Introduction
Tumor angiogenesis, which provides oxygen and
nutrients to and removes metabolic waste from tumor cells, serves
an important function in tumor cell proliferation and metastasis
(1–3).
An understanding of tumor angiogenesis is advantageous for
evaluating the efficacy of tumor therapies, including radiation
therapy, chemotherapy and interventional therapy (4,5).
Therefore, angiogenesis is a major focus of tumor research.
Vascular endothelial growth factor (VEGF), which promotes a network
of signaling processes that induce endothelial cell growth,
migration and survival from preexisting vasculature and mediates
vessel permeability, is a key mediator of tumor angiogenesis. It is
also an anti-apoptotic factor for newly formed blood vessels and
functions as an inducer of the mobilization of endothelial
progenitor cells from bone marrow to distant sites (6,7).
Microvessel density (MVD) has been demonstrated to be correlated
with VEGF expression (8). As MVD
increases, tumor aggressiveness also increases (9,10).
Currently, MVD is considered the ‘gold standard’ for measuring
tumor angiogenesis (11).
It is important to measure angiogenesis
longitudinally due to its dynamic nature (12). However, MVD measurement requires an
invasive procedure, which, when coupled with specimen sampling
error, causes limitations for its study (5). Additionally, in clinical practice there
is a requisite to not only evaluate tumor angiogenesis, but also to
obtain information regarding tumor morphology (e.g., tumor size,
shape and the presence of necrosis) (13). For these reasons, a novel method for
simultaneously obtaining data on angiogenesis and tumor morphology
is required.
Due to recent developments in medical imaging,
magnetic resonance imaging (MRI) may have a unique advantage for
evaluating angiogenesis and tumor morphology. Dynamic
contrast-enhanced (DCE)-MRI and its volume transfer coefficient
(Ktrans) have been demonstrated to correlate with MVD,
and may quantitatively reflect tumor angiogenesis (5,14).
Furthermore, studies have demonstrated that diffusion-weighted
imaging (DWI) and the apparent diffusion coefficient (ADC) are
useful in evaluating cellularity and monitoring the tumor response
to therapy (15,16).
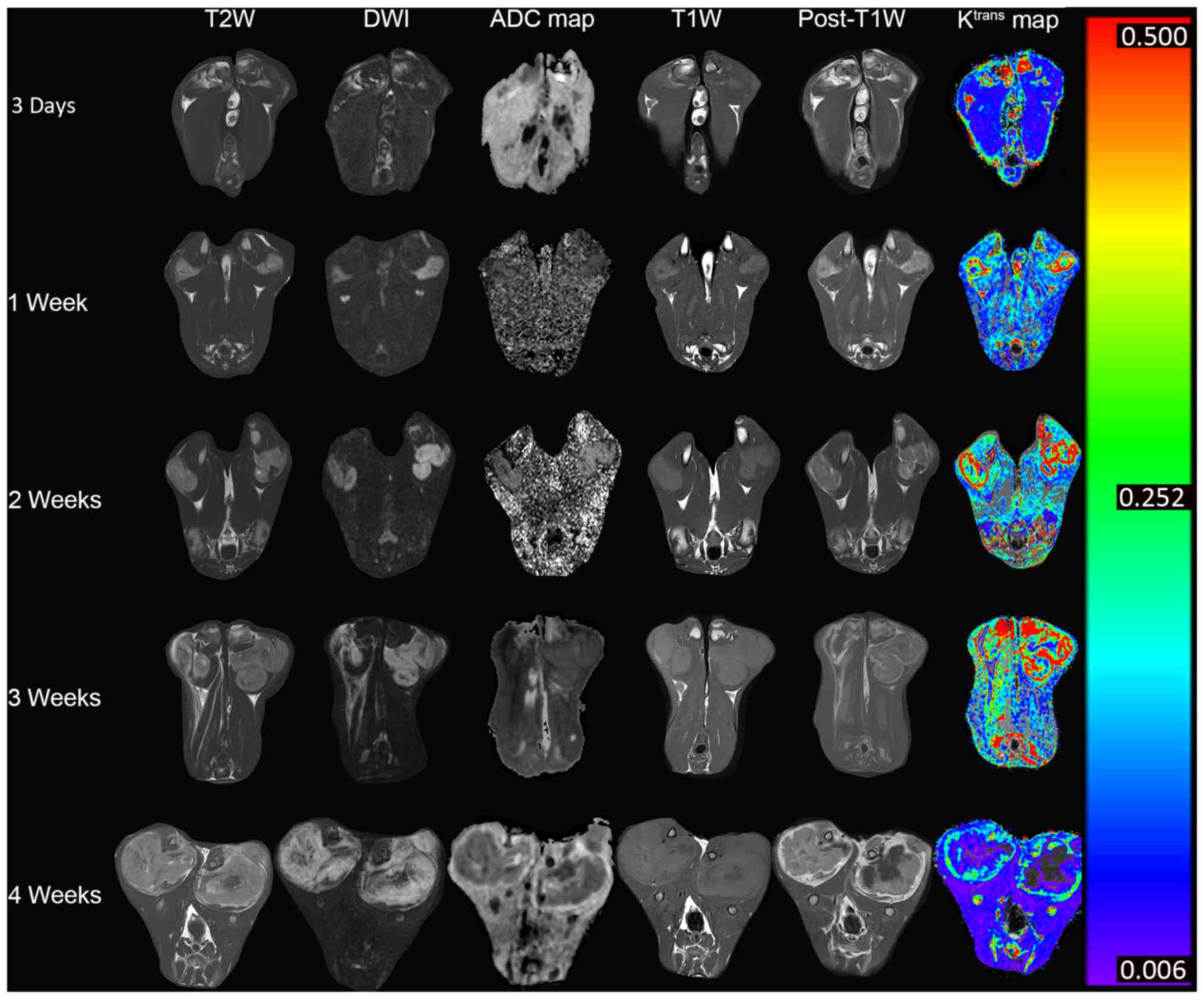
In the present study, DCE-MRI combined with DWI and
conventional MRI, including T1-weighted (T1W) and T2Wsequences,
were used to investigate rabbit VX2 tumor changes during the 4
weeks following tumor implantation. Specifically, changes in
angiogenesis, cellularity and necrosis were observed and
recorded.
Materials and methods
Animals
The current study was approved by the Animal
Research Committee of the Harbin Medical University Cancer Hospital
(Harbin, China), and conducted in accordance with the guidelines of
the International Council on Animal Care (17). A total of 15 male New Zealand white
rabbits (3–4 months old and weighing 2.5–3.5 kg, purchased from the
Laboratory Animal Centre of the Harbin Medical University), were
used in the present study. The rabbits were housed in individual
cages under controlled laboratory conditions (temperature, 22±1°C;
air humidity, 50–60%). Lights were on between 6:00 a.m. and 6:00
p.m., and animals had unrestricted access to food and water). The
implanted VX2 tumor was originally grown in the right hind limb of
two tumor-bearing rabbits. The tumors were removed from the muscles
of tumor-bearing rabbit and cut into 1–2 mm3 blocks,
which were placed in a small volume of normal saline, when the VX2
tumor grew to approximately 1–2 cm in diameter. Prior to tumor
implantation, each rabbit was anesthetized with 2.5% pentobarbital
sodium (1 ml/kg) via the auricular vein. Then the muscle tissue of
the bilateral proximal shins of the hind-legs were cut open with
the length of incision about 2.0 cm. Next, either two or three VX2
tissue blocks were implanted into the muscular tissue of each of
the bilateral proximal shins of the hind-legs. Finally, the muscle
and skin were sutured.
Study protocol
MRI was performed 3 days after tumor implantation to
confirm the successful establishment of rabbit VX2 models. MRI was
repeated at 1, 2, 3 and 4 weeks post-implantation. Following the
final MRI scan, all rabbits were euthanized for histological
analysis.
MRI
A clinical 3.0T MRI scanner (InteraAchieva; Philips
Medical Systems, Inc., Bothell, WA, USA) with an 8-channel head
coil was used. The MRI sequences included: i) T1W imaging:
repetition time (TR)/echo time (TE), 543/20 msec; number of single
averages (NSA), 6; slice thickness, 2 mm; field of view (FOV),
100×100 mm; and matrix, 224×270; ii) T2W imaging: TR/TE, 1,600/100
msec; NSA,6; slice thickness, 2 mm; FOV, 100×100 mm; and matrix,
200×192; iii) DWI: TR/TE, 1210/75 msec; NSA, 4; thickness, 3 mm;
FOV, 100×100 mm; and matrix, 92×90; iv) DCE-MRI; and v) post-T1W
imaging. DWI was performed using a single-shot echo planar
technique with 2b values (0, 800 sec/mm2) applied along
3 gradients, coinciding with 3 physical axes (x, y
and z). The 3D-THRIVE sequence (TR/TE=7.1/3.3 msec) with 2
and 15° flip angles (FAs) were used to generate a T1-map. Next, 30
THRIVE measurements with 15° FAs were used for DCE-MRI. Following
construction of the T1-map and a first baseline measurement, 0.1
mmol/kg Gd-DTPA (0.5 mol/l Magnevist; Bayer HealthCare
Pharmaceuticals, Guangzhou, Guangdong, China) was injected into the
auricular vein at a constant rate of 0.2 ml/kg/min with an
automated injector (Sino Angio, Shenzhen, China). The temporal
resolution of THRIVE was 13 sec.
Data processing
The DCE-MRI images were transferred to IDL-based
image permeability processing software (Cine Tool version 6.6.1; GE
Healthcare, Chicago, IL, USA). The femoral artery was selected as
the input artery. The permeability parameter Ktrans,
which represents the transport rate of the contrast agent from the
intravascular space into the extravascular extracellular space
(EES), was calculated based on the two-compartment modified Tofts
model, which assumes that the total concentration of contrast agent
in a tissue is equal to the concentrations in the two compartments,
namely the intravascular and the extravascular extracellular
spaces, and that no other compartments take up the contrast agent
(18). The DWI images were
transferred to a View Forum 5.1 workstation (Philips Medical
Systems) to generate ADC maps. Post-T1W images, and the
Ktrans and ADC maps, were then transferred to 3DMed
software (version 4.6; Medical Imaging Tool Kit, Beijing, China)
for image registration prior to determination of the regions of
interest (ROIs). ImageJ software (Version 1.47; National Institutes
of Health, Bethesda, MD, USA) was used to manually draw the ROIs.
Specifically, they were drawn along the parenchymal areas in the
largest tumor slice, avoiding areas of necrosis by referring to the
post-T1W images. Subsequently, the ROIs were copied and placed on
the Ktrans and ADC maps. Thigh muscle was used as a
reference. In addition, the tumor volume was calculated using the
following formula: [Area × slice number × (slice thickness +
inter-slice gap)] based on the post-T1W images. Tumor necrosis was
evaluated by using the necrosis degree (necrotic area/total area)
in the largest slice determined based on the T1W, T2WI and post-T1W
images.
Histological analysis
The MVD of the largest tumor slice was calculated
under microscopy by marking the tumor vessel with a CD31 monoclonal
antibody incubated for 1 h at room temperature (cat no., M082301;
1:50; Dako; Agilent Technologies, Inc., Santa Clara, CA, USA),
according to Weidner's technique (19). Following the final MRI scan, rabbits
were sacrificed by intravenous pentobarbital sodium overdose (100
mg/kg). Following fixation in 10% formaldehyde solution, the VX2
tumors located at the bilateral proximal shins and distal thighs of
the hind-legs were removed in their entirety from the rabbits,
embedded in paraffin and then sliced at 3 mm intervals in the axial
plane, corresponding to the plane of the MR images. The section
that corresponded to the largest slice of the tumor on the DCE-MRI
was prepared for microscopic examination by routine
immunohistochemical methods using the monoclonal mouse antibody
against CD31 (Dako; Agilent Technologies, Inc.). Microvessels were
counted as previously described (19). First, a low magnification (×40) was
used to identify the areas of highest vascular density (‘hot
spots’), and then 3 ‘hot spots’ were selected to count the number
of microvessels under a high magnification (×200). The average
value of these three counts represented the MVD for that case. A
microvessel was considered as a brown-stained endothelial cell or
an endothelial cell cluster with or without lumens which was
clearly separated from adjacent tissue. Branches appeared with
discrete breaks were also counted as single countable
microvessels.
Statistical analysis
SPSS software (version 16.0; SPSS, Inc., Chicago,
IL, USA) was used for statistical analysis, and P<0.05 was
considered to indicate a statistically significant difference.
Values are presented as the mean ± standard deviation (SD).
Differences between the tumor and muscle Ktrans levels
at 5 time points were calculated using the Mann-Whitney U test.
Serial changes in Ktrans and ADC across the five time
points were compared using the Friedman test, followed by post hoc
analysis with the Wilcoxon signed-rank tests with the Bonferroni
correction. Correlations between tumor Ktrans and MVD at
4 weeks, and between tumor Ktrans and ADC at all time
points, were calculated using the Spearman's correlation test. The
necrosis degree of tumor (necrotic area/total area) was analyzed
using the Friedman followed by post hoc analysis with Wilcoxon
signed-rank tests with the Bonferroni correction.
Results
A total of 30 VX2 tumors were present in the 15
experimental rabbits. The average tumor volume was 375.0±134.9 at 3
days, and then 1,561.4±498.9, 3,351.8±477.7, 8,943.0±1,936.9 and
1,8835.1±4,770.2 mm3at 1, 2, 3 and 4 weeks,
respectively. Tumor growth was rapid, and necrosis appeared by 1
week after tumor implantation. The necrosis degree of tumor was
gradually increased from the occurrence of necrosis with)in the
4-week time span of the present study (1 vs. 2 weeks, P=0.008; 2
vs. 3 weeks, P<0.001; 3 vs. 4 weeks, P<0.001) (Table I).
 | Table I.Tumor volume and necrosis at
different time points. |
Table I.
Tumor volume and necrosis at
different time points.
|
|
|
|
|
|
| P-value |
|---|
| Categories | 3 days | 1 week | 2 weeks | 3 weeks | 4 weeks | p1 | p2 | p3 | p4 |
|---|
| Tumor volume
(mm3) | 375.0±134.9 | 1,561.4±498.9 | 3,351.8±477.7 |
8,943.0±1,936.9 |
18,835.1±4,770.2 | – | – | – | – |
| Necrosis |
|
|
|
|
|
|
|
|
|
| Number
(n) | 0 | 2 | 9 | 27 | 29 |
|
|
|
|
| Degree
(necrosis area/total area, %) | 0 | 6 | 21 | 31.9 | 57.8 | 0.18 | 0.008 | <0.001 | <0.001 |
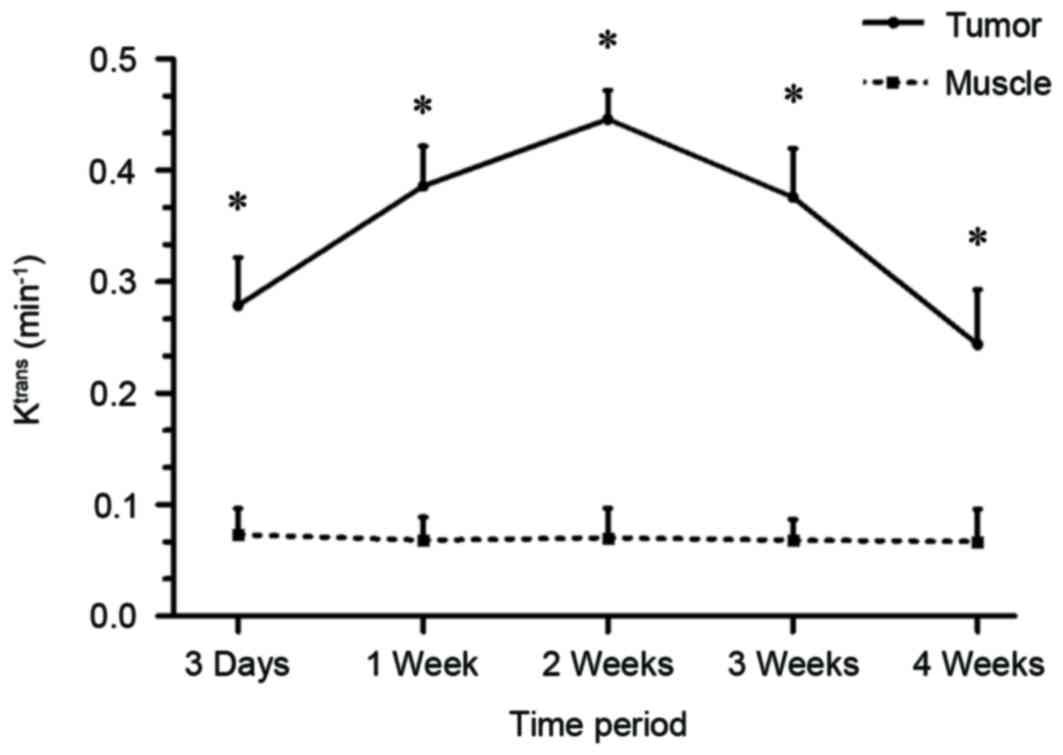
Ktrans measurements
No difference in the Ktrans levels of the
thigh muscles was identified amongst the 5 time points (P=0.430;
Fig. 1), which indicated that the
Ktrans measurement was reliable in this study.
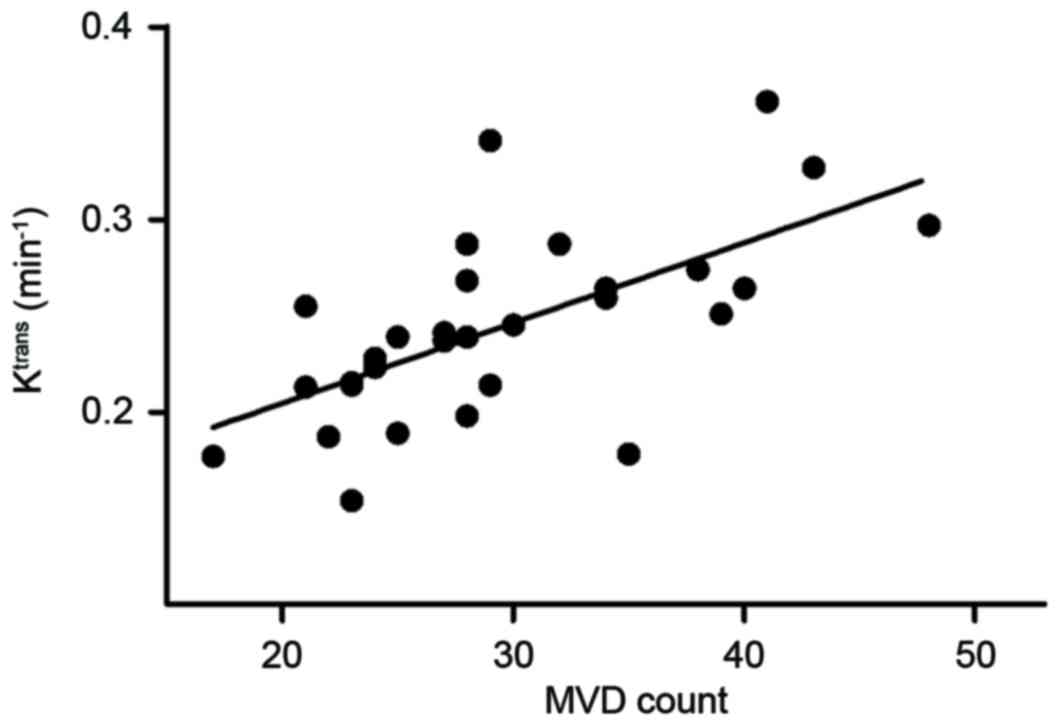
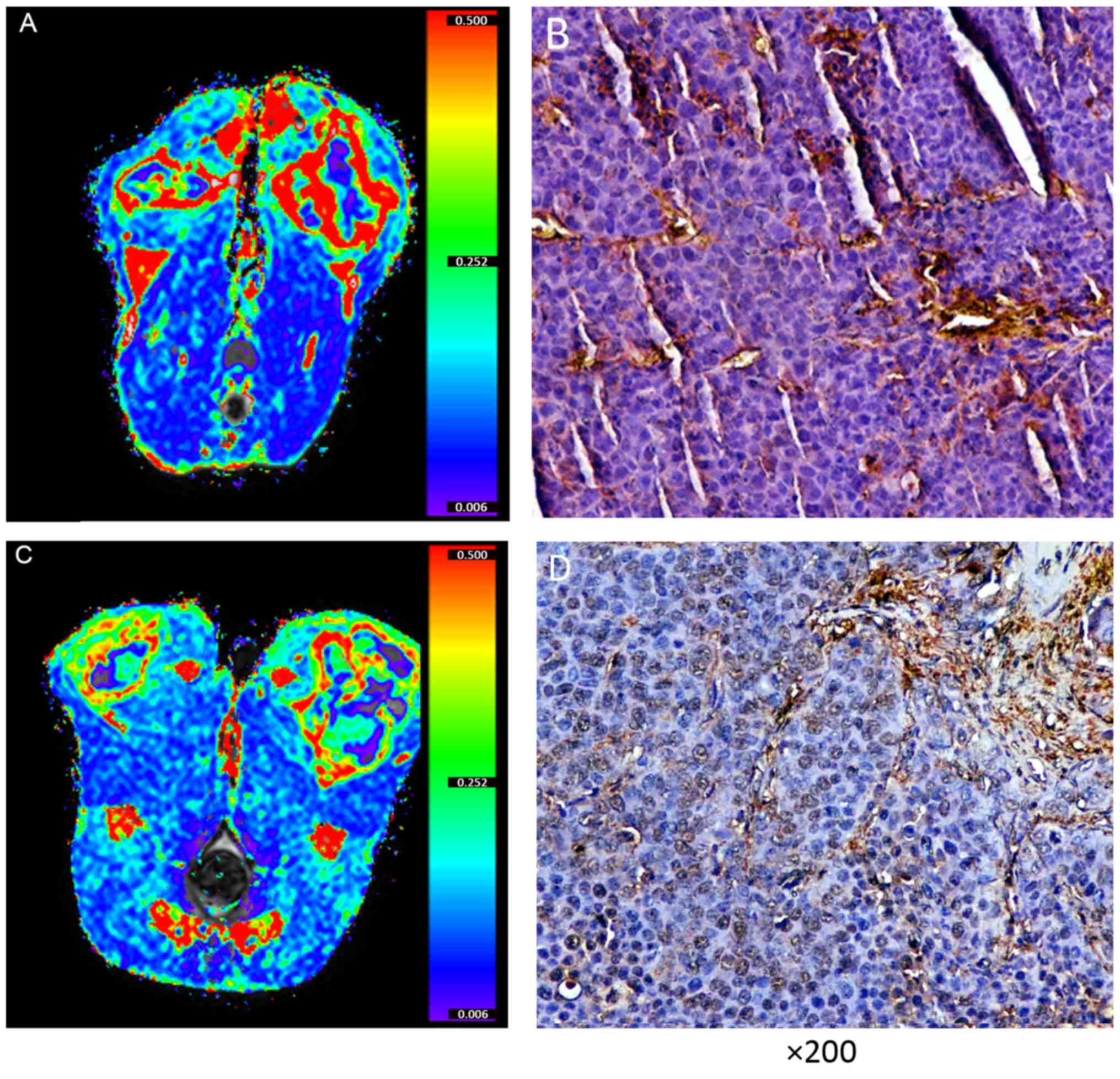
Furthermore, the present study compared the tumor Ktrans
with MVD at 4 weeks and identified a positive correlation (r=0.674,
P<0.001; Figs. 2 and 3). This assisted in the confirmation that
Ktrans reflected MVD. Tumor Ktrans was higher
than muscle Ktrans at each time point (P<0.001 for
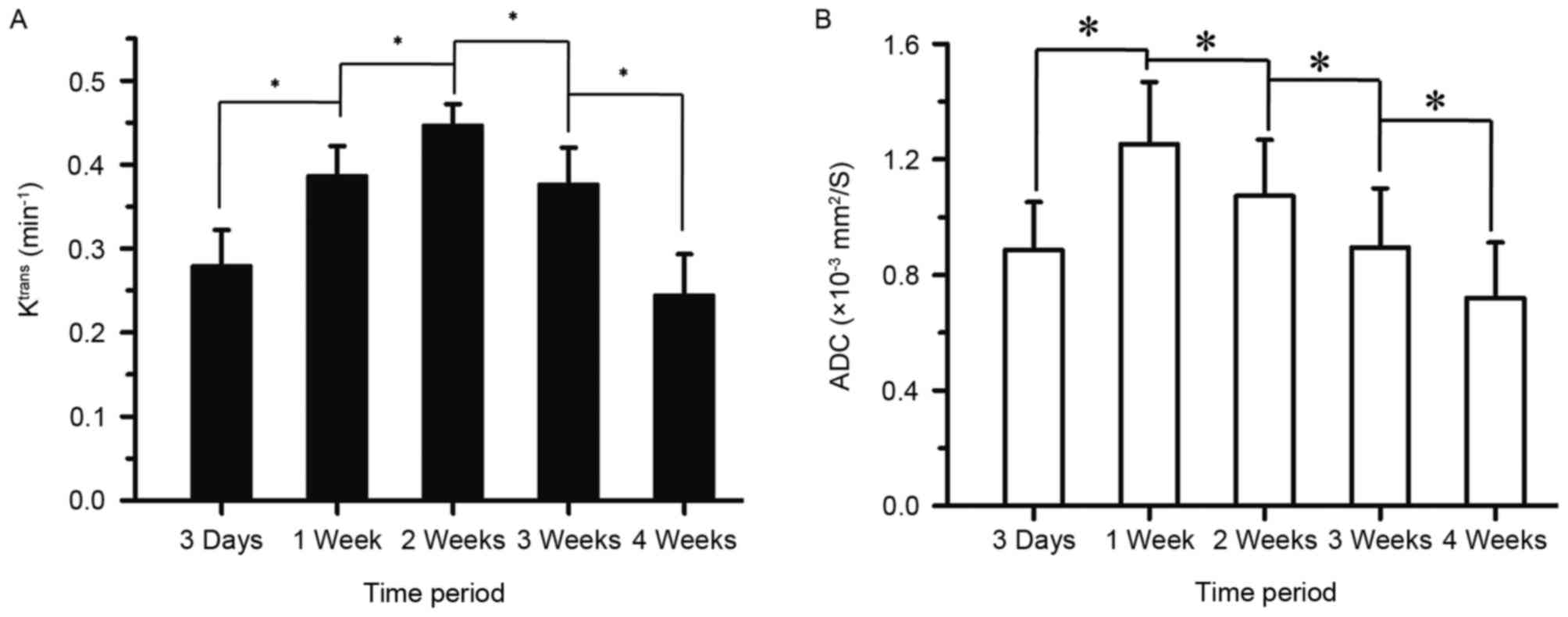
all). Furthermore, tumor Ktrans values were
significantly different between all adjacent time points
(P<0.001 for all). Specifically, tumor Ktrans values
at 1 week were higher than those at 3 days, and those at 2 weeks
were higher than at 1 week; tumor Ktrans values at 3
weeks were lower than at 2 weeks, and those at 4 weeks were lower
than at 3 weeks. Thus, the results demonstrate that, following
tumor implantation, the tumor Ktrans level rose for 2
weeks and then began to decline, reaching its lowest point at 4
weeks (Figs. 1, 4A and 5).
ADC measurements
The ADC values also differed between all adjacent
time points (P<0.001 for all). Specifically, the ADC values at 1
week were higher than at 3 days, but then declined consistently for
up to 4 weeks. Cellularity was observed to reach its highest level
1 week following tumor implantation (Figs. 4B and 5).
Correlations between Ktrans
and ADC
No correlation was revealed between the tumor
Ktrans and the ADC at any time point.
Discussion
In the present study, DCE-MRI and DWI, combined with
conventional MRI, were used to monitor the VX2 tumor for a 4-week
period following tumor implantation. The results suggest that the
Ktrans value quantitatively reflects tumor angiogenesis.
Furthermore, angiogenesis of VX2 tumors was discovered to be a
dynamic process that increased for 2 weeks following tumor
implantation and began to decline thereafter. Changes in the tumor
parenchyma were also identified, namely cellularity, and the extent
of necrosis.
Previous studies have suggested that DCE-MRI
reflects MVD and angiogenesis (5,14). VX2 MVD
at 4 weeks was used as a reference and Ktrans was
positively correlated with MVD, indirectly reflecting tumor
angiogenesis. It has been demonstrated that the neovasculature of
malignant tumors lacks normal architecture, differing
morphologically and hemodynamically from the vascular networks in
normal tissues (10). These new,
immature vessels have a high permeability (20). In the current study, the modified
Tofts model was used to calculate Ktrans. This model
assumes that the total amount of contrast agent in a tissue is
determined by its concentration in the extravascular and
intravascular extracellular spaces combined. Ktrans
represents the influx rate of contrast agent from the intravascular
space to the extravascular extracellular space (18). Leakage of contrast agent into the
extravascular extracellular space will increase with expansion of
tumor angiogenesis. Therefore, Ktrans may reflect VX2
tumor angiogenesis.
Understanding tumor angiogenesis and its dynamic
process are of great value in the treatment of tumors. Although
there have been numerous studies on angiogenesis in VX2 tumors
(21,22), the dynamic process of angiogenesis in
VX2 tumors in the same animal, and the distinctive association
between the dynamic processes of angiogenesis and of tumor growth
require clarification. The present study demonstrated that VX2
tumor angiogenesis is a dynamic process, in that it increased for
the initial 2 weeks after tumor implantation and then began to
decline. Anti-angiogenic therapy has demonstrated efficacy
(23) and thus, having an
understanding of this dynamic process is useful.
Previous research has suggested that tumor growth
requires neovasculature when the tumor diameter is >2 mm
(24). In the current study, the
Ktrans of the tumor parenchyma was higher than that of
the muscle 3 days after tumor implantation, at which time tumor
angiogenesis was evident. Tumor angiogenesis continued to rise
until it peaked at 2 weeks. However, ADC values were higher at 1
week compared with at 3 days. It is recognized that the ADC value
results from a combination of true molecular diffusion and
microcirculatory perfusion (25,26). Early
on in tumor angiogenesis, the increase in ADC induced by
microcirculatory perfusion may have been larger than the decrease
in ADC from tumor cell propagation and proliferation. If so, it
would provide an explanation as to why ADC values were higher at 1
week than at 3 days. Over time, tumor density and cellularity
increased significantly, such that the ADC value began to decrease
after 1 week.
The Ktrans values of tumor tissues in the
present study were higher than those of muscle tissues for each
time point, indicating that tumor angiogenesis occurred throughout
the entire study period. Although no correlation between
Ktrans and ADC values were identified for any time
point, the ADC began to decrease after 1 week and continued to
decline until 4 weeks. This demonstrates that tumor density and
cellularity continued to rise, and suggests that tumor growth was
accompanied by tumor angiogenesis throughout the study period.
Absence of a correlation may be due to the small sample size, as
well as a lack of synchronization between tumor angiogenesis and
tumor cell propagation and proliferation.
Although the Ktrans of the tumor
parenchyma was higher than that of the muscle during the 4-week
study time span, it began to decline at 2 weeks, reaching a minimum
at 4 weeks, suggesting that tumor angiogenesis began to decrease at
2 weeks. Tumor necrosis was identified at 1 week, and the necrosis
degree gradually increased with tumor development. Tumor necrosis
is often associated with rapid growth and insufficient blood supply
(27). Therefore, the increase in
tumor angiogenesis after 2 weeks may be a reason for the higher
rate and extent of necrosis. This also confirms the importance of
tumor angiogenesis in tumor growth.
There are certain limitations to the present study.
First, the present study did not analyze the correlation between
Ktrans and tumor size. Tumor size may be influenced by
necrosis, which in turn, may induce bias in the evaluation of tumor
angiogenesis and therefore, the association between
Ktrans and tumor size was not analyzed. Additionally, it
is considered that the physiological indicators of the VX2 tumor
are stable at 2 weeks following implantation. However, the
Ktrans and ADC continued to change 2 weeks after
implantation in the current study. A previous study reported that
certain diffusion MRI parameters (including ADC) may continue to
change within the first month of tumor implantation (28). Therefore, the Ktrans and
ADC changes reflect the tumor angiogenesis and tumor celluarity,
which may be the result of tumor physiological indicators and thus,
may occur later than the changes in physiological indicators.
Finally, the present study did not use other DCE-MRI parameters
(e.g., Kep and Ve) to evaluate tumor angiogenesis. Kep (reverse
reflux rate constant) is the reflux of the contrast agent from the
EES to the intravascular space. Ve (volume fraction of EES) is the
indirect measurement of the cellular density of the tissue
(29). However, for Kep and Ve, there
are some inconsistent results in evaluating tumor angiogenesis in
different studies (5,30,31).
Ktrans, which represents the transport rate of the
contrast agent from the intravascular space into the EES, may
reflect tumor neovasculature more accurately and be used more
widely (5,32).
In conclusion, DCE-MRI and Ktrans, its
quantitative coefficient, may reflect tumor parenchymal MVD and be
helpful in evaluating angiogenesis. Thus, they may be useful tools
for tumor management. Furthermore, tumor angiogenesis following VX2
implantation was identified to be a dynamic process, which
continued to increase until reaching a peak at 2 weeks following
tumor implantation, and then began to decrease; this process also
appears to serve a function in tumor growth.
Acknowledgements
The present study was supported the National Natural
Science Foundation of China (grant no. 81671771) and the grant of
Harbin Science and Technology Bureau (grant no. 2016RAXYJ066).
References
|
1
|
Folkman J: Role of angiogenesis in tumor
growth and metastasis. Semin Oncol. 29(6 Suppl 16): S15–S18. 2002.
View Article : Google Scholar
|
|
2
|
Iagaru A and Gambhir SS: Imaging tumor
angiogenesis: The road to clinical utility. AJR Am J Roentgenol.
201:W183–W191. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nomura T, Hirata K, Shimaoka T, Yamakawa
M, Koizumi N, Suzuki R, Maruyama K and Utoguchi N: Cancer vaccine
therapy using tumor endothelial cells as antigens suppresses solid
tumor growth and metastasis. Biol Pharm Bull. 40:1661–1668. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gerstner ER, Emblem KE and Sorensen GA:
Vascular magnetic resonance imaging in brain tumors during
antiangiogenic therapy-are we there yet? Cancer J. 21:337–342.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen J, Qian T, Zhang H, Wei C, Meng F and
Yin H: Combining dynamic contrast enhanced magnetic resonance
imaging and microvessel density to assess the angiogenesis after
PEI in a rabbit VX2 liver tumor model. Magn Reson Imaging.
34:177–182. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pinto MP, Owen GI, Retamal I and Garrido
M: Angiogenesis inhibitors in early development for gastric cancer.
Expert Opin Investig Drugs. 26:1007–1017. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Peng FW, Liu DK, Zhang QW, Xu YG and Shi
L: VEGFR-2 inhibitors and the therapeutic applications thereof: A
patent review (2012–2016). Expert Opin Ther Pat. 27:987–1004. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen HF and Wu KJ: Endothelial Trans
differentiation of tumor cells triggered by the Twist1-Jagged1-KLF4
Axis: Relationship between Cancer Stemness and Angiogenesis. Stem
Cells Int. 2016:64398642016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bremnes RM, Camps C and Sirera R:
Angiogenesis in non-small cell lung cancer: The prognostic impact
of neoangiogenesis and the cytokines VEGF and bFGF in tumours and
blood. Lung Cancer. 51:143–158. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mischi M, Turco S, Lavini C, Kompatsiari
K, de la Rosette JJ, Breeuwer M and Wijkstra H: Magnetic resonance
dispersion imaging for localization of angiogenesis and cancer
growth. Invest Radiol. 49:561–569. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jia WR, Chai WM, Tang L, Wang Y, Fei XC,
Han BS and Chen M: Three-dimensional contrast enhanced ultrasound
score and dynamic contrast-enhanced magnetic resonance imaging
score in evaluating breast tumor angiogenesis: Correlation with
biological factors. Eur J Radiol. 83:1098–1105. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
McCarville MB, Coleman JL, Guo J, Li Y, Li
X, Honnoll PJ, Davidoff AM and Navid F: Use of quantitative dynamic
Contrast-Enhanced ultrasound to assess response to antiangiogenic
therapy in children and adolescents with solid malignancies: A
pilot study. AJR Am J Roentgenol. 206:933–939. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nedelcu RI, Zurac SA, Brînzea A, Cioplea
MD, Turcu G, Popescu R, Popescu CM and Ion DA: Morphological
features of melanocytic tumors with depigmented halo: Review of the
literature and personal results. Rom J Morphol Embryol. 56(2
Suppl): S659–S663. 2015.
|
|
14
|
Arteaga-Marrero N, Rygh CB, Mainou-Gomez
JF, Nylund K, Roehrich D, Heggdal J, Matulaniec P, Gilja OH, Reed
RK, Svensson L, et al: Multimodal approach to assess tumour
vasculature and potential treatment effect with DCE-US and DCE-MRI
quantification in CWR22 prostate tumour xenografts. Contrast Media
Mol Imaging. 10:428–437. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Razek AA, Megahed AS, Denewer A, Motamed
A, Tawfik A and Nada N: Role of diffusion-weighted magnetic
resonance imaging in differentiation between the viable and
necrotic parts of head and neck tumors. Acta Radiol. 49:364–370.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ludwig JM, Camacho JC, Kokabi N, Xing M
and Kim HS: The role of Diffusion-weighted imaging (DWI) in
Locoregional therapy outcome prediction and response assessment for
hepatocellular carcinoma (HCC): The New Era of Functional imaging
biomarkers. Diagnostics (Basel). 5:546–563. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
International Council for Laboratory
Animal Science (ICLAS), . http://www.iclas.orgJuly 13–2012
|
|
18
|
Tofts PS, Brix G, Buckley DL, Evelhoch JL,
Henderson E, Knopp MV, Larsson HB, Lee TY, Mayr NA, Parker GJ, et
al: Estimating kinetic parameters from dynamic contrast-enhanced
T(1)-weighted MRI of a diffusable tracer: Standardized quantities
and symbols. J Magn Reson Imaging. 10:223–232. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Weidner N: Current pathologic methods for
measuring intratumoral microvessel density within breast carcinoma
and other solid tumors. Breast Cancer Res Treat. 36:169–180. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hida K, Hida Y and Shindoh M:
Understanding tumor endothelial cell abnormalities to develop ideal
anti-angiogenic therapies. Cancer Sci. 99:459–466. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lijowski M, Caruthers S, Hu G, Zhang H,
Scott MJ, Williams T, Erpelding T, Schmieder AH, Kiefer G, Gulyas
G, et al: High sensitivity: High-resolution SPECT-CT/MR molecular
imaging of angiogenesis in the Vx2 model. Invest Radiol. 44:15–22.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Feng G, Lei Z, Wang D, Xu N, Wei Q, Li D
and Liu J: The evaluation of anti-angiogenic effects of Endostar on
rabbit VX2 portal vein tumor thrombus using perfusion MSCT. Cancer
Imaging. 14:172014.PubMed/NCBI
|
|
23
|
Manzo A, Montanino A, Carillio G, Costanzo
R, Sandomenico C, Normanno N, Piccirillo MC, Daniele G, Perrone F,
Rocco G and Morabito A: Angiogenesis Inhibitors in NSCLC. Int J Mol
Sci. 18:pii: E20212017. View Article : Google Scholar
|
|
24
|
Folkman J: What is the evidence that
tumors are angiogenesis dependent. J Natl Cancer Inst. 82:4–6.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Thoeny HC, De Keyzer F, Vandecaveye V,
Chen F, Sun X, Bosmans H, Hermans R, Verbeken EK, Boesch C, Marchal
G, et al: Effect of vascular targeting agent in rat tumor model:
Dynamic contrast-enhanced versus diffusion-weighted MR imaging.
Radiology. 237:492–499. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Panagiotaki E, Walker-Samuel S, Siow B,
Johnson SP, Rajkumar V, Pedley RB, Lythgoe MF and Alexander DC:
Noninvasive quantification of solid tumor microstructure using
VERDICT MRI. Cancer Res. 74:1902–1912. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen FH, Wang CC, Liu HL, Fu SY, Yu CF,
Chang C, Chiang CS and Hong JH: Decline of tumor vascular function
as assessed by dynamic Contrast-Enhanced magnetic resonance imaging
is associated with poor responses to radiation therapy and
chemotherapy. Int J Radiat Oncol Biol Phys. 95:1495–1503. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wu H, Liu H, Liang C, Zhang S, Liu Z, Liu
C, Liu Y, Hu M, Li C and Mei Y: Diffusion-weighted multiparametric
MRI for monitoring longitudinal changes of parameters in rabbit VX2
liver tumors. J Magn Reson Imaging. 44:707–714. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen BB and Shih TT: DCE-MRI in
hepatocellular carcinoma-clinical and therapeutic image biomarker.
World J Gastroenterol. 20:3125–3134. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kim SH, Lee HS, Kang BJ, Song BJ, Kim HB,
Lee H, Jin MS and Lee A: Dynamic Contrast-Enhanced MRI perfusion
parameters as imaging biomarkers of angiogenesis. PLoS One.
11:e01686322016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kim YE, Lim JS, Choi J, Kim D, Myoung S,
Kim MJ and Kim KW: Perfusion parameters of dynamic
Contrast-enhanced magnetic resonance imaging in patients with
rectal cancer: Correlation with microvascular density and vascular
endothelial growth factor expression. Korean J Radiol. 14:878–885.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhang W, Chen HJ, Wang ZJ, Huang W and
Zhang LJ: Dynamic contrast enhanced MR imaging for evaluation of
angiogenesis of hepatocellular nodules in liver cirrhosis in
N-nitrosodiethylamine induced rat model. Eur Radiol. 27:2086–2094.
2017. View Article : Google Scholar : PubMed/NCBI
|