Introduction
Patients with loco-regionally advanced head and neck
squamous cell carcinoma (HNSCC) are usually treated with surgery
and postoperative adjuvant radiotherapy. However, the prognosis for
loco-regionally advanced HNSCC patients remains poor. To improve
loco-regional control and survival, various chemotherapy drugs that
have shown antitumor activity in HNSCC as single agents have also
been tested in combination (1–6).
Docetaxel, an analog of taxane, is an inhibitor of microtubule
depolymerisation that causes cell cycle arrest at the G2/M
transition. As a single agent, docetaxel shows significant
antitumor activity in HNSCC when used as a neoadjuvant therapy. It
also exhibits a potent radiosensitizing effect (7), and has therefore been used as induction
chemotherapy or concomitantly with radiotherapy.
In order to reduce the general toxicities associated
with this treatment, weekly docetaxel and concomitant radiotherapy
were tried as an alternative (8,9). Even
low-dose docetaxel showed a strong antitumor effect in combination
with radiation, with a high survival rate amongst patients who
showed a complete response (8,10),
although there were grade 3 or 4 adverse events consisting of
stomatitis, dermatitis, and anorexia.
Thioredoxin (TRX), a small redox-active
multifunctional protein, acts as a potent antioxidant and redox
regulator in signal transduction (11). TRX expression is elevated in various
types of cancer (12–14), and its over expression is associated
with a poor prognosis (15,16). TRX is negatively regulated by
thioredoxin interacting protein (TXNIP) (17), and reduced levels of active TRX lead
to an accumulation of reactive oxygen species (18). TXNIP mediates the inhibition of cell
proliferation and the induction of apoptosis through activation of
apoptosis signal regulating kinase 1 (17). TXNIP has also been reported to act as
a transcriptional repressor (19).
These findings suggest that TXNIP could be a tumor suppressor gene,
and furthermore, that the regulation of the redox state might be an
important strategy in cancer treatment.
D-allose is a rare sugar that is found at only very
low levels in nature. A number of studies have recently
characterized the biological functions of D-allose, and we recently
showed that it induces TXNIP expression and suppresses the growth
of several types of cancer cells (20,21) by
increasing the level of intracellular reactive oxygen species (ROS)
and radiation induced apoptosis (22).
In this study, we investigated the effect of
D-allose on normal human fibroblasts in order to establish its
safety. The combined effect of D-allose and low-dose docetaxel plus
radiation was also investigated using a mouse model of human head
and neck cancer.
Materials and methods
Cell culture
The human head and neck carcinoma cell line HSC3
(tongue carcinoma) was obtained from the Health Science Research
Resources Bank, Osaka, Japan. HSC3 cells were cultured in Eagle's
minimal essential medium (EMEM). Medium contained 10%
heat-inactivated fetal bovine calf serum and 1%
penicillin-streptomycin. The human fibroblast cell line TIG-1 was
kindly supplied by the Laboratory of Physiological Chemistry,
Faculty of Pharmaceutical Sciences at Kagawa, Tokushima Bunri
University, Sanuki, Japan. TIG-1 cells were cultured in DMEM with
10% FBS. Cells were incubated in a humidified 5% CO2
atmosphere at 37°C.
Determination of TIG-1 cell
survival
D-allose was supplied by the Department of
Biochemistry and Food Science, Faculty of Agriculture, Kagawa
University, Kagawa, Japan. Docetaxel was obtained from Sanofi S.A.
(Paris, France) and stored in frozen aliquots. Before use, it was
thawed and diluted to the desired concentrations in the cell
culture medium or normal saline. The growth inhibitory effect of
D-allose was compared with that of D-glucose or medium only. TIG-1
cells were seeded in 96-well plates at 1.0×103 cells/100
µl and cultured for 24 h. The medium was then removed, and fresh
medium containing D-allose or D-glucose was added. The cells that
were seeded in 5 separate wells in each group were incubated for an
additional 24–72 h. To investigate the effects of radiation, cells
were treated with 25 mM D-allose or D-glucose 6 h before
irradiation with X-rays (0, 4, 8 Gy), and then incubated for a
further 72 h. The cells were irradiated with a dose of 0.59 Gy/min
using an X-ray irradiator (HITEX type HW 260, 200 kV, mA, Osaka,
Japan). The net number of viable cells was then determined using a
Cell Counting Kit-8 (CCK-8; Dojindo Laboratories, Kumamoto, Japan)
according to the manufacturer's instructions. The absorbance was
measured by a microplate reader at 450 nm after 2 h incubation.
Values are the mean of 3 independent experiments.
Measurement of apoptosis
A terminal deoxynucleotidyl transferase d-UTP
nick-end labelling (TUNEL) assay was performed using the Apoptosis
Detection System Fluorescein kit (Promega Corporation, Madison, WI,
USA). Briefly, treated TIG-1 cells were spread on a poly-L-lysine
slide (Sigma-Aldrich; Merck KGaA, Darmstadt, Germany), fixed with
4% paraformaldehyde, and permeabilized with 0.2% Triton X-100.
Cells were incubated in 50 µl of TdT incubation buffer (nucleotide
mix [fluorescein-12-dUTP] and TdT enzyme prepared according to the
manufacturer's protocol) for 60 min at 37°C in a humidified
chamber. The reaction was terminated by washing the cells in 2X
saline sodium citrate buffer followed by 2 washes in PBS. Cells
were counterstained with 1 µg/ml propidium iodide and then washed
in distilled water. Staining was observed under a fluorescence
microscope. Green fluorescence indicated DNA fragmentation due to
fluorescein-12-dUTP labeling.
Analysis of mRNA expression
To investigate the effects of D-allose on the
expression of TXNIP and TRX, cells were cultured in 6
cm dishes with 25 mM D-allose for 24 h. To investigate the effects
of radiation on the expression of TXNIP and TRX,
D-allose treated or untreated cells were incubated at 37°C for 6 h,
and then exposed to a single 8 Gy X-ray dose. The cells were then
incubated for a further 24 h. Quantitative polymerase chain
reaction (qPCR) was carried out using TaqMan gene expression assay
primers and the ABI7700 Real-Time PCR system. Each reaction was
performed in duplicate. The GAPDH gene was used to normalize
expression across assays and runs, and a quantification value (Cq)
for each sample was used to determine the expression level of the
gene.
In vivo xenograft experiment
HSC3 cells were used in a xenograft model with
female athymic nude mice (BALB/c nu/nu, 5–6 weeks old). A
suspension of 1×106 cells in 0.1 ml EMEM was injected
subcutaneously into both sides of the posterior flank using a 1-cc
syringe with a 27G needle. Tumors were grown for 10 days until
attaining an average size of 100 mm3 (day 0). A total of
42 nude mice were assigned to 7 treatment groups (including the
control group), each consisting of 6 mice. The control group mice
were injected with 0.1 ml normal saline at the same time points
(group 1). For the two different D-allose treatment groups, 0.1 ml
of 25 mM D-allose was injected into the tumor region once a week
(group 2) or 5 times a week (group 3). For the low-dose weekly
docetaxel and radiation treatment group which is established as
clinical model, 3 mg/kg docetaxel (20% of the maximum tolerable
dose) was injected intraperitoneally, and the mice were also
irradiated on days 1 and 4 (Group 4). For the combined D-allose and
radiation treatment, D-allose (with the same dosing regimen as
Group 3) plus radiation with a 4 Gy dose on days 1 and 4 (Group 5).
The docetaxel, radiation, and D-allose group was treated with the
same regimen (group 5) and 0.1 ml of 25 mM D-allose was injected
into tumor tissue on day 1 (group 6) or 5 times a week (group 7).
These treatments were repeated for 3 weeks. This study was approved
by the Animal Care and Use Committees of Kagawa University.
Immunohistochemical staining
For the histological studies, one mouse in each
treatment group was euthanized 3 weeks after the initiation of
treatment. The posterior flank skin specimens were fixed in
phosphate-buffered paraformaldehyde (4%), embedded in paraffin, and
cut into 4 µm thick sections. The immunohistochemistry was
performed using the Vectastain ABC rabbit IgG kit (Vector
Laboratories, Inc., Burlingame, CA, USA) following the
manufacturer's instructions. The following primary antibodies were
used: anti-tumor necrosis factor (TNF)-α (NBP1-19532) polyclonal
(Novus Biologicals, LLC, Littleton, CO, USA), anti-TXNIP rabbit
polyclonal (Sigma-Aldrich; Merck KGaA), and anti-TRX (C63C6) rabbit
monoclonal (Cell Signaling Technology, Inc., Danvers, MA, USA).
Intensity of staining were divided into four
groups-no staining, weak staining, moderate staining and strong
staining. One pathologist evaluated all pathological sections
without the information of experimental design.
Western blot analysis
Protein was extracted from untreated normal skin,
normal skin treated with 25 mM D-allose for 2 weeks, untreated
tumor tissue, and tumor tissue treated with 25 mM D-allose for 2 or
3 weeks. For the Western blot analyses, proteins were separated on
10% SDS-PAGE gels, transferred to nitrocellulose membranes, blocked
with 5% (w/v) non-fat dried milk in PBS, and incubated with
anti-TXNIP (MBL, Nagoya, Japan), anti-TRX (MBL), and anti-GAPDH
(14c10) antibodies (Cell Signaling Technology, Inc., Tokyo, Japan).
Membranes were probed with a horseradish peroxidase-conjugated
anti-mouse IgG (Amersham, Tokyo, Japan), and signals were detected
using an enhanced chemiluminescence system (Amersham).
Statistical analysis
Comparisons between groups for cell growth assay and
mRNA expressions were compared using the Kruskal-Wallis test.
Post-hoc test was carried out using the Tukey's test. Pretreatment
mRNA expressions between TIG cell and HSC3 cell were compared using
the Student's t-test. Significant difference between in vivo
experimental groups was estimated using the Kruskal-Wallis test.
Post-hoc test was carried out using the Mann-Whitney U test with
Bonferrioni's correction. P<0.05 was considered to indicate a
statistically significant difference.
Results
Effect of D-allose on the
proliferation of TIG-1 cells
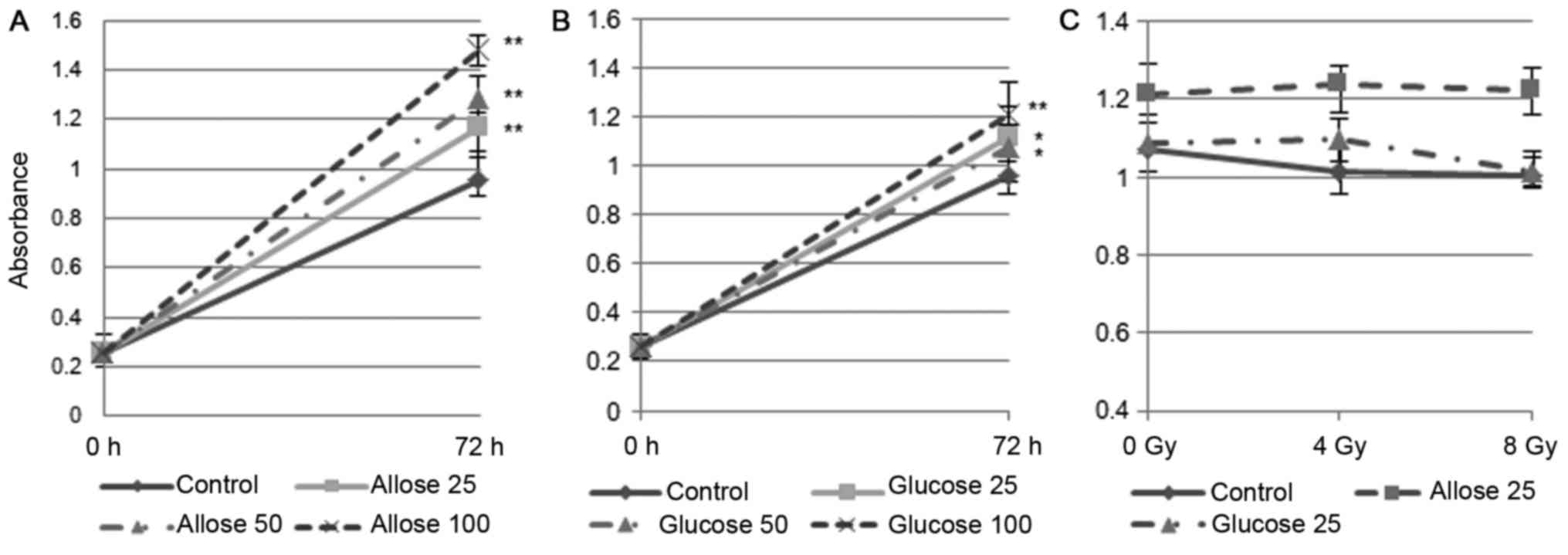
Compared to untreated cells, the growth of TIG-1
cells exposed to 25 mM D-allose or D-glucose increased
significantly, by 116.8% (P<0.001) and 112.1% (P<0.01),
respectively. The growth promoting effect of D-allose was dose
dependent (Fig. 1A and B). No
significant reduction in cell number was observed following
irradiation with 4 Gy (94.6%, P=0.2) or 8 Gy (93.9%, P=0.2) in the
control cells. D-glucose treated cells were also unaffected by 4 Gy
irradiation (101%, P=0.84), although their growth was marginally
suppressed after an 8 Gy irradiation (93%, P=0.051). D-allose
treated cells were unaffected by either of the radiation doses (4
Gy: 102%, P=0.62; 8 Gy: 101%, P=0.784) (Fig. 1C).
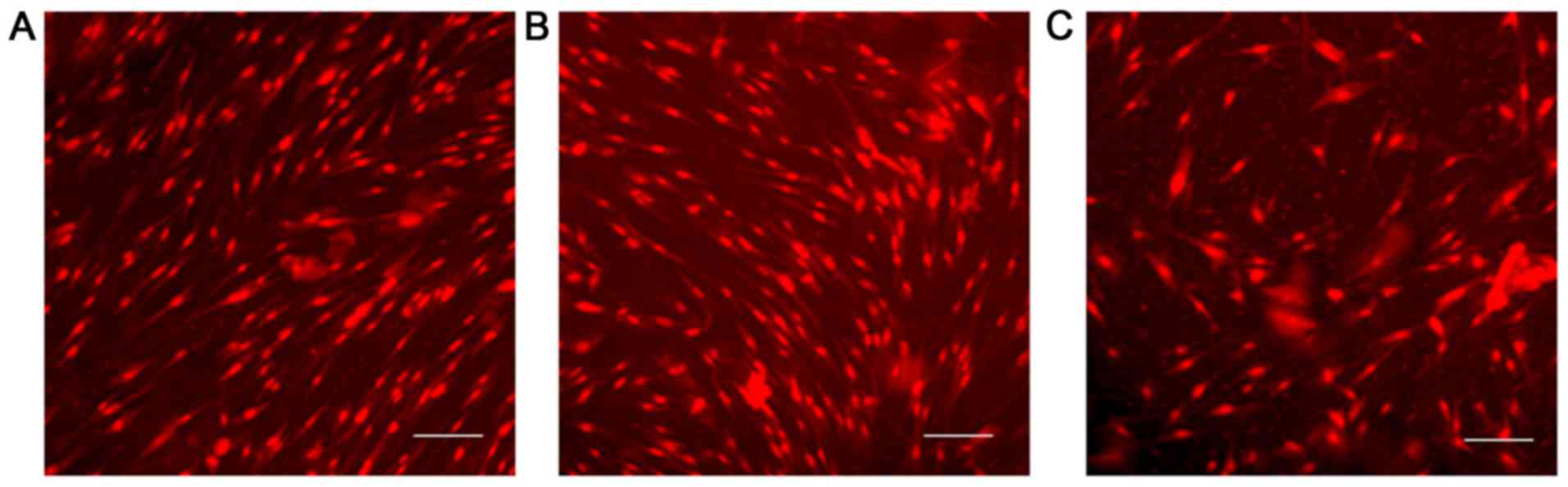
The TUNEL assay was carried out on the TIG-1 cell
line exposed to each sugar at 25 mM for 48 h, but no apoptotic
changes were observed (Fig. 2).
D-allose alters TRX and TXNIP mRNA
expression
To assess the effect of radiation on normal cells, 8
Gy was selected as the irradiation dose in this study. The mRNA
expression of TRX and TXNIP is summarized in Table I. In untreated TIG-1 cells, the ratio
of TRX and TXNIP (TRX/TXNIP) was 6.4.
The mRNA expression of TXNIP after D-allose treatment
increased approximately 2-fold, and as a result,
TRX/TXNIP decreased to 2.2. No apparent changes were
observed in either TXNIP or TRX mRNA expression after
8 Gy irradiation (ratio to control: 0.97 and 0.92, respectively),
and the TRX/TXNIP ratio was only slightly lower
(6.1). The effect of D-allose plus radiation was the same as that
of D-allose treatment alone. Compared with TIG-1 cells, the mRNA
expression level of TXNIP in HSC3 cells was relatively low
(50.4 vs. 1.5) and TRX/TXNIP was very high (61.7).
The mRNA expression of TXNIP after D-allose treatment had
increased about 74-fold and TRX/TXNIP dramatically
reduced to 1.4. The change of TXNIP mRNA expression after
radiation treatment was no greater than 2.6-fold and
TRX/TXNIP was 25.4. Combined D-allose and radiation
treatment enhanced TXNIP mRNA expression (ratio to control:
135.6), and TRX/TXNIP was reduced to 1.1.
 | Table I.Change of mRNA expression after the
D-allose and radiation treatment. |
Table I.
Change of mRNA expression after the
D-allose and radiation treatment.
| Cell line | Treatment | TXNIP | Ratio to
control | TRX | Ratio to
control | TRX/TXNIP |
|---|
| TIG-1 | Control | 50.4 |
| 323.2 |
| 6.4 |
|
| D-allose 25 mM | 106.5 | 2.1 | 237.5 | 0.74 | 2.2 |
|
| 8 Gy
irradiation | 48.7 | 0.97 | 295.9 | 0.92 | 6.1 |
|
| D-allose 25 mM+8
Gy | 95.3 | 1.9 | 232.8 | 0.72 | 2.4 |
| HSC3 | Control | 1.5 |
| 92.5 |
| 61.7 |
|
| D-allose 25 mM | 110.6 | 73.8 | 153.5 | 1.7 | 1.4 |
|
| 8 Gy
irradiation | 3.9 | 2.6 | 98.7 | 1.1 | 25.4 |
|
| D-allose 25 mM+8
Gy | 203.3 | 135.6 | 220.7 | 2.4 | 1.1 |
D-allose inhibits tumor growth and
enhances the efficacy of docetaxel and radiation in a mouse model
of HNSCC
In order to determine the appropriate dose for tumor
treatment, several different doses were tested, and we found that
25 mM D-allose had the same antitumor effect as 50 mM or even
higher D-allose concentrations (data not shown).
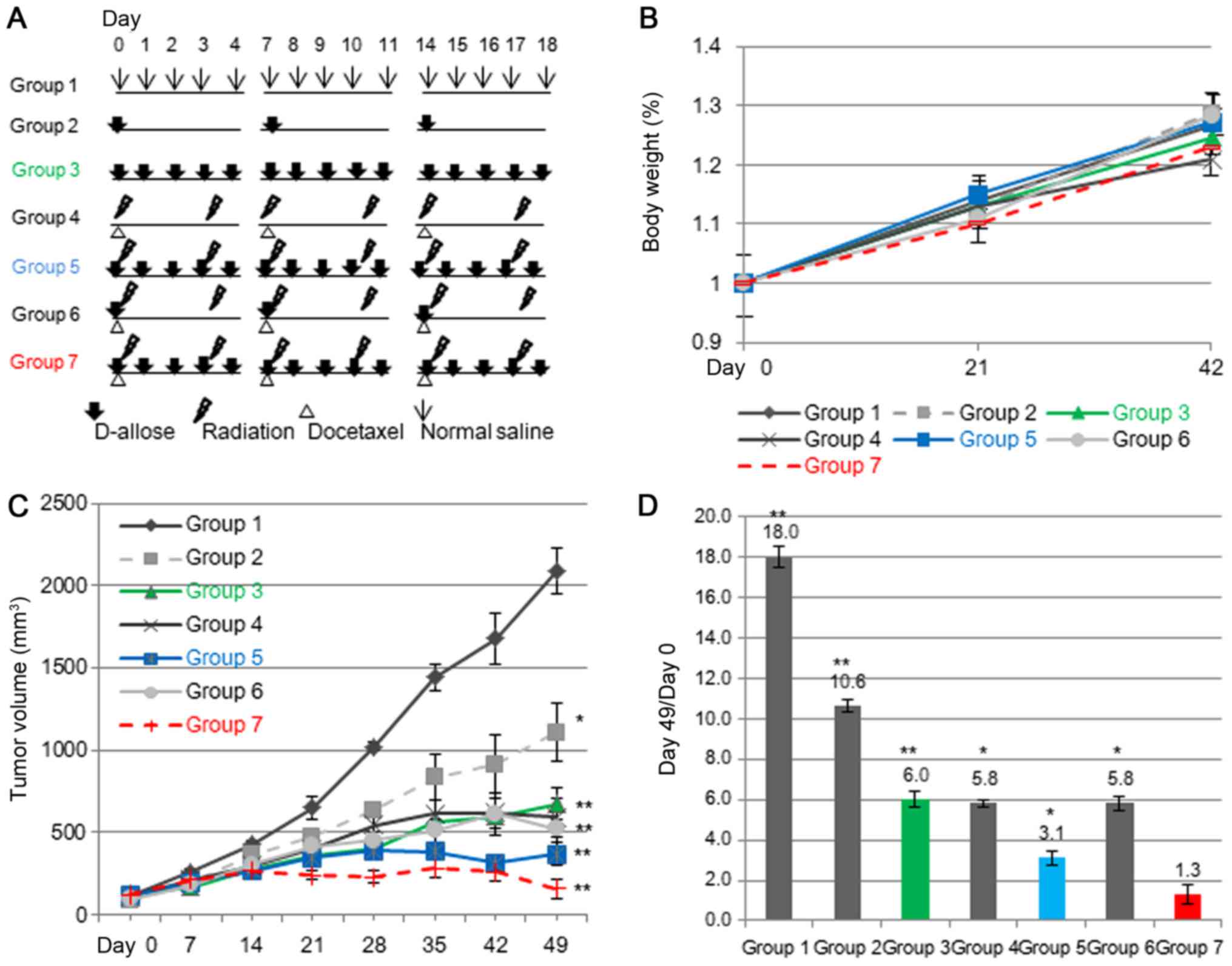
We then examined the growth inhibitory effect of
D-allose with or without radiation or docetaxel in this model. The
treatment schedules are shown in Fig.
3A. Although docetaxel plus radiation treated mice on average
suffered a ~5% decrease in body weight compared with normal saline
treated mice, the difference in weight was not statistically
significant (Fig. 3B). Overall, drug
treatment was well tolerated, with no apparent toxicity, and organ
macroscopic examinations were normal at sacrifice. The tumor growth
curves are shown in Fig. 3C. The mean
tumor volumes in all of the treated groups were significantly lower
than that of the control group at day 49 (P<0.0005). The
greatest tumor inhibition was observed in group 7 and then group 5,
with weaker inhibition in groups 3, 4 and 6. A moderate inhibition
was achieved in group 2. The mean tumor volume in the group treated
with multiple-doses of D-allose, weekly-docetaxel, and radiation
(group 7) was significantly lower than in mice treated with
weekly-docetaxel plus radiation (group 4) (P<0.001). The changes
in tumor volume ratios are shown in Fig.
3D. The tumor volume had increased 18-fold in the saline
treated group (group 1) at day 49, but only 10.6- and 6-fold in the
mice treated with D-allose once or 5 times a week (group 2 and 3,
respectively). The treatment effect in group 3 was the same as that
achieved with docetaxel plus radiation (group 4, 5.8-fold).
Treatment with D-allose 5 times a week and radiation (group 5)
reduced the tumor volume significantly (3.1-fold). Compared with
group 4, additional D-allose treatment once a week did not enhance
the tumor inhibitory effect at day 49 (group 6: 5.8-fold). However,
the growth inhibitory effect in group 6 persisted 11 weeks after
the initiation of treatment, while the tumors in the group 4 and
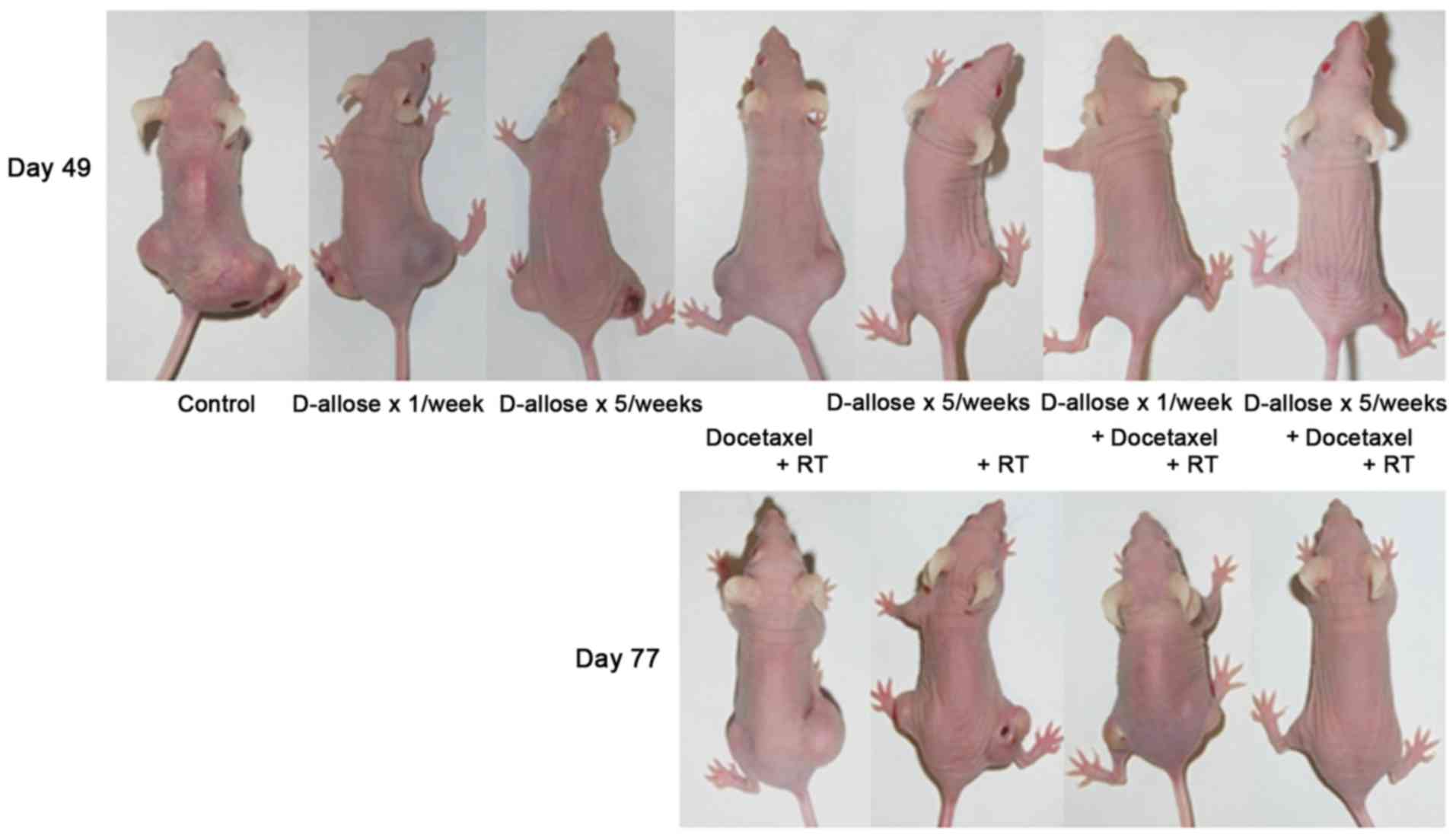
group 5 mice had re-grown. Half of the tumors disappeared in the
group treated with multiple-doses of D-allose, weekly low-dose
docetaxel, and radiation (group 7) (Fig.
4).
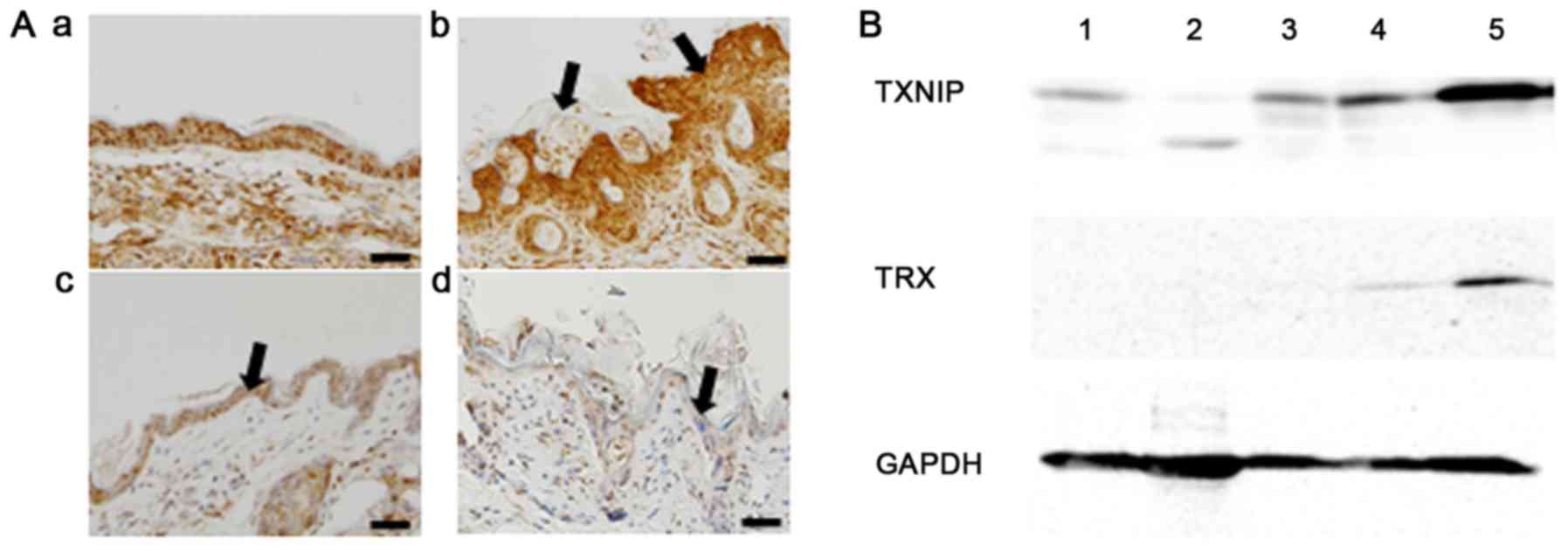
Radiation-induced skin
inflammation
Histopathological findings of normal skin are shown
in Fig. 5Aa. Weak to moderate
increased TNF-α expression was observed in untreated epithelium.
Radiation exposure resulted in an increase in epidermal thickening
and hyperkeratosis (Fig. 5Ab). Strong
increased TNF-α expression was also observed in the irradiated
epithelium. Weak increased TNF-α expression was found in the
D-allose treated epithelium (Fig.
5Ac). D-allose treatment suppressed TNF-α expression and
epidermal thickening, whilst, hyperkeratosis followed the combined
use of D-allose and radiation treatment (Fig. 5Ad).
 | Figure 5.TNF-α, TXNIP and TRX expression after
the treatment. Histological features of the skin region. Three
weeks after the initial treatment, skin specimens were obtained and
fixed with 4% PFA. To observe inflammatory changes, TNF-α antibody
was used. (Aa) Normal, saline-treated skin was included as a
control (bar, 50 µm). (Ab) Hyperkeratosis and epidermal thickening
(arrows) were observed after radiotherapy, with strong TNF-α
staining. (Ac) Weak TNF-α staining was observed with D-allose
treatment (arrow). (Ad) Radiation-induced epidermal thickening and
TNF-α staining were reduced with additional D-allose treatment
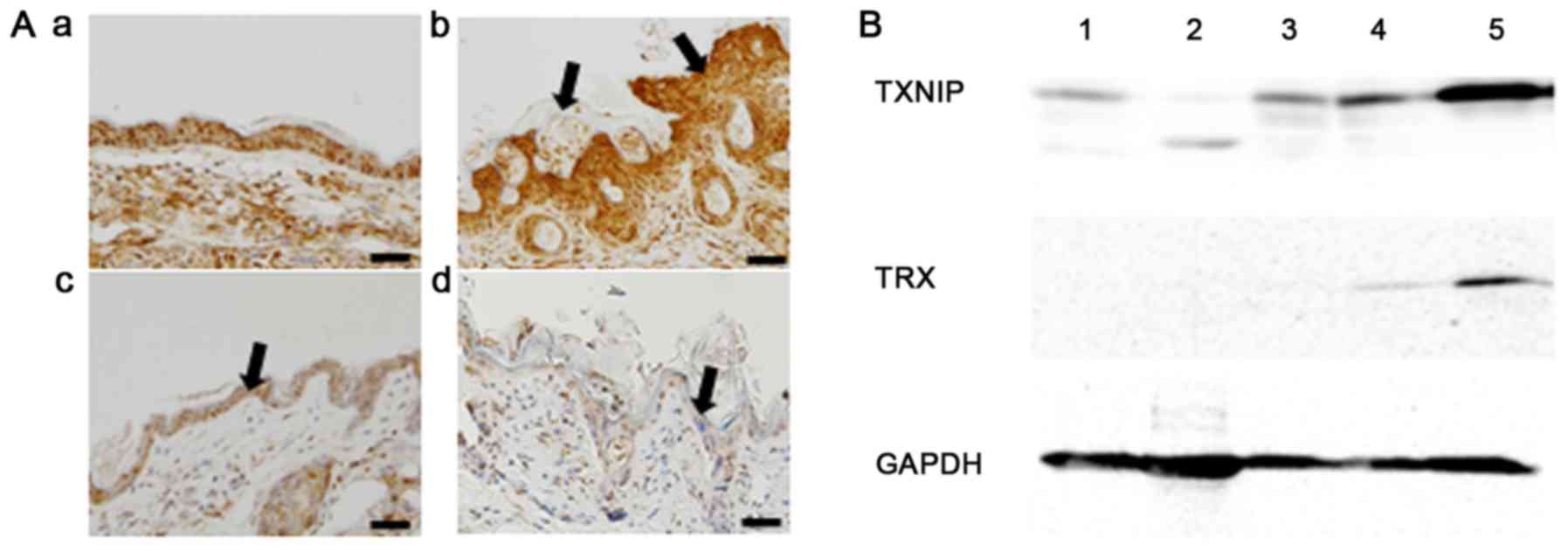
(arrow). (B) Western blot analysis of TXNIP and TRX expression.
Proteins were obtained from: 1, normal skin with saline treatment;
2, normal skin with D-allose treatment for 2 weeks; 3, tumor tissue
with saline treatment; 4, tumor tissue with D-allose treatment for
2 weeks; and 5, tumor tissue with D-allose treatment for 3 weeks.
TXNIP, thioredoxin interacting protein; TRX, thioredoxin; TNF-α,
tumor necrosis factor-α. |
Additive effect of D-allose
Western blot analyses revealed that no apparent
change was observed about the expression of TXNIP in normal skin by
D-allose treatment. The expression of TXNIP in transplanted tumor
tissue after 3 weeks of D-allose treatment was markedly increased
in comparison to tumors treated with D-allose for only 2 weeks
(Fig. 5B). TRX expression increased
slightly after 3 weeks of D-allose treatment.
Discussion
Oxidant stress induced by irradiation or anticancer
drugs produces a variety of highly reactive free radicals that
damage cells, initiate signal transduction pathways, and alter gene
expression. Therefore, regulation of the redox state is one of the
key mechanisms that can be used to control cancer cell growth.
In the present study, the mRNA expression of
TXNIP in HSC3 cancer cells increased about 74 times (1.5 to
110.6), and the TRX/TXNIP ratio was reduced from 61.7
to 1.4 after D-allose treatment. We previously reported that
induction of TXNIP by D-allose can enhance the radiation effects by
increasing the intracellular ROS level and radiation-induced
apoptosis (22). Combined use of
D-allose and docetaxel also enhanced antitumor effect following
upregulation of TXNIP expression and control of the intracellular
ROS level (23).
In addition, D-allose inhibited the growth of head
and neck cancer cells by inducing of cell cycle arrest, apoptosis
and competition with glucose uptake (24). On the other hand, TXNIP
expression in normal cells (TIG-1) was high (50.4) and the
TRX/TXNIP ratio was much lower than in HSC3 cancer
cells (6.4 vs. 61.7).
The in vivo experiment revealed that the
tumor inhibitory effect of D-allose was greater when it was
administered 5 times a week rather than once a week. Western blot
analysis also showed that the expression of TXNIP was greater after
D-allose treatment for 3 weeks compared to only 2 weeks. These
results suggest that the tumor inhibitory effect of D-allose
depends on the frequency or period of administration rather than
just the total dose. D-allose combined with weekly-docetaxel and
radiation markedly suppressed tumor growth, and 5 of the 10
transplanted tumors disappeared when treated with additional,
multiple doses of D-allose together with docetaxel and radiation.
None of the remaining 5 residual tumors showed any sign of
re-growth in the observation period. Furthermore, D-allose had no
growth inhibitory effect on human fibroblast TIG-1 cells, although
the mRNA expression of TXNIP was slightly increased
following D-allose administration. There was also no apoptotic
change in these cells after D-allose treatment. TIG-1 cell line was
established from human embryonic lung fibroblast and widely used as
a standard normal cell with limited life span (25). These findings suggest that D-allose
may not induce the local damage to normal tissue. In the mouse
model, D-allose treatment seemed to suppress radiation toxicities
such as epidermal thickening and inflammation. TNF-α is one of the
important mediators of inflammation, a key event in the cutaneous
radiation reaction (26). Radiation
induced TNF-α expression was reduced with combined use of D-allose.
Taken together, these findings suggest that D-allose might
specifically radiosensitize cancer cells and thus could potentially
reduce treatment-related toxicity in the clinical setting.
Several agents have been shown to act as
chemosensitizers and radiosensitizers, including nimorazole
(27), flavoperidol (28), and curcumin (29). Although each agent showed efficacy in
preclinical tests, this has not been supported by the findings of
clinical trials. Suberoylanilide hydroxamic acid, which is a strong
histone deacetylase inhibitor (HDACi), arrests cancer cell growth
by up-regulating TXNIP and down-regulating TRX expression (30). The modulation of DNA damage signaling
and repair by HDACi may be one underlying mechanism by which they
radiosensitize cancer cells (31–33).
Several clinical trials have been carried out using combined HDACi
and radiation (34–36). Although HDACi was more effective as a
single agent in hematological malignancies rather than in solid
tumors, its ability to radiosensitize cells remains unclear.
Generally, head and neck cancers are present within
the field of vision and are palpable. Therefore, local injection
might be a more effective route than oral intake or intravenous
injection. However, other delivery routes or systems are needed to
deliver D-allose to other tumor types. In addition, further
evaluation is needed of D-allose combined with other anticancer
drugs.
In conclusion, our findings show that D-allose acts
as an enhancer of radiotherapy and chemotherapy and may reduce the
severity of radiation-induced reactions such as dermatitis and
mucositis. These preclinical studies justify clinical trials to
further evaluate the potential of D-allose for the treatment of
HNSCC.
Acknowledgements
This study was supported in part by a Grant-in-Aid
for Project to accelerate development of Rare Sugar Research in
2017, Kagawa Prefectural Government, Japan.
References
|
1
|
Pignon JP, Bourhis J, Domenge C and
Designé L: Chemotherapy added to locoregional treatment for head
and neck squamous-cell carcinoma: Three meta-analyses of updated
individual data. MACH-NC Collaborative Group. Meta-analysis of
chemotherapy on head and neck cancer. Lancet. 355:949–955. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bourhis J, Le Maître A, Baujat B, Audry H
and Pignon J; Meta-Analysis of Chemotherapy in Head, Neck Cancer
Collaborative Group, ; Meta-Analysis of Radiotherapy in Carcinoma
of Head, Neck Collaborative Group, ; Meta-Analysis of Chemotherapy
in Nasopharynx Carcinoma Collaborative Group, : Individual
patients' data meta-analyses in head and neck cancer. Curr Opin
Oncol. 19:188–194. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Browman GP, Hodson DI, Mackenzie RJ,
Bestic N and Zuraw L; Cancer Care Ontario Practice Guideline
Initiative Head and Neck Cancer Disease Site Group, : Choosing a
concomitant chemotherapy and radiotherapy regimen for squamous cell
head and neck cancer: A systematic review of the published
literature with subgroup analysis. Head Neck. 23:579–589. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Forastiere AA, Goepfert H, Maor M, Pajak
TF, Weber R, Morrison W, Glisson B, Trotti A, Ridge JA, Chao C, et
al: Concurrent chemotherapy and radiotherapy for organ preservation
in advanced laryngeal cancer. N Engl J Med. 349:2091–2209. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Denis F, Garaud P, Bardet E, Alfonsi M,
Sire C, Germain T, Bergerot P, Rhein B, Tortochaux J and Calais G:
Final results of the 94-01 french head and neck oncology and
radiotherapy group randomized trial comparing radiotherapy alone
with concomitant radiochemotherapy in advanced-stage oropharynx
carcinoma. J Clin Oncol. 22:69–76. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wendt TG, Grabenbauer GG, Rödel CM, Thiel
HJ, Aydin H, Rohloff R, Wustrow TP, Iro H, Popella C and Schalhorn
A: Simultaneous radiochemotherapy versus radiotherapy alone in
advanced head and neck cancer: A randomized multicenter study. J
Clin Oncol. 16:1318–1324. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nabell L and Spencer S: Docetaxel with
concurrent radiotherapy in head and neck cancer. Semin Oncol. 30 6
Suppl 18:S89–S93. 2003. View Article : Google Scholar
|
|
8
|
Fujii M, Tsukuda M, Satake B, Kubota A,
Kida A, Kohno N, Okami K and Inuyama Y; Japan Cooperative Head and
Neck Oncology Group (JCHNOG), : Phase I/II trial of weekly
docetaxel and concomitant radiotherapy for squamous cell carcinoma
of the head and neck. Int J Clin Oncol. 9:107–112. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Furusaka T, Matsuda A, Saito T, Katsura Y
and Ikeda M: Concurrent chemoradiation therapy with docetaxel (DOC)
for laryngeal preservation in T2N0M0 glottic squamous cell
carcinomas. Acta Otolaryngol. 133:99–112. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Calais G, Bardet E, Sire C, Alfonsi M,
Bourhis J, Rhein B, Tortochaux J, Man YT, Auvray H and Garaud P:
Radiotherapy with concomitant weekly docetaxel for stages III/IV
oropharynx carcinoma. Results of the 98-02 GORTEC phase II trial.
Int J Radiat Oncol Biol Phys. 58:161–166. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Holmgren A: Thioredoxin. Annu Rev Biochem.
54:237–271. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Miyazaki K, Noda N, Okada S, Hagiwara Y,
Miyata M, Sakurabayashi I, Yamaguchi N, Sugimura T, Terada M and
Wakasugi H: Elevated serum level of thioredoxin in patients with
hepatocellular carcinoma. Biotherapy. 11:277–288. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nakamura H, Bai J, Nishinaka Y, Ueda S,
Sasada T, Ohshio G, Imamura M, Takabayashi A, Yamaoka Y and Yodoi
J: Expression of thioredoxin and glutaredoxin, redox-regulating
proteins, in pancreatic cancer. Cancer Detect Prev. 24:53–60.
2000.PubMed/NCBI
|
|
14
|
Grogan TM, Fenoglio-Prieser C, Zeheb R,
Bellamy W, Frutiger Y, Vela E, Stemmerman G, Macdonald J, Richter
L, Gallegos A and Powis G: Thioredoxin, a putative oncogene
product, is overexpressed in gastric carcinoma and associated with
increased proliferation and increased cell survival. Hum Pathol.
31:475–481. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kakolyris S, Giatromanolaki A, Koukourakis
M, Powis G, Souglakos J, Sivridis E, Georgoulias V, Gatter KC and
Harris AL: Thioredoxin expression is associated with lymph node
status and prognosis in early operable non-small cell lung cancer.
Clin Cancer Res. 7:3087–3091. 2001.PubMed/NCBI
|
|
16
|
Raffel J, Bhattacharyya AK, Gallegos A,
Cui H, Einspahr JG, Alberts DS and Powis G: Increased expression of
thioredoxin-1 in human colorectal cancer is associated with
decreased patient survival. J Lab Clin Med. 142:46–51. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nishiyama A, Matsui M, Iwata S, Hirota K,
Masutani H, Nakamura H, Takagi Y, Sono H, Gon Y and Yodoi J:
Identification of thioredoxin-binding protein-2/vitamin D(3)
up-regulated protein 1 as a negative regulator of thioredoxin
function and expression. J Biol Chem. 274:21645–21650. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Junn E, Han SH, Im JY, Yang Y, Cho EW, Um
HD, Kim DK, Lee KW, Han PL, Rhee SG and Choi I: Vitamin D3
up-regulated protein 1 mediates oxidative stress via suppressing
the thioredoxin function. J Immunol. 164:6287–6295. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Han SH, Jeon JH, Ju HR, Jung U, Kim KY,
Yoo HS, Lee YH, Song KS, Hwang HM, Na YS, et al: VDUP1 upregulated
by TGF-beta1 and 1,25-dihydorxyvitamin D3 inhibits tumor cell
growth by blocking cell-cycle progression. Oncogene. 22:4035–4046.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sui L, Dong Y, Watanabe Y, Yamaguchi F,
Hatano N, Izumori K and Tokuda M: Growth inhibitory effect of
D-allose on human ovarian carcinoma cells in vitro. Anticancer Res.
25:2639–2644. 2005.PubMed/NCBI
|
|
21
|
Yamaguchi F, Takata M, Kamitori K, Nonaka
M, Dong Y, Sui L and Tokuda M: Rare sugar D-allose induces specific
up-regulation of TXNIP and subsequent G1 cell cycle arrest in
hepatocellular carcinoma cells by stabilization of p27kip1. Int J
Oncol. 32:377–385. 2008.PubMed/NCBI
|
|
22
|
Hoshikawa H, Indo K, Mori T and Mori N:
Enhancement of the radiation effects by D-allose in head and neck
cancer cells. Cancer Lett. 306:60–66. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Indo K, Hoshikawa H, Kamitori K, Yamaguchi
F, Mori T, Tokuda M and Mori N: Effects of D-allose in combination
with docetaxel in human head and neck cancer cells. Int J Onclol.
45:2044–2050. 2014. View Article : Google Scholar
|
|
24
|
Mitani T, Hoshikawa H, Mori T, Hosokawa T,
Tsukamoto I, Yamaguchi F, Kamitori K, Tokuda M and Mori N: Growth
inhibition of head and neck carcinomas by D-allose. Head Neck.
31:1049–1055. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kamada M, Kumazaki T, Matsuo T, Mitsui Y
and Takahashi T: Establishment of ultra long-lived cell lines by
transfection of TERT into normal human fibroblast TIG-1 and their
characterization. Cell Biol Int. 36:519–527. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Müller K and Meineke V: Radiation-induced
alterations in cytokine production by skin cells. Exp Hematol. 35 4
Suppl 1:S96–S104. 2007. View Article : Google Scholar
|
|
27
|
Metwally MA, Frederiksen KD and Overgaard
J: Compliance and toxicity of the hypoxic radiosensitizer
nimorazole in the treatment of patients with head and neck squamous
cell carcinoma (HNSCC). Acta Oncol. 53:654–661. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhai S, Senderowicz AM, Sausville EA and
Figg WD: Flavopiridol, a novel cyclin-dependent kinase inhibitor,
in clinical development. Ann Pharmacother. 36:905–911. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Goel A and Aggarwal BB: Curcumin, the
golden spice from indian saffron, is a chemosensitizer and
radiosensitizer for tumors and chemoprotector and radioprotector
for normal organs. Nutr Cancer. 62:919–930. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Butler LM, Zhou X, Xu WS, Scher HI,
Rifkind RA, Marks PA and Richon VM: The histone deacetylase
inhibitor SAHA arrests cancer cell growth, up-regulates
thioredoxin-binding protein-2, and down-regulates thioredoxin. Proc
Natl Acad Sci USA. 99:pp. 11700–11705. 2002; View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Nolan L, Johnson PW, Ganesan A, Packham G
and Crabb SJ: Will histone deacetylase inhibitors require
combination with other agents to fulfil their therapeutic
potential? Br J Cancer. 99:689–694. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Shabason JE, Tofilon PJ and Camphausen K:
Grand rounds at the national institutes of health: HDAC inhibitors
as radiation modifiers, from bench to clinic. J Cell Mol Med.
15:2735–2744. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Spiegel S, Milstien S and Grant S:
Endogenous modulators and pharmacological inhibitors of histone
deacetylases in cancer therapy. Oncogene. 31:537–551. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Masoudi A, Elopre M, Amini E, Nagel ME,
Ater JL, Gopalakrishnan V and Wolff JE: Influence of valproic acid
on outcome of high-grade gliomas in children. Anticancer Res.
28:2437–2442. 2008.PubMed/NCBI
|
|
35
|
Ree AH, Dueland S, Folkvord S, Hole KH,
Seierstad T, Johansen M, Abrahamsen TW and Flatmark K: Vorinostat,
a histone deacetylase inhibitor, combined with pelvic palliative
radiotherapy for gastrointestinal carcinoma: The Pelvic Radiation
and Vorinostat (PRAVO) phase 1 study. Lancet Oncol. 11:459–464.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Candelaria M, Cetina L, Pérez-Cárdenas E,
De La Cruz-Hernández E, González-Fierro A, Trejo-Becerril C,
Taja-Chayeb L, Chanona J, Arias D and Dueñas-González A: Epigenetic
therapy and cisplatin chemoradiation in FIGO stage IIIB cervical
cancer. Eur J Gynaecol Oncol. 31:386–391. 2010.PubMed/NCBI
|