Introduction
Hepatocellular carcinoma (HCC) is the most common
primary malignant cancer in the liver, accounting for ~90% of liver
cancer cases and ranking as the fifth most common cancerous disease
in males and the ninth in females worldwide in 2012 (1). In total, 30–40% of patients with HCC in
Asia are suitable for potentially curative therapy, including
surgical resection and liver transplantation, since patients are
often diagnosed at moderate and advanced stages (2).
Transcatheter arterial chemoembolization (TACE) is
recommended for the treatment of advanced patients with HCC
worldwide. This approach is based on blocking the arteries feeding
the tumor, causing irreversible damage (3), necrosis and apoptosis of local tumor
cells and endothelial cells in an ischemic anoxia environment and
thereby inhibiting the growth of tumor cells, as confirmed using
two meta analyses (4,5). For those patients not eligible to
receive surgical resection and who are candidates to receive
systemic chemotherapy or conservative treatment, TACE serves as an
improved, more tolerable option (6).
TACE may benefit patients with HCC preoperatively and
postoperatively. Preoperative TACE may shrink the tumor volume,
reduce the blood supply to the tumor, make surgical excisions
easier and embolize small, difficult to visualize tumors (7). Postoperative TACE is used to treat
recurrent HCC and may improve the survival rate and slow the
progression of the disease (8).
However, opposing arguments suggest that
preoperative TACE may damage liver function, possibly leading to
liver failure, and that it may delay surgical resection, make
previously resectable liver cancer unresectable and leave residual
tumor cells that are more aggressive in cases of
poorly-differentiated HCC. Furthermore, incomplete tumor necrosis
may reduce the adhesion of tumor cells, allowing them free access
to the blood, which may result in intrahepatic or extrahepatic
metastasis (9). Postoperative TACE
may also damage the residual liver function and activate the
hepatitis B virus, which may in turn lead to extrahepatic
metastases and a poor prognosis (10,11).
Whether TACE promotes progression remains controversial, and a
number of studies have focused on the influence of TACE on numerous
tumor progression-associated factors, including the expression of
vascular endothelial growth factor (VEGF) and hypoxia inducible
factor 1-α. It has been proposed that TACE may create a
hypoxic-ischemic environment that would increase the expression of
such factors, promote the angiogenesis of HCC, and initiate the
recurrence and metastasis of HCC (12–14).
Cluster of differentiation (CD)151 was the first
tetraspanin to be associated with tumour metastasis (15), including gastric, colon, lung and
prostate cancer metastasis (16–19), and
is believed to be associated with a poor prognosis. A previous
study conducting an in vitro experiment demonstrated that
cells expressing high levels of CD151 secrete more matrix
metalloproteinase (MMP)-9 and possess a marked ability for invasion
and metastasis, whilst in the same previous study an in vivo
experiment demonstrated that patients expressing high levels of
CD151 exhibited a decreased overall survival rate at 3, 5 and 7
years and an increased recurrence rate (15).
The present study aimed to prospectively assess the
level of serum CD151 prior to and following TACE, and its
association with clinicopathological characteristics.
Materials and methods
Materials and reagents
The equipment and reagents used in this study
included a digital angiography machine (Innova 3100; GE Healthcare,
Chicago, IL, USA), a high-pressure injector (Medrad Mark V ProVis;
Bayer, Newbury, UK), 2% lidocaine hydrochloride (Shanghai Zhaohui
Pharmaceutical Co., Ltd, Shanghai, China), an 18-G puncture needle
(Terumo Medical Corporation, Tokyo, Japan), a 5-F arterial sheath
(Terumo Medical Corporation), a 5-F Yashiro catheter (Terumo
Medical Corporation), a 5-F RH catheter (Terumo Medical
Corporation), an 0.035-inch Loach guide wire (Terumo Medical
Corporation), a microtubule (Terumo Medical Corporation), micro
guide wire (Terumo Medical Corporation), ioversol (100 ml:67.8 g;
Jiangsu Hengrui Medicine Co., Ltd., Lianyungang, China), iodinized
oil (1 ml; Shandong Luyin Pharmaceutical Co., Shandong, China),
pirarubicin (10 mg; Shenzhen Wanle Pharmaceutical Co. Ltd.,
Shenzhen, China), fluorouracil (10 ml: 0.25 g; Hainan Zhonghua
United Pharmaceutical Industry Co. Ltd., Hainan, China), nedaplatin
(10 mg; Aosaikang Pharmaceutical Co. Ltd., Jiangsu, China), a CD151
ELISA detection kit (cat. no. CSB-EL00HU; Cusabio Life Science,
Baltimore, MD, USA), a high-speed centrifuge (Thermo Fisher
Scientific, Inc., Waltham, MA, USA), a microplate absorbance reader
(Thermo Fisher Scientific, Inc.) and a pipettor (Eppendorf,
Hamburg, Germany).
Inclusion/exclusion criteria
The inclusion criteria were as follows: Patients
with HCC, regardless of primary or recurrent disease or metastasis,
with a diagnosis based on clinical symptoms (emaciation, anorexia,
abdominal distension, abdominal pain or liver mass, etc.) and
imaging [liver mass on computed tomography (CT) or magnetic
resonance imaging (MRI)] and a serological α-fetoprotein (AFP)
level of >400 ng/ml or confirmation using pathological analysis.
The exclusion criteria consisted of patients with HCC confirmed
clinically or pathologically but who rejected TACE.
Serum specimen collection and
conservation
The present study was approved by Ethics Committee
of the Second Xiangya Hospital (Changsha, China) and written
informed consent was collected from each patient who took part in
this study. Blood specimens were collected pre-TACE, at 5–7 days
post-TACE and at 30 days post-TACE. Samples were centrifuged in a
high-speed centrifuge (1,006.2 × g at 4°C for 3 min) and the serum
was collected and stored in Eppendorf tubes at −70°C.
TACE procedures
Radiologists at the Second Xiangya Hospital
performed TACE procedures. Following anesthesia of the right
femoral artery sheath with 2% lidocaine and deposition of a 5-F
arterial sheath, a vascular catheter was inserted into the celiac
artery. Following conventional hepatic angiography, a vascular
catheter was subsequently inserted superselectively into the branch
of the hepatic artery that was believed to feed the tumor.
Chemoembolization was then performed. Lipiodol (10 ml) was mixed
with 40 mg pirarubicin, 80 mg nedaplatin and 1 g fluorouracil to
create an emulsified milky solution. The emulsion was slowly
infused into the liver tumor. The dose administered depended on the
size of the HCC tumor, the position of the catheter, the patient's
liver function, and the patient's tolerance and response to
previous courses of TACE. The embolization procedure was abandoned
if the patient was unable to tolerate treatment or approached
predetermined limits of 15 ml emulsion or the emulsion flow showed
stasis or backflow.
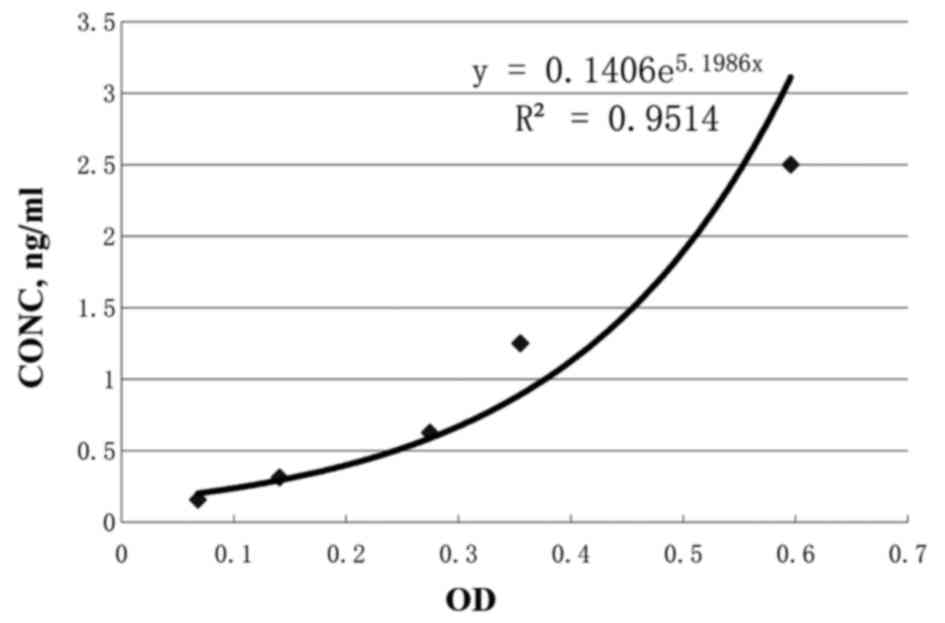
ELISA measurement of serum CD151
A detection kit for human serum CD151 was used
according to the manufacturer's protocol. The minimum concentration
of human CD151 that could be detected was 0.039 ng/ml. Optical
density (OD) values were transformed to the concentration of serum
CD151. Standard curves were calculated using the standard provided
with the kit. The standard specimen information is presented in
Table I. Based on the OD values
measured using ELISA and the corresponding concentration of CD151,
a scatter diagram was created and the following equation/values
were obtained: y=0.1406e5.1986x, R2=0.9514
(Fig. 1).
 | Table I.Information for the standard
specimen. |
Table I.
Information for the standard
specimen.
| Serial | S5 | S4 | S3 | S2 | S1 | S0 |
|---|
| Absorbance (blank
removed) |
0.5957 |
0.3550 |
0.2746 |
0.1408 |
0.0681 |
0.0000 |
| Concentration,
ng/ml | 2.500 | 1.250 | 0.625 | 0.312 | 0.156 | 0.000 |
Statistical analysis
SPSS (version 17.0; SPSS, Inc., Chicago, IL, USA),
MedCalc (version 11.4.2.0; MedCalc Software bvba, Ostend, Belgium)
and GraphPad Prism (version 5.0; GraphPad Software, Inc., La Jolla,
CA, USA) software were used for the statistical analysis.
Descriptive statistics of the serum CD151 level were used to
calculate the means and ranges of the distribution (range and
standard deviation). Mann Whitney test was used to compare
differences between two independent samples. Paired Student's
t-tests were used to compare differences between the serum CD151
values pre- and post-TACE. Correlation analysis was used to
evaluate the correlation of measurement data. Kaplan-Meier
estimator analysis was used to generate the survival curve.
Single-factor and multi-factor logistic regression analyses were
used to assess the risk factors associated with the progression of
HCC. Receiver operating characteristic (ROC) curves were generated
to assess CD151 expression in predicting the progression of HCC.
Threshold values for neutrophil to lymphocyte ratio (NLR), platelet
to lymphocyte ratio (PLR) and platelet count were based on previous
studies (20–22). A two-tailed P-value of <0.05 was
considered to indicate a statistically significant difference.
Results
Clinical data of the included
patients
Patients with HCC (n=28) were selected, including 26
males and 2 females. A total of 21 patients had not previously
received TACE, while 7 patients had previously received TACE. The
majority of patients were diagnosed according to their clinical
symptoms, together with imaging results and serum AFP levels
(>400 ng/ml), while the 7 remaining patients were diagnosed
using pathological analysis through CT-guided biopsy due to serum
AFP levels being below the aforementioned threshold. The mean
average age of these patients was 49.8±17.7 years (range, 22–72
years). Hepatitis B surface antigen (HBsAg) positivity was
identified in 23/28 patients. Of all the selected patients, 24 were
classified as Child-Pugh A and 4 as Child-Pugh B (23). The tumor mass measured 8.5–13 cm in
the treatment-naïve patients. Portal thrombus was identified in 10
patients. A total of 9 patients had recurrent or metastatic HCC
presenting with multiple nodules upon imaging. The 7 patients who
had received TACE previously exhibited poor iodinized oil
deposition and required intensive therapy. The baseline clinical
data are presented in Table II.
 | Table II.Baseline clinical data of the
included patients. |
Table II.
Baseline clinical data of the
included patients.
| Characteristic | n |
|---|
| Sex |
|
|
Male | 26 |
|
Female | 2 |
| HBsAg |
|
| + | 23 |
| − | 5 |
| TACE received prior
to study |
|
|
Treatment naïve | 21 |
| >1
session | 7 |
| Child-Pugh
stage |
|
| A | 24 |
| B | 4 |
| C | 0 |
| Vascular
invasion |
|
| Portal
thrombus | 10 |
| No
vascular invasion | 18 |
| AFP level,
ng/ml |
|
|
>400 | 21 |
|
<400 | 7 |
| HCC type |
|
|
Recurrent or metastatic
HCC | 9 |
| Primary
HCC | 19 |
Expression of serum CD151 in patients
with HCC treated by TACE
Serum CD151 expression pre-TACE and the
association with the baseline clinical data
The expression of CD151 pre-TACE and the association
with the baseline clinical data were analyzed. The Mann Whitney
test revealed that the expression of CD151 pre-TACE demonstrated no
statistically significant association with the patient's age, sex,
HBsAg status, vascular invasion status, AFP level, HCC type, NLR,
PLR, platelet count or TACE number received, as presented in
Table III.
 | Table III.Association between CD151 expression
pre-TACE and at 5–7 days post-TACE and the baseline clinical
data. |
Table III.
Association between CD151 expression
pre-TACE and at 5–7 days post-TACE and the baseline clinical
data.
| Variants | CD151 pre-TACE,
ng/ml | P-value
(Mann-Whitney test) | CD151 5–7 days
post-TACE, ng/ml | P-value
(Mann-Whitney test) |
|---|
| Age, years |
| 0.71 |
| 0.8 |
| ≥50
(n=14) |
0.34±0.08 |
|
0.46±0.17 |
|
| ≤50
(n=14) |
0.37±0.11 |
|
0.45±0.12 |
|
| Sex |
| 0.05 |
|
|
| Male
(n=26) |
0.34±0.1 |
|
0.45±0.15 | 0.18 |
| Female
(n=2) |
0.49±0.04 |
|
0.58±0.08 |
|
| HBsAg |
| 0.06 |
| 0.37 |
| +
(n=23) |
0.37±0.1 |
|
0.45±0.16 |
|
| −
(n=5) |
0.29±0.03 |
|
0.49±0.1 |
|
| Vascular
invasion |
| 0.06 |
| 0.28 |
| Portal
thrombus (n=10) |
0.4±0.1 |
|
0.51±0.19 |
|
| No
vascular invasion (n=18) |
0.33±0.07 |
|
0.42±0.11 |
|
| AFP, ng/ml |
| 0.56 |
| 0.06 |
| >400
(n=21) |
0.36±0.11 |
|
0.42±0.13 |
|
| <400
(n=7) |
0.33±0.06 |
|
0.56±0.17 |
|
| HCC type |
| 0.09 |
| 0.004a |
| Primary
HCC (n=19) |
0.33±0.08 |
|
0.41±0.15 |
|
|
Recurrent or metastatic HCC
(n=9) |
0.4±0.11 |
|
0.55±0.09 |
|
| NLR |
| 0.77 |
| 0.87 |
|
<1.85 (n=7) |
0.33±0.02 |
|
0.48±0.21 |
|
|
>1.85 (n=21) |
0.36±0.11 |
|
0.45±0.13 |
|
| PLR |
| 0.72 |
| 0.77 |
|
<111.23 (n=4) |
0.35±0.06 |
|
0.52±0.28 |
|
|
>111.23 (n=24) |
0.36±0.1 |
|
0.44±0.12 |
|
| Platelet count |
| 0.69 |
| 0.95 |
| <118
(n=4) |
0.35±0.06 |
|
0.52±0.28 |
|
| >212
(n=13) |
0.35±0.1 |
|
0.46±0.1 |
|
| TACE received |
| 0.20 |
| 0.79 |
|
Treatment-naïve (n=21) |
0.34±0.1 |
|
0.46±0.15 |
|
| >1
(n=7) |
0.4±0.11 |
|
0.46±0.14 |
|
Serum CD151 expression 5–7 days post-TACE and the
association with the baseline clinical data
The expression levels of CD151 5–7 days post-TACE
and the association with the baseline clinical data were analyzed,
and the Mann Whitney test revealed that the expression of CD151 5–7
days post-TACE was significantly increased in recurrent or
metastatic HCC compared with primary HCC (P=0.004; Table III).
Comparison of CD151 expression pre-TACE and at
5–7 days post-TACE
The mean average CD151 expression level pre-TACE was
0.35 ng/ml, compared with 0.46 ng/ml at 5–7 days post-TACE, with
the paired t-test revealing a statistically significant difference
between time points (P<0.001; Table
IV; Fig. 2).
 | Table IV.Comparison of CD151 pre-TACE and at
5–7 days post-TACE. |
Table IV.
Comparison of CD151 pre-TACE and at
5–7 days post-TACE.
| Time | CD151, ng/ml | P-value (two-tailed
test) |
|---|
| Pre-TACE
(n=28) |
0.35±0.1 |
|
| 5–7days post-TACE
(n=28) |
0.46±0.15 | P<0.001 |
Comparison of CD151 expression pre-TACE and at 30
days post-TACE
Serum specimens from 12 patients with HCC who were
not previously treated were obtained at 30 days post-TACE. A paired
student's t-test revealed no significant difference in the
expression of CD151 pre-TACE and at 30 days post-TACE (Table V; Fig.
3).
 | Table V.Comparison of CD151 pre-TACE and at
30 days post-TACE. |
Table V.
Comparison of CD151 pre-TACE and at
30 days post-TACE.
| Time | CD151, ng/ml | P-value (two-tailed
test) |
|---|
| Pre-TACE
(n=12) |
0.35±0.1 |
|
| 30 days post-TACE
(n=12) |
0.42±0.2 | P=0.09 |
CD151 expression pre- and post-TACE
Among the 12 patients who provided serum samples for
all three time points, the mean average levels of CD151 expression
pre-TACE, at 5–7 days post-TACE and at 30 days post-TACE were 0.35,
0.41 and 0.42 ng/ml, respectively. These results identified a
tendency for a rapid increase followed by a relatively slower
increase, although no statistically significant differences were
identified (P=0.44; Fig. 4).
Follow-up standard
Imaging and digital subtraction angiography findings
for patients who received a second TACE treatment were reviewed,
and the Response Evaluation Criteria for Solid Tumors (24) were modified and applied for assessment
of the progression of HCC. During imaging analysis, tumor
progression was reported if the largest diameter of the mass had
increased since the previous examination or if a new mass or nodule
was noted beside the previous mass (Fig.
5). On the digital subtraction angiograph, tumor progression
was considered if the feeding blood vessels had increased in size
or vascularity and were disordered. However, if the mass did not
exhibit any marked change in size or vascularity, the tumor was not
considered to have progressed and remained under control (Fig. 6).
Follow-up data
During the 18-month follow-up period, 9/28 patients
were lost to follow-up and 2 outpatients exhibited tumor
progression and did not receive additional treatment. A total of 11
patients were regarded as censored. The remaining 17 patients
received the second TACE treatment within the first 2 months. At
the 7-month interval, 12 patients had survived and received another
TACE treatment. By the 1-year interval, 9 patients had survived. At
the end of 18 months, 5 patients remained (Table VI). Using these data, the approximate
survival rate was calculated, revealing a decrease in overall
survival rate with time (Fig. 7).
 | Table VI.Follow-up data for the included
patients by time interval. |
Table VI.
Follow-up data for the included
patients by time interval.
| Follow-up time,
months | Patients
remaining | TACE
treatments | Survival rate,
% |
|---|
| 0 | 28 | 1 | 100.0 |
| 2 | 17 | 2 | 60.7 |
| 7 | 12 | ≥2 | 42.9 |
| 12 | 9 | ≥3 | 32.1 |
| 15 | 7 | ≥3 | 25.0 |
| 18 | 5 | 3–5 | 17.9 |
Risk factors associated with the progression of
HCC for patients receiving their first TACE
Following the first TACE treatment, 9 patients were
censored and classed as exhibiting tumor progression. For the
remaining 19 patients, their medical records were reviewed, along
with angiography and CT or MRI images. A total of 9 patients
demonstrated marked tumor progression, while the other 10 patients
exhibited no tumor progression. In total, there were 18 patients
with tumor progression and 10 patients with no tumor progression.
Single-factor analysis identified that preoperative high levels of
AFP (>400 ng/ml), CD151 expression pre-TACE and CD151 expression
5–7 days post-TACE were risk factors for tumor progression
following a single TACE treatment. Embolism volume was a protective
factor. Multiple factor analysis failed to provide significant
results (Table VII).
 | Table VII.Risk factor associations with tumor
progression after the first TACE, as assessed by logistic
regression analysis. |
Table VII.
Risk factor associations with tumor
progression after the first TACE, as assessed by logistic
regression analysis.
|
| Single-factor
analysis | Multiple factor
analysis |
|---|
|
|
|
|
|---|
| Variable | Test statistic | P-value | Test statistic | P-value |
|---|
| Categorical |
|
|
|
|
|
HBsAg | 1.564a | 0.315 |
|
|
|
Vascular invasion | 0.221a | 0.703 |
|
|
|
AFP | 5.185a | 0.03b | 0.000 | 0.998 |
| HCC
type | 1.052a | 0.417 |
|
|
| TACE
received | 1.052a | 0.417 |
|
|
|
NLR | 5.185a | 0.063 |
|
|
|
PLR | 0.415a | 0.601 |
|
|
| Continuous |
|
|
|
|
| CD151
expression pre-TACE | −2.891c | 0.008b | 2.915 | 0.088 |
| CD151
expression at 5–7 days post-TACE | −2.353c | 0.026b | 2.760 | 0.097 |
|
Embolism volume | 2.999c | 0.006b | 2.696 | 0.101 |
The predictive value of CD151 expression pre-TACE
and 5–7 days post-TACE for tumor progression was analyzed. ROC
analysis revealed that for a CD151 expression level of >0.3247
ng/ml pre-TACE, the sensitivity and specificity to predict tumor
progression were 66.7 and 80.0%, respectively, with an area under
the curve (AUC) of 0.753 (95% confidence interval (CI),
0.554–0.895; P=0.007). For a CD151 expression level of >0.3146
ng/ml at 5–7 days post-TACE, the sensitivity and specificity to
predict tumor progression were 94.4 and 50.0%, respectively, with
an AUC of 0.761 (95% CI, 0.563–0.901; P=0.007) (Fig. 8).
Risk factors associated with the progression of
HCC for patients at the end of follow-up
The patients were followed up for 18 months. A total
of 5 patients exhibited no marked tumor progression, while 14
patients presented with hepatic masses that grew larger or
exhibited blood vessels of increased size or vascularity on digital
subtraction angiography. In total, 23 patients were deemed to have
experienced tumor progression, and 5 patients were deemed to have
experienced no tumor progression. Single-factor analysis identified
that HBsAg positivity and an NLR of >1.85 at the end of
follow-up were risk factors for tumor progression among patients
receiving TACE. Furthermore, the total number of TACE treatments
received and the embolism volume were protective factors (Table VIII). Multiple factor analysis
failed to identify any statistically significant differences.
 | Table VIII.Risk factors correlating with tumour
progression at the end of follow-up, as assessed by logistic
regression analysis. |
Table VIII.
Risk factors correlating with tumour
progression at the end of follow-up, as assessed by logistic
regression analysis.
|
| Single-factor
analysis | Multiple factor
analysis |
|---|
|
|
|
|
|---|
| Variable | Test statistic | P-value | Test statistic | P-value |
|---|
| Categorical |
|
HBsAg | 7.370a | 0.027b | 0 | 0.998 |
|
Vascular invasion | 3.382a | 0.128 |
|
|
|
AFP | 2.029a | 0.290 |
|
|
| HCC
type | 2.883a | 0.144 |
|
|
|
NLR | 18.261a |
<0.001b | 0 | 0.997 |
|
PLR | 3.287a | 0.135 |
|
|
| Ordinal |
| Total
TACE received | 7c | 0.002b | 0 | 0.996 |
| Continuous |
| CD151
expression pre-TACE | −1.228d | 0.230 |
|
|
| CD151
expression at 5–7 days post-TACE | −1.473d | 0.153 |
|
|
|
Embolism volume | 3.824d | 0.001b | 0 | 0.996 |
Discussion
CD151 was first identified on the surface of
platelets by Ashman et al (25) in 1991 and was referred to as
platelet-endothelial tetraspan antigen-3, the activation of which
led to platelet aggregation. Later, cDNA for CD151 was isolated
from the meganucleus metrocyte leukemia MO7e cell line and the
adult T lymphocytic leukemia SF-HT cell line. In 1997, fluorescence
in situ hybridization located the gene for CD151 on
chromosome 11p15.5, and gene and protein analysis identified CD151
as part of the tetraspanin family (26,27). This
molecule was nominated to join the CD molecular family at the 6th
International Human Leucocyte Differentiation Antigen conference
(28) and was designated CD151. CD151
is widely expressed in human tissues, including the myocardium,
smooth muscle, skeletal muscle cells, endothelial cells, and
immune-related Schwann cells and dendritic cells (29). CD151 is now considered an important
molecule that is involved in tumor progression. A previous study
conducting in vivo, in vitro and clinical experiments has
demonstrated that CD151 is involved in tumor progression at
different levels (15); CD151 may
impact the behaviour of tumor cells, assist tumor cells in
communicating with neighbouring cells and the microenvironment, and
regulate the events following tumor adhesion, including cell
proliferation, migration and invasion, and the subsequent processes
of infiltration and metastasis. These molecular mechanisms involved
in cancer processes are based on the ability of CD151 to interact
with integrins (α3β1, α6β1 and α6β4), growth factor receptors
(hepatocyte growth factor receptor, epidermal growth factor
receptor and transforming growth factor-β1 receptor) and MMPs
(MMP-7, MMP-2 and MMP-9), which together are involved in the
development of cancer (30).
The present study demonstrated that pre-TACE, CD151
expression had no statistical correlation with age, sex, hepatitis
B status, vascular invasion, AFP, HCC type, TACE number received,
NLR, PLR or platelet count. Post-TACE, CD151 expression in
recurrent or metastatic liver cancer cases was significantly more
increased compared with the increase observed in primary HCC cases,
suggesting that the CD151 expression level is associated with
distinct types of HCC following TACE treatment. The results of the
present study suggested that CD151 is involved in the metastasis of
HCC, which is consistent with the results of the study by Ke et
al (15). CD151 expression tended
to exhibit a rapid increase within 5–7 days post-TACE, followed by
a smaller increase between 5–7 and 30 days post-TACE. The rapid
early increase in CD151 may indicate the invasive characteristics
of tumor cells due to the ischemic anoxic environment.
Univariate analysis identified that factors
associated with tumor progression following a single TACE treatment
included AFP, pre-TACE CD151 and post-TACE CD151. A previous study
demonstrated that AFP may promote AKT phosphorylation through
interaction with the phosphatase and tensin homolog protein,
thereby increasing the expression of the C-X-C chemokine receptor
type 4 (CXCR4) protein (also known as stromal-derived factor-1α)
(31). At the same time, mechanistic
target of rapamycin enters the nucleus to combine with the CXCR4
gene promoter, which promotes the growth and metastasis of HCC
(28). CD151 was the first
tetraspanin to be associated with tumor metastasis. The present
study identified pre-TACE CD151 and post-TACE CD151 expression as
risk factors for HCC progression following a single TACE treatment.
The results also suggested that interactions may occur between
CD151 and AFP. CD151 is able to upregulate MMP-9 through the
phosphoinositide 3-kinase/Akt/glycogen synthase kinase-3β/snail
signaling pathways (32) and form
functional complexes with integrins α3β1 and α6β1 to promote tumor
invasion and metastasis (33,34). However, no studies have focused on
CD151 and AFP complex formation or signal interaction, which may
serve as a promising focus of future research, particularly the
genes and underlying molecular mechanisms involved. It has been
demonstrated that VEGF expression increases with tumor
angiogenesis, and a VEGF-A level of >16.7 pg/ml at 7 days
post-TACE may serve as an independent criteria for the diagnosis of
tumor growth, with a diagnostic sensitivity of 76% and specificity
of 66.7% (12), which may increase
the risk of HCC metastasis (35). The
present study revealed that preoperative and 5–7 days postoperative
CD151 expression levels were risk factors for HCC progression, and
it was identified that a preoperative CD151 level of >0.3247
ng/ml and a postoperative CD151 level of >0.3146 ng/ml were
sufficient to predict HCC progression with a sensitivity and
specificity of 66.7 and 80%, and 94.4 and 80%, respectively.
Furthermore, the AUC values were 0.753 and 0.761, respectively,
revealing that the detection of CD151 may be used to predict the
progression of HCC following TACE, with the diagnostic value of
pre- and post-TACE almost equivalent to each other. In the patients
with HCC exhibiting tumor progression, it was identified that CD151
expression levels at 5–7 days post-TACE were increased compared
with pre-TACE levels; tumor progression slowed following a decrease
in CD151 levels, and if CD151 fell below the pre-TACE level, the
patient was likely to remain free of tumor progression. If the
postoperative CD151 level decreased, the tumor was likely to
maintain the same status as assigned previously, indicating that
CD151 may serve an important role in the development of liver
cancer following TACE. The expression of CD151 in comparison to the
preoperative level may be used to predict tumor progression and
monitor the effectiveness of TACE treatment.
Embolism volume was identified as a protective
factor following a single TACE treatment and at the end of
follow-up, regardless of the treatment the patient received. This
finding indicates that intervention by physicians should maximize
the embolism volume, which may be beneficial to patients with HCC.
With an increase in the number of TACE treatments received, HCC
final progression decreased, indicating that TACE did not promote
invasion and metastasis of HCC.
The NLR is used as an indicator of the systemic
inflammatory response and associates with the prognosis of a number
of tumors. Patients with a normal NLR post-TACE experience an
increased survival time compared with those with an elevated NLR
(median survival time, 17.5 and 8 months respectively).
Furthermore, the 1-, 3- and 5-year survival rates of patients were
improved in those with a normal NLR post-TACE. Previous ROC curve
analysis demonstrated that when an NLR of 1.85 was used as the
threshold, the NLR pre-TACE predicted the outcome of TACE treatment
(20). The present study confirmed
this result, identifying that the NLR was one of the risk factors
for the final progression of HCC.
Increased platelets are associated with the
metastasis of a number of tumors. However, taking into account the
development of liver cirrhosis, which is a disease process
accompanied by a reduction in platelets, it is unclear whether the
platelet count pre-TACE has any association with the patient's
outcome. It has been demonstrated that patients with platelet
counts of <118,000/µl exhibit a lower metastatic rate, while a
platelet count of >212,000/µl is associated with tumor
metastasis (22). Furthermore, a
lower PLR (≤111.23) is likely to result in an improved survival
rate; the overall survival rate at 3 months was previously reported
at 57.6 (≤111.23) vs. 37.6% (≥111.23) (21). However, in the present study, no
association between the platelet count and PLR and the expression
of CD151 and tumor progression was identified, suggesting that
platelets serve a weak role in the progression of HCC.
All patients included in the current study presented
with large tumors (diameter between 8.5 and 13 cm) or recurrent
HCC, which is likely to result in a poor prognosis. However, the
patients were classified as Child-Pugh A and B, indicating
relatively good liver function. According to the Barcelona Clinic
Liver Cancer staging system (36),
TACE treatment was recommended. Intention analysis was applied in
the present study; patients who did not come to the hospital or who
were not re-examined were regarded as deceased. The results
indicated that with increasing time and TACE treatments, the
mortality rate increased; however, the 1-year survival rate was
~32%, indicating satisfactory results of the treatment.
The present study was limited by the small sample
size and differences between patients in disease characteristics.
Additionally, the majority of the hepatic masses were large and a
number of patients were lost to follow-up, which may have had a
negative influence on the results. Furthermore, numerous factors
may interact with one another during disease progression. It is
also hypothesized that serum stored for 1 month may exhibit
decreased expression of CD151, even if stored at −70°C. Measurement
error for ELISA may also exist in the experimental process.
To conclude, the present study identified that CD151
expression at 5–7 days post-TACE was increased compared with that
observed pre-TACE, that CD151 expression pre-TACE and at 5–7 days
post-TACE served as a risk factor for the progression of HCC, and
that the CD151 level may be used to predict the progression of HCC,
with optimal threshold values of >0.3247 ng/ml CD151 pre-TACE
and >0.3146 ng/ml at 5–7 days post-TACE. The risk factors for
HCC progression following a single TACE treatment included AFP,
pre-TACE CD151 and post-TACE CD151, while the embolism volume
served as a protective factor. The risk factors for final HCC
progression included HBsAg positivity, a NLR of >1.85 and final
TACE received, while the embolism volume served as a protective
factor. The present study also provides insight into how to reduce
the progression of HCC through inhibiting CD151. Whether this
approach may be used in the management of HCC is worthy of further
study.
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Song P, Tang W, Tamura S, Hasegawa K,
Sugawara Y, Dong J and Kokudo N: The management of hepatocellular
carcinoma in Asia: A guideline combining quantitative and
qualitative evaluation. Biosci Trends. 4:283–287. 2010.PubMed/NCBI
|
|
3
|
Lee KH, Sung KB, Lee DY, Park SJ, Kim KW
and Yu JS: Transcatheter arterial chemoembolization for
hepatocellular carcinoma: Anatomic and hemodynamic considerations
in the hepatic artery and portal vein. Radiographics. 22:1077–1091.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Llovet JM and Bruix J: Systematic review
of randomized trials for unresectable hepatocellular carcinoma:
Chemoembolization improves survival. Hepatology. 37:429–442. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Marelli L, Stigliano R, Triantos C,
Senzolo M, Cholongitas E, Davies N, Tibballs J, Meyer T, Patch DW
and Burroughs AK: Transarterial therapy for hepatocellular
carcinoma: Which technique is more effective? A systematic review
of cohort and randomized studies. Cardiovasc Interv Radiol.
30:6–25. 2007. View Article : Google Scholar
|
|
6
|
Murata S, Mine T, Ueda T, Nakazawa K,
Onozawa S, Yasui D and Kumita S: Transcatheter arterial
chemoembolization based on hepatic hemodynamics for hepatocellular
carcinoma. ScientificWorldJournal. 2013:4798052013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cheung TT, Poon RT, Jenkins CR, Chu FS,
Chok KS, Chan AC, Tsang SH, Dai WC, Yau TC, Chan SC, et al:
Survival analysis of high-intensity focused ultrasound therapy vs.
transarterial chemoembolization for unresectable hepatocellular
carcinomas. Liver Int. 34:e136–e143. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhong JH and Li LQ: Postoperative adjuvant
transarterial chemoembolization for participants with
hepatocellular carcinoma: A meta-analysis. Hepatol Res. 40:943–953.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gao ZH, Bai DS, Jiang GQ and Jin SJ:
Review of preoperative transarterial chemoembolization for
resectable hepatocellular carcinoma. World J Hepatol. 7:40–43.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lai EC, Lo CM, Fan ST, Liu CL and Wong J:
Postoperative adjuvant chemotherapy after curative resection of
hepatocellular carcinoma: A randomized controlled trial. Arch Surg.
133:183–188. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lin CI, Lin ZY, Hsieh MY, Huang CF, Chen
SH and Chuang WL: Potential risk factors for the reactivation of
the replication of hepatitis B and C viruses after transcatheter
arterial chemoembolization of hepatocellular carcinoma. Kaohsiung J
Med Sci. 27:554–559. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hsieh MY, Lin ZY and Chuang WL: Serial
serum VEGF-A, angiopoietin-2, and endostatin measurements in
cirrhotic patients with hepatocellular carcinoma treated by
transcatheter arterial chemoembolization. Kaohsiung J Med Sci.
27:314–322. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang Z, Zhou J, Fan J, Tan CJ, Qiu SJ, Yu
Y, Huang XW and Tang ZY: Sirolimus inhibits the growth and
metastatic progression of hepatocellular carcinoma. J Cancer Res
Clin Oncol. 135:715–722. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xiang ZL, Zeng ZC, Fan J, Tang ZY, Zeng HY
and Gao DM: Gene expression profiling of fixed tissues identified
hypoxia-inducible factor-1α, VEGF, and matrix metalloproteinase-2
as biomarkers of lymph node metastasis in hepatocellular carcinoma.
Clin Cancer Res. 17:5463–5472. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ke AW, Shi GM, Zhou J, Wu FZ, Ding ZB, Hu
MY, Xu Y, Song ZJ, Wang ZJ, Wu JC, et al: Role of overexpression of
CD151 and/or c-Met in predicting prognosis of hepatocellular
carcinoma. Hepatology. 49:491–503. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kwon MJ, Seo J, Kim YJ, Kwon MJ, Choi JY,
Kim TE, Lee DH, Park S, Shin YK, Han J and Choi YL: Prognostic
significance of CD151 overexpression in non-small cell lung cancer.
Lung Cancer. 81:109–116. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hashida H, Takabayashi A, Tokuhara T,
Hattori N, Taki T, Hasegawa H, Satoh S, Kobayashi N, Yamaoka Y and
Miyake M: Clinical significance of transmembrane 4 superfamily in
colon cancer. Br J Cancer. 89:158–167. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yang YM, Zhang ZW, Liu QM, Sun YF, Yu JR
and Xu WX: Overexpression of CD151 predicts prognosis in patients
with resected gastric cancer. PLoS One. 8:e589902013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Palmer TD, Martínez CH, Vasquez C, Hebron
KE, Jones-Paris C, Arnold SA, Chan SM, Chalasani V, Gomez-Lemus JA,
Williams AK, et al: Integrin-free tetraspanin CD151 can inhibit
tumor cell motility upon clustering and is a clinical indicator of
prostate cancer progression. Cancer Res. 74:173–187. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Xu X, Chen W, Zhang L, Miao R, Zhou Y, Wan
Y, Dong Y and Liu C: Prognostic significance of neutrophil to
lymphocyte ratio in patients with hepatocellular carcinoma after
transcatheter arterial chemoembolization. Chin Med J (Engl).
127:4204–4209. 2014.PubMed/NCBI
|
|
21
|
Li X, Chen ZH, Xing YF, Wang TT, Wu DH,
Wen JY, Chen J, Lin Q, Dong M, Wei L, et al: Platelet-to-lymphocyte
ratio acts as a prognostic factor for patients with advanced
hepatocellular carcinoma. Tumor Biol. 36:2263–2269. 2015.
View Article : Google Scholar
|
|
22
|
Lee CH, Lin YJ, Lin CC, Yen CL, Shen CH,
Chang CJ and Hsieh SY: Pretreatment platelet count early predicts
extrahepatic metastasis of human hepatoma. Liver Int. 35:2327–2336.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pugh RN, Murray-Lyon IM, Dawson JL,
Pietroni MC and Williams R: Transection of the oesophagus for
bleeding oesophageal varices. Br J Surg. 60:646–649. 1973.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shuster A, Huynh TJ, Rajan DK, Marquez MA,
Grant DR, Huynh DC and Jaskolka JD: Response evaluation criteria in
solid tumors (RECIST) criteria are superior to European Association
for Study of the Liver (EASL) criteria at 1 month follow-up for
predicting long-term survival in patients treated with
transarterial chemoembolization before liver transplantation for
hepatocellular cancer. J Vasc Interv Radiol. 24:805–812. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ashman LK, Aylett GW, Mehrabani PA,
Bendall LJ, Niutta S, Cambareri AC, Cole SR and Berndt MC: The
murine monoclonal antibody, 14A2.H1, identifies a novel platelet
surface antigen. Br J Haematol. 79:263–270. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hasegawa H, Watanabe H, Nomura T,
Utsunomiya Y, Yanagisawa K and Fujita S: Molecular cloning and
expression of mouse homologue of SFA-1/PETA-3 (CD151), a member of
the transmembrane 4 superfamily. Biochim Biophys Acta.
1353:125–130. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hasegawa H, Kishimoto K, Yanagisawa K,
Terasaki H, Shimadzu M and Fujita S: Assignment of SFA-1 (PETA-3),
a member of the transmembrane 4 superfamily, to human chromosome
11p15.5 by fluorescence in situ hybridization. Genomics.
40:193–196. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Nicole Johnson and Susan B Wormsley: Human
leukocyte differentiation antigens of the sixth international
workshop: What can we expect to see in the clinic? Clinical
Immunology Newsletter. 18:33–42. 1998. View Article : Google Scholar
|
|
29
|
Sincock PM, Mayrhofer G and Ashman LK:
Localization of the transmembrane 4 superfamily (TM4SF) member
PETA-3 (CD151) in normal human tissues: Comparison with CD9, CD63,
and alpha5beta1 integrin. J Histochem Cytochem. 45:515–525. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sadej R, Grudowska A, Turczyk L, Kordek R
and Romanska HM: CD151 in cancer progression and metastasis: A
complex scenario. Lab Invest. 94:41–51. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhu M, Guo J, Xia H, Li W, Lu Y, Dong X,
Chen Y, Xie X, Fu S and Li M: Alpha-fetoprotein activates AKT/mTOR
signaling to promote CXCR4 expression and migration of hepatoma
cells. Oncoscience. 2:59–70. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Shi GM, Ke AW, Zhou J, Wang XY, Xu Y, Ding
ZB, Devbhandari RP, Huang XY, Qiu SJ, Shi YH, et al: CD151
modulates expression of matrix metalloproteinase 9 and promotes
neoangiogenesis and progression of hepatocellular carcinoma.
Hepatology. 52:183–196. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Fei Y, Wang J, Liu W, Zuo H, Qin J, Wang
D, Zeng H and Liu Z: CD151 promotes cancer cell metastasis via
integrins α3β1 and α6β1 in vitro. Mol Med Rep. 6:1226–1230. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ke AW, Shi GM, Zhou J, Huang XY, Shi YH,
Ding ZB, Wang XY, Devbhandari RP and Fan J: CD151 amplifies
signaling by integrin α6β1 to PI3K and induces the
epithelial-mesenchymal transition in HCC cells. Gastroenterology.
140:1629–1641.e15. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Jia ZZ, Jiang GM and Feng YL: Serum
HIF-1alpha and VEGF levels pre- and post-TACE in patients with
primary liver cancer. Chin Med Sci J. 26:158–162. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Cillo U, Vitale A, Grigoletto F, Farinati
F, Brolese A, Zanus G, Neri D, Boccagni P, Srsen N, D'Amico F, et
al: Prospective validation of the Barcelona clinic liver cancer
staging system. J Hepatol. 44:723–731. 2006. View Article : Google Scholar : PubMed/NCBI
|