Introduction
Multiple myeloma (MM) is a hematological tumor of
plasma cells that shows characteristic expansion of tumor cells
within the bone marrow. Since the microenvironment within bone
marrow is unique in terms of cytokine production and its
interaction with various cells including MM cells, these
environments can influence the survival and drug resistance of MM
cells (1–3). In particular, oxygen concentration in
the microenvironment is one of the greatest factors controlling
survival of MM cells (4).
Oxygen plays an important role for MM cells by
influencing the sensitivity to chemotherapeutic reagents. Previous
studies showed that the sensitivity of MM cells to melphalan is
reduced by hypoxia (5). Similar
findings with other chemotherapeutic drugs have also been reported
in various solid tumors (6–9). Therefore, these data suggest the
existence of universal mechanisms by which oxygen concentration can
regulate drug sensitivity. Notably, it is well known that oxygen
concentration is extremely low in bone marrow, where MM cells
survive and grow, and that drug-resistant MM cells can be generated
within bone marrow, thus contributing to recurrence of the disease.
Therefore, manipulation of hypoxia-induced drug resistance should
be essential to improve survival of MM patients.
In this study, we searched for chemical compounds
with the ability to kill myeloma cells under hypoxic conditions. We
performed drug screening using a natural compound library and
identified bufalin, a component of a Chinese medicine (Chan Su). We
also analyzed the molecular mechanisms underlying the cytotoxicity
of bufalin to MM cells under hypoxic conditions which has not been
reported.
Materials and methods
Screening of compounds
A natural compound library consisting of 258
compounds was obtained from the Institute of Natural Medicine,
Toyama University (Toyama, Japan). Each compound was supplemented
to myeloma cell lines at a concentration of 10 µM and treated cells
were cultured for 5 days under 1% oxygen concentration using a
hypoxic culture chamber (Astec, Fukuoka, Japan).
Cell lines and cell culture
Two human myeloma cell lines, KMS12PE (10) and U266 (11) were utilized. Cells were cultured in
RPMI-1640 medium supplemented with 10% fetal calf serum at 37°C
with humidified air. Human peripheral blood mononuclear cells
(PMBCs) were obtained from a healthy volunteer and purified by
Ficoll density gradation.
Cytotoxic and apoptosis assays
Cytotoxicity of the compounds was analyzed by Cell
Counting Kit-8 (Dohjin Chemicals, Kumamoto, Japan) or trypan blue
dye exclusion assay according to the manufacturer's protocol. The
MEBCYTO Apoptosis kit was used to detect apoptosis by flow
cytometry using FACSVerse (BD Biosciences, Franklin Lakes, NJ, USA)
according to the manufacturer's protocol. Melphalan and
lenalidomide were purchased from Santa Cruz Biotechnology, Inc.
(Santa Cruz, CA, USA) and Sigma-Aldrich; Merck KGaA, (Darmstadt,
Germany), respectively. A pan-caspase inhibitor, ZVAD-fmk (Medical
and Biological Laboratories, Nagoya, Japan), was utilized in some
experiment at a concentration of 32 nM.
Detection of reactive oxygen species
(ROS)
Production of ROS was analyzed using CellROX flow
cytometry assay kits (Thermo Fisher Scientific, Yokohama, JAPAN)
and FACS Verse according to the manufacturer's protocols.
Western blotting
Cell lysates were obtained by lysing cells with
M-PER mammalian protein extraction reagent (Thermo Fisher
Scientific, Inc., Yokohama, Japan) supplemented with phosphatase
inhibitor cocktail and protease inhibitor cocktail (Nacalai Tesque,
Kyoto, Japan). Antibodies for PARP, γ-H2A.X and HIF-1α were
purchased from Cell Signaling Technology, Inc. (Tokyo, Japan).
Statistical analysis
Statistical analysis between two groups was
performed by Student's t-test. For multiple group comparisons,
one-way or two-way ANOVA was performed. The data were analyzed
statistically by using GraphPad Prism software (GraphPad Software,
Inc., La Jolla, CA, USA) and P<0.05 was considered to indicate a
statistically significant difference.
Results
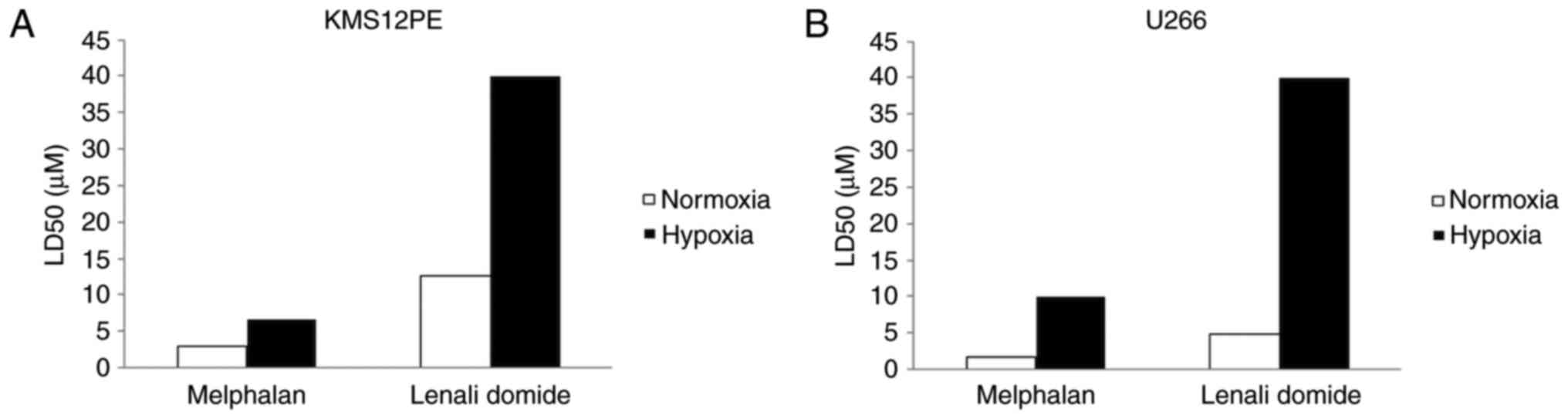
To confirm that myeloma cells show drug resistance
under hypoxic conditions, we treated myeloma cells with melphalan
and lenalidomide under normoxic or hypoxic conditions (Fig. 1). The LD50 values of melphalan in both
KMS12PE and U266 cells under normoxic conditions were 3.0 and 1.8
µM and those of lenalidomide were 12.6 and 4.9 µM, respectively.
Notably, the LD50 values of these reagents were elevated at hypoxic
conditions. The LD50 values of melphalan in KMS12PE and U266 cells
under hypoxic conditions were 6.7 and 9.9 µM, respectively, and the
LD50 values of lenalidomide in KMS12PE and U266 cells were above 40
µM. Together these data indicate that myeloma cells showed drug
resistance for these two reagents under low concentrations of
oxygen.
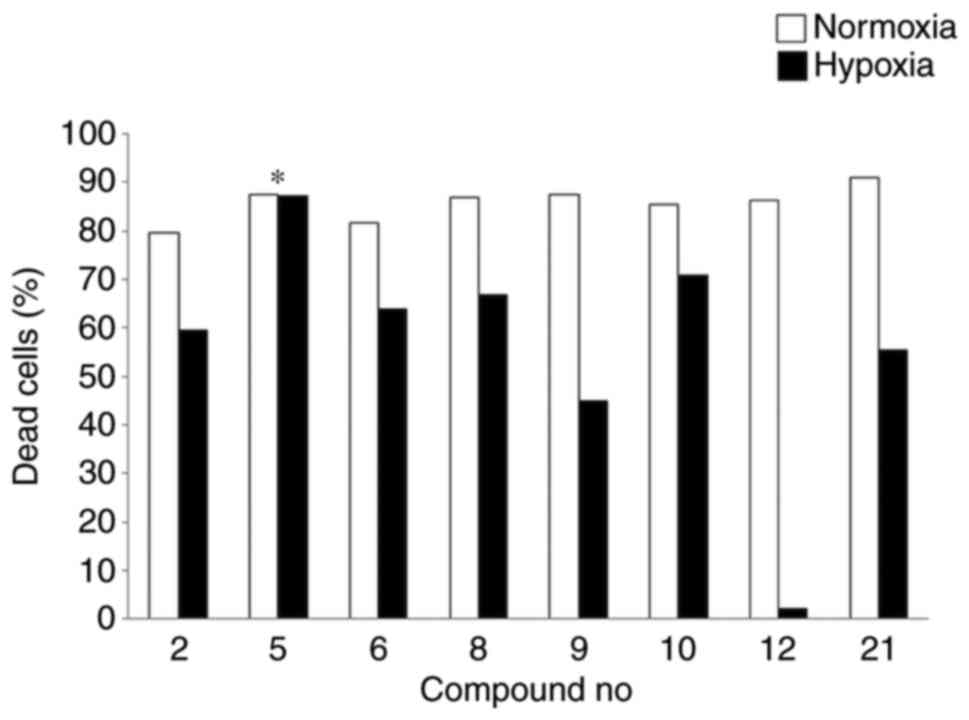
We next screened 258 compounds in a natural compound
library under hypoxic conditions in KMS12PE and U266 cells and
found that 8 compounds induced significant cell death of more than
50% of the whole cell population. We analyzed cytotoxicity of each
of these compounds in KMS12PE cells under both normoxic and hypoxic
conditions and found that bufalin exerted high cytotoxicity at both
conditions (compound no. 5 in Fig. 2)
while other compounds showed reduction in cell death at hypoxic
condition.
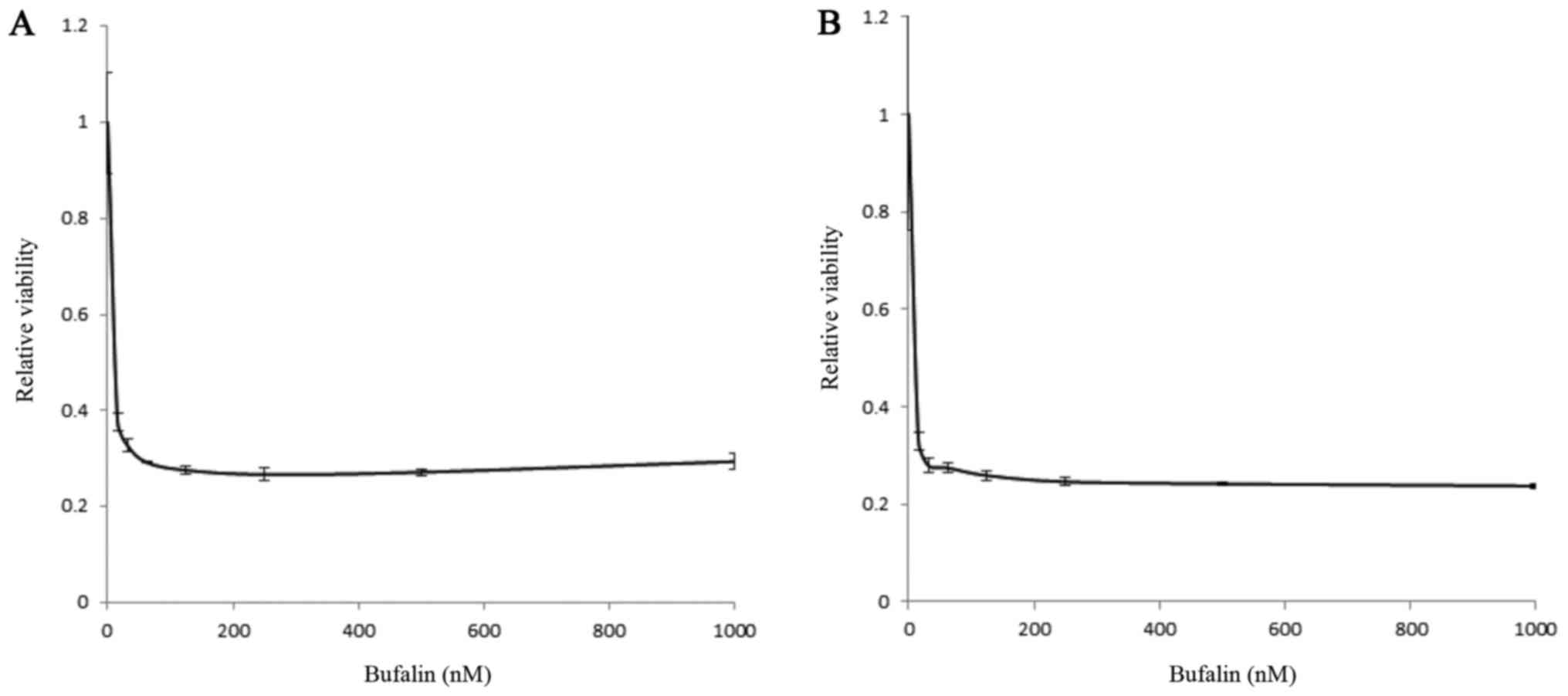
We thus further analyzed bufalin as a potential
candidate that retains cytotoxicity regardless of oxygen
concentration. A myeloma cell line, KMS12PE, was treated by bufalin
at various concentrations either under normoxic or hypoxic
conditions. As shown in Fig. 3,
bufalin induced significant cytotoxicity below micro-molar levels
independent of oxygen concentrations.
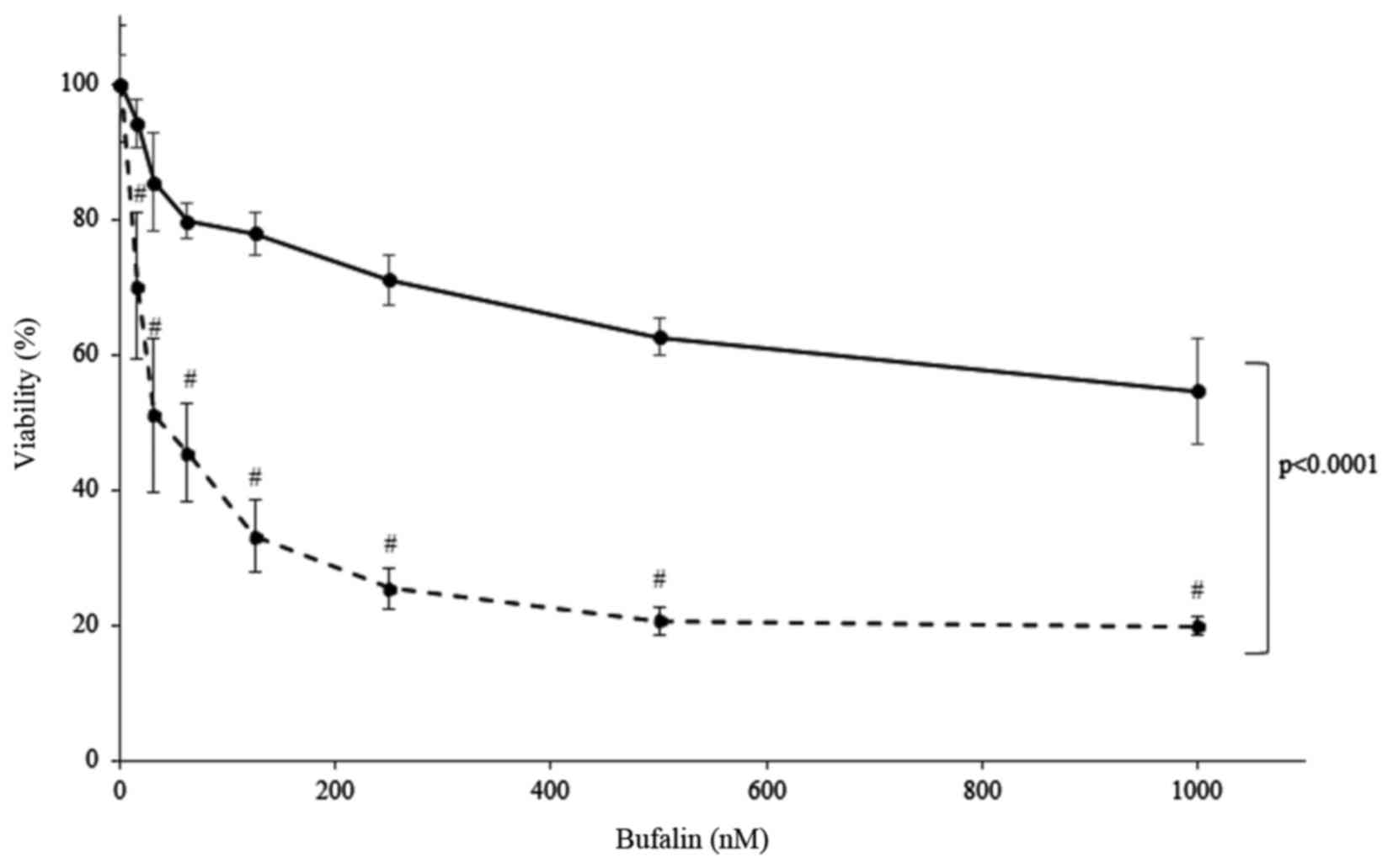
To elucidate whether bufalin shows toxicity to
freshly isolated cells, MM cells obtained from patient bone marrow
and PBMCs obtained from healthy volunteer were cultured and treated
with bufalin. The results showed that bufalin induced significant
cell death to primary MM cells, while it did not induce cell death
in PBMCs as much as those observed in primary MM cells
(P<0.0001, analyzed by two-way Anova) (Fig. 4). Together this suggests that bufalin
may not show toxicity to non-malignant cells.
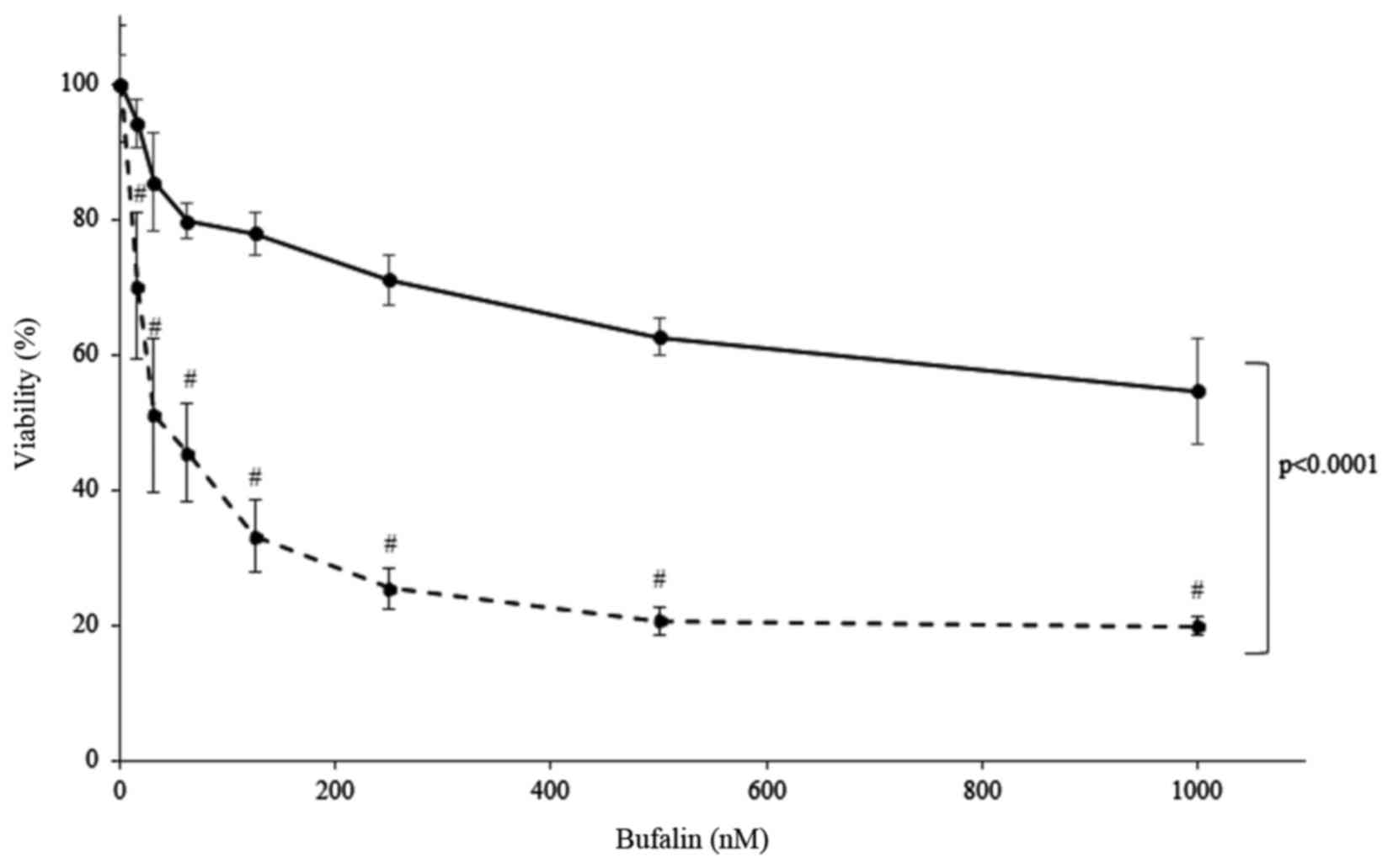 | Figure 4.Cytotoxic effect of bufalin in primary
myeloma cells (dotted line) and PBMCs from a healthy donor (solid
line) under normoxic conditions. Cells were incubated with the
indicated concentration of bufalin at 15.625, 31.25, 62.5, 125,
250, 500 and 1,000 nM for 24 h and cytotoxicity was evaluated by
cell counting kit. Freshly isolated myeloma cells showed marked
cytotoxicity by bufalin at dose dependent manner
(#P<0.0001 compared to bufalin 0 nM, analyzed by
one-way ANOVA and Bonferroni multiple comparison test) while
viability of PBMCs was retained more than 60%, suggesting PBMC is
less susceptible to bufalin than MM cells (P<0.0001, analyzed by
two-way ANOVA and Bonferroni multiple comparison test). PBMC,
peripheral blood mononuclear cell; MM, multiple myeloma. |
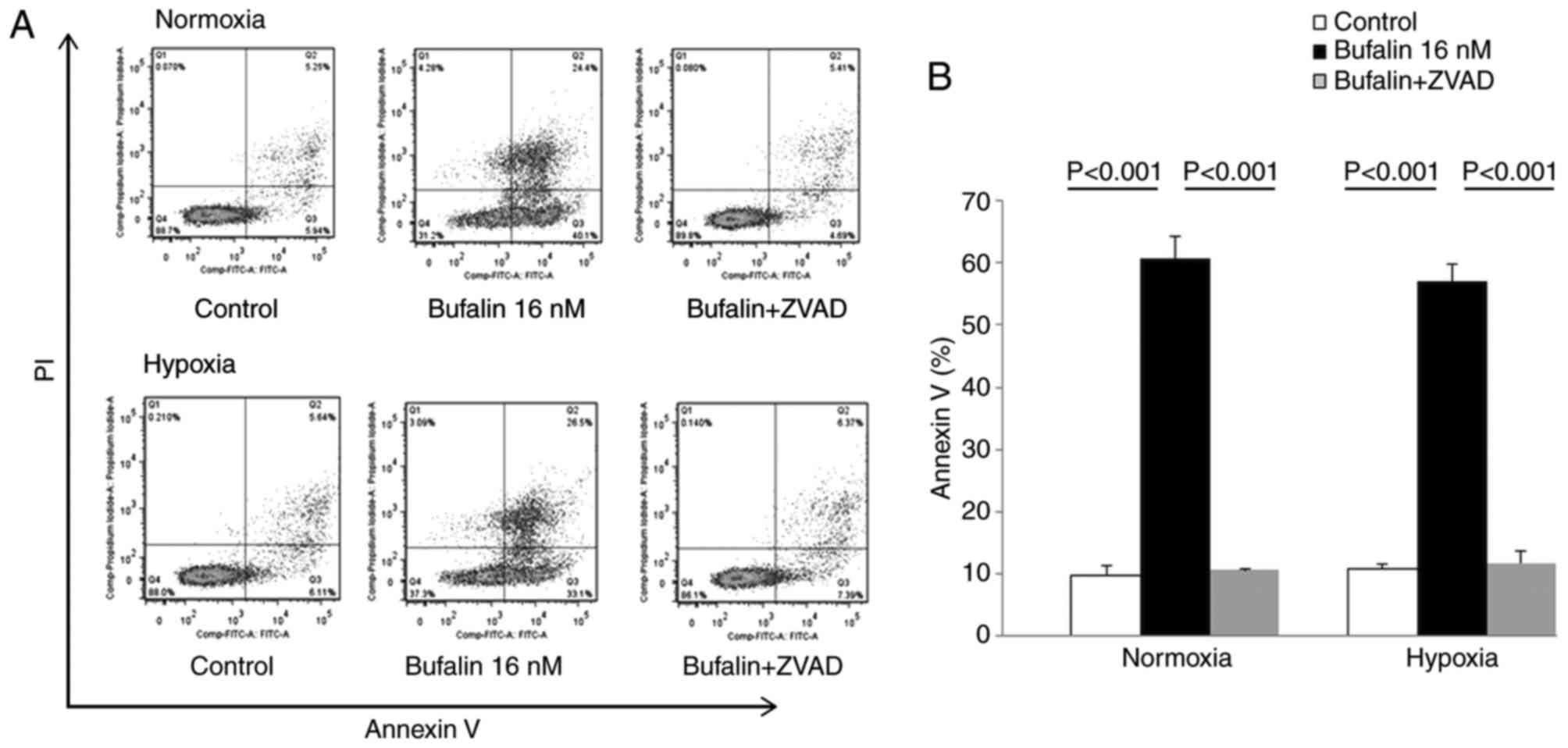
To further characterize the cytotoxicity by bufalin,
we performed Annexin V/PI analysis of KMS12PE cells treated with 32
nM bufalin for 24 h either at normoxic or hypoxic conditions.
Bufalin induced both early and late phase apoptosis and this
increase in apoptosis was reduced by treatment with a caspase
inhibitor (Fig. 5). These results
indicate that the cytotoxicity induced by bufalin involves
apoptosis mediated by caspase activation either in normoxic and
hypoxic conditions.
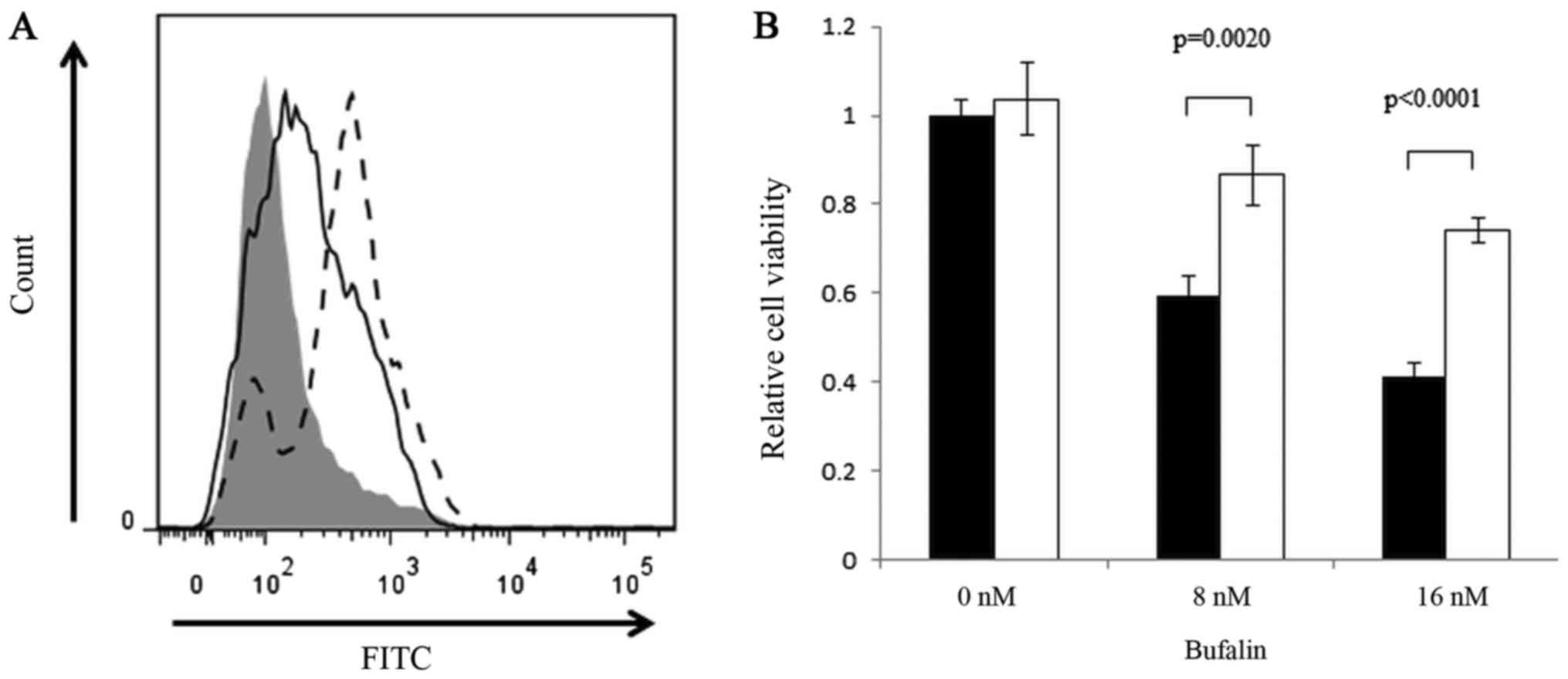
As ROS is an inducer of apoptosis, we next analyzed
the production of ROS in response to bufalin treatment. We observed
a significant induction of ROS with bufalin treatment, and this
induction was partially inhibited by N-acetyl cysteine (Fig. 6). This finding indicates that ROS
production may be one of the contributors for the cytotoxic effects
of bufalin.
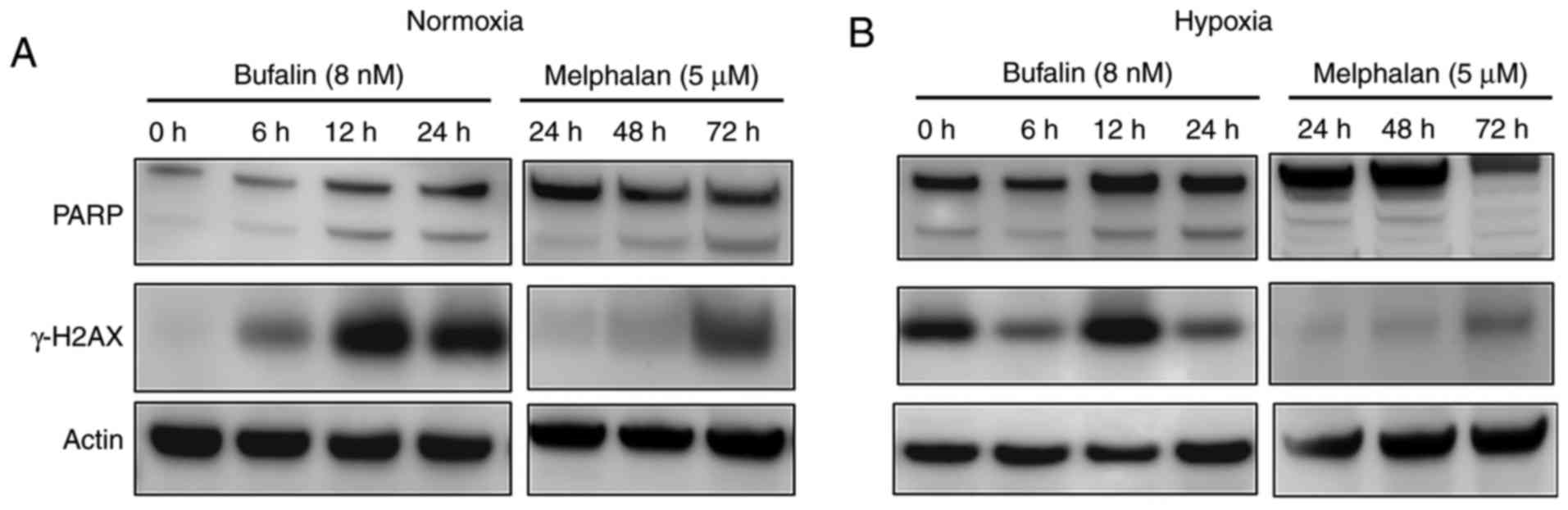
Since several reports previously showed that bufalin
induces DNA double strand breaks (DSBs) (12–14), we
analyzed γ-H2AX induction, which is a hallmark of the DSB response.
As shown in Fig. 7A, bufalin induced
γ-H2AX in myeloma cells in a time-dependent manner under normoxic
conditions. We also examined DSB induction under hypoxia
conditions, and found induction of γ-H2AX by bufalin as found at
normoxia (Fig. 7B). However,
induction of γ-H2AX by melphalan at normoxia was found at fewer
amounts and delayed as compared to bufalin. Moreover,
melphalan-induced γ-H2AX even impaired at hypoxic conditions
compared with normoxic conditions. Because melphalan did not show
anti-tumor effect not earlier than 24 h, western blot analysis at
earlier occasions is not shown. Cleavage of PARP was also observed
in response to bufalin treatment regardless of oxygen
concentration, while melphalan-inducing PARP cleavage was inhibited
at hypoxic conditions (Fig. 7A and
B).
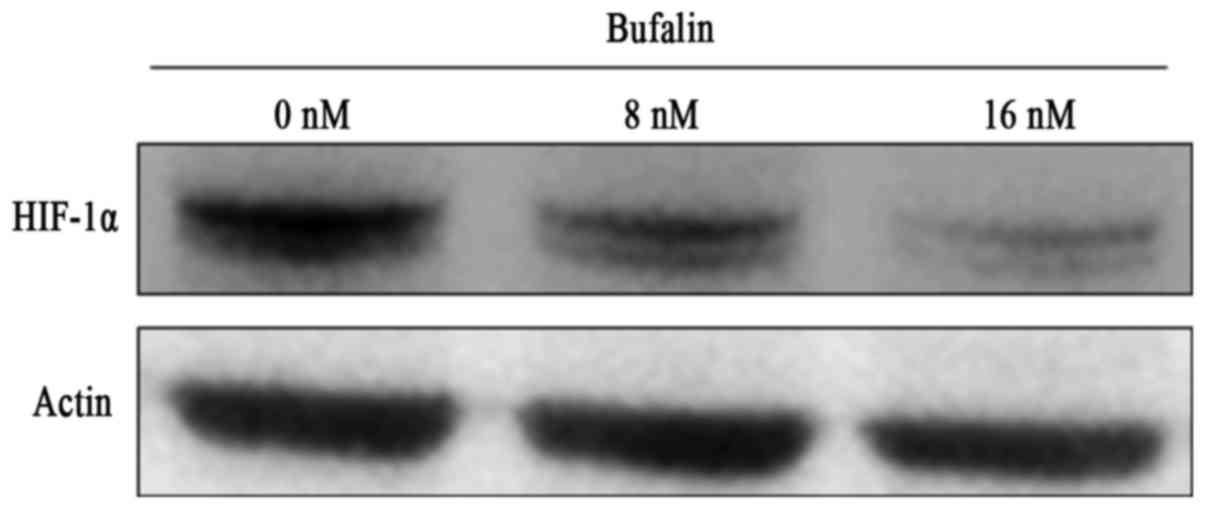
Since HIF-1α is induced and considered to contribute
drug resistance in hypoxia, we evaluated whether bufalin modulates
HIF-1α under hypoxic conditions. Interestingly, treatment of
myeloma cells with bufalin at 16 nM for 24 h significantly
inhibited the expression of HIF-1α in hypoxic conditions (Fig. 8), suggesting that the cytotoxic effect
of bufalin under hypoxia may involve the reduction of HIF-1α.
Discussion
Oxygen concentration plays a crucial role in the
survival of cancer cells. Low oxygen concentration induces
expression of numerous genes regulated by HIF-1α, a master
transcriptional factor under hypoxic conditions. One of the
features mediated by hypoxia is acquisition of drug resistance.
Previous reports demonstrated acquisition of drug resistance by
hypoxia in various types of cancer cells (4,7–9,15).
Mechanisms regulating drug resistance under hypoxia have been
described, involving microRNAs (16),
the multi-drug resistant (MDR) gene (15,17) or the
autophagy pathway (18). Modulating
these pathways is thought to re-sensitize tumor cells to
anti-cancer reagents.
Previous studies have examined the correlation
between hypoxia and cancer stem cells other than drug resistance
(19). Hypoxic conditions can
transform tumor cells to cancer stem cells and are required for the
maintenance of cancer stem cells (20–22).
Targeting cancer stem cells should be important to eradicate tumor
cells. We previously reported that hypoxic conditions transform
myeloma cells to an immature phenotype, suggesting that myeloma
stem cells may adapt to hypoxic conditions (23). Because melphalan and lenalidomide
showed reduced efficacy at hypoxic conditions as shown in this
report, our results suggest that these treatments may not retain
the ability to target myeloma stem cells, although we did not
perform confirmatory experiments using myeloma stem cells this
time. Recently, Sun et al, reported that bufalin inhibits
stemness and overcome drug resistance of colon cancer cells
(24). This finding enforces our
results and warrants usage of bufalin to exterminate myeloma stem
cells.
We found, for the first time, that bufalin induced
the DSB response in MM cells independent of oxygen concentrations.
Although DSB response mediated by bufalin at normoxic condition has
scarcely been reported in solid tumors, especially interacting to
topoisomerase II (12–14), the function of bufalin under hypoxic
conditions has not been fully elucidated. Only two previous reports
described a correlation between bufalin and hypoxia in colon,
cervical and hepatocellular carcinoma cells, and these studies
suggested that reduction of HIF-1 could be involved in the
cytotoxicity induced by bufalin (25,26).
Interestingly, we found a decrease of HIF-1α in response to
treatment with bufalin under hypoxic conditions in MM cells. As a
growing body of evidence has shown a central role of hypoxia in the
acquisition of drug resistance, targeting HIF-1α is now considered
to be an important approach to overcome drug resistance (27,28).
Indeed, targeting HIF-1α sensitizes myeloma cells to
chemotherapeutic agents and reduces the number of myeloma stem
cells (5,29). Our finding of HIF-1α inhibition by
bufalin should contribute to the development of a HIF-1α targeted
strategy for treatment of MM. The demonstrated cytotoxicity by
bufalin regardless of oxygen concentration enforces the
significance of bufalin in the treatment of cancers survive within
hypoxic niche other than myeloma. However, we did not evaluated
ubiquitination or degradation of HIF-1 by the treatment with
bufalin at this time. Regulatory effect of bufalin in expression of
HIF-1 remains to be elucidated.
Adverse events, especially cardiotoxicity (30), caused by bufalin is an important issue
when using this reagent at clinical setting. However, the
concentration inducing cardiotoxicity was estimated as 1 mM which
was significantly higher than those exerting anti-tumor effect
presented in this manuscript, suggesting clinical usage of bufalin
might spare cardiotoxicity. Indeed, there have been several reports
showing in vivo findings (31,32). Given
the low working concentration of bufalin, as low as nano-molar
levels, the achievement of an effective concentration of bufalin
should be possible. Successful in vivo treatment of an
osteosarcoma-bearing mouse by bufalin suggests its future usage in
the clinical setting (33). In
addition, our findings demonstrating the low toxicity of bufalin in
normal PBMCs implies a low toxicity profile for normal tissues.
Acknowledgements
The authors would like to thank Dr Gabrielle White
Wolf for editing a draft of this manuscript.
Funding
This study was supported by in part by a grant from
the Japanese Amyloidosis Research Committee from the Ministry of
Health, Labor and Welfare (grant no. ippan-022).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
EF, YI and MK executed the experiments. NN, SE, SF,
NW, YO and TS supervised the experimental procedures and analysed
the results. YK performed the statistical analysis. HH conducted
experiments, organized the discussions and finalized the
manuscript.
Ethics approval and consent to
participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Di Marzo L, Desantis V, Solimando AG,
Ruggieri S, Annese T, Nico B, Fumarulo R, Vacca A and Frassanito
MA: Microenvironment drug resistance in multiple myeloma: Emerging
new players. Oncotarget. 7:60698–60711. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kawano Y, Moschetta M, Manier S, Glavey S,
Görgün GT, Roccaro AM, Anderson KC and Ghobrial IM: Targeting the
bone marrow microenvironment in multiple myeloma. Immunol Rev.
263:160–172. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang J, Faict S, Maes K, De Bruyne E, Van
Valckenborgh E, Schots R, Vanderkerken K and Menu E: Extracellular
vesicle cross-talk in the bone marrow microenvironment:
Implications in multiple myeloma. Oncotarget. 7:38927–38945.
2016.PubMed/NCBI
|
|
4
|
Garvalov BK and Acker T: Implications of
oxygen homeostasis for tumor biology and treatment. Adv Exp Med
Biol. 903:169–185. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hu Y, Kirito K, Yoshida K, Mitsumori T,
Nakajima K, Nozaki Y, Hamanaka S, Nagashima T, Kunitama M, Sakoe K
and Komatsu N: Inhibition of hypoxia-inducible factor-1 function
enhances the sensitivity of multiple myeloma cells to melphalan.
Mol Cancer Ther. 8:2329–2338. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Daster S, Amatruda N, Calabrese D, Ivanek
R, Turrini E, Droeser RA, Zajac P, Fimognari C, Spagnoli GC, Iezzi
G, et al: Induction of hypoxia and necrosis in multicellular tumor
spheroids is associated with resistance to chemotherapy treatment.
Oncotarget. 8:1725–1736. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhao W, Xia SQ, Zhuang JP, Zhang ZP, You
CC, Yan JL and Xu GP: Hypoxia-induced resistance to
cisplatin-mediated apoptosis in osteosarcoma cells is reversed by
gambogic acid independently of HIF-1α. Mol Cell Biochem. 420:1–8.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Qin Y, Roszik J, Chattopadhyay C,
Hashimoto Y, Liu C, Cooper ZA, Wargo JA, Hwu P, Ekmekcioglu S and
Grimm EA: Hypoxia-driven mechanism of vemurafenib resistance in
melanoma. Mol Cancer Ther. 15:2442–2454. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mao XG, Wang C, Liu DY, Zhang X, Wang L,
Yan M, Zhang W, Zhu J, Li ZC, Mi C, et al: Hypoxia upregulates HIG2
expression and contributes to bevacizumab resistance in
glioblastoma. Oncotarget. 7:47808–47820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ohtsuki T, Yawata Y, Wada H, Sugihara T,
Mori M and Namba M: Two human myeloma cell lines, amylase-producing
KMS-12-PE and amylase-non-producing KMS-12-BM, were established
from a patient, having the same chromosome marker,
t(11;14)(q13;q32). Br J Haematol. 73:199–204. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ikeyama S, Nakagawa S, Arakawa M, Sugino H
and Kakinuma A: Purification and characterization of IgE produced
by human myeloma cell line, U266. Mol Immunol. 23:159–167. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pastor N and Cortés F: Bufalin influences
the repair of X-ray-induced DNA breaks in Chinese hamster cells.
DNA Repair (Amst). 2:1353–1360. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wu SH, Hsiao YT, Chen JC, Lin JH, Hsu SC,
Hsia TC, Yang ST, Hsu WH and Chung JG: Bufalin alters gene
expressions associated DNA damage, cell cycle and apoptosis in
human lung cancer NCI-H460 cells in vitro. Molecules. 19:6047–6057.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wu SH, Wu TY, Hsiao YT, Lin JH, Hsu SC,
Hsia TC, Yang ST, Hsu WH and Chung JG: Bufalin induces cell death
in human lung cancer cells through disruption of DNA damage
response pathways. Am J Chin Med. 42:729–742. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li D, Zhou L, Huang J and Xiao X: Effect
of multidrug resistance 1/P-glycoprotein on the hypoxia-induced
multidrug resistance of human laryngeal cancer cells. Oncol Lett.
12:1569–1574. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhou C, Tan W, Lv H, Gao F and Sun J:
Hypoxia-inducible microRNA-488 regulates apoptosis by targeting Bim
in osteosarcoma. Cell Oncol (Dordr). 39:463–471. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chen YL, Yang TY, Chen KC, Wu CL, Hsu SL
and Hsueh CM: Hypoxia can impair doxorubicin resistance of
non-small cell lung cancer cells by inhibiting MRP1 and P-gp
expression and boosting the chemosensitizing effects of MRP1 and
P-gp blockers. Cell Oncol (Dordr). 39:411–433. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Feng H, Wang J, Chen W, Shan B, Guo Y, Xu
J, Wang L, Guo P and Zhang Y: Hypoxia-induced autophagy as an
additional mechanism in human osteosarcoma radioresistance. J Bone
Oncol. 5:67–73. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mohyeldin A, Garzón-Muvdi T and
Quiñones-Hinojosa A: Oxygen in stem cell biology: A critical
component of the stem cell niche. Cell Stem Cell. 7:150–161. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hoshino H, Nagano H, Haraguchi N,
Nishikawa S, Tomokuni A, Kano Y, Fukusumi T, Saito T, Ozaki M,
Sakai D, et al: Hypoxia and TP53 deficiency for induced pluripotent
stem cell-like properties in gastrointestinal cancer. Int J Oncol.
40:1423–1430. 2012.PubMed/NCBI
|
|
21
|
Li Z and Rich JN: Hypoxia and hypoxia
inducible factors in cancer stem cell maintenance. Curr Top
Microbiol Immunol. 345:21–30. 2010.PubMed/NCBI
|
|
22
|
Ma Y, Liang D, Liu J, Axcrona K, Kvalheim
G, Stokke T, Nesland JM and Suo Z: Prostate cancer cell lines under
hypoxia exhibit greater stem-like properties. PLoS One.
6:e291702011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kawano Y, Kikukawa Y, Fujiwara S, Wada N,
Okuno Y, Mitsuya H and Hata H: Hypoxia reduces CD138 expression and
induces an immature and stem cell-like transcriptional program in
myeloma cells. Int J Oncol. 43:1809–1816. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sun J, Xu K, Qiu Y, Gao H, Xu J, Tang Q
and Yin P: Bufalin reverses acquired drug resistance by inhibiting
stemness in colorectal cancer cells. Oncol Rep. 38:1420–1430. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wang H, Zhang C, Xu L, Zang K, Ning Z,
Jiang F, Chi H, Zhu X and Meng Z: Bufalin suppresses hepatocellular
carcinoma invasion and metastasis by targeting HIF-1α via the
PI3K/AKT/mTOR pathway. Oncotarget. 7:20193–20208. 2016.PubMed/NCBI
|
|
26
|
Xie CM, Liu XY, Yu S and Cheng CH: Cardiac
glycosides block cancer growth through HIF-1α- and NF-κB-mediated
Plk1. Carcinogenesis. 34:1870–1880. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jahanban-Esfahlan R, de la Guardia M,
Ahmadi D and Yousefi B: Modulating tumor hypoxia by nanomedicine
for effective cancer therapy. J Cell Physiol. 233:2019–2031. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yu T, Tang B and Sun X: Development of
inhibitors targeting hypoxia-inducible factor 1 and 2 for cancer
therapy. Yonsei Med J. 58:489–496. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Borsi E, Terragna C, Brioli A, Tacchetti
P, Martello M and Cavo M: Therapeutic targeting of hypoxia and
hypoxia-inducible factor 1 alpha in multiple myeloma. Transl Res.
165:641–650. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Bick RJ, Poindexter BJ, Sweney RR and
Dasgupta A: Effects of Chan Su, a traditional Chinese medicine, on
the calcium transients of isolated cardiomyocytes: Cardiotoxicity
due to more than Na, K-ATPase blocking. Life Sci. 72:699–709. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Liu M, Feng LX, Sun P, Liu W, Wu WY, Jiang
BH, Yang M, Hu LH, Guo DA and Liu X: A novel bufalin derivative
exhibited stronger apoptosis-inducing effect than bufalin in A549
lung cancer cells and lower acute toxicity in mice. PLoS One.
11:e01597892016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wu SH, Bau DT, Hsiao YT, Lu KW, Hsia TC,
Lien JC, Ko YC, Hsu WH, Yang ST, Huang YP and Chung JG: Bufalin
induces apoptosis in vitro and has antitumor activity against human
lung cancer xenografts in vivo. Environ Toxicol. 32:1305–1317.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Xie XB, Yin JQ, Wen LL, Gao ZH, Zou CY,
Wang J, Huang G, Tang QL, Colombo C, He WL, et al: Critical role of
heat shock protein 27 in bufalin-induced apoptosis in human
osteosarcomas: A proteomic-based research. PLoS One. 7:e473752012.
View Article : Google Scholar : PubMed/NCBI
|