Introduction
Sinonasal undifferentiated carcinoma (SNUC) is a
rare malignancy with neuroendocrine differentiation accounting for
nearly 5% of all sinonasal malignancies (1). SNUC is a distinct clinicopathologic
entity that must be distinguished from other sinonasal
malignancies.
SNUC arises in the nasal cavity and is usually
locally advanced when first diagnosed (2). Presenting symptoms depend on the
primary site and often include epistaxis, bloody rhinorrhea, visual
changes, nasal obstruction, headache, and facial pain (3).
Clinically positive regional lymph nodes are present
at diagnosis in 10 to 30% of patients (4). Although distant metastases are uncommon
at presentation, their occurrence has been often reported mainly
involving the lungs and bones (2).
The presence of a sole metastasis to the liver at diagnosis in a
patient with SNUC is unusual and only a few cases have been
reported in the literature. In this article, we report the case of
a 50-year-old woman presenting with nasal obstruction and diagnosed
with a liver metastasis from SNUC.
Case report
A 50-year-old women presented to the Otolaryngology
Department of our University reporting a three-month progressively
worsening history of left maxillary swelling with mild facial pain
and left nasal obstruction. The patient denied recent history of
epistaxis, abdominal pain or previous virus-related hepatitis. No
alcohol consumption or smoking were reported.
Otolaryngologic examination showed a painful, tough
swelling in the left maxillary region. No periorbital proptosis,
cranial nerve palsy or paresthesia were found. Neck examination
showed the presence of palpable nodes in the submandibular level
adherent to the underlying structures. Fiberoptic examination
showed a reddish mass in the middle meatus, arising from the medial
wall of the maxillary sinus; no signs of recent bleeding were
observed.
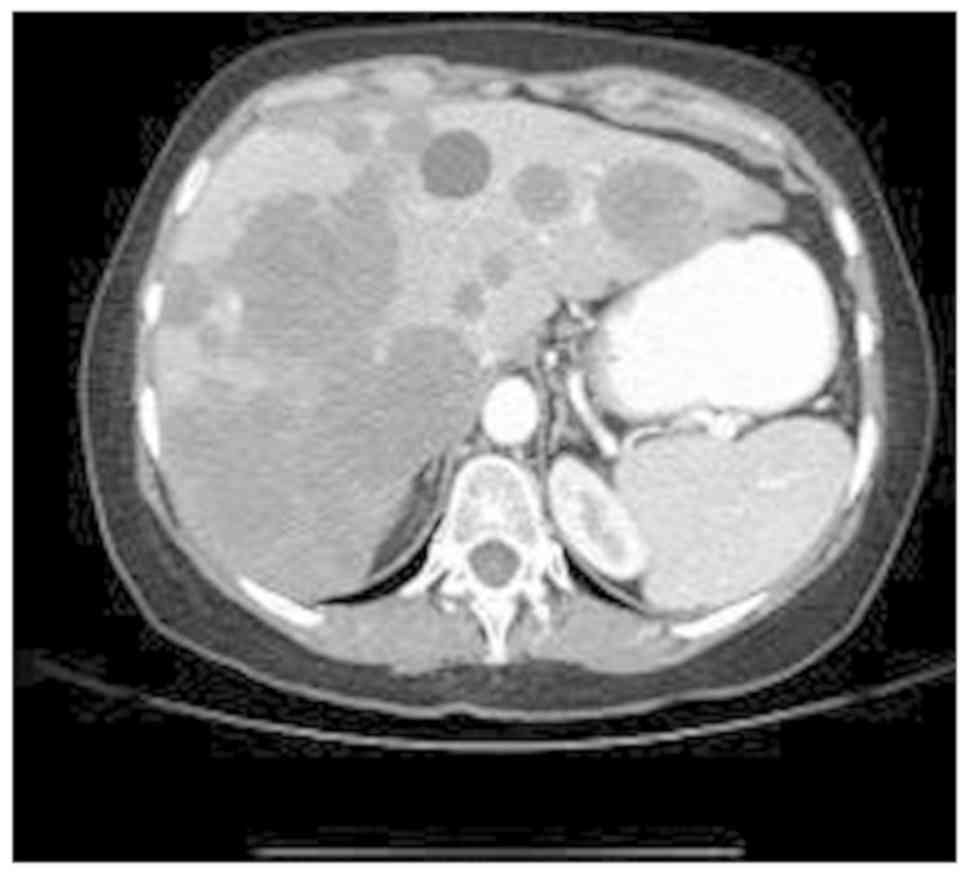
A total body computed tomography (CT) scan with
iodine contrast was performed. The exam showed a soft tissue mass
in the left maxillary sinus measuring 4.6×4.1 cm and extending to
the nasal cavity, with signs of bone erosion in the medial and
anterior wall of the maxillary sinus. Contrast enhancement was
uniformly distributed in the neoplastic tissue (Fig. 1). Necrotic lymph nodes were present
in the left submandibular angle near the jugular digastric region.
Abdominal CT scan showed multiple liver expansive lesions localized
in the right lobe (Fig. 2). No CT
features of liver cirrhosis or hepatocellular carcinoma were
present.
A18F-FDG PET/CT scan was performed to
exclude the presence of further distant metastasis and no
additional localization of the disease were observed (Fig. 3).
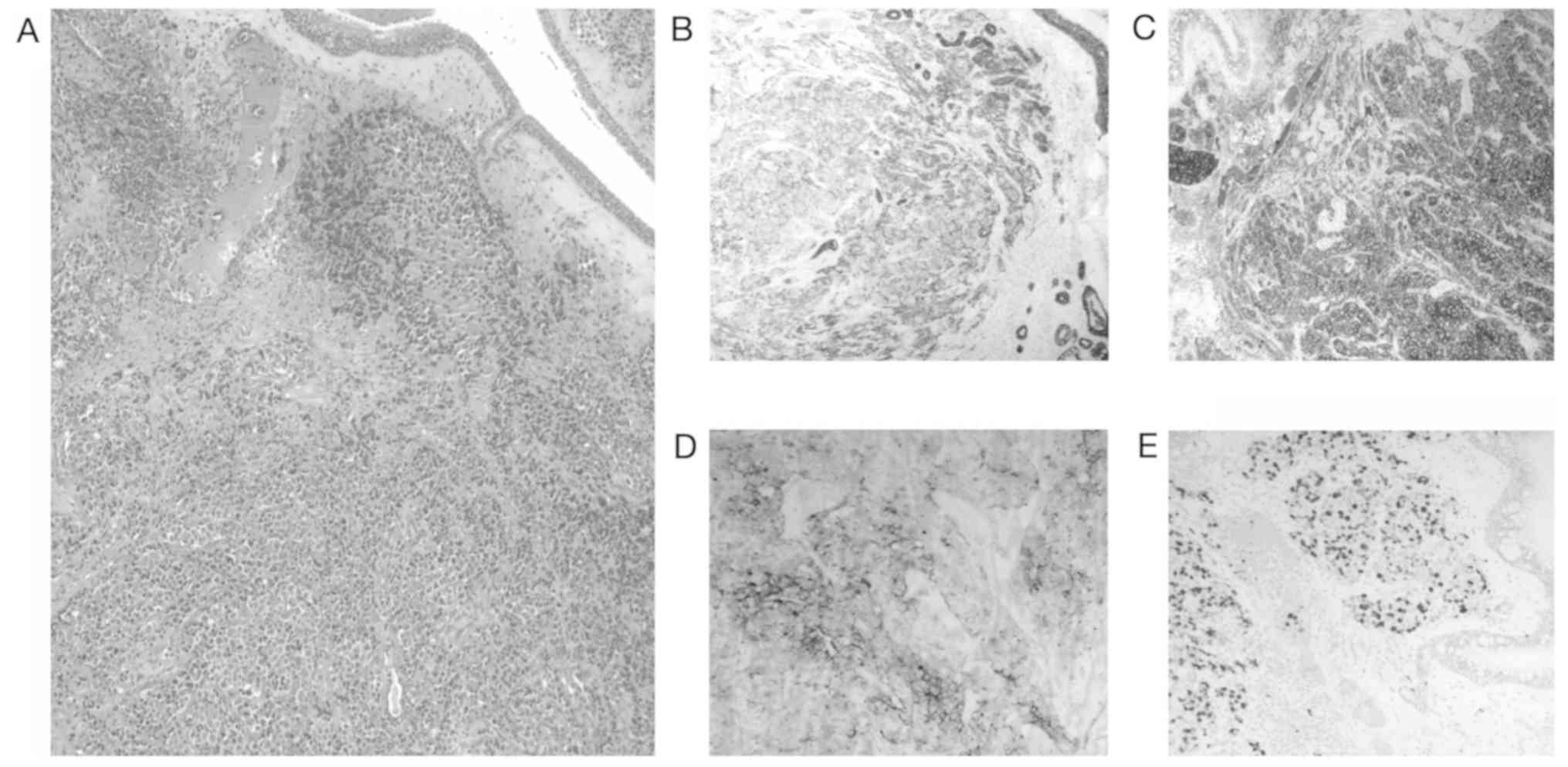
After informing the patient, biopsies of both nasal
and liver tissues were performed. Biopsy of the left maxillary
sinus showed massive infiltration of undifferentiated epithelial
neoplastic cells, with scarce cytoplasm and enlarged nucleus,
organized in nests of cells and surrounded by a fibrous stroma.
High mitotic activity without necrotic areas was present.
Immunohistochemical assay confirmed the diagnosis of
undifferentiated maxillary sinus carcinoma (Fig. 4).
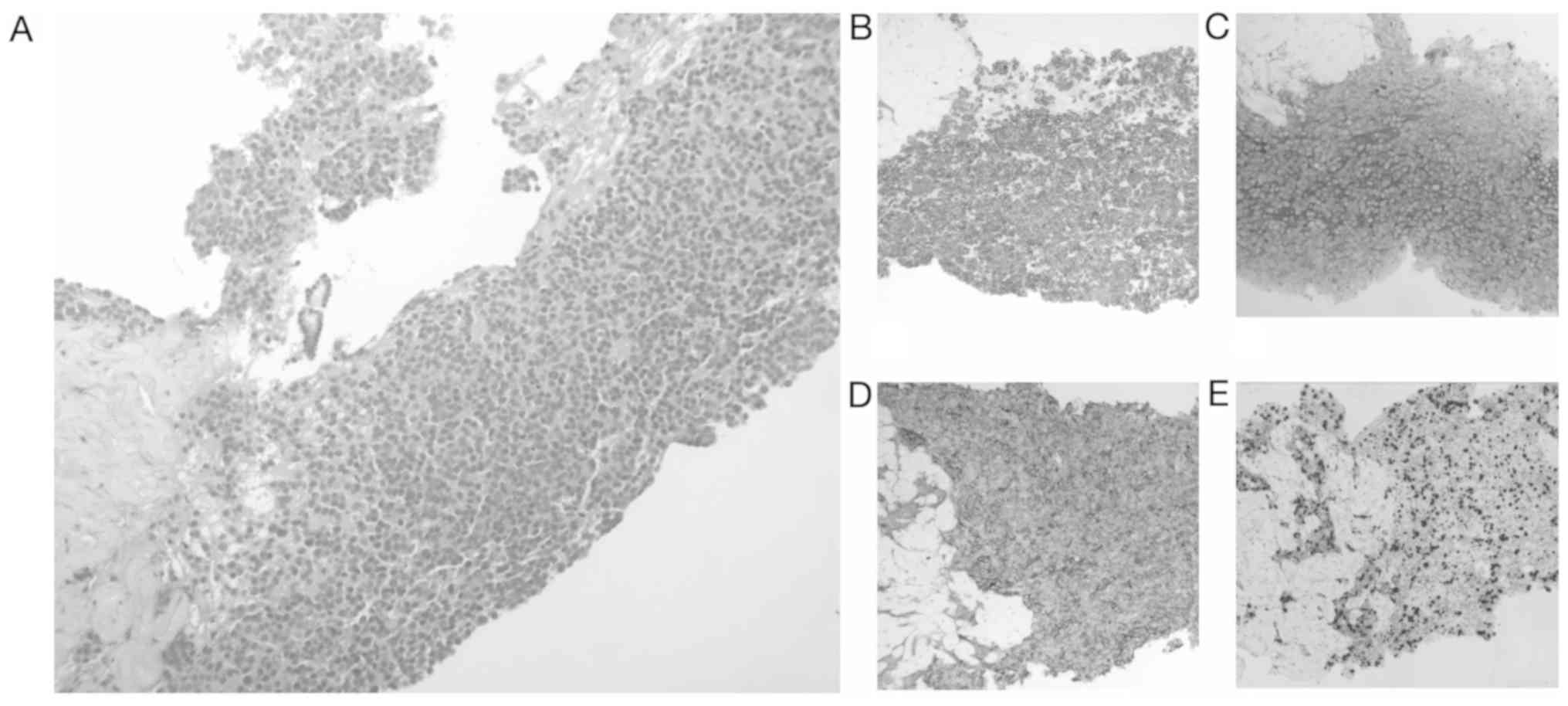
Ultrasound-guided percutaneous liver biopsy of the
largest lesion revealed nests of cells with irregular margins and
slightly eosinophilic cytoplasm, with enlarged nuclei and
basophilic inclusions. Immunohistochemical analysis revealed
positivity for CK MNF 116, CK7 CK8 NSE and CEA. Proliferation cell
index evaluated through Ki-67 was nearly 60%. No signs of
cirrhosis, hepatocellular carcinoma features and additional masses
in the surrounding hepatic parenchyma were found (Fig. 5). According to these findings, a
diagnosis of metastatic SNUC was made.
After multidisciplinary discussion of the case,
surgery was excluded due to presence of liver metastases, and
induction chemotherapy followed by a chemo-radio therapy was
proposed. The patient underwent 6 cycles of chemotherapy with
carboplatin plus taxol before radiation therapy (2 Gy/die-33
cycles). Although induction chemotherapy was able to reduce both
nasal and liver masses, the patient died shortly after.
Discussion
SNUC is a rare malignancy first described by
Frierson et al (5) in 1986.
The etiology of SNUC is unknown; however, it is believed that the
tumor arises from malignant epithelial cells in the nasal mucosa
(5). SNUC occurs most predominantly
in males, suggesting etiological involvement of sexual hormones,
smoking or occupational hazards (6).
The classification of this condition as a specific
identity is still debated and nomenclature is often ambiguous.
Thus, the application of a uniform classification system for
neuroendocrine carcinoma of the head and neck is required (7). Nowadays, SNUC is considered to be part
of the spectrum of neuroendocrine carcinomas including
esthesioneuroblastoma, neurondocrine carcinoma, and small cell
carcinoma (8). While
esthesioneuroblastoma is considered a neuroectodermal malignancy,
sinonasal neuroendocrine carcinoma (SNC) must be considered an
epithelial malignancy and should be classified based on
differentiation grade into well, moderately and poorly
differentiated. Moreover, poorly differentiated SNC are further
subdivided into a small and large cell variant (4). Thus, histological diagnosis of these
malignancies always requires carefully assessment of the specimen
by an expert pathologist.
The prognosis of SNUC is better than small cell
carcinoma, similar to neuroendocrine carcinoma, and worse than
esthesioneuroblastoma (8). Prognosis
in influenced by the lack of specific symptoms leading to delayed
diagnosis (4); nearly 75% of SNUC
patients present with a stage IV disease.
SNUC shows higher propensity to nodal and distant
metastasis compared to other sinonasal malignancies (9). metastases can be found in unexpected
organs due to dissemination via collateral venous plexuses. The
presence of metastasis in the liver from the sinonasal region
without further localizations, as reported in this case, is quite
uncommon. In fact, the hematogenous spread of metastases to the
liver would typically require passage through the lungs before
entering the liver via the hepatic artery; therefore the exclusion
of other metastases is essential (10). The absence of lung metastases, as in
the present case, could be explained by dissemination via the
vertebral venous plexus and its numerous anastomoses with the
azygos veins, which constitute a longitudinal network parallel to
the inferior vena cava (10). In
this case, tumor cells may have reached the liver via the portal
system through the azygos and peri-oesophageal veins although other
collateral pathways cannot be excluded.
A recent paper reported a case of a patient with
metastatic SNUC with a single metastasis in the liver. The authors
reported surgical resection of the liver followed by an orthotopic
liver transplantation. The patient underwent a post-transplantation
immuno-suppressive regimen followed by systemic adjuvant
chemotherapy. However, the follow-up period was limited to 13
months and the chemotherapy regimen was not reported (11).
Another case of solitary liver metastasis from an
ethmoid sinus adenocarcinoma has been reported. The patient was
treated with endonasal tumor resection, followed by external beam
radiotherapy with a dose fractionation of 60 Gy in 30 fractions
over 6 weeks. After about 3 years of follow-up, a single liver
metastasis of intestinal-type adenocarcinoma was detected and
treated by partial hepatectomy without adjuvant therapy (10).
Due to the common delayed diagnosis, treatment of
SNUC is multimodal. For locally advanced stages, open craniofacial
resection has been proposed as the main treatment for a long time
(6), although the introduction of
endoscopic sinus and skull base surgery has modified the surgical
options.
Radiotherapy should always be considered as part of
treatment in the postoperative setting. Moreover, the addition of
chemotherapy to radiotherapy seems to provide a survival advantage,
although evidence is limited and still controversial (6). In fact, although SNUC is considered a
chemo-sensitive disease, data about responses to induction
chemotherapy are limited. The use of induction chemotherapy may
improve both locoregional control and decrease distant metastases
(12) and provides a rationale for
the use of both induction and concurrent chemotherapy.
The role of chemotherapy in metastatic SNUC has not
been clearly established yet (10).
The administration of a platinum-base chemotherapy concurrent with
radiation has been demonstrated to improve locoregional control and
survival and has been the mainstream of treatment in many
institutions for metastatic SNUC (12). Moreover, platinum-base chemotherapy
had been associated with additional drugs, such as etoposide and
taxol, to improve local control.
In conclusion, SNUC is a rare malignancy with
neuroendocrine differentiation. Since the tumor arises in the nasal
cavity, patients generally present nonspecific symptoms such as
nasal obstruction and epistaxis, thus SNUC is often locally
advanced or metastatic when first diagnosed. Metastatic SNUC should
always be suspected in patients with locally advanced SNUC;
metastases can be found in unexpected organs due to dissemination
via collateral venous plexuses.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
VD and MR wrote the manuscript. VD, MR, AG and MDV
contributed to the treatment of the case. BC reviewed histological
specimens. All authors read and approved the manuscript.
Ethics approval and consent to
participate
Written informed consent for the publication of any
associated data and accompanying images was obtained from the
patients or their guardians.
Patient consent for publication
The patient provided written informed consent for
the publication of their data in this study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mitchell EH, Diaz A, Yilmaz T, Roberts D,
Levine N, DeMonte F, Hanna EY and Kupferman ME: Multimodality
treatment for sinonasal neuroendocrine carcinoma. Head Neck.
34:1372–1376. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mendenhall WM, Mendenhall CM, Riggs CE Jr,
Villaret DB and Mendenhall NP: Sinonasal undifferentiated
carcinoma. Am J Clin Oncol. 29:27–31. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Musy PY, Reibel JF and Levine PA:
Sinonasal undifferentiated carcinoma: The search for a better
outcome. Laryngoscope. 112:1450–1455. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
van der Laan TP, Iepsma R, Witjes MJ, van
der Laan BF, Plaat BE and Halmos GB: Meta-analysis of 701 published
cases of sinonasal neuroendocrine carcinoma: The importance of
differentiation grade in determining treatment strategy. Oral
Oncol. 63:1–9. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Frierson HF Jr, Mills SE, Fechner RE, Taxy
JB and Levine PA: Sinonasal undifferentiated carcinoma. An
aggressive neoplasm derived from schneiderian epithelium and
distinct from olfactory neuroblastoma. Am J Surg Pathol.
10:771–779. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Morand GB, Anderegg N, Vital D, Ikenberg
K, Huber GF, Soyka MB, Egger M and Holzmann D: Outcome by treatment
modality in sinonasal undifferentiated carcinoma (SNUC): A
case-series, systematic review and meta-analysis. Oral Oncol.
75:8–34. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
van der Laan TP, Bij HP, van Hemel BM,
Plaat BE, Wedman J, van der Laan BF and Halmos GB: The importance
of multimodality therapy in the treatment of sinonasal
neuroendocrine carcinoma. Eur Arch Otorhinolaryngol. 270:2565–2568.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rosenthal DI, Barker JL Jr, El-Naggar AK,
Glisson BS, Kies MS, Diaz EM Jr, Clayman GL, Demonte F, Selek U,
Morrison WH, et al: Sinonasal malignancies with neuroendocrine
differentiation: Patterns of failure according to histologic
phenotype. Cancer. 101:2567–2573. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Castelnuovo P, Turri-Zanoni M, Battaglia
P, Antognoni P, Bossi P and Locatelli D: Sinonasal malignancies of
anterior skull base: Histology-driven treatment strategies.
Otolaryngol Clin North Am. 49:183–200. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Caselhos S, Ferreira C, Jácome M and
Monteiro E: Liver metastasis of ethmoid sinus adenocarcinoma. Eur
Ann Otorhinolaryngol Head Neck Dis. 132:157–159. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
De Simone P, Coletti L, Campani D, Falcone
A and Filipponi F: Liver transplantation for metastatic sinonasal
undifferentiated carcinoma: A case report. Transplant Proc.
40:3821–3822. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rischin D, Porceddu S, Peters L, Martin J,
Corry J and Weih L: Promising results with chemoradiation in
patients with sinonasal undifferentiated carcinoma. Head Neck.
26:435–441. 2004. View Article : Google Scholar : PubMed/NCBI
|