Introduction
Total laryngectomy is an established, effective
treatment for locally advanced laryngeal cancer (1). However, it is a disfiguring procedure
that markedly alters the patient's post-operative quality of life.
The results of pilot studies have indicated that primary
non-surgical procedures, that is, neoadjuvant systemic cytostatic
chemotherapy followed by radiotherapy or concomitant
chemoradiotherapy, may be just as effective as surgery (1); this assumes that total laryngectomy is
available when conservative treatments fail. The benefit of these
procedures lies in the potential to preserve the larynx in a
relatively large proportion of patients (1,2). Primary
indications for non-surgical treatment (preservation protocols) and
total laryngectomy are presently very topical and a consensus has
not yet been reached.
Conventional treatment for advanced laryngeal cancer
(T3 and T4) with total laryngectomy, or total laryngectomy with
post-operative radiotherapy, is associated with significant patient
disfiguration (3). Permanent
tracheostomy, loss of a natural speaking voice and occasionally
dysphagia means that physicians continue to seek alternative
treatments to total laryngectomy, according to our opinion. Certain
advanced types of cancer that are managed with partial laryngectomy
or primary radiotherapy (with preservation of laryngeal function)
may achieve results similar to those of total laryngectomy.
However, primary radiotherapy is associated with lower patient
survival rates, particularly in more advanced disease states,
although salvage total laryngectomy remains a backup in cases of
radiotherapy failure (4). The results
of several studies suggest that patients with advanced cancer of
the larynx or hypopharynx with tumor regression following
neoadjuvant systemic cytostatic chemotherapy and subsequent
radiotherapy may be expected to have improved survival rates,
compared with those that undergo radiotherapy alone (5,6).
In 1985, the Veterans Affairs Medical Center
conducted a landmark prospective, multicenter, randomized study
(The VA Study) to determine whether neoadjuvant chemotherapy
followed by radiotherapy (with salvage total laryngectomy in the
case of treatment failure) was a more appropriate approach than
total laryngectomy with post-operative radiotherapy for patients
with advanced stage III and IV laryngeal cancer (1). The results revealed that, to preserve
the larynx without reducing overall patient survival, neoadjuvant
chemotherapy followed by radiotherapy may be effective for many
patients with advanced laryngeal cancer. This previous study
initiated a series of preservation protocols, which confirmed that
neoadjuvant chemotherapy followed by radiotherapy was an effective
alternative treatment for advanced laryngeal cancer (7). As a result, there was a subsequent
reduction in the number of total laryngectomies performed (8).
A second study, the Radiation Therapy Oncology Group
(RTOG) 91–11 study, was led by the RTOG and the Head and Neck
Intergroup. It aimed to determine the efficacy of chemotherapy and
radiotherapy in larynx-preserving treatments for advanced laryngeal
cancer (2). The RTOG 91–11 study
compared the effects of radiotherapy alone, neoadjuvant
chemotherapy followed by radiotherapy and concomitant
chemoradiotherapy. All treatment modalities were revealed to result
in comparable overall patient survival rates, with concomitant
chemoradiotherapy determined to be the most likely to preserve the
larynx. As such, concomitant chemoradiotherapy became the primary
alternative to total laryngectomy in the treatment of advanced
laryngeal cancer. Subsequently there was a decline in the use of
primary total laryngectomy treatment, and a shift toward reserving
it for salvage procedures in cases where primary non-surgical
treatments failed (9).
The present study analyzed treatment results of
advanced laryngeal cancer patients at the Royal Vinohrady Teaching
Hospital (RVTH) to assess whether they were consistent with the
aforementioned observations. The primary objective of the current
study was not to determine the percentage of laryngeal
preservations, but to determine what effect a departure from
primary total laryngectomy, for advanced laryngeal cancer, would
have on overall patient survival.
Materials and methods
Patients
Between January 1997 and December 2013, the Charles
University 3rd Medical School and RVTH Ear, Nose and Throat (ENT)
oncology team (Prague, Czech Republic) treated 185 patients (30
females, 155 males; mean age, 60.7±9.4 years; age range, 40–86
years) with advanced laryngeal cancer, which (from a surgical
perspective) required total laryngectomy. Written informed consent
was obtained from all patients prior to enrollment in the present
study and the study was approved by The Ethics Committee of The
Medical Faculty of Charles University. Patients with inoperable
disease or with poor overall health who were not candidates for
surgical treatment were excluded from the study. None of the
patients in the present sample group had tumors that were
manageable with partial laryngectomy. Any patient that had
previously treated head and neck cancer, or any duplicity, were
also excluded. Inclusion criteria were operable laryngeal cancer
between T2-T4 stages with a Karnofsky index >60% (10). In this retrospective analysis, the
sample was divided into patients who underwent total laryngectomy
and post-operative radiotherapy, and those who were treated
conservatively without primary surgery (for example by
radiotherapy, neoadjuvant systemic cytostatic chemotherapy followed
by radiotherapy, or concomitant chemoradiotherapy). Inclusion in
the surgical and non-surgical arms of the present study was
primarily based on the personal preference of the patient.
Patient analysis
Overall, ~70% of the patients (n=129) had undergone
conventional surgery [total laryngectomy with post-operative
radiotherapy (TL)], and ~30% (n=56) had been treated with larynx
preservation protocols (PP). The majority of patients had extensive
T4 tumors (41.6%) and stage IV disease (51.9%; Table I), as classified using the 2009 Union
for International Cancer Control Tumor Node Metastasis
Classification of Malignant tumors 7th edition (3).
 | Table I.Patient sample characteristics. |
Table I.
Patient sample characteristics.
| Variables | Total, n (%) | Primary surgical
treatment, n (%) | No surgery, n
(%) |
χ2-value | P-value |
|---|
| Extent |
|
|
| 37.690 | 0.001a |
| T2 | 38 (20.5) | 14 (10.8) | 24 (42.9) |
|
|
| T3 | 70 (37.8) | 45 (34.9) | 25 (44.6) |
|
|
| T4 | 77 (41.6) | 70 (54.3) | 7
(12.5) |
|
|
| Stage |
|
|
| 42.124 | 0.001a |
| II | 28 (15.1) | 7
(5.4) | 21 (37.5) |
|
|
| III | 61 (33.0) | 38 (29.5) | 23 (41.1) |
|
|
| IV | 96 (51.9) | 84 (65.1) | 12 (21.4) |
|
|
| Sex |
|
|
| 1.739 | 0.098 |
|
Female | 30
(16.2) | 17
(13.2) | 13
(23.2) |
|
|
| Male | 155 (83.8) | 112 (86.8) | 43 (76.8) |
|
|
| Local recurrence |
|
|
| 15.422 | 0.001a |
| No | 157 (84.9) | 118 (91.5) | 39 (69.6) |
|
|
| Yes | 28
(15.1) | 11
(8.5) | 17 (30.4) |
|
|
| Cervical nodal
recurrence |
|
|
| 0.423 | 0.515 |
| No | 175 (94.6) | 123 (95.3) | 52 (92.9) |
|
|
| Yes | 10
(5.4) |
6 (4.7) | 4
(7.1) |
|
|
Statistical analysis
The following statistical methods were used: The
nonparametric Mann-Whitney U-test was used to compare the effect of
age on treatment, the χ2 test of independence was used
to analyze the characteristics of the patient population (extent,
stage of disease, sex, local recurrence and nodal recurrence).
Kaplan-Meier survival analysis with the Mantel-Cox test of survival
functions between categories was performed. The data was presented
as the mean ± standard deviation. SPSS 13.0 statistical software
(SPSS, Inc., Chicago, IL, USA) was used for all statistical
analysis. P<0.05 was considered to indicate a statistically
significant difference.
Results
A total of 28 patients exhibited local recurrence
after treatment (15.1%). Of these 28, 11 local recurrences were
identified in primary surgical TL patients (8.5%), and 17/28
recurrences were present in primary non-surgical PP patients
(30.4%). In total, 14 patients who received preservation treatment
(25%) underwent a salvage total laryngectomy due to failed primary
non-surgical treatment. Cervical nodal recurrence was observed in
10 patients (5.4% of treated patients), of whom 6 (4.7%) were TL
patients and 4 (7.1%) PP patients.
Sex and age
The TL and PP groups were examined in an effort to
identify dependencies and differences among specified parameters
(sex, age, tumor extent, disease stage, local recurrence, cervical
nodal recurrence and 5-year survival rate). Primary surgery had
been performed on 56.7% of the females, and on 72.3% of the males
in the present study. Male patients underwent surgery more
frequently and this difference was not statistically significant
(P<0.100; Table I). The mean age
of PP patients was significantly higher than that of TL patients
(66 vs. 59 years, respectively; P<0.001; Table II).
 | Table II.Patient sample characteristics with
respect to age. |
Table II.
Patient sample characteristics with
respect to age.
| Surgical
treatmenta | Patients, n | Age,
yearsb |
|---|
| No | 56 |
65.68±11.02 |
| Yes | 129 |
58.58±7.76 |
Tumor extent and disease stage
Patients with relatively extensive tumors were more
frequently indicated for primary surgical treatment, a finding that
was statistically significant (P<0.001). In total, 54.3% of TL
patients had T4 tumors, whereas 12.5% of PP patients had T4 tumors
(Table I). There was also a
difference between the groups with respect to disease stage. Stage
IV disease was the diagnosis of 21.4% of PP patients, compared with
65.1% of TL patients. This difference was statistically significant
(P<0.001; Table I).
Local and cervical nodal
recurrence
Primary non-surgical patients had a significantly
higher frequency of locally recurrent laryngeal cancer
(P<0.001). Only 8.5% of TL patients experienced local
recurrence, compared with 30.4% of PP patients (Table I). The two patient groups had a low
frequency of recurrent cervical node metastases, and no
statistically significant differences were recorded relative to
this parameter (Table I).
Survival analyses
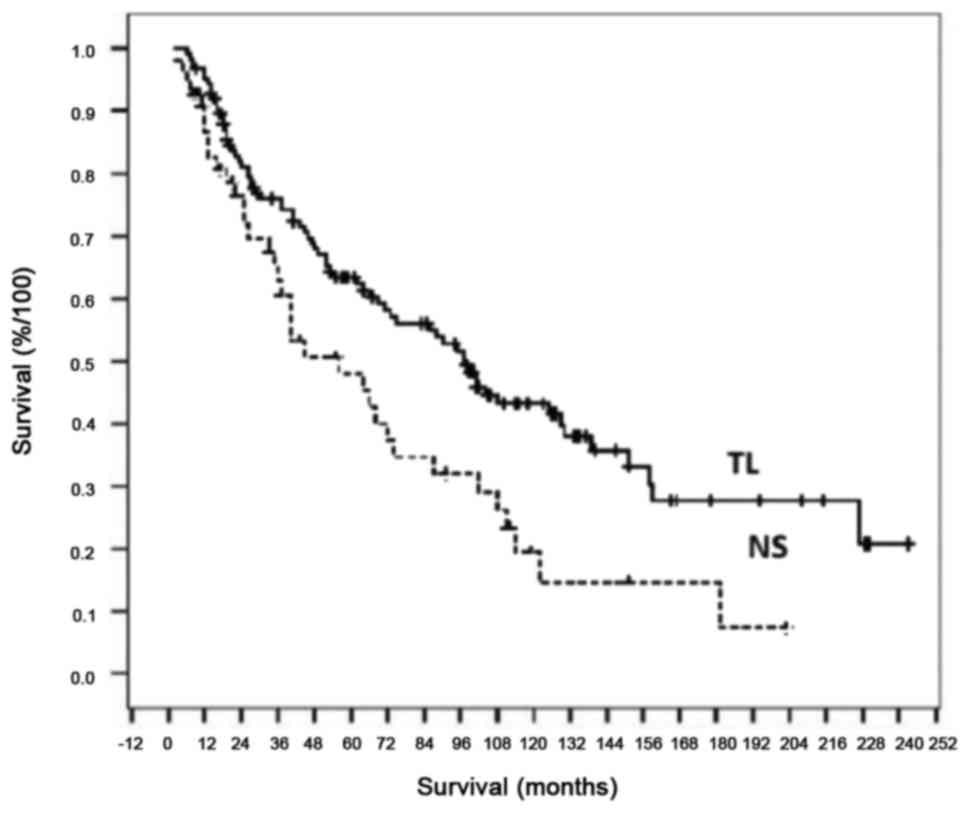
Kaplan-Meier survival analyses revealed that PP
patients had a 5-year survival probability of ~48%, whereas TL
patients had a 5-year survival probability of ~63% (Fig. 1). No statistically significant
difference was observed between the 2- and 5-year survival rates
(at the P<0.050 significance level), regardless of whether
patients underwent primary surgical or non-surgical treatment. TL
patients exhibited a statistically significant longer survival
(P<0.010) compared with PP patients.
An overview of survival analyses in association with
the studied parameters (sex, age, tumor extent, disease stage,
local recurrence and cervical nodal relapse) is presented for TL
and PP patients in Tables III and
IV, respectively. The data
demonstrate that survival is particularly affected by local and
cervical node disease recurrence in TL patients (P<0.001), and
by recurrent local carcinoma in PP patients (P<0.100).
Kaplan-Meier survival analyses confirmed that sex did not affect
the probability of survival. Male and female patients treated for
laryngeal cancer that, according to standard indications, required
total laryngectomy had a 5-year survival probability of ~60%,
irrespective of treatment approach.
 | Table III.Kaplan-Meier survival analysis of the
primary surgical treatment group and the Mantel-Cox test between
categories of individual, and possibly dependent, parameters. |
Table III.
Kaplan-Meier survival analysis of the
primary surgical treatment group and the Mantel-Cox test between
categories of individual, and possibly dependent, parameters.
| Group | Patients, n | Mortalities, n | Survival Rate, % | Median | Mantel-Cox
Z-value | P-value |
|---|
| Sex |
|
|
|
| 1.286 | 0.257 |
|
Female | 17 | 6 | 64.7 | 158.0 |
|
|
| Male | 112 | 64 | 42.9 | 95.0 |
|
|
| Age, years |
|
|
|
| 3.828 | 0.148 |
| ≤50 | 20 | 12 | 40.0 | 108.0 |
|
|
|
51–70 | 99 | 49 | 50.5 | 99.0 |
|
|
|
>70 | 10 | 8 | 20.0 | 47.0 |
|
|
| Tumor extent |
|
|
|
| 2.791 | 0.248 |
| T2 | 14 | 6 | 57.1 | 158.0 |
|
|
| T3 | 45 | 24 | 46.7 | 101.0 | 7.317 | 0.026a |
| T4 | 70 | 39 | 44.3 |
71.0 |
|
|
| Disease stage |
|
|
|
| 3.020 | 0.221 |
| II | 7 | 3 | 57.1 | 158.0 |
|
|
|
III | 38 | 20 | 47.4 | 125.0 | 7.110 | 0.026a |
| IV | 84 | 46 | 45.2 |
75.0 |
|
|
| Local
recurrence |
|
|
|
| 35.125 | 0.001a |
| No | 118 | 59 | 50.0 | 101.0 |
|
|
|
Yes | 11 | 10 |
9.1 |
14.0 |
|
|
| Cervical
nodalrecurrence |
|
|
|
| 46.474 | 0.001a |
| No | 123 | 63 | 48.8 | 101.0 |
|
|
|
Yes | 6 | 6 |
0.0 |
14.0 |
|
|
 | Table IV.Kaplan-Meier survival analysis of the
laryngeal cancer patients in the primary non-surgical treatment
group and the Mantel-Cox test between categories of individual,
possibly dependent, parameters. |
Table IV.
Kaplan-Meier survival analysis of the
laryngeal cancer patients in the primary non-surgical treatment
group and the Mantel-Cox test between categories of individual,
possibly dependent, parameters.
| Group | Patients, n | Mortalities, n | Survival rate,
% | Median |
Mantel-CoxZ-value | P-value |
|---|
| Sex |
|
|
|
| 0.203 | 0.652 |
|
Female | 13 | 7 | 46.2 | 45.0 |
|
|
|
Male | 43 | 30 | 30.2 | 56.0 |
|
|
| Age, years |
|
|
|
| 2.164 | 0.339 |
|
≤50 | 3 | 1 | 66.7 |
|
|
|
|
51–70 | 33 | 20 | 39.4 | 64.0 |
|
|
|
>70 | 20 | 16 | 20.0 | 40.0 |
|
|
| Tumor extent |
|
|
|
| 3.887 | 0.143 |
| T2 | 24 | 13 | 45.8 | 68.0 |
|
|
| T3 | 25 | 19 | 24.0 | 40.0 |
|
|
| T4 | 7 | 5 | 28.6 | 25.0 |
|
|
| Disease stage |
|
|
|
| 2.831 | 0.243 |
| II | 21 | 12 | 42.9 | 68.0 |
|
|
|
III | 23 | 17 | 26.1 | 40.0 |
|
|
| IV | 12 | 8 | 33.3 | 56.0 |
|
|
| Local
recurrence |
|
|
|
| 3.624 | 0.057 |
| No | 39 | 23 | 38.5 | 66.0 |
|
|
|
Yes | 17 | 13 | 23.5 | 25.0 |
|
|
| Cervical nodal
recurrence |
|
|
|
| 1.515 | 0.218 |
| No | 52 | 34 | 34.6 | 56.0 |
|
|
|
Yes | 4 | 3 | 25.0 | 19.0 |
|
|
Patients >71 years of age had a significantly
lower 5-year survival probability (~35%) than younger patients
(>60%; P<0.010). The highest 5-year survival probability was
observed in patients with the least extensive tumors (T2, ≤75%; T3,
~62%, T4, ~50%); however, these differences were not statistically
significant. Disease stage also affected 5-year survival
probability. Irrespective of the treatment method, 5-year survival
probability was ~75% in patients with stage II, 65% in patients
with stage III, and 55% in patients with stage IV disease; however,
these differences were not statistically significant.
Local disease recurrence had a marked effect on
5-year survival probability. Regardless of treatment approach,
patients without local recurrence had a 5-year survival probability
of ~70%, whereas patients with local recurrence had a 5-year
survival probability of only 20%, a significant difference
(P<0.001). Recurrent cervical node metastases had a major effect
on patient survival. Irrespective of treatment method, laryngeal
cancer patients without cervical node recurrence had a 5-year
survival probability of 65%, where as that of patients with
cervical nodal recurrence was <20%, a significant difference
(P<0.001).
An evaluation of the entire patient cohort indicated
that the treatment method affected survival probability, and that
TL patients survived significantly longer (P<0.010). The median
survival time (the period during which at least 50% of patients are
alive) was 97 months (>8 years) for TL patients, but only 56
months (<5 years) for PP patients. Survival probabilities were
significantly different for various age groups (patients >70
years survived the treatments for a significantly shorter period;
P<0.010), those that exhibited local recurrence vs. those that
did not (P<0.001) and those that exhibited cervical node
recurrence vs. those that did not (P<0.001; Table V).
 | Table V.Complete overview: Kaplan-Meier
survival analysis for the entire patient sample and the Mantel-Cox
test between categories of individual, possibly dependent,
parameters. |
Table V.
Complete overview: Kaplan-Meier
survival analysis for the entire patient sample and the Mantel-Cox
test between categories of individual, possibly dependent,
parameters.
| Group | Patients, n | Mortalities, n | Survival Rate,
% | Median | Mantel-Cox
Z-value | P-value |
|---|
| Surgical
treatment |
|
|
|
| 7.585 | 0.006 |
| No | 56 | 37 | 33.9 | 56.0 |
|
|
|
Yes | 129 | 70 | 45.7 | 97.0 |
|
|
| Sex |
|
|
|
| 0.553 | 0.457 |
|
Female | 30 | 13 | 56.7 | 122.0 |
|
|
|
Male | 155 | 94 | 39.4 |
74.0 |
|
|
| Age |
|
|
|
| 10.244 | 0.006 |
|
≤50 | 23 | 13 | 43.5 | 108.0 |
|
|
|
51–70 | 132 | 69 | 47.7 |
90.0 |
|
|
|
>70 | 30 | 24 | 20.0 |
45.0 |
|
|
| Tumor extent |
|
|
|
| 1.752 | 0.416 |
| T2 | 38 | 19 | 50.0 | 111.0 |
|
|
| T3 | 70 | 43 | 38.6 |
88.0 |
|
|
| T4 | 77 | 45 | 41.6 |
54.0 |
|
|
| Disease stage |
|
|
|
| 1.038 | 0.595 |
| II | 28 | 15 | 46.4 | 111.0 |
|
|
|
III | 61 | 37 | 39.3 |
88.0 |
|
|
| IV | 96 | 55 | 42.7 |
62.0 |
|
|
| Local
recurrence |
|
|
|
| 38.656 | 0.001 |
| No | 157 | 82 | 47.8 | 99.0 |
|
|
|
Yes | 28 | 24 | 14.3 | 24.0 |
|
|
| Cervical node
recurrence |
|
|
|
| 28.399 | 0.001 |
| No | 175 | 97 | 44.6 | 90.0 |
|
|
|
Yes | 10 | 9 | 10.0 | 15.0 |
|
|
To determine which of the chosen parameters most
significantly affected survival, stepwise Cox regression analysis
was used to examine sex, patient age, tumor extent, disease stage,
choice of primary treatment, local recurrence and cervical node
recurrence. From these analyses, recurrence was selected at the
first step as the parameter that most affected survival
(P<0.001), age >70 years was selected at the second step
(P<0.001), cervical node recurrence was selected at the third
step (P<0.001) and disease stage was selected at the fourth step
(P<0.010). The remaining parameters did not have a statistically
significant impact on survival.
Discussion
The analyses of the present study differed
fundamentally from the aforementioned VA and RTOG 91–11 studies
(1,2),
in that the current study was not a prospective randomized
multicenter one, but rather a retrospective study based on the
experience of one center. The present cohort included patients with
laryngeal cancer who, from a surgical view point, would normally
require total laryngectomy. Overall patient health and disease
extent governed the recommendations of the ENT oncology team (i.e.,
T4 tumors were recommended for surgical management). As such, the
patient representation in the two study groups contained a bias
that would be in admissible in a prospective randomized study.
Patient samples
The present study included 185 patients with
advanced cancer; 129 of these patients underwent primary surgical
treatment and 56 underwent primary non-surgical treatment in an
effort to preserve the larynx. The VA study was based on an
evaluation of 332 patients; ~50% of these patients were in the
surgical group (i.e., treated with total laryngectomy and
post-operative radiotherapy), while the remaining half were
assigned to the non-surgical group. The primary non-surgical
treatment group of the present study consisted of patients treated
with: i) Neoadjuvant systemic chemotherapy according to the VA
study protocol; ii) patients treated with concomitant
chemoradiotherapy according to the RTOG 91–11 study protocol; iii)
patients treated with radiotherapy alone. The merging of these
different patient groups into one was based on the outcome of the
RTOG 91–11 study, which identified no statistically significant
difference in overall survival between the three types of
treatment. The RTOG 91–11 study evaluated 518 patients.
The mean patient age in the present study was 60.7
years, with a median age of 60 years. This was very similar to the
mean patient ages in the VA study (mean age, 62 years) and in the
RTOG 91–11 study, which had a median age of 59 years for patients
treated with radiotherapy or neoadjuvant chemotherapy, and a median
age of 60 years for patients treated with concomitant
chemoradiotherapy. In contrast to these two randomized prospective
studies, the present RVTH patient sample had a statistically
significant age difference between patients in the surgical (mean
age, 58.6 years) and non-surgical (mean age, 65.7 years) treatment
groups. Thus, younger patients were more often recommended for
surgery.
Regarding gender distribution, the present study
included 155 males (84%) and 30 females (16%), the VA study
included 321 males (97%) and 11 females (3%) and the RTOG 91–11
study included 401 males (77%) and 117 females (23%). The VA study
had a significantly lower representation of female patients. Given
that no statistically significant difference in the overall
survival of males and females was identified in the RVTH sample,
the variation in the number of males and females among the studies
was not considered significant.
The inclusion criteria for the VA study protocol
included stage III or IV laryngeal cancer with a Karnofsky index of
>50. Patients with T1N1 tumors and inoperable tumors were
excluded, as were patients with distant metastasis or a history of
prior radiotherapy to the head and neck region. The majority of
patients had stage III supraglottic cancer.
None of the patients in the present sample group had
tumors that were manageable with partial laryngectomy, unlike the
VA study. The non-surgical study arm of the current study was
mostly represented by patients with stage III cancer and T3 tumor
extension. Of the surgically treated patients, the majority had
stage IV cancer with T4 extension. This reflects the strategy to
recommend patients with advanced tumors for surgery. In contrast to
the VA study, the present patient sample also included patients at
stage II with T2 tumors (particularly in the non-surgical group).
This stems from the understanding that even T2 laryngeal tumors can
sometimes require surgical management with total laryngectomy.
Furthermore, the RVTH ENT oncology team strictly adhered to the
Union for International Cancer Control (UICC) recommendations.
Therefore, if doubts exist regarding the TNM classification, the
lower category (less advanced) is selected (6). It is, therefore, possible that a large
number of T2 laryngeal cancer cases in the present patient cohort
may have been classified as T3 at a different treatment center.
The majority of patients had T3 supraglottic cancer
without vocal cord fixation (N0, stage III) in the RTOG 91–11
study. The RTOG 91–11 study also had the inclusion criterion of
stage III or IV laryngeal cancer with a Karnofsky index of >60,
and excluded synchronous duplicate tumors. Tumors with T1 extension
and (unlike the present patient sample) T4 tumors with extension
through the thyroid cartilage or a >1 cm extension into the base
of the tongue were excluded.
Study outcomes
In the VA study non-surgical treatment group, 64% of
patients had a preserved larynx two years following treatment.
Total laryngectomy was required in 7% of patients owing to late
tumor recurrence (>3 months after treatment), 80% of which
occurred during the first-year post-treatment. Salvage laryngectomy
was performed in 29% of patients owing to disease persistence
following chemotherapy, or within three months of the conclusion of
radiotherapy. A greater frequency of local recurrence was observed
in tumors with glottis localization, tumors with vocal cord
fixation, and thyroid cartilage invasion; however, these factors
did not affect the statistical significance of local recurrence.
Salvage total laryngectomy was performed significantly more often
in stage IV cancer cases with a T4 extension. Subsequent
stand-alone block dissection was only performed in 10 patients.
Local disease recurrence occurred significantly less often in the
surgical study arm (2 vs. 12% in the non-surgical arm, P<0.001).
Cervical node recurrence was observed in 5% of patients in the
surgical arm and in 8% of patients in the chemotherapy groups,
though this difference was not statistically significant.
Similarly, local disease recurrence occurred
statistically significantly more often in the non-surgical
treatment group of the present study (30.4 vs. 8.5%; P<0.001),
although in contrast to the VA study, the division of tumor
extension and stage was not symmetrical (i.e., the surgical group
had more patients with T4 tumors and stage IV disease). This
implies that surgical management has an unambiguously positive
impact in the prevention of local recurrence. In total, 17 patients
in the non-surgical treatment group of the present study had local
recurrences, of which 14 (82.4%) underwent a salvage total
laryngectomy. Of the remaining three patients, one patient refused
salvage laryngectomy and two were inoperable owing to the overall
poor health of the patients (one patient had suffered an acute
myocardial infarction, and one patient had suffered a severe
cerebrovascular accident). Cervical node recurrence was diagnosed
in 4.7% of the patients in the primary surgical treatment group,
and in 7.1% of the primarily non-surgical treatment group, which
was not a statistically significant difference. As with the VA
study, ~66% of non-surgical treatment patients in the present study
had a preserved larynx. In contrast to the VA study, however,
one-third of the patients of the present study had stage II disease
or, more precisely, were borderline between stage II and III.
However, the non-surgical approach was burdened by a higher risk of
recurrence.
The RTOG 91–11 study, which compared the efficacy of
non-surgical treatment for the entire sample, achieved a 2-year
patient survival rate of 65% without total laryngectomy. The 2-year
survival rates with larynx preservation were: 88% in patients
treated with concomitant chemoradiotherapy; 75% in patients treated
with induction chemotherapy; 70% in patients treated with
radiotherapy alone. Successful concomitant chemoradiotherapy was
significantly better for laryngeal preservation than induction
chemotherapy or radiotherapy alone. In terms of larynx
preservation, no significant difference was observed between the
efficacy of induction chemotherapy and radiotherapy alone. The
conclusions of the RTOG 91–11 study demonstrated that primary
non-surgical treatment may save the larynx in ~66% of patients with
locally-advanced laryngeal cancer. In this respect, concomitant
chemoradiotherapy is the most efficacious approach. Since induction
chemotherapy does not produce (in terms of laryngeal preservation)
better results than radiotherapy alone, if chemoradiotherapy is not
possible then radiotherapy alone without chemotherapy is
indicated.
Analysis and comparison of the
studies
The fundamental parameter of cancer treatment
assessed in the present study was overall patient survival.
Analyses of the patient sample of the present study indicate that
treatment method significantly affects patient survival. TL
patients survived significantly longer than patients with PP
patients (P<0.010). The 2-year survival probability of PP
patients was 75 vs. 82% in TL patients and the 5-year survival
probability was 48% in PP patients vs. 63% in TL patients. However,
the difference between 2- and 5-year survival rates was not
determined to be significant in either group. In TL patients,
survival was affected by the pre-operative parameters of tumor
extent and disease stage (P<0.05), as well as the post-operative
parameters of local recurrence and cervical node recurrence
(P<0.001). In PP patients, none of the pre-treatment parameters
(sex, age, tumor extent and disease stage) were determined to
significantly affect survival. The post-treatment parameter local
recurrence was revealed to have a no statistically significant
impact (P<0.100).
Analysis of the entire patient sample of the current
study identified that pre-treatment parameters, treatment method
and patient age, had a significant impact on the survival of
patients with advanced laryngeal cancer (P<0.010); however, the
post-treatment parameters local and cervical node recurrence were
even more significant (P<0.001). Analyses of the patient samples
of the current study suggested that primary non-surgical treatment
could be used to save the larynx in ~66% of patients, but it is
burdened with a higher risk of local recurrence, and negatively
impacts patient survival (P<0.01); however, it did not
statistically significantly affect the 2- and 5-year survival
rates.
In the VA study, the 2-year survival probability for
total laryngectomy patients and primary non-surgical treatment
patients was identical (68%) and therefore was similar to (or
slightly worse than) the sample of the current study (82 and 75%,
respectively). In the RTOG 91–11 study, the 2-year survival
probability was 76% for patients in the induction chemotherapy
group, 74% in the chemoradiotherapy group and 75% in the
radiotherapy alone group. The respective 5-year survival
probabilities for these groups were 55, 54 and 56%, with no
significant difference between them. These results are comparable
with the previous two samples. Analysis from the RTOG 91–11 study
revealed that none of the primary conservative treatment methods
improved overall patient survival and that the incorporation of
chemotherapy improved larynx preservation only in form
chemoradiotherapy. Since induction chemotherapy did not increase
likelihood of larynx preservations compared with radiotherapy
alone, the method of choice was to include chemotherapy as part of
a chemoradiotherapy regimen. On the basis of the results of the
present study, platinum-based induction chemotherapy alone is not
appropriate.
Analyses of the sample of the present study
confirmed the conclusions of the VA and RTOG 91–11 pilot studies,
which identified that primary non-surgical treatment of advanced
laryngeal cancer may save the larynx in ~66% of patients. However,
the present analyses also confirmed that primary non-surgical
treatment has a significantly higher risk of local recurrence.
Although no statistically significant difference was observed
between 2 and 5-year survival rates (in agreement with the VA
study), primary non-surgical treatment impaired overall patient
survival (11). The results of the
analysis of the present study must be viewed as the results of a
retrospective, non-randomized study. The primary surgical treatment
group included younger patients with more extensive tumors and a
higher disease stage. However, the present study did confirm that
primary non-surgical treatment is an alternative approach to total
laryngectomy. Conversely, salvage total laryngectomy is an integral
component of the larynx preservation protocol (primary non-surgical
treatment of advanced resectable laryngeal cancer). The final
decision regarding treatment approach should be left to the
patient. Nonetheless, the reduced patient survival rate,
particularly for more extensive tumors and in younger individuals,
means that primary surgical treatment should be recommended in
similar cases. If a patient opts for primary non-surgical
treatment, the indicated treatment is concomitant
chemoradiotherapy, which is currently based on the results of the
RTOG 91–11 study. If a patient is unable to undergo chemotherapy,
they should undergo radiotherapy alone; the administration of
platinum-based systemic cytostatic induction chemotherapy is not
considered justifiable. However, there is little doubt that the
addition of novel cytostatic drugs such as taxanes and biological
therapies such as cetuximab to induction chemotherapy may lead to
its renaissance (12). The toxicity
of platinum-based chemoradiotherapy is substantial and many
patients are unable to complete the prescribed chemotherapy or
radiotherapy treatments. It is likely that primary non-surgical
treatment combinations will vary in the future, depending on
results from new, randomized, multicenter, prospective studies such
as EORTC 24954 or TREMPLIN (13–15).
When deciding on treatment methods, it is also
necessary to consider that, although primary non-surgical treatment
approach can save the larynx in ~66% of patients, the preserved
larynx may not be fully functional. Some patients with laryngeal
preservation following primary non-surgical treatment who do not
present with loco regional recurrence may nonetheless require
tracheostomy, or even gastrostomy, for dysphagia. This reality adds
further complications to the choice of laryngeal preservation
protocols (16).
A patient sample treated by the RVTH ENT oncology
team between 1997 and 2013 was divided into those that received
conventional treatment (i.e., total laryngectomy and post-operative
radiotherapy), and those treated with laryngeal preservation
protocols (i.e., chemoradiotherapy, neoadjuvant cytostatic
chemotherapy followed by radiotherapy, or radiotherapy alone, and,
in the event of non-surgical treatment failure, possible subsequent
total laryngectomy). The aim of the present study was to compare
both groups in an effort to prove or refute the findings of the VA
and RTOG 91–11 pilot studies: That primary non-surgical treatment
of locally advanced laryngeal cancer does not reduce the likelihood
of patient survival, and may preserve a functional larynx in ~66%
of patients. The 2-year survival probability of primary
non-surgical patients was 75%, and the 5-year survival probability
was 48%. In primary surgical patients, the 2-year survival
probability was 82% and the 5-year survival probability was 63.
However, this difference was not identified to be statistically
significant. The present study confirmed that primary non-surgical
treatment can save the larynx in approximate two-thirds of
patients, but also identified that primary non-surgical treatment
is burdened with a higher risk of local recurrence and a poorer
overall survival rate (P<0.010).
In conclusion, the current study confirmed that
primary non-surgical treatment is an alternative approach to total
laryngectomy. Conversely, salvage total laryngectomy remains an
integral component of laryngeal preservation protocols. The final
decision regarding treatment approach should be left to the
informed patient. A decreased overall survival rate, particularly
in more extensive tumors and in younger patients, means that
surgical treatment is recommended in these cases. If a patient opts
for primary non-surgical treatment, it should be based on the RTOG
91–11 study results, which call for concomitant chemoradiotherapy.
If the patient is unable to undergo cytostatic chemotherapy,
radiotherapy alone should be used. The administration of
platinum-based systemic cytostatic induction chemotherapy is not
considered justified.
References
|
1
|
The Department of Veterans Affairs
Laryngeal Cancer Study Group, . Wolf GT, Fisher SG, Hong WK,
Hillman R, Spaulding M, Laramore GE, Endicott JW, McClatchey K and
Henderson WG: Induciton chemotherapy plus radiation compared with
surgery plus radiation in patients with advanced laryngeal cancer.
N Engl J Med. 324:1685–1690. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Forastiere AA, Goepfert H, Maor M, Pajak
TF, Weber R, Morrison W, Glisson B, Trotti A, Ridge JA, Chao C, et
al: Concurrent chemotherapy and radiotherapy for organ preservation
in advanced laryngeal cancer. N Engl J Med. 349:2091–2098. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
International Union Against Cancer (UICC):
TNM Classification of Malignant Tumours. Sobin LH, Gospodarowicz MK
and Wittekind C: 7th edition. Wiley-Blackwell; New York, NY:
2009
|
|
4
|
Harris HS Jr, Watson FR and Spratt JS Jr:
Carcinoma of the larynx: A retrospective study of 144 cases. Am J
Surg. 118:674–684. 1969. View Article : Google Scholar
|
|
5
|
Demard F, Chauvel P, Santini J, Vallicioni
J, Thyss A and Schneider M: Response to chemotherapy as
justification for modification of the therapeutic strategy for
pharyngolaryngeal carcinomas. Head Neck. 12:225–231. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Karp D, Carter R and Vaughan C: Voice
preservation using induction chemotherapy plus radiation therapy as
an alternative to laryngectomy in advanced head and neck cancer:
Long term follow-up. Proc Am Soc Clin Oncol. 7:1521988.
|
|
7
|
Forastiere AA, Weber RS and Trotti A:
Organ preservation for advanced larynx cancer: Issues and outcomes.
J Clin Oncol. 33:3262–3268. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Klozar J, Cada Z and Koslabova E:
Complications of total laryngectomy in the era of chemoradiation.
Eur Arch Otorhinolaryngol. 269:289–293. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Weber RS, Berkey BA, Forastiere A, Cooper
J, Maor M, Goepfert H, Morrison W, Glisson B, Trotti A, Ridge JA,
et al: Outcome of salvage total laryngectomy following organ
preservation therapy: The radiation therapy oncology group trial
91–11. Arch Otolaryngol Head Neck Surg. 129:44–49. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Karnofsky David A, Abelmann WH, Craver LF
and Joseph Burchenal H: The use of the nitrogen mustards in the
palliative treatment of carcinoma-with particular reference to
bronchogenic carcinoma. Cancer. 1:634–656. 1948. View Article : Google Scholar
|
|
11
|
Megwalu UC and Sikora AG: Survival
outcomes in advanced laryngeal cancer. JAMA Otolaryngol Head Neck
Surg. 140:855–860. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mesía R, Garcia-Saenz JA, Lozano A, Pastor
M, Grau JJ, Martínez-Trufero J, Lambeaz J, Martínez-Galán J, Mel
JR, González B, et al: Could the addition of cetuximab to
conventional radiation therapy improve organ preservation in those
patients with locally advanced larynx cancer who respond to
induction chemotherapy? An organ preservation spanish head and neck
cancer cooperative group phase 2 study. Int J Radiat Oncol Biol
Phys. 97:473–480. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fayette J, Pointreau Y, Bourhis J and
Lefebvre JL: Squamous cell carcinoma of the hypopharynx and larynx:
Evidence-based care. Bull Cancer. 101:438–444. 2014.(In French).
PubMed/NCBI
|
|
14
|
Lefebvre JL, Pointreau Y, Rolland F,
Alfonsi M, Baudoux A, Sire C, de Raucourt D, Malard O, Degardin M,
Tuchais C, et al: Induction chemotherapy followed by either
chemoradiotherapy or bioradiotherapy for larynx preservation: The
TREMPLIN randomized phase II study. J Clin Oncol. 31:853–859. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lefebvre JL, Rolland F, Tesselaar M,
Bardet E, Leemans CR, Geoffrois L, Hupperets P, Barzan L, de
Raucourt D, Chevalier D, et al: EORTC head and neck cancer
cooperative group; EORTC radiation oncology group: Phase 3
randomized trial on larynx preservation comparing sequential vs.
alternating chemotherapy and radiotherapy. J Natl Cancer Inst.
101:142–152. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Theunissen EA, Timmermans AJ, Zuur CL,
Hamming-Vrieze O, de Boer Paul J, Hilgers FJ and van den Brekel MW:
Total laryngectomy for a dysfunctional larynx after
(chemo)radiotherapy. Arch Otolaryngol Head Neck Surg. 138:548–555.
2012. View Article : Google Scholar : PubMed/NCBI
|