Introduction
Three-dimensional conformal radiotherapy (3D-CRT)
has gradually developed and spread since the 90s. Currently this
technique is the standard radiotherapy (RT) treatment in many
centers worldwide. It is based on virtual simulation and requires
three-dimensional treatment planning systems (3D-TPS) and linear
accelerators equipped with multileaf collimators (MCLs) (1).
In several RT centers, especially in developing
countries, 3D-CRT is not available and 2D-RT is still the only used
technique (2). In 2014 an estimation
of over 10,846 high-energy RT machines operating showed that 2,386
were still represented by cobalt units (3).
RT of pancreatic cancer (CaP) has been tested in
recent decades in different settings (neoadjuvant, adjuvant, and
palliative treatment) and nowadays is considered as a therapeutic
option for CaP (4). However, RT in
CaP is currently less used in developing countries due to
technological limitations. In fact, in these centers RT fields are
still planned with conventional simulators or a C-arm X-ray unit
and the treatments are frequently delivered with cobalt machines. A
precise targeting of CaP is difficult because these tumors are not
visible on plain radiographs. In addition, 2D-RT is not able to
produce an optimal and homogeneous dose distributions. This issue
is particularly relevant in CaP, considering several organs at risk
(OARs) such as spinal cord, duodenum, liver and kidneys that
surround the pancreas.
Currently with the diffuse use of computerized
tomography (CT) images now available in almost all centers and the
conventional X-ray images produced by a simulator equipment.
Therefore, theoretically we could hypothesis conformation of
treatment fields by combination of extrapolated radiological
information from the available images.
Based on these premises, the objective of this
analysis was to propose an optimized planning technique for CaP.
This technique is based on double simulation which resolves the
problems of radiographic image distortion.
Materials and methods
Patients
In our center, 5 patients (2 female, 3 male) with
locally advanced pancreatic head cancer undergoing RT treatment,
aged 46 to75 years and with median body mass index of 23 (range:
21–29) were identified. Patients written informed consent for the
use of their data and CT images to perform this analysis was sought
prior. The Institutional Ethical Committee Board of High Technology
Center for Research and Education (Campobasso, Italy) approved the
study. Treatment planning was performed with 3 different methods:
Standard two-dimensional (2D-SRT), three-dimensional-conformal
(3D-CRT) and 2D-conformal (2D-CRT). In Table I, the characteristics of the 3
planning techniques are briefly summarized.
 | Table I.Fields definition for standard 2D
radiotherapy. |
Table I.
Fields definition for standard 2D
radiotherapy.
| Fields | Margin | Reference points and
directions | Co60 | 10 MV |
|---|
| Anterior- | Cranial | From point A (middle
of T11 vertebra): caudally | 0 | 5 |
| Posterior | Caudal | From point B (bottom
of the duodenal wall): caudally | 15 | 10 |
|
| Right | From point C (most
external point of the duodenum): laterally | 10 | 8 |
|
| Left | From point D (left
margin of L1 vertebra): laterally | 15 | 13 |
|
|
| Same as
anterior-posterior |
|
|
| Lateral | Cranial | Same as
anterior-posterior | 0 | 5 |
|
| Caudal | Same as
anterior-posterior | 15 | 10 |
|
| Anterior | From point E
(anterior surface of L1 vertebra): anteriorly | 95 | 93 |
|
| Posterior | From point E
(anterior surface of L1 vertebra): posteriorly | 20 | 18 |
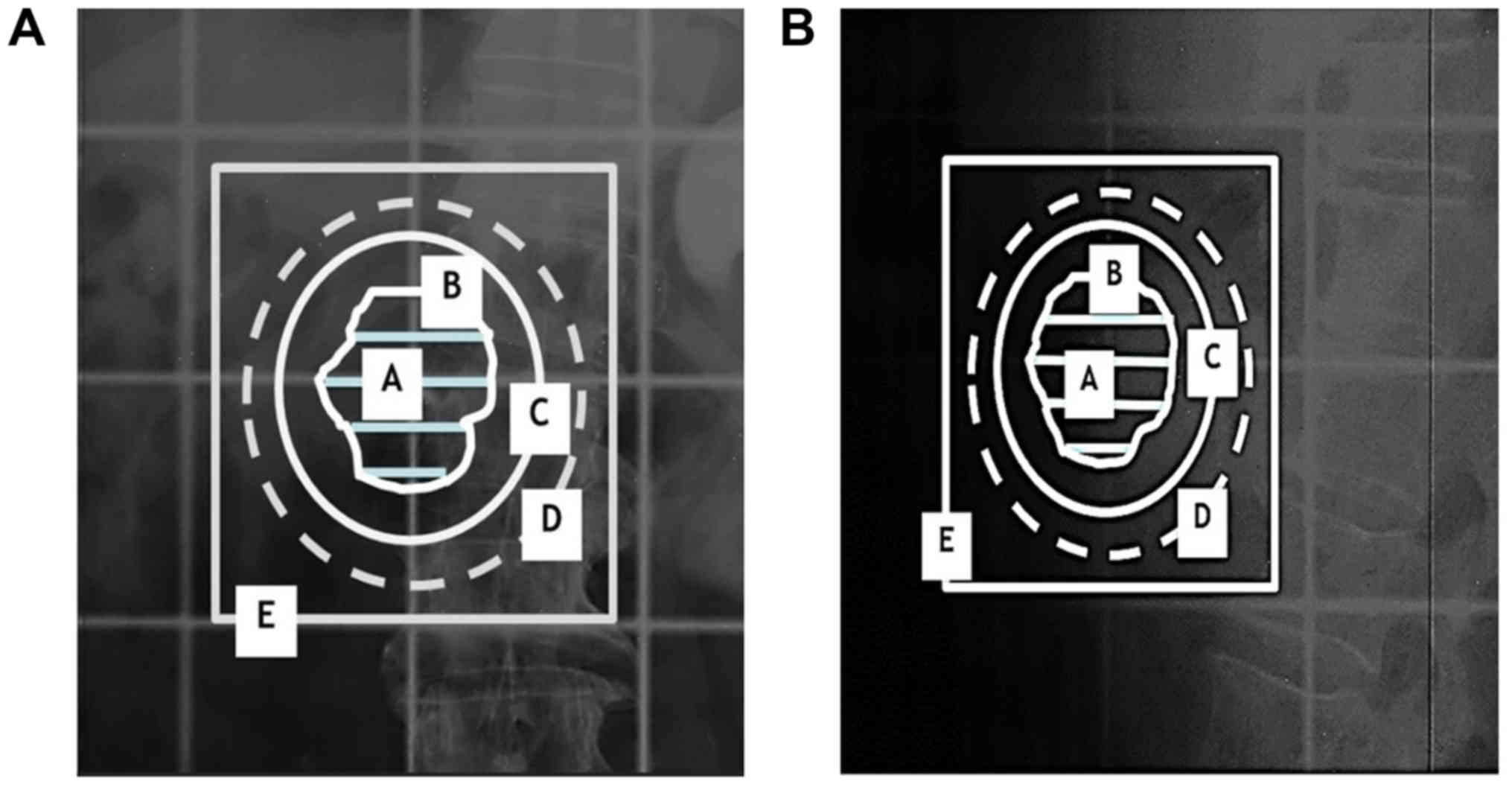
2D-SRT
Based on our previous analysis (5), a box-technique based on standard fields
was tested. In short, the treatment was planned as follows: i)
Standard fields were placed in reference to anatomical structures
visible on X-ray images (vertebrae and the duodenum. The latter was
opacified at the time of simulation with oral contrast medium; ii)
fields sizes were adapted according to the beam energy as shown in
Table II (Fig. 1A and B).
 | Table II.Planning characteristics. |
Table II.
Planning characteristics.
| Characteristics | 2D-SRT | 2D-CRT | 3D-CRT |
|---|
| Standard
simulation | With fields
definition based on bony landmarks and duodenum | With fields
definition based on manual reconstruction of the target shape,
dimension and position | Not performed |
| CT scan | Not performed | T9-l5; 5 mm scan
interval | CT-simulation; T9-l5;
5 mm scan interval |
| Target
definition | Not defined | GTV=tumor; CTV=GTV;
PTV=CTV + 11 mm radially and 14 in cranio-caudal direction; further
margin of 1 cm added for potential ‘transfer errors’ | GTV=tumor; CTV=GTV;
PTV=CTV + 11 mm radially and 14 in cranio-caudal direction |
| Fields margins | Based on anatomical
landmarks | Around the PTV: 2 cm
(Co60), 1.5 cm (10 MV) | Adapted based on dose
distribution using 3D TPS |
| Beam weight | Adapted based on dose
distribution using 2D TPS (only at isocenter) | Adapted based on dose
distribution using 2D TPS (only at isocenter) | Adapted based on dose
distribution using 3D TPS |
3D-CRT
Irradiation treatment plans were generated according
to the standard processes of CT-simulation, target definition, and
optimization of 3D dose distribution by using Dose Volume
Histograms (DVHs) for Planning Target Volume (PTV) and Organs at
Risk (OARs). Dose prescription was based on ICRU 62 indications
(6).
2D-CRT
With correct patients' alignment in supine position,
conventional simulation was performed. For anterior-posterior (AP)
radiographs, the centering point was on the posterior end of the L1
spinous process [defined as point A] (Fig. 1C). Lateral view (LL) radiographs had
their center at the same anatomical landmark (Fig. 1D).
CT scans with the patient in the same position for
treatment reproducibility were performed (Table I), extending from T9 to L5 with an
interval between scans of 5 mm. CT images were printed with a scale
indicator display. The tumor had to be identified on all scans
where it was visible. The scan displaying the center (in
cranio-caudal direction) of the tumor was identified. The geometric
center of the tumor [defined as the center of the rectangle
circumscribing the visible tumor mass] (Fig. 2A) was indicated on this scan. This
point was defined as point B.
Then, the distance in 3 dimensions (x, y, z) between
point A and point B was calculated: i) The distance of point B from
the center of the lumbar spine was measured, which corresponds to
the lateral distance from point B to point A, if the patient is
correctly aligned (distance x, Fig.
2B); ii) the cranio-caudal distance was calculated as the
distance between the level of the scan in which point A and B were
visible (distance y); iii) the antero-posterior distance was
defined by measuring the distance between point A and B from the CT
bed and then calculating their relative difference (distance z,
Fig. 2C and D);.
Another simulation was then performed. Using the
distances between point A and point B, the simulator table/bed with
the patient was moved to align point B (center of the target) with
the simulator isocenter. Two new X-rays centered at point B, one in
the anterior-posterior projection and the other in lateral
projection, were taken (Fig. 3A and
B).
In consideration of the magnification factor, the
Gross Tumor Volume (GTV) profiles at different scan levels were
manually drawn (Fig. 3A and B). This
profile defined GTV/Clinical Target Volume (CTV). Furthermore, PTV
margins definition (14 mm cranial caudal direction and 11 mm in the
radial direction, Fig. 3A and B) were
added to the CTV. Another, margin of 10 mm to account for any
inaccuracies in the profiles transfer from the CT images to the
simulation radiographs was added to the PTV (Fig. 3A and B). The irradiation fields were
obtained by adding an extra margin of 10 mm in cranio-caudal
direction and 5 mm in the radial direction. Finally, a 2D dose
distribution optimization was realized at the isocenter level
only.
Comparison
Using a 3D TPS (Masterplan, Nucletron BV,
Veenendaal, The Netherlands), 3D dose distributions and DVHs
achieved with the 3 different treatment techniques were calculated
using 10 MV photons beams. For 2D techniques, calculation of the
dose distribution by a cobalt source was also performed. Finally,
compliance with the dose-volume constraints (QUANTEC) obtained with
the 3 different techniques were evaluated (7). This evaluation was performed by
calculating a set of parameters for the main OARs and assuming two
different PTV dose prescriptions (30 Gy in 3 Gy/fraction and 50 Gy
in 2 Gy/fraction).
Results
Target irradiation
Using the 10 MV beam, the ICRU 62 indications were
achieved in all patients (Dmin >95%, Dmax
<107%) with all techniques (SRT-2D, 3D-CRT, CRT-2D) (Table III).
 | Table III.Planning results. |
Table III.
Planning results.
| A, Cobalt 60
source |
|---|
|
|---|
| Organs at risk | Parameter, median
(range) | 2D-SRT | 2D-CRT | 3D-CRT |
|---|
| PTV | V95% | 98.9
(95.3–100.0) | 99.6
(95.1–100.0) | NE |
|
| V107% | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | NE |
|
| Dmean | 99.5
(99.1–100.2) | 99.9
(98.4–100.0) | NE |
| Duodenum | Dmax | 102.0
(101.2–103.5) | 102.3
(64.8–102.4) | NE |
| Liver | Dmean | 33.4 (7.1–49.3) | 22.3 (12.1–27.6) | NE |
| Spinal cord | Dmax | 77.7 (74.8–96.7) | 83.9 (81.3–90.4) | NE |
| Kidney |
Dmean | 30.7
(23.3–52.5) | 16.9
(9.4–43.9) | NE |
|
| B, LINAC 10
MV |
|
| Organs at
risk | Parameter,
median (range) | 2D-SRT | 2D-CRT | 3D-CRT |
|
| PTV |
V95% | 100 (100–100) | 100 (100–100) | 100 (100–100) |
|
|
V107% | 0 (0–0) | 0 (0–0) | 0 (0–0) |
|
|
Dmean | 100.8
(100.3–101.3) | 100.4
(99.8–100.9) | 100.0
(99.4–100.2) |
| Duodenum |
Dmax | 103.0
(101.6–104.2) | 101.9
(100.5–103.7) | 101.2
(100.3–102.6) |
| Liver |
Dmean | 30.8
(9.7–45.7) | 17.3
(3.8–21.9) | 11.0
(2.1–16.6) |
| Spinal cord |
Dmax | 72.8
(67.6–98.1) | 71.5
(67.8–72.5) | 71.1
(66.5–72.3) |
| Kidney |
Dmean | 35.6
(20.7–47.6) | 10.6
(4.8–21.7) | 5.8 (2.9–16.2) |
Using the cobalt source, both 2D techniques achieved
PTV Dmin <95% and PTV Dmax <107% in all
patients. However, a dose >95% of the prescribed was
administered to >95% of the PTV (V95% >95%) in all
patients (Table III).
OAR irradiation
Using the 10 MV beams, the duodenum and spinal cord
Dmax were substantially similar using the 3 treatment
techniques. In terms of liver and kidneys Dmean, there
was a gradual improvement from 2D-SRT, 2D-CRT, and 3D-CRT
technique. Furthermore, 2D-CRT, compared with 2D-SRT, halved liver
Dmean and reduced to approximately 1/3 the kidney
Dmean (Table III).
Using the cobalt 60 source beams, similar results in
terms of spinal cord and duodenum Dmax with both 2D
techniques were recorded. A marked dose reduction to the kidneys
Dmean (from 30.7 to 16.9%) and liver (from 33.4 to
22.3%) were observed with 2D-CRT.
Dose-volume constraints
Tables IV and
V show the results in terms of
irradiation of the OAR, at the two different prescribed dose levels
of 30 and 50 Gy, respectively. The duodenum, spinal cord and liver
dose-volume constraints were always met, for any prescribed dose
and with all used techniques. Regarding the kidney
Dmean, only 10 MV photons with 30 Gy dose met the
constraint in all patients, irrespective of the technique. At the
same dose level, and by using the cobalt 60 source, only 2D-CRT
respected the constraint Dmean <15 Gy in all
patients, while exceeded this limit in one patient using 2D-SRT.
Using the 50 Gy dose with 10 MV energy, 2D-CRT and 3D-CRT complied
in all patients with the kidneys Dmean constraint. At
the same dose level, with a cobalt source, neither of the two 2D
techniques achieved a Dmean <15 Gy in all
patients.
 | Table IV.Dosimetrical results for Organs at
Risk with total prescribed dose of 30 Gy. |
Table IV.
Dosimetrical results for Organs at
Risk with total prescribed dose of 30 Gy.
| A, Cobalt 60
source |
|---|
| Organ | Parameter,
constraint | Standard 2D | Optimized 2D | Conformal 3D |
|---|
| Duodenum | Dmax
<55 | 30.6
(30.4–31.0) | 30.7
(19.4–30.7) | NE |
| Liver | Dmean
<30 | 10.2
(2.1–14.8) | 6.7 (3.6–8.3) | NE |
| Spinal cord | Dmax
<50 | 23.3
(22.4–29.0) | 25.2
(24.4–27.1) | NE |
| Kidney | Dmean
<15 | 9.2 (7.0–15.7) | 5.1 (2.8–13.2) | NE |
|
| B, LINAC 10
MV |
|
| Organ | Parameter,
constraint | Standard
2D | Optimized
2D | Conformal
3D |
|
| Duodenum | Dmax
<55 | 30.9
(30.5–31.3) | 30.6
(30.1–31.1) | 30.4
(30.1–30.8) |
| Liver | Dmean
<30 | 9.2 (2.9–13.7) | 5.2 (1.1–6.6) | 3.3 (0.6–4.9) |
| Spinal cord | Dmax
<50 | 21.8
(20.3–29.4) | 21.4
(20.3–21.7) | 21.3
(19.9–21.7) |
| Kidney | Dmean
<15 | 10.7
(6.2–14.3) | 3.2 (1.4–6.5) | 1.7 (0.9–4.9) |
 | Table V.Dosimetrical results for Organs at
Risk with total prescribed dose of 50 Gy. |
Table V.
Dosimetrical results for Organs at
Risk with total prescribed dose of 50 Gy.
| A, Cobalt 60
source |
|---|
|
|---|
| Organ | Parameter,
constraint | 2D-SRT | 2D-CRT | 3D-CRT |
|---|
| Duodenum | Dmax
<55 | 51.0
(50.6–51.7) | 51.1
(32.4–51.2) | NE |
| Liver | Dmean
<30 | 16.7
(3.5–24.6) | 11.1
(6.0–13.8) | NE |
| Spinal cord | Dmax
<50 | 38.8
(37.4–48.3) | 41.9
(40.6–45.2) | NE |
| Kidney | Dmean
<15 | 15.3
(11.6–26.2) | 8.4 (4.7–21.9) | NE |
|
| B, LINAC 10
MV |
|
| Organ | Parameter,
constraint | 2D-SRT | 2D-CRT | 3D-CRT |
|
| Duodenum | Dmax
<55 | 51.5
(50.8–52.1) | 50.9
(50.2–51.8) | 50.6
(50.1–51.3) |
| Liver | Dmean
<30 | 15.4
(4.8–22.8) | 8.6 (1.9–10.9) | 5.5 (1.0–8.3) |
| Spinal cord | Dmax
<50 | 36.4
(33.8–49.0) | 35.7
(33.9–36.2) | 35.5
(33.2–36.1) |
| Kidney | Dmean
<15 | 17.8
(10.3–23.8) | 5.3 (2.4–10.8) | 2.9 (1.4–8.1) |
Discussion
In the past, different methods for 3D information
transfer from CT scans to simulator X-rays were proposed (8–10). The
interest in these solutions disappeared due to the spread of 3D-CRT
based on CT-simulation, 3D-TPS and MCLs. However, 2D technology is
still the only technique available in most developing countries.
The lack of 3D-CRT in some centers, limits the use of RT especially
in the treatment of malignancies requiring precision in target
definition and OARs sparing.
In a previous study, we observed that with 2D-SRT,
it is possible to meet the current standard dose-volume constraints
(7) only by using lower total doses
(30–36 Gy) (11). In a subsequent
study, we defined the optimal fields size for involved-field
irradiation of CaP with 2D-SRT technique (5).
In our current study, again CaP was used as a model
for an optimized irradiation 2D technique (2D-CRT) feasibility for
consistency. The main problem in the transfer of images from a CT
slice to a simulator radiograph is the radiological image
distortion depending on the beam projection. In the technique
proposed in this study, this problem is solved by ‘double’
simulation. The GTV is drawn on a second simulated image where the
machine isocentre is placed directly at the center of the target.
This solution eliminates the problems of image distortion.
When we conducted a comparison between 2D-SRT and
the two optimized CT information-based 3D-CRT and 2D-CRT
techniques. The analysis showed that the latter technique can
substantially improve the dosimetric results compared to 2D-SRT
even with ‘standard’ RT doses (50 Gy) by a linear accelerator.
Using a cobalt source, only a reduced dose (30 Gy) can be delivered
by 2D-CRT. However, it should be noted that these types of
accelerated-hypo-fractionated treatments (30 Gy, 3 Gy/fraction)
were successfully used not only for palliation (12) but also in curative (13) and neoadjuvant (14) treatments.
As expected, the results of 2D-CRT were slightly
lower compared to 3D-CRT. Probably, this difference was partially
due to the additional margin to account for possible inaccuracies
in the calculation of the distances between point A and point B
(transfer error). In this analysis, to this margin was arbitrarily
assigned a value of 1 cm. Prospective assessments on the extent of
the ‘transfer error’ could allow an optimization of this
margin.
It should be emphasized that using 2D-CRT technique
is of utter most importance that the patient is properly aligned.
This allows precise measurement of the distance between point A and
B in the lateral direction.
Unfortunately, to achieve a wide spread of 3D-CRT
technology in all RT centres in the world will require several
years given the economic costs and logistic problems. In the
meantime, the use of 2D-CRT technique may be useful to improve the
quality of treatments in various anatomical sites even for centers
in low and middle-income countries. Therefore, it could be useful
to assess this method in RT treatment of other tumors. Furthermore,
testing and clinical validation of the feasibility and
reproducibility of this technique in the setting of developing
countries is highly encouraged.
For these reasons, further studies have been planned
in our center to evaluate 2D-CRT in the treatment of prostate
cancer and in palliative treatments of advanced pelvic
malignancies.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
MB, SaC, FD, GM, TW, AFMK, MAS and AGM were involved
in the study conception and design. SaC, MB, SiC, VP, AA, EF, RF
and AGM were involved in treatment planning, analysis and
interpretation of the data. MB, FD, EF, RF, SaC and AGM drafted the
article. TW, AFMK, MAS and AGM performed critical revision of the
article for important intellectual content.
Ethics approval and consent to
participate
Patients written informed consent for the use of
their data and CT images to perform this analysis was sought prior.
The institutional ethical committee board approved the study.
Patient consent for publication
Patients written informed consent for the use of
their data and CT images to perform this analysis was sought
prior.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
American College of Radiology: ACR
practice parameter for 3D external beam radiation planning and
conformal therapy. 2016.https://www.acr.org/-/media/ACR/Files/Practice-Parameters/3DConformal.pdfMarch
1–2018
|
|
2
|
Zubizarreta EH, Fidarova E, Healy B and
Rosenblatt E: Need for radiotherapy in low and middle-income
countries-the silent crisis continues. Clin Oncol (R Coll Radiol).
27:107–114. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Page BR, Hudson AD, Brown DW, Shulman AC,
Abdel-Wahab M, Fisher BJ and Patel S: Cobalt, linac, or other: What
is the best solution for radiation therapy in developing countries?
Int J Radiat Oncol Biol Phys. 89:476–480. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
National Comprehensive Cancer Network:
NCCN clinical practice guidelines in oncology: Pancreatic
adenocarcinoma. Version 3. 2017.http://www.nccn.org/professionals/physician_gls/f_guidelines.aspMarch
1–2018
|
|
5
|
Buwenge M, Marinelli A, Deodato F, Macchia
G, Wondemagegnhu T, Salah T, Cammelli S, Uddin Kamal AFM, Sumon MA,
Donati CM, et al: Definition of fields margins for palliative
radiotherapy of pancreatic carcinoma. Mol Clin Oncol. 8:715–718.
2018.https://doi.org/10.3892/mco.2018.1605PubMed/NCBI
|
|
6
|
Morgan-Fletcher SL: Prescribing, recording
and reporting photon beam therapy (Supplement to ICRU Report 50),
ICRU Report 62. ICRU, pp. ix+ 52, 1999 (ICRU Bethesda, MD) $65.00
ISBN 0-913394-61-0. British Journal of Radiology. 74:294. 2001.
View Article : Google Scholar
|
|
7
|
Bentzen SM, Constine LS, Deasy JO,
Eisbruch A, Jackson A, Marks LB, Ten Haken RK and Yorke ED:
Quantitative Analyses of Normal Tissue Effects in the Clinic
(QUANTEC): An introduction to the scientific issues. Int J Radiat
Oncol Biol Phys. 76 3 Suppl:S3–S9. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cheng CW, Chin LM and Kijewski PK: A
coordinate transfer of anatomical information from CT to treatment
simulation. Int J Radiat Oncol Biol Phys. 13:1559–1569. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Flickinger JC and Deutsch M: Manual
reconstruction of tumor volumes from CT scans for radiotherapy
planning. Radiother Oncol. 14:151–158. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rutten EH, Abma W and van Erning L:
Digiplot: A PC programme for drawing tumor volumes for radiation
therapy treatment planning using computer tomography images.
Radiother Oncol. 24:117–119. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Morganti AG, Marinelli A, Buwenge M,
Macchia G, Deodato F, Massaccesi M, Kigula-Mugambe J, Wondemagegnhu
T, Dawotola D, Caravatta L, et al: Palliative two-dimensional
radiotherapy of pancreatic carcinoma: A feasibility study. Tumori.
99:488–492. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Morganti AG, Trodella L, Valentini V,
Barbi S, Macchia G, Mantini G, Turriziani A and Cellini N: Pain
relief with short term irradiation in locally advanced carcinoma of
the pancreas. J Palliat Care. 19:258–262. 2003.PubMed/NCBI
|
|
13
|
Crane CH, Abbruzzese JL, Evans DB, Wolff
RA, Ballo MT, Delclos M, Milas L, Mason K, Charnsangavej C, Pisters
PW, et al: Is the therapeutic index better with gemcitabine-based
chemoradiation than with 5-fluorouracil-based chemoradiation in
locally advanced pancreatic cancer? Int J Radiat Oncol Biol Phys.
52:1293–1302. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pisters PW, Wolff RA, Janjan NA, Cleary
KR, Charnsangavej C, Crane CN, Lenzi R, Vauthey JN, Lee JE,
Abbruzzese JL and Evans DB: Preoperative paclitaxel and concurrent
rapid-fractionation radiation for resectable pancreatic
adenocarcinoma: Toxicities, histologic response rates, and
event-free outcome. J Clin Oncol. 20:2537–2544. 2002. View Article : Google Scholar : PubMed/NCBI
|