Introduction
Endometriosis is a complicated and chronic disease
that has been debated for decades. Although it is known to be
estrogen dependent and an estrogen-inhibiting therapy has been
identified to be beneficial, the exact etiopathology of
endometriosis is, at present, not clear (1,2).
Gonadotropin-releasing hormone agonist and gestrinone are able to
suppress the ectopic growth of endometrial tissue and are
frequently used to treat endometriosis (3). However, these hormone drugs are
associated with high recurrence rates and side effects, which limit
their long-term use (4). There has
been no optimal treatment method for endometriosis so far.
Although endometriosis is not a malignant disease,
it has been reported that endometriosis and ovarian cancer are
associated at the molecular level (5). The association between endometriosis and
cancer is a matter of growing concern (6). With the progress of endometriosis
research, histological, biochemical and epidemiological studies
have identified the features of endometriosis as a precursor lesion
of ovarian cancer (7–14). Genetic research has also identified
gene mutations directly associated with neoplasms in endometriotic
lesions, including the AT-rich interaction domain 1A, KRAS,
p53 and phosphatase and tensin homolog genes (15).
Endometrioid adenocarcinoma and clear cell
adenocarcinoma are the two most common pathological types of cancer
resulting from the malignant transformation of endometriosis
(16). Cisplatin (CDDP) is the most
widely used drug in the treatment of ovarian cancer and endometrial
carcinoma. CDDP-based chemotherapy is the preferred method against
these cancer types (17–19). The anti-neoplastic activity of CDDP is
a result of its binding to DNA in target cells to induce DNA
cross-links (20). CDDP was also
demonstrated to induce the downregulation of parkin-like
cytoplasmic protein and apoptosis in the target cells through a
p53-associated pathway; this is hypothesized to be associated with
its anti-neoplastic mechanism (21).
To the best of our knowledge there has been no study
conducted to demonstrate the effects of CDDP in an endometriosis
rat model. Therefore, the aim of the present study was to
investigate the effects of CDDP on endometriotic tissue and the
expression of proliferation- and angiogenesis-associated proteins
in a rat model of endometriosis.
Materials and methods
Mouse model
A total of 36 female Sprague-Dawley rats maintained
in a specific pathogen-free (SPF) facility (8 weeks old and
weighing 200–235 g) were purchased from Peking Union Medical
College and the Institute of Laboratory Animal Science, Chinese
Academy of Medical Science (Beijing, China). The rats were
sacrificed using abdominal aortic bleeding. The present study was
approved by the Institutional Animal Care and Use Committee of the
Institute of Laboratory Animal Science, and the research was
conducted in accordance with the institutional guidelines (22). All the rats were caged in pairs in a
SPF facility, temperature 20–26°C, relative humidity 40–70%, with a
12-h light/dark cycle and ad libitum access to food and
water (23).
Experimental procedures and tissue
collection
All the rats underwent three consecutive surgical
procedures. The rats were anesthetized via intraperitoneal
administration of 3% pentobarbital sodium (Sigma-Aldrich; Merck
KGaA, Darmstadt, Germany) at a dose of 35 mg/kg.
Procedure 1
In order to observe the estrous cycles of rats,
vaginal smears were obtained and subject to Papanicolaou staining,
as previously described (24). When
the rat was in estrus, endometriosis was surgically induced
according to the method described by Körbel et al with
slight modifications (25). Under
aseptic conditions, the rat's abdominal skin was shaved and a
ventral midline incision ~5 cm long was created to open the
abdominal cavity. The left uterine horn was ligated and excised,
and the excised uterine horn was placed in normal saline. The
serosal (outer) layer of the excised segment was removed, and the
uterine segment was trimmed into a 5×5 mm2 piece. Next,
the endometrial piece was sutured to the inner side of the
abdominal wall, with the endometrial surface facing the peritoneal
cavity. Finally, the abdominal muscles and skin were sutured.
Procedure 2
Following the surgical induction of endometriosis,
all rats were allowed to recover for 4 weeks, during which period
they were not administered any medication. All 36 animals survived.
A second exploratory laparotomy was performed on each rat to
observe the growth of the endometriotic implants. The peritoneal
cavity was irrigated with 5 ml normal saline. The peritoneal fluid
obtained was centrifuged at 1,000 × g for 20 min at room
temperature and the solution obtained was stored at −20°C. The
surface areas of the implants were measured (length [mm] × width
[mm]). The endometriotic lesions were photographed, and the lesion
sizes were recorded. Finally, the peritoneal cavity was closed.
Procedure 3
All rats were allowed to rest for three days
following the second procedure. The 36 rats were then randomly
divided into three groups of twelve rats each. There was no
significant difference in the area of the implants between the
groups prior to the treatment (Table
I). The rats in Group 1 (n=12) served as controls and were
administered 1 ml of normal saline daily via peritoneal perfusion.
The rats in Group 2 (n=12) were administered 35 mg/m2
CDDP via peritoneal perfusion every 4 days. The rats in Group 3
(n=12) were administered 70 mg/m2 CDDP via peritoneal
perfusion every 4 days. The skin surface areas of the rats were
measured using the Meeh-Rubner equation A=Kx
(W2/3/10000), where A is the skin surface area
(m2), the K value is 9.1 for rats, and W is the body
weight (g) (26). CDDP in the powder
form (Sigma-Aldrich; Merck KGaA) was crushed and dissolved in
normal saline. All rats were treated for a total of 24 days, which
was equivalent to 6 estrous cycles. A total of 4 days after the
final treatment, a third laparotomy was performed. The rats were
anesthetized with 3% pentobarbital sodium (50 mg/kg), and the
abdominal cavity was opened. Then, the implants were measured
(length [mm] × width [mm]) and photographed. The peritoneal cavity
was then irrigated with 5 ml normal saline and the peritoneal fluid
obtained was centrifuged at 1,000 × g for 20 min at room
temperature, and the solution was stored at −20°C. Finally, the
implants were excised, and a portion of the endometriotic implant
was fixed in formalin for histopathological examination and
immunohistochemistry (IHC). The remainder of the endometriotic
implant was fixed in liquid nitrogen and stored at −80°C for
further analyses.
 | Table I.Treatment results and comparisons of
the study groups. |
Table I.
Treatment results and comparisons of
the study groups.
| Measures | Group 1
(control) | Group 2 (35
mg/m2 CDDP) | Group 3 (70
mg/m2 CDDP) | P-value |
|---|
| Number of rats | 12 | 12 | 12 |
|
| Mean surface area
of implants (mm2) |
| Prior to
medication | 38.17±8.61 | 36.08±6.89 | 37.92±4.72 | 0.89 |
| Following
medication | 47.08±8.27 | 18.67±2.99 | 6.50±2.01 | 0.01 |
| Histopathological
score of implants |
2.50±0.67 |
1.67±0.65 | 0.90±0.57 | 0.01 |
| VEGF level in
peritoneal fluid (pg/ml) |
| Prior to
medication | 278.33±19.90 | 289.37±12.30 | 275.16±27.19 | >0.05 |
| Following
medication | 324.84±53.55 | 168.91±24.79 | 115.27±19.50 | <0.05 |
Histopathological examination and
IHC
In procedure 3, the endometriotic implants were
excised following the rats being sacrificed, and then the implants
were fixed in the formalin solution at 4°C for one month.
Subsequently, the implants were embedded in paraffin and were
sliced at 4-µm thickness. Hematoxylin and eosin staining was used
for histopathological examination. Subsequently, for the IHC
analysis process, the slides were deparaffinized and rehydrated in
ethanol (ethanol concentrations: 100, 95, 80 and 70%); this was
followed by steaming in sodium citrate buffer (cat. no. ZLI-9065;
Beijing Noble Technology Co., Ltd., Beijing, China). Then, the
slides were incubated in a 3% H2O2 solution
at 26°C for 15 min to deactivate endogenous peroxidase and washed
with phosphate-buffered saline twice for 5 min each time. Once the
nonspecific antigens were blocked at 26°C for 60 min using normal
goat serum (1:20; cat. no. SL038; Beijing Solarbio Science &
Technology Co., Ltd., Beijing, China), the slides were incubated
with primary antibodies overnight at 4°C. The primary antibodies
included rabbit anti-rat vascular endothelial growth factor (VEGF;
cat. no. Ab14078), aromatase P450 (P450arom; cat. no. Ab34193),
transforming growth factor-β (TGF-β; cat. no Ab66043) and matrix
metalloproteinase (MMP)-2 polyclonal antibodies (cat. no. Ab110186)
(1:100; Abcam, Cambridge, UK). The slides were washed and then
incubated with the horseradish peroxidase (HRP)-conjugated goat
anti-rabbit IgG H&L secondary antibodies at 26°C for 30 min
(1:200; cat. no. Ab6721; Abcam); this was followed by
counterstaining with hematoxylin (0.2%) using the ABC kit (Abcam)
according to the manufacturer's protocol. For semi-quantitative
analysis, the researcher assessing the slides was blinded to all
the groups. The slides were evaluated as described previously
(27). According to the percentage of
cells that stained positive, the following scores from 0 to 3 were
assigned: 0: <5%, 1: 5–25%, 2: 26–50%, and 3: >50%. The
staining intensity of the cells was scored as follows: 0: Negative,
1: Weakly positive, 2: Moderately positive, and 3: Strongly
positive. The IHC score for each rat was determined by multiplying
the two scores (staining intensity and percentage of cells
stained).
Enzyme-linked immunosorbent assay
(ELISA)
The concentration of VEGF in the peritoneal fluid
samples and the concentrations of VEGF, P450arom, TGF-β and MMP-2
in the endometriotic implants were assayed using ELISA kits (cat.
no. K2649R, K2652R, K2763R and K2337R, respectively; R&D
Systems, Inc., Minneapolis, MN, USA), according to the
manufacturer's protocol. The endometriotic implant samples were
homogenized and lysed in phosphate-buffered saline at 4°C for 60
min. Whole-tissue lysates were obtained by subsequent
centrifugation at 1,000 × g at 4°C for 20 min and then stored at
−20°C. Double replicates of each sample were run in each assay. The
lower detection limits for the ELISA kits were <1.5 pg/ml
(VEGF), <1.5 U/l (P450arom), <0.1 ng/ml (MMP-2) and <1.5
pg/ml (TGF-β).
Western blot analysis
Endometriotic implant samples were homogenized using
the Fluka Tissue Grinder and lysed in cold radioimmunoprecipitation
assay buffer for 20 min at 4°C (cat. no. BDIT0037; Beijing
Biodragon Immunotechnologies Co., Ltd., Beijing, China). Tissue
lysates were collected and centrifuged at 5,000 × g for 20 min at
4°C. Protein levels were detected using the BCA Protein assay kit
with bovine serum albumin (5 mg/ml) as the standard (cat. no.
BDIT0101; Beijing Biodragon Immunotechnologies Co., Ltd.). Protein
lysate samples (50 µg each) were separated on a 12% SDS-PAGE gel
and were subsequently transferred onto a nitrocellulose membrane.
Following blocking with a 3% bovine serum albumin at 26°C for 30
min (cat. no. BF03075; Beijing Biodragon Immunotechnologies Co.,
Ltd.), the membranes were incubated overnight at 4°C with primary
antibodies. The primary antibodies included rabbit anti-P450arom
polyclonal antibody (1:1,000; cat. no. Ab18995; Abcam), rabbit
anti-VEGF polyclonal antibody (1:1,000; cat. no. Ab46154; Abcam)
and mouse anti-β-actin monoclonal antibody (1:5,000; cat. no.
TDY041; Beijing TDY Biotech Co., Ltd., Beijing, China), which was
used as the internal standard. Then, the membranes were washed and
incubated with a goat anti-rabbit secondary antibody conjugated to
horseradish peroxidase at 26°C for 40 min (1:10,000; cat. no. S004;
Beijing TDY Biotech Co., Ltd.). Immunodetection was performed based
on chemiluminescence (ECL reagent; EMD Millipore, Billerica, MA,
USA. Protein-antibody complexes were quantified using the Bio-Rad
Quantity One software, version 4.6.9 (Bio-Rad Laboratories, Inc.,
Hercules, CA, USA).
Statistical analysis
Statistical analyses were performed using SPSS 11.0
(SPSS, Inc., Chicago, IL, USA). Values were expressed as mean ±
standard deviation. Multiple comparisons were performed using a
one-way analysis of variance and post-hoc Tukey's test.
Non-normally distributed variables were analyzed using
Kruskal-Wallis test and Mann-Whitney U-test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Side effects and survival
Following peritoneal administration of CDDP for 15
days, 4 rats in Group 3 exhibited hair loss, which continued until
the last day of the medication, and a similar phenomenon was not
observed in the other two groups. All rats survived until the day
of sacrifice.
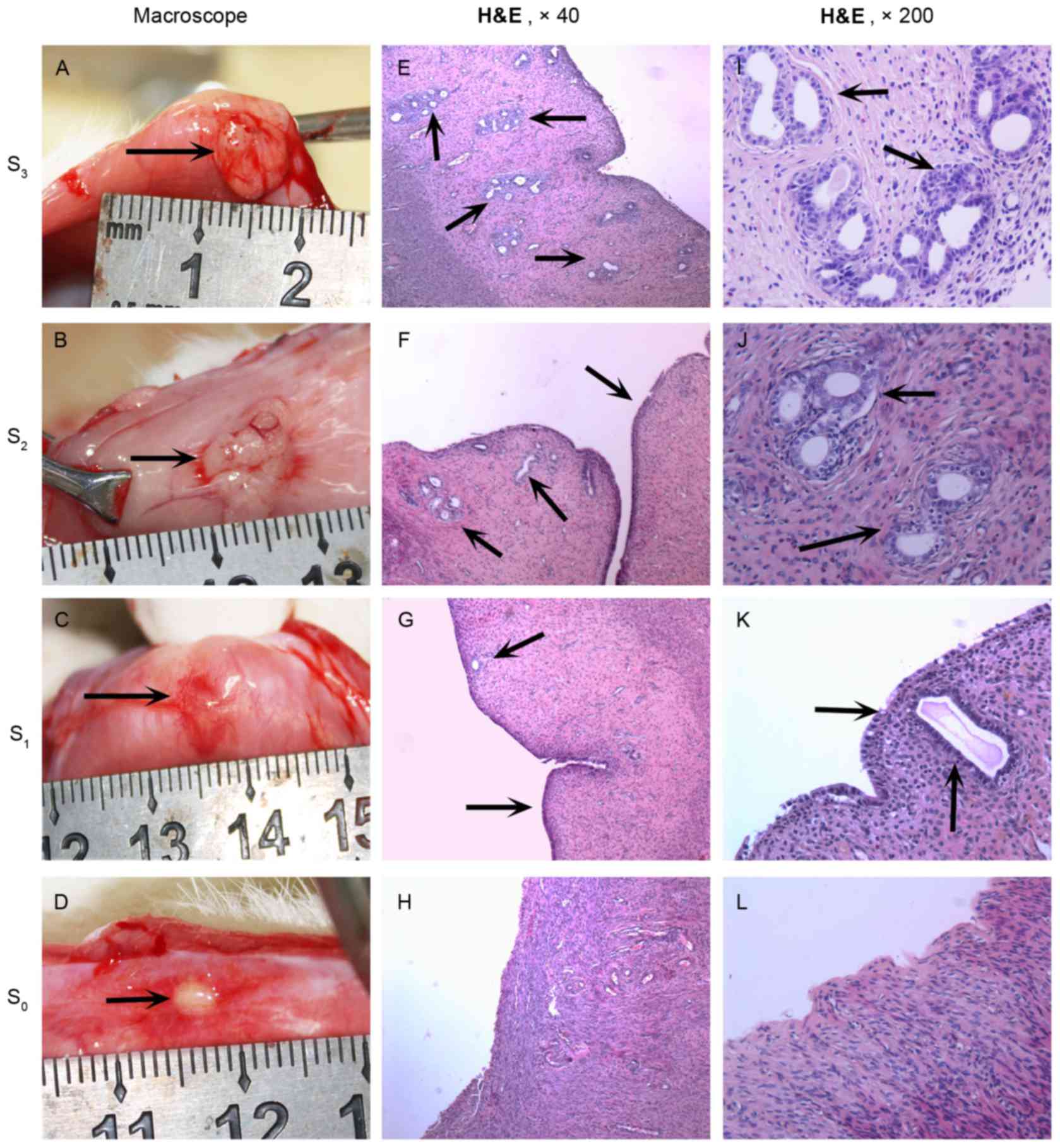
Growth of endometriotic tissues
The formation of cystic and vascularized
endometriotic tissues was successfully induced in all 36 rats. The
mean surface area of the endometriotic implants was similar in all
the groups prior to treatment (P>0.05; Table I). However, at the end of the
treatment, the mean area of the implants in the CDDP groups were
significantly reduced, compared with that in the control group
(P<0.05; Table I). The mean
surface area of the endometriotic implants following medication
demonstrated a significant decrease in Group 2 (from 36.08±6.89 to
18.67±2.99 mm2; P<0.05) and in Group 3 (from
37.92±4.72 to 6.50±2.01 mm2; P<0.05), but it
non-significantly increased in Group 1 (from 38.17±8.61 to
47.08±8.27 mm2; P>0.05) compared with prior to
medication. In addition, the decrease in the mean surface area was
significantly greater in Group 3 compared with in Group 2
(P<0.05). Macroscopic images of the endometriotic implants are
presented in Fig. 1.
HE staining of the implant sections
revealed the presence of ectopic epithelium
The growth of the epithelium in the endometrial
explants was scored as follows: 3, well-preserved epithelium; 2,
moderately preserved epithelium; 1, poorly preserved epithelium
(occasional epithelial cells only); and 0, no epithelium. This
scoring system was based on a previously published study for rat
endometriosis (28). The mean
histopathological score of the implants at the end of the treatment
was significantly lower in Group 3 (0.90±0.57) compared with in
Group 2 (1.67±0.65; P<0.05; Table
I). The mean histopathological score in Group 2 was
significantly lower compared with in Group 1 (2.50±0.67; P<0.05;
Table I). The representative images
from staining of the endometriotic implants based on the histologic
assessment are presented in Fig.
1.
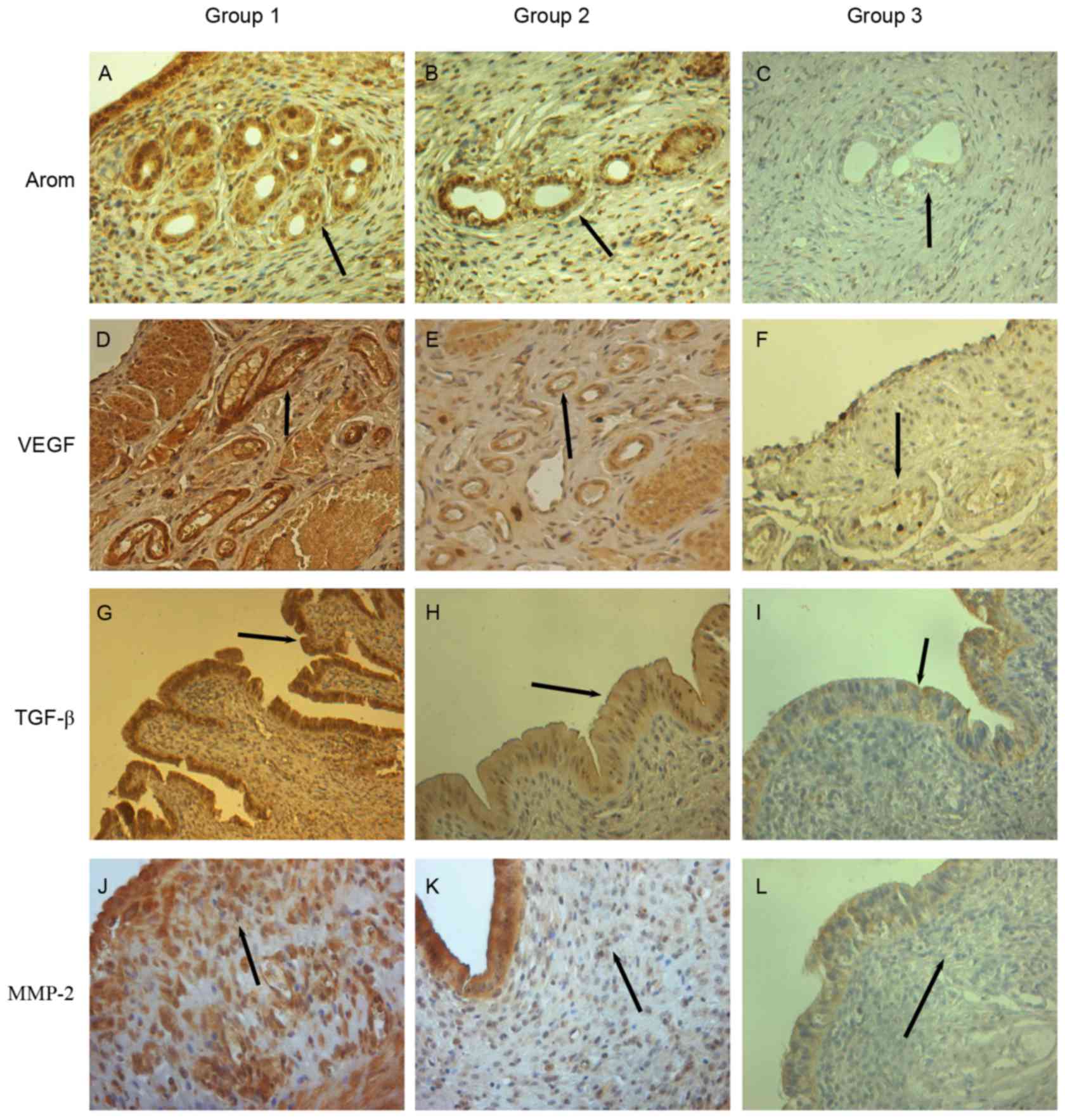
IHC expression of VEGF, P450arom,
MMP-2 and TGF-β in endometriotic tissues
In the endometriotic tissues, the VEGF protein was
present mainly in the vascular endothelial cells, and P450arom was
present mainly in the glandular epithelial cells. The expression
levels of the VEGF and P450arom proteins were significantly lower
in Group 2 (3.00±0.74 and 3.25±0.87, respectively) and Group 3
(1.25±0.45 and 1.08±0.29, respectively) compared with in Group 1
(4.33±0.78 and 4.50±0.90, respectively; P<0.05). Furthermore,
the VEGF and P450arom levels were significantly lower in Group 3
compared with in Group 2 (P<0.05). The IHC expression of VEGF
and P450arom proteins in the endometriotic tissues is presented in
Fig. 2A-C and D-F, respectively. The
TGF-β proteins were observed in the endometrial epithelium, and the
MMP-2 proteins were principally located in the mesenchymal tissue.
The IHC expression of TGF-β and MMP-2 was significantly lower in
Group 2 (3.01±0.60 and 2.67±0.65, respectively) and Group 3
(1.17±0.39 and 0.92±0.29, respectively) compared with in Group 1
(4.23±0.71 and 4.92±0.79 respectively; P<0.05). Furthermore,
TGF-β and MMP-2 expression was significantly lower in Group 3
compared with in Group 2 (P<0.05). The IHC expression of TGF-β
and MMP-2 proteins in the endometriotic tissues is presented in
Fig. 2G-I and J-L, respectively.
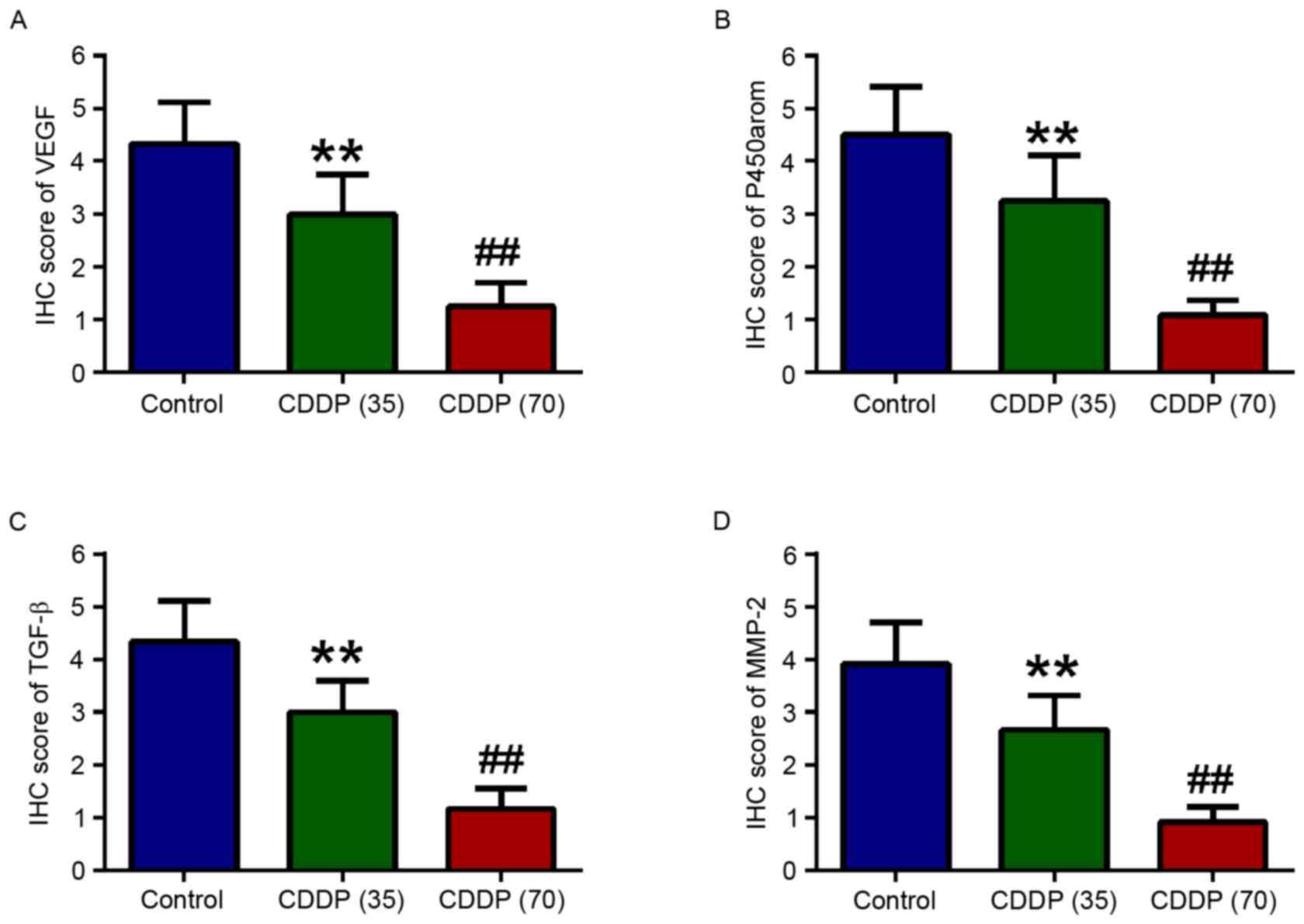
Comparison of the IHC scores of VEGF and P450arom proteins between
the groups is presented in Fig. 3A and
B. Comparison of the IHC scores of TGF-β and MMP-2 proteins
between the groups is presented in Fig.
3C and D.
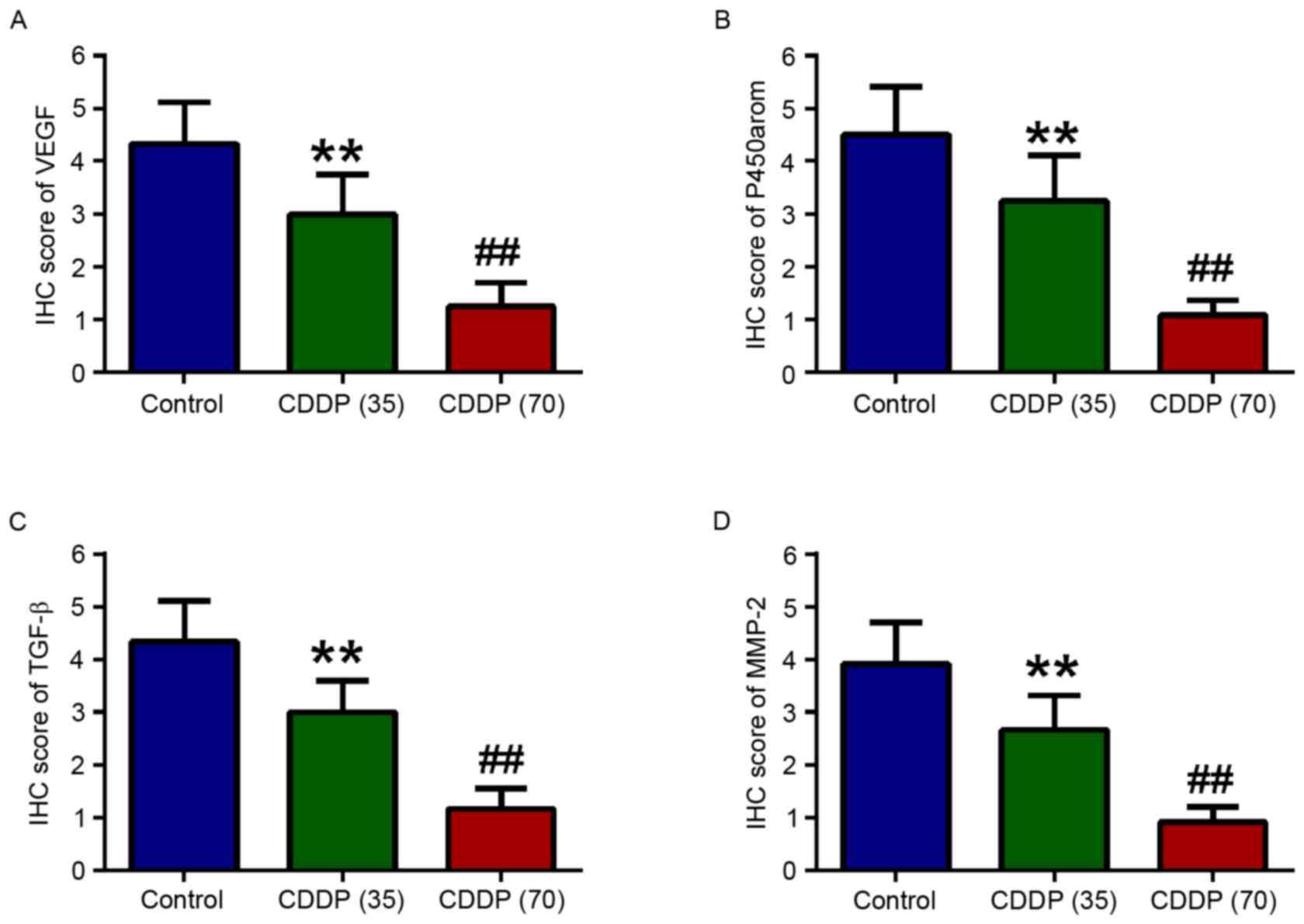 | Figure 3.Comparisons of the IHC scores of
VEGF, P450arom, TGF-β and MMP-2 proteins between the groups. The
IHC score values of (A) VEGF, (B) P450arom, (C) TGF-β and (D) MMP-2
proteins in the endometriotic tissues were presented as the mean ±
standard deviation. Control: Group 1; CDDP (35): Group 2, CDDP dosage is 35
mg/m2; CDDP (70): Group 3, CDDP dosage is 70
mg/m2. **P<0.05 vs. control, ##P<0.05
vs. group CDDP (35). IHC,
immunohistochemistry; VEGF, vascular endothelial growth factor;
P450arom, aromatase P450; TGF-β, transforming growth factor-β;
MMP-2, matrix metalloproteinase 2; CDDP, cisplatin. |
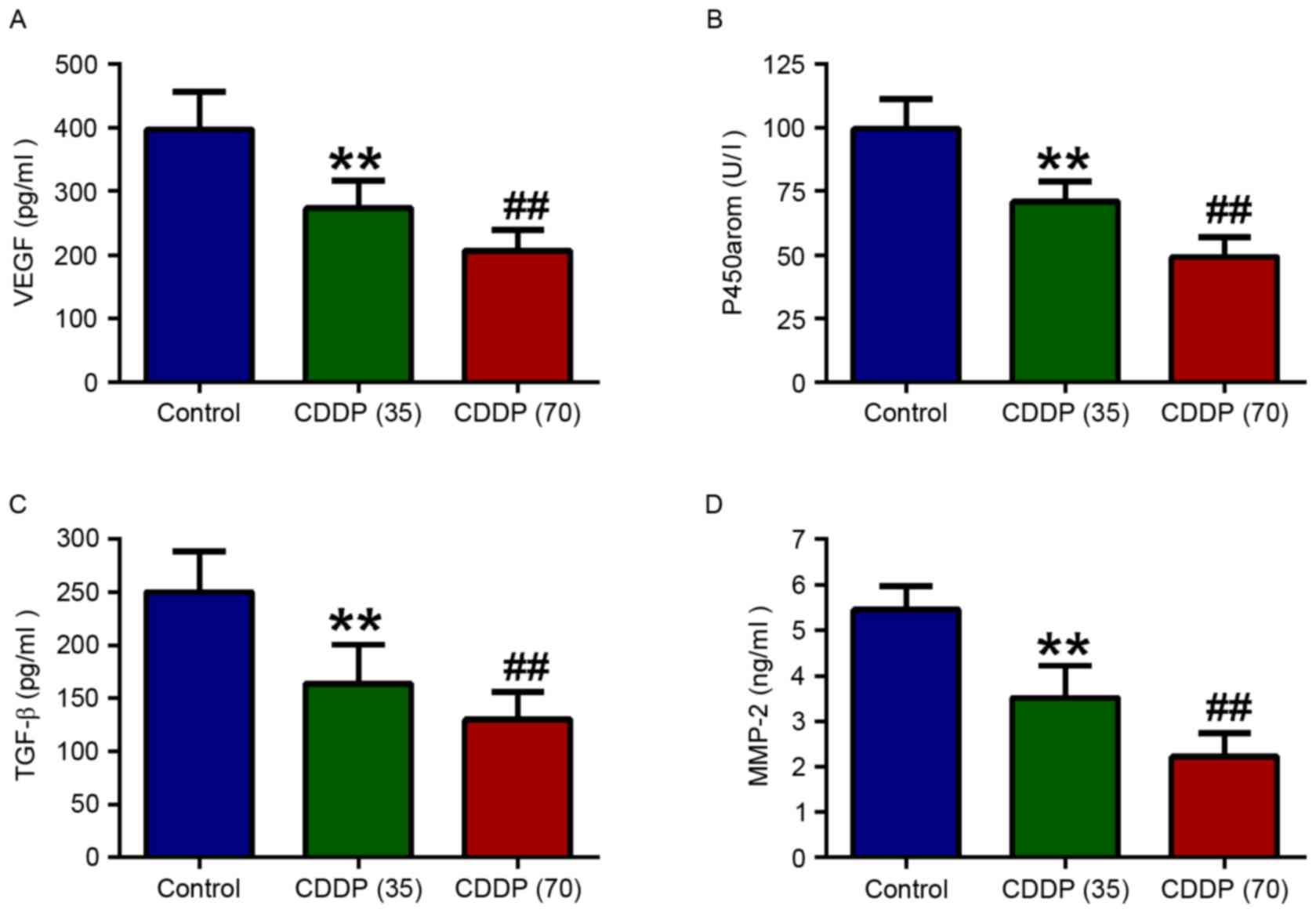
VEGF level in the peritoneal fluid and
VEGF, P450arom, TGF-β and MMP-2 levels in endometriotic
tissues
The VEGF level in the peritoneal fluid was similar
in all groups prior to administration of CDDP/saline (Table I). Following treatment, the VEGF
levels in the peritoneal fluid were significantly lower in Groups 2
(168.91±24.79 pg/ml) and 3 (115.27±19.50 pg/ml) compared with Group
1 (324.84±53.55 pg/ml; P<0.05). In addition, the decrease in the
level of VEGF in peritoneal fluid was significant in Group 2 (from
289.37±12.30 to 168.91±24.79 pg/ml; P<0.05) and in Group 3 (from
275.16±27.19 to 115.27±19.50 pg/ml; P<0.05), while the VEGF
level non-significantly increased in Group 1 (from 278.33±19.90 to
324.84±53.55 pg/ml; P>0.05; Table
I). Following treatment, the VEGF, P450arom, TGF-β and MMP-2
levels in endometriotic tissues were significantly reduced in
Groups 2 (272.83±43.76 pg/ml, 70.92±8.94 U/l, 164.16±36.91 pg/ml
and 3.52±0.72 pg/ml; respectively) and 3 (206.74±36.07 pg/ml,
49.16±7.90 U/l, 130.09±28.72 pg/ml and 2.22±0.57 pg/ml;
respectively), compared with in Group 1 (388.61±79.41 pg/ml,
99.45±11.73 U/l, 250.63±37.69 pg/ml and 5.28±1.06 pg/ml;
respectively; P<0.05; Fig. 4A-D).
Furthermore, these levels were lower in Group 3 than in Group 2
following CDDP treatment. Comparison of the study groups is
presented in Fig. 4A-D.
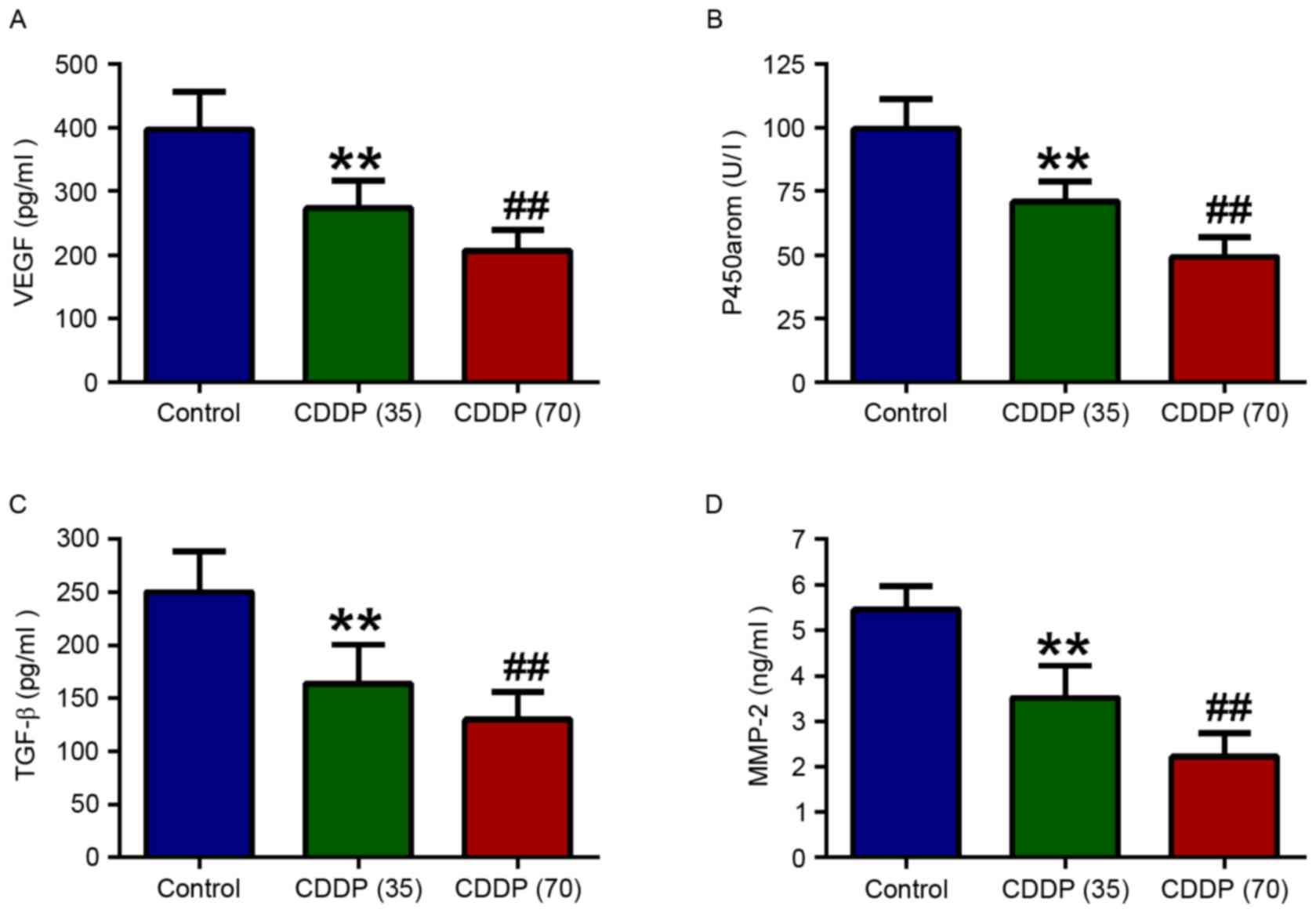 | Figure 4.Comparisons of the VEGF, P450arom,
TGF-β and MMP-2 levels in the endometriotic tissues between the
examined groups. The levels of (A) VEGF, (B) P450arom, (C) TGF-β
and (D) MMP-2 proteins in the endometriotic tissues were quantified
with enzyme-linked immunosorbent assay kits. Data are presented as
the mean ± standard deviation. Control: Group 1; CDDP (35): Group 2, CDDP dosage is 35
mg/m2; CDDP (70): Group 3, CDDP dosage is 70
mg/m2. **P<0.05 vs. control, ##P<0.05
vs. group CDDP (35). VEGF, vascular
endothelial growth factor; P450arom, aromatase P450; TGF-β,
transforming growth factor-β; MMP-2, matrix metalloproteinase 2;
CDDP, cisplatin. |
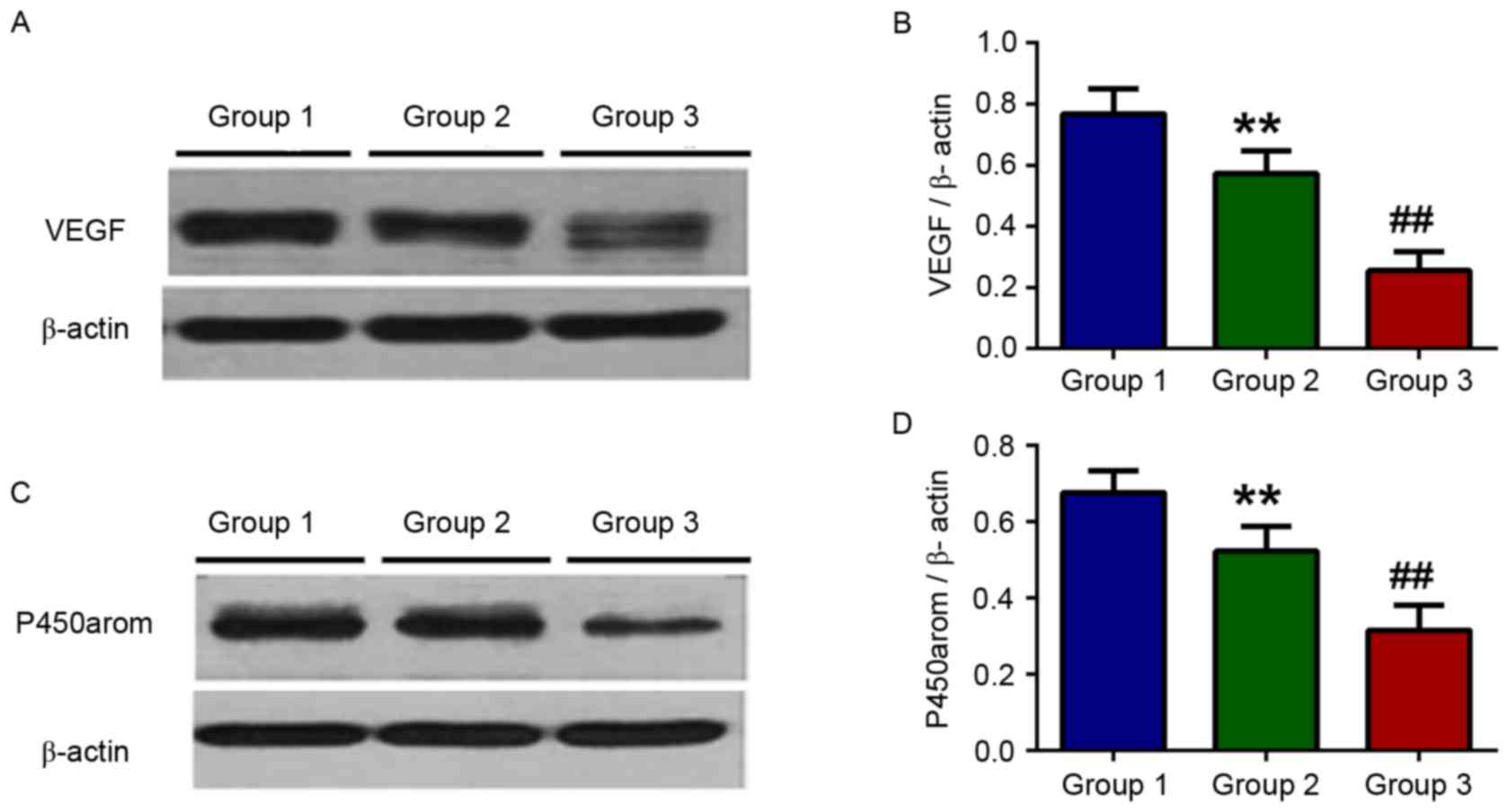
Western blot analysis of VEGF and
P450arom
Western blot analysis of VEGF protein of the
endometriotic tissues demonstrated similar results to the IHC
results (Fig. 5A). The VEGF protein
level in the endometriotic tissues were significantly reduced in
Groups 2 and 3 compared with in Group 1 (P<0.05; Fig. 5B). Western blot analysis of P450arom
protein of the endometriotic tissues also demonstrated similar
results to the IHC results (Fig. 5C).
The P450arom protein levels in the endometriotic tissues were also
significantly reduced in Groups 2 and 3, compared with Group 1
(P<0.05; Fig. 5D). In addition,
the VEGF and P450arom levels were significantly lower in Group 3
compared with in Group 2 (P<0.05; Fig.
5B and D).
Discussion
The rat model established by autologous
transplantation of endometrial tissue has been used extensively in
endometriosis research (25,27,29,30). The
advantages of this model are the low cost involved and the
potential for genetic manipulation using transgenic animals for
etiology studies (31–34). The endometriotic tissues of rats
perform in a similar manner to human endometriotic tissues in organ
explant culture, and the rat model is a valuable tool for the
exploration of novel therapeutic medicines, permitting the research
of pathogenesis and pathophysiology of endometriosis (35).
Blood vessels are necessary for the development and
maintenance of endometriosis (36).
Angiogenesis is essential for the development of a number of
diseases, including cancer and endometriosis (37). Local angiogenesis is regulated by
VEGF, which stimulates the proliferation and migration of vascular
endothelial cells (38). The VEGF
concentration in peritoneal fluid and endometriotic tissue has been
reported to be increased in women with endometriosis (39–41).
Furthermore, TGF-β also serves important roles in
the control of cellular proliferation, differentiation and
apoptosis (42). Evidence
demonstrated that TGF-β is produced by endometriotic lesions and
could be involved in the establishment and progression of the
disease (42,43). The receptors and signaling pathways of
these proteins may be altered in patients with endometriosis and
these proteins may therefore be potential targets for the
development of therapeutic agents (42). VEGF and TGF-β are thought to be
critical for the implantation and infiltration of ectopic
endometrium, as well as the invasion and metastasis of ovarian
tumor cells (44–47). In the present study, following the
administration of CDDP, the regression of endometriotic implants
was observed, along with a significant decrease in the VEGF level
in the peritoneal fluid of rats. Furthermore, the protein
expression of VEGF and TGF-β in the endometriotic implants also
decreased significantly. These results suggest that CDDP may be
involved in the regression of the endometriotic lesions via
suppression of cell proliferation and inhibition of the
angiogenesis of endometriotic tissue.
MMPs and tissue inhibitor of metalloproteinases are
critical factors in the breakdown of the extracellular matrix and
remodeling of endometrial tissue in endometriosis (36). The overexpression of MMP-2 has been
observed in patients with endometriosis (48). MMP-2 is involved in extracellular
matrix disruption in the early angiogenic stage of vascular budding
and sprouting (49). In the present
study, the MMP-2 protein was principally detected in the
mesenchymal cells, and its IHC expression level was significantly
lower in the CDDP-treated groups when compared with the control
group, which was corroborated by and was more evident in the ELISA
results. Therefore, the effect of CDDP's on endometriotic implants
may result from its suppression of MMP-2, which results in the
inhibition of the breakdown of the extracellular matrix and
remodeling of endometrial tissue in the progression of
endometriosis in the rats, and this effect of CDDP may be combined
with its suppression of VEGF and TGF-β; however, the exact
mechanism and action of this association need to be further
studied.
Endometriosis is widely accepted as an
estrogen-dependent condition, the progression of which is strongly
affected by the level of serum estrogen (50). Several studies have reported that
endometriotic tissues express aromatase and synthesize their own
estrogen (1,50–53).
P450arom is the key enzyme for estrogen synthesis, and catalyzes
the conversion of androstenedione and testosterone to estrone and
estradiol (2). As aromatases are
involved in the synthesis of estrogen, the application of aromatase
inhibitors is a valuable advance in the treatment of endometriosis
(54–56). In the present study, P450arom was
principally detected in the glandular epithelial cells of the
endometriotic implants, and the expression levels of the P450arom
protein were significantly lower following CDDP treatment. The
results of ELISA and western blot analyses were in concurrence with
these results. This inhibitory effect of CDDP on estrogen synthesis
was in accordance with the function of aromatase inhibitors
reported in a previous study (56).
In addition, researchers have also demonstrated that CDDP
chemotherapy is associated with effects on ovarian function in
clinical and experimental animal studies (57,58). These
results suggest that CDDP may be involved in the regression of the
endometriotic tissue in an estrogen-inhibiting manner.
The histopathological examination and protein
expression analyses of endometriotic tissue in the present study
demonstrated that angiogenesis-associated factors, including VEGF
and TGF-β, and the extracellular matrix-disrupting protein MMP-2
are all downregulated following CDDP administration. Furthermore,
the expression of the P450arom protein, which is crucial for
estrogen synthesis, was also suppressed by CDDP. As a result,
regression of the endometriotic implants and decrease in the
histological scores were observed in the CDDP-treated groups.
In the present study, a dosage of 70
mg/m2 CDDP was administered every 4 days, which
corresponds with the chemotherapy dosage administered for ovarian
cancer and endometrial cancer in clinical practice, a total of 4
rats in the CDDP-treated group exhibited loss of hair following
treatment for 15 days. However, this was not observed in the group
administered the lower dosage of 35 mg/m2 CDDP.
Furthermore, a dose-dependent effect was observed in the regression
and protein expression of the endometriotic tissues in the two
CDDP-treated groups. These results imply that the CDDP dosage is a
critical factor associated with its effects and side effects in the
treatment of endometriosis and requires exploration in future
studies. However, one should also take into consideration that CDDP
is a drug which has a number of severe side effects, including
severe kidney problems, allergic reactions, decrease immunity to
infections, gastrointestinal disorders, hemorrhage and
neurotoxicity (14,19,59,60);
particularly for CDDP's gonadal toxicity and the concern of
reproductive function preservation (61). Therefore, it may be more appropriate
to administer CDDP medication to cases with endometriosis
refractory at the same time in clinical practice to conventional
therapies for patients who have decided not to have more children
ever. Balancing the benefits and risk of CDDP and the proper
indications of CDDP treatment in endometriosis requires further
study.
In the present study, rats were treated for a total
of 24 days, which was equivalent to 6 estrous cycles of rat. This
was based on the consideration that 6 courses (which equals 6
menstrual cycles of women) of chemotherapy is the standard
treatment protocol for patients with ovarian cancer and endometrial
cancer in clinical practice. To the best of our knowledge, the
present study is the first to apply CDDP treatment in a surgically
induced endometriosis rat model.
In conclusion, the present study demonstrated that
CDDP causes significant regression of surgically induced
endometriotic implants in model rats, and this effect is
accompanied by a decrease in the expression of VEGF, P450arom,
TGF-β and MMP-2 in these tissues. CDDP exhibited promising
therapeutic effects in the rat endometriosis model. Further animal
and clinical studies should be conducted to determine whether CDDP
may be used as an effective therapeutic option for the treatment of
endometriosis.
Acknowledgements
The authors would like to thank Dr Li Yanf, Dr Li
Xue Yuan, and Professor He Jun for their instructive advice and
useful technical support on this research.
Funding
Peking Union Medical College Hospital financially
supported this study.
Availability of data and materials
All data generated and analyzed during this study
are included in this published article.
Authors' contributions
ZL and JL designed the study. ZL, HL, GZ and ZH were
responsible for the collection, analysis and interpretation of data
in the literature. ZL, HL and JL prepared the manuscript together
and were involved in drafting the manuscript or revising it
critically for important intellectual content. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Institutional
Animal Care and Use Committee of the Institute of Laboratory Animal
Science, and the research was conducted in accordance with the
institutional guidelines.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Nothnick WB: The emerging use of aromatase
inhibitors for endometriosis treatment. Reprod Biol Endocrinol.
9:872011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bulun SE, Imir G, Utsunomiya H, Thung S,
Gurates B, Tamura M and Lin Z: Aromatase in endometriosis and
uterine leiomyomata. J Steroid Biochem Mol Biol. 95:57–62. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bedaiwy MA, Allaire C and Alfaraj S:
Long-term medical management of endometriosis with dienogest and
with a gonadotropin-releasing hormone agonist and add-back hormone
therapy. Fertil Steril. 107:537–548. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Surrey ES and Hornstein MD: Prolonged GnRH
agonist and add-back therapy for symptomatic endometriosis:
Long-term follow-up. Obstet Gynecol. 99:709–719. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Meng Q, Sun W, Jiang J, Fletcher NM,
Diamond MP and Saed GM: Identification of common mechanisms between
endometriosis and ovarian cancer. J Assist Reprod Genet.
28:917–923. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang S, Qiu L, Lang JH, Shen K, Huang HF,
Pan LY, Wu M, Yang JX and Guo LN: Prognostic analysis of
endometrioid epithelial ovarian cancer with or without
endometriosis: A 12-year cohort study of Chinese patients. Am J
Obstet Gynecol. 209:241 e241–e249. 2013. View Article : Google Scholar
|
|
7
|
Li F, Tie R, Chang K, Wang F, Deng S, Lu
W, Yu L and Chen M: Does risk for ovarian malignancy algorithm
excel human epididymis protein 4 and CA125 in predicting epithelial
ovarian cancer: A meta-analysis. BMC Cancer. 12:2582012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Augoulea A, Alexandrou A, Creatsa M,
Vrachnis N and Lambrinoudaki I: Pathogenesis of endometriosis: The
role of genetics, inflammation and oxidative stress. Arch Gynecol
Obst. 286:99–103. 2012. View Article : Google Scholar
|
|
9
|
Olovsson M: Immunological aspects of
endometriosis: An update. Am J Reprod Immunol. 66 Suppl
1:S101–S104. 2011. View Article : Google Scholar
|
|
10
|
Ogawa S, Kaku T, Amada S, Kobayashi H,
Hirakawa T, Ariyoshi K, Kamura T and Nakano H: Ovarian
endometriosis associated with ovarian carcinoma: A
clinicopathological and immunohistochemical study. Gynecol Oncol.
77:298–304. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Somigliana E, Vigano P, Parazzini F,
Stoppelli S, Giambattista E and Vercellini P: Association between
endometriosis and cancer: A comprehensive review and a critical
analysis of clinical and epidemiological evidence. Gynecol Oncol.
101:331–341. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Vlahos NF, Kalampokas T and Fotiou S:
Endometriosis and ovarian cancer: A review. Gynecol Endocrinol.
26:213–219. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Aris A: Endometriosis-associated ovarian
cancer: A ten-year cohort study of women living in the Estrie
Region of Quebec, Canada. J Ovarian Res. 3:22010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Brinton LA, Lamb EJ, Moghissi KS, Scoccia
B, Althuis MD, Mabie JE and Westhoff CL: Ovarian cancer risk
associated with varying causes of infertility. Fertil Steril.
82:405–414. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Siufi Neto J, Kho RM, Siufi DF, Baracat
EC, Anderson KS and Abrao MS: Cellular, histologic, and molecular
changes associated with endometriosis and ovarian cancer. J Minim
Invasive Gynecol. 21:55–63. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhao C, Wu LS and Barner R: Pathogenesis
of ovarian clear cell adenofibroma, atypical proliferative
(borderline) tumor, and carcinoma: Clinicopathologic features of
tumors with endometriosis or adenofibromatous components support
two related pathways of tumor development. J Cancer. 2:94–106.
2011. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bookman MA: Optimal primary therapy of
ovarian cancer. Ann Oncol. 27 Suppl 1:i58–i62. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
da Costa Miranda V, de Souza Fêde ÂB, Dos
Anjos CH, da Silva JR, Sanchez FB, da Silva Bessa LR, de Paula
Carvalho J, Filho EA, de Freitas D and Del Pilar Estevez Diz M:
Neoadjuvant chemotherapy with six cycles of carboplatin and
paclitaxel in advanced ovarian cancer patients unsuitable for
primary surgery: Safety and effectiveness. Gynecol Oncol.
132:287–291. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yu X, Zheng H, Chan MT and Wu WK:
Modulation of chemoresponsiveness to platinum-based agents by
microRNAs in cancer. Am J Cancer Res. 7:1769–1778. 2017.PubMed/NCBI
|
|
20
|
Wang QE, Milum K, Han C, Huang YW, Wani G,
Thomale J and Wani AA: Differential contributory roles of
nucleotide excision and homologous recombination repair for
enhancing cisplatin sensitivity in human ovarian cancer cells. Mol
Cancer. 10:242011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Woo MG, Xue K, Liu J, McBride H and Tsang
BK: Calpain-mediated processing of p53-associated parkin-like
cytoplasmic protein (PARC) affects chemosensitivity of human
ovarian cancer cells by promoting p53 subcellular trafficking. J
Biol Chem. 287:3963–3975. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ingelmo JM, Quereda F and Acien P: Effect
of human interferon-alpha-2b on experimental endometriosis in rats:
Comparison between short and long series of treatment. Eur J Obst
Gynecol Reprod Biol. 167:190–193. 2013. View Article : Google Scholar
|
|
23
|
Sun J, Jin C, Wu H, Zhao J, Cui Y, Liu H,
Wu L, Shi Y and Zhu B: Effects of electro-acupuncture on ovarian
P450arom, P450c17α and mRNA expression induced by letrozole in PCOS
rats. PLoS One. 8:e793822013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Simsek Y, Celik O, Karaer A, Gul M, Yılmaz
E, Koc O, Colak C, Zengin S and Aydin NE: Therapeutic efficiency of
Atosiban, an oxytocin receptor blocking agent in the treatment of
experimental endometriosis. Arch Gynecol Obstet. 286:777–783. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Körbel C, Menger MD and Laschke MW: Size
and spatial orientation of uterine tissue transplants on the
peritoneum crucially determine the growth and cyst formation of
endometriosis-like lesions in mice. Hum Reprod. 25:2551–2558. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Spiers DE and Candas V: Relationship of
skin surface area to body mass in the immature rat: A
reexamination. J Appl Physiol Respir Environ Exerc Physiol.
56:240–243. 1984.PubMed/NCBI
|
|
27
|
Ceyhan ST, Onguru O, Fidan U, Ide T, Yaman
H, Kilic S and Baser I: Comparison of aromatase inhibitor
(letrozole) and immunomodulators (infliximab and etanercept) on the
regression of endometriotic implants in a rat model. Eur J Obstet
Gynecol Reprod Biol. 154:100–104. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Keenan JA, Williams-Boyce PK, Massey PJ,
Chen TT, Caudle MR and Bukovsky A: Regression of endometrial
explants in a rat model of endometriosis treated with the immune
modulators loxoribine and levamisole. Fertil Steril. 72:135–141.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Edwards AK, Nakamura DS, Virani S, Wessels
JM and Tayade C: Animal models for anti-angiogenic therapy in
endometriosis. J Reprod Immunol. 97:85–94. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Li Z, Liu H, He Z, Zhang G and Lang J:
Effects of cisplatin and letrozole on surgically induced
endometriosis and comparison of the two medications in a rat model.
Eur J Pharm Sci. 93:132–140. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Stanic AK, Kim M, Styer AK and Rueda BR:
Dendritic cells attenuate the early establishment of
endometriosis-like lesions in a murine model. Reprod Sci.
21:1228–1236. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Aydin Y, Atis A, Uludag S, Tezer I, Sakiz
D, Acar H and Toklu A: Remission of endometriosis by hyperbaric
oxygen treatment in rats. Reprod Sci. 18:941–947. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mansour G, Sharma RK, Agarwal A and
Falcone T: Endometriosis-induced alterations in mouse metaphase II
oocyte microtubules and chromosomal alignment: A possible cause of
infertility. Fertil Steril. 94:1894–1899. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chen QH, Zhou WD, Pu DM, Huang QS, Li T
and Chen QX: 15-Epi-lipoxin A(4) inhibits the progression of
endometriosis in a murine model. Fertil Steril. 93:1440–1447. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sharpe-Timms KL: Using rats as a research
model for the study of endometriosis. Ann NY Acad Sci. 955:318–406.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Osteen KG, Yeaman GR and Bruner-Tran KL:
Matrix metalloproteinases and endometriosis. Semin Reprod Med.
21:155–164. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Griffioen AW and Molema G: Angiogenesis:
Potentials for pharmacologic intervention in the treatment of
cancer, cardiovascular diseases, and chronic inflammation.
Pharmacol Rev. 52:237–268. 2000.PubMed/NCBI
|
|
38
|
Ozer H, Boztosun A, Acmaz G, Atilgan R,
Akkar OB and Kosar MI: The efficacy of bevacizumab, sorafenib, and
retinoic acid on rat endometriosis model. Reprod Sci. 20:26–32.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Machado DE, Abrao MS, Berardo PT, Takiya
CM and Nasciutti LE: Vascular density and distribution of vascular
endothelial growth factor (VEGF) and its receptor VEGFR-2 (Flk-1)
are significantly higher in patients with deeply infiltrating
endometriosis affecting the rectum. Fertil Steril. 90:148–155.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
McLaren J, Prentice A, Charnock-Jones DS
and Smith SK: Vascular endothelial growth factor (VEGF)
concentrations are elevated in peritoneal fluid of women with
endometriosis. Hum Reprod. 11:220–223. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Donnez J, Smoes P, Gillerot S,
Casanas-Roux F and Nisolle M: Vascular endothelial growth factor
(VEGF) in endometriosis. Hum Reprod. 13:1686–1690. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Dela Cruz C and Reis FM: The role of TGFβ
superfamily members in the pathophysiology of endometriosis.
Gynecol Endocrinol. 31:511–515. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Zhang Q, Duan J, Liu X and Guo SW:
Platelets drive smooth muscle metaplasia and fibrogenesis in
endometriosis through epithelial-mesenchymal transition and
fibroblast-to-myofibroblast transdifferentiation. Mol Cell
Endocrinol. 428:1–16. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Rein DT, Schmidt T, Bauerschmitz G, Hampl
M, Beyer IM, Paupoo AA, Curiel DT and Breidenbach M: Treatment of
endometriosis with a VEGF-targeted conditionally replicative
adenovirus. Fertil Steril. 93:2687–2694. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Mohamed ML, El Behery MM and Mansour SA:
Comparative study between VEGF-A and CA-125 in diagnosis and
follow-up of advanced endometriosis after conservative laparoscopic
surgery. Arch Gynecol Obstet. 287:77–82. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Perini JA, Cardoso JV, Berardo PT,
Vianna-Jorge R, Nasciutti LE, Bellodi-Privato M, Machado DE and
Abrão MS: Role of vascular endothelial growth factor polymorphisms
(−2578C>A, −460 T>C, −1154G>A, +405G>C and +936C>T)
in endometriosis: A case-control study with Brazilians. BMC Womens
Health. 14:1172014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Tamburro S, Canis M, Albuisson E,
Dechelotte P, Darcha C and Mage G: Expression of transforming
growth factor beta1 in nerve fibers is related to dysmenorrhea and
laparoscopic appearance of endometriotic implants. Fertil Steril.
80:1131–1136. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Huang HF, Hong LH, Tan Y and Sheng JZ:
Matrix metalloproteinase 2 is associated with changes in steroid
hormones in the sera and peritoneal fluid of patients with
endometriosis. Fertil Steril. 81:1235–1239. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Carmeliet P: Mechanisms of angiogenesis
and arteriogenesis. Nat Med. 6:389–395. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Bulun SE: Endometriosis. N Engl J Med.
360:268–279. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Burney RO and Giudice LC: Pathogenesis and
pathophysiology of endometriosis. Fertil Steril. 98:511–519. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Bulun SE, Zeitoun KM, Takayama K and
Sasano H: Molecular basis for treating endometriosis with aromatase
inhibitors. Hum Reprod Update. 6:413–418. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Abu Hashim H: Potential role of aromatase
inhibitors in the treatment of endometriosis. Int J Womens Health.
6:671–680. 2014.PubMed/NCBI
|
|
54
|
Ailawadi RK, Jobanputra S, Kataria M,
Gurates B and Bulun SE: Treatment of endometriosis and chronic
pelvic pain with letrozole and norethindrone acetate: A pilot
study. Fertil Steril. 81:290–296. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Abushahin F, Goldman KN, Barbieri E, Milad
M, Rademaker A and Bulun SE: Aromatase inhibition for refractory
endometriosis-related chronic pelvic pain. Fertil Steril.
96:939–942. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Oner G, Ozcelik B, Ozgun MT, Serin IS,
Ozturk F and Basbug M: The effects of metformin and letrozole on
endometriosis and comparison of the two treatment agents in a rat
model. Hum Rep. 25:932–937. 2010. View Article : Google Scholar
|
|
57
|
Li X, Kang X, Deng Q, Cai J and Wang Z:
Combination of a GnRH agonist with an antagonist prevents flare-up
effects and protects primordial ovarian follicles in the rat ovary
from cisplatin-induced toxicity: A controlled experimental animal
study. Reprod Biol Endocrinol. 11:162013. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Blumenfeld Z, Avivi I, Linn S, Epelbaum R,
Ben-Shahar M and Haim N: Prevention of irreversible
chemotherapy-induced ovarian damage in young women with lymphoma by
a gonadotrophin-releasing hormone agonist in parallel to
chemotherapy. Hum Reprod. 11:1620–1626. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Dasari S and Tchounwou PB: Cisplatin in
cancer therapy: Molecular mechanisms of action. Eur J Pharmacol.
740:364–378. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Ruggiero A, Trombatore G, Triarico S,
Arena R, Ferrara P, Scalzone M, Pierri F and Riccardi R: Platinum
compounds in children with cancer: Toxicity and clinical
management. Anticancer Drugs. 24:1007–1019. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Chahvar ST, Al-Shawaf T and Tranquilli AL:
Pharmacologic ovarian preservation in young women undergoing
chemotherapy. Curr Med Chem. 21:223–229. 2014. View Article : Google Scholar : PubMed/NCBI
|