou W, Yue C, Deng J, Hu R, Xu J, Feng L,
Lan Q, Zhang W, Ji D, Wu J, et al: Autophagic protein beclin 1
serves as an independent positive prognostic biomarker for
non-small cell lung cancer. PLoS One. 8:e803382013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Baspinar S, Bircan S, Yavuz G and
Kapucuoglu N: Beclin 1 and bcl-2 expressions in bladder urothelial
tumors and their association with clinicopathological parameters.
Pathol Res Pract. 209:418–423. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dong M, Wan XB, Yuan ZY, Wei L, Fan XJ,
Wang TT, Lv YC, Li X, Chen ZH, Chen J, et al: Low expression of
beclin 1 and elevated expression of HIF-1α refine distant
metastasis risk and predict poor prognosis of ER-positive,
HER2-negative breast cancer. Med Oncol. 30:3552013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cai M, Hu Z, Liu J, Gao J, Liu C, Liu D,
Tan M, Zhang D and Lin B: Beclin 1 expression in ovarian tissues
and its effects on ovarian cancer prognosis. Int J Mol Sci.
15:5292–5303. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Han Y, Xue XF, Shen HG, Guo XB, Wang X,
Yuan B, Guo XP, Kuang YT, Zhi QM and Zhao H: Prognostic
significance of beclin-1 expression in colorectal cancer: A
meta-analysis. Asian Pac J Cancer Prev. 15:4583–4587. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chen YB, Hou JH, Feng XY, Chen S, Zhou ZW,
Zhang XS and Cai MY: Decreased expression of beclin 1 correlates
with a metastatic phenotypic feature and adverse prognosis of
gastric carcinomas. J Surg Oncol. 105:542–547. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Korsmeyer SJ: Bcl-2 initiates a new
category of oncogenes: Regulators of cell death. Blood. 80:879–886.
1992.PubMed/NCBI
|
|
21
|
Seto M, Jaeger U, Hockett RD, Graninger W,
Bennett S, Goldman P and Korsmeyer SJ: Alternative promoters and
exons, somatic mutation and deregulation of the Bcl-2-Ig fusion
gene in lymphoma. EMBO J. 7:123–131. 1988.PubMed/NCBI
|
|
22
|
Reed JC, Miyashita T, Krajewski S,
Takayama S, Aime-Sempe C, Kitada S, Sato T, Wang HG, Harigai M,
Hanada M, et al: Bcl-2 family proteins and the regulation of
programmed cell death in leukemia and lymphoma. Cancer Treat Res.
84:31–72. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Naccarato AG, Viacava P, Vignati S,
Fanelli G, Bonadio AG, Montruccoli G and Bevilacqua G:
Bio-morphological events in the development of the human female
mammary gland from fetal age to puberty. Virchows Arch.
436:431–438. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Reed JC, Miyashita T, Takayama S, Wang HG,
Sato T, Krajewski S, Aimé-Sempé C, Bodrug S, Kitada S and Hanada M:
BCL-2 family proteins: Regulators of cell death involved in the
pathogenesis of cancer and resistance to therapy. J Cell Biochem.
60:23–32. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Teraki Y and Shiohara T: Apoptosis and the
skin. Eur J Dermatol. 9:413–425. 1999.PubMed/NCBI
|
|
26
|
Tomaszewska R, Karcz D and Stachura J: An
immunohistochemical study of the expression of bcl-2 and p53
oncoproteins in pancreatic intraepithelial neoplasia and pancreatic
cancer. Int J Pancreatol. 26:163–171. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Won KY, Kim GY, Kim YW, Song JY and Lim
SJ: Clinicopathologic correlation of beclin-1 and bcl-2 expression
in human breast cancer. Hum Pathol. 41:107–112. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Baspinar S, Bircan S, Orhan H, Kapucuoglu
N and Bozkurt KK: The relation of beclin 1 and bcl-2 expressions in
high grade prostatic intraepithelial neoplasia and prostate
adenocarcinoma: A tissue microarray study. Pathol Res Pract.
210:412–418. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Liang XH, Kleeman LK, Jiang HH, Gordon G,
Goldman JE, Berry G, Herman B and Levine B: Protection against
fatal sindbis virus encephalitis by beclin, a novel
Bcl-2-interacting protein. J Virol. 72:8586–8596. 1998.PubMed/NCBI
|
|
30
|
Decuypere JP, Parys JB and Bultynck G:
Regulation of the autophagic bcl-2/beclin 1 interaction. Cells.
1:284–312. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhou F, Yang Y and Xing D: Bcl-2 and
Bcl-xL play important roles in the crosstalk between autophagy and
apoptosis. FEBS J. 278:403–413. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Cao SS, Su AP, Du XJ, Li A, Hu WM, Zhang
ZD, Tian BL, Lu HM, Ke NW and He ZP: The expressions and
correlation of bcl-2 and beclin-1 in pancreatic cancer. Sichuan Da
Xue Xue Bao Yi Xue Ban. 43:156–160. 2012.(In Chinese). PubMed/NCBI
|
|
33
|
Chun YS, Pawlik TM and Vauthey JN: 8th
Edition of the AJCC cancer staging manual: Pancreas and
hepatobiliary cancers. Ann Surg Oncol. 2017.(Epub ahead of
print).
|
|
34
|
Song S, Wang B, Zhang X, Hao L, Hu X, Li Z
and Sun S: Long-term diabetes mellitus is associated with an
increased risk of pancreatic cancer: A meta-analysis. PloS one.
10:e01343212015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Asiyanbola B, Gleisner A, Herman JM, Choti
MA, Wolfgang CL, Swartz M, Edil BH, Schulick RD, Cameron JL and
Pawlik TM: Determining pattern of recurrence following
pancreaticoduodenectomy and adjuvant 5-flurouracil-based
chemoradiation therapy: Effect of number of metastatic lymph nodes
and lymph node ratio. J Gastrointest Surg. 13:752–759. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kim HS, Lee SH, Do SI, Lim SJ, Park YK and
Kim YW: Clinicopathologic correlation of beclin-1 expression in
pancreatic ductal adenocarcinoma. Pathol Res Pract. 207:247–252.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
McDonnell TJ and Korsmeyer SJ: Progression
from lymphoid hyperplasia to high-grade malignant lymphoma in mice
transgenic for the t (14; 18). Nature. 349:254–256. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
McDonnell TJ, Troncoso P, Brisbay SM,
Logothetis C, Chung LW, Hsieh JT, Tu SM and Campbell ML: Expression
of the protooncogene bcl-2 in the prostate and its association with
emergence of androgen-independent prostate cancer. Cancer Res.
52:6940–6944. 1992.PubMed/NCBI
|
|
39
|
Pietenpol JA, Papadopoulos N, Markowitz S,
Willson JK, Kinzler KW and Vogelstein B: Paradoxical inhibition of
solid tumor cell growth by bcl2. Cancer Res. 54:3714–3717.
1994.PubMed/NCBI
|
|
40
|
Callagy GM, Webber MJ, Pharoah PD and
Caldas C: Meta-analysis confirms BCL2 is an independent prognostic
marker in breast cancer. BMC Cancer. 8:1532008. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Campani D, Esposito I, Boggi U, Cecchetti
D, Menicagli M, De Negri F, Colizzi L, Del Chiaro M, Mosca F,
Fornaciari G and Bevilacqua G: Bcl-2 expression in pancreas
development and pancreatic cancer progression. J Pathol.
194:444–450. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Casneuf VF, Fonteyne P, Van Damme N,
Demetter P, Pauwels P, de Hemptinne B, De Vos M, Van de Wiele C and
Peeters M: Expression of SGLT1, Bcl-2 and p53 in primary pancreatic
cancer related to survival. Cancer Invest. 26:852–859. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Knowlton K, Mancini M, Creason S, Morales
C, Hockenbery D and Anderson BO: Bcl-2 slows in vitro breast cancer
growth despite its antiapoptotic effect. J Surg Res. 76:22–26.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zinkel S, Gross A and Yang E: BCL2 family
in DNA damage and cell cycle control. Cell Death Differ.
13:1351–1359. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Ke H, Parron VI, Reece J, Zhang JY,
Akiyama SK and French JE: BCL2 inhibits cell adhesion, spreading,
and motility by enhancing actin polymerization. Cell Res.
20:458–469. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Yang D, Chen MB, Wang LQ, Yang L, Liu CY
and Lu PH: Bcl-2 expression predicts sensitivity to chemotherapy in
breast cancer: A systematic review and meta-analysis. J Exp Clin
Cancer Res. 32:1052013. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Jiang LC, Huang SY, Zhang DS, Zhang SH, Li
WG, Zheng PH and Chen ZW: Expression of beclin 1 in primary
salivary adenoid cystic carcinoma and its relation to Bcl-2 and p53
and prognosis. Braz J Med Biol Res. 47:252–258. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Pattingre S, Tassa A, Qu X, Garuti R,
Liang XH, Mizushima N, Packer M, Schneider MD and Levine B: Bcl-2
antiapoptotic proteins inhibit beclin 1-dependent autophagy. Cell.
122:927–939. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Klöppel G, Hruban R, Klimstra D, et al:
Solid-pseudopapillary Tumor of Pancreas. Bosman FT, Carneiro F,
Hruban RH and Theise ND: 327–333. 2010.
|
|
50
|
Potrc S, Kavalar R, Horvat M and Gadzijev
EM: Urgent Whipple resection for solid pseudopapillary tumor of the
pancreas. J Hepatobiliary Pancreat Surg. 10:386–389. 2003.
View Article : Google Scholar : PubMed/NCBI
|