Introduction
Osteochondroma (OC) or osteocartilagenous exostosis,
a cartilage-capped osseous lesion that protrudes from the surface
of the affected bone, is the most common tumor of the axial
skeleton, accounting for 35–50% of benign bone tumors, and 8–15% of
bone tumors overall (1,2). OC frequently arises from the long bones
(3), such as the proximal metaphysis
of the tibia or the distal metaphysis of the femur, and rarely
occurs in the craniofacial region (<1% of cases) (4,5). The
embryonic development of the mandibular condyle from cartilaginous
ossification makes it the most frequent facial site of this type of
tumor (5). Although extremely rare,
involvements of the coronoid process (6), the posterior maxillary region (7), the maxillary sinus (8) and the body (9), symphysis (10) and ramus of the mandible (11) were also reported. Different from OCs
of the long bones, craniofacial OCs occur at older ages (mean age,
36.4 years), and grow slowly long after the end of puberty
(12). The etiology of the tumor is
not fully understood, and the most accepted theory was hypothesized
by Lichtenstein (13), which
suggests that periosteum had the pluripotentiality to give rise to
chondroblasts or osteoblasts, and that OC results from metaplastic
change in the periosteum.
The present study reviewed the literature concerning
coronoid OCs from 1989–2018 and also describes the case of a
patient treated surgically and followed up for 21 months in the
Hospital of Stomatology (Guangzhou, Guangdong, China). The case
involved a giant OC on the coronoid process, and the patient
presented with facial asymmetry and a limited ability to open her
mouth.
Case report
A 34-year-old woman presented to the Hospital of
Stomatology with progressive restriction of mouth opening over a
period of 20 years and facial asymmetry with swelling in the right
zygomatic region within the past 2 years. No history of trauma was
reported. A physical examination revealed swelling in the right
zygomatic arch region, facial asymmetry and the ability to open
their mouth only 5 mm. There were no associated temporomandibular
joint (TMJ) complaints such as pain or clicking when opening their
mouth.
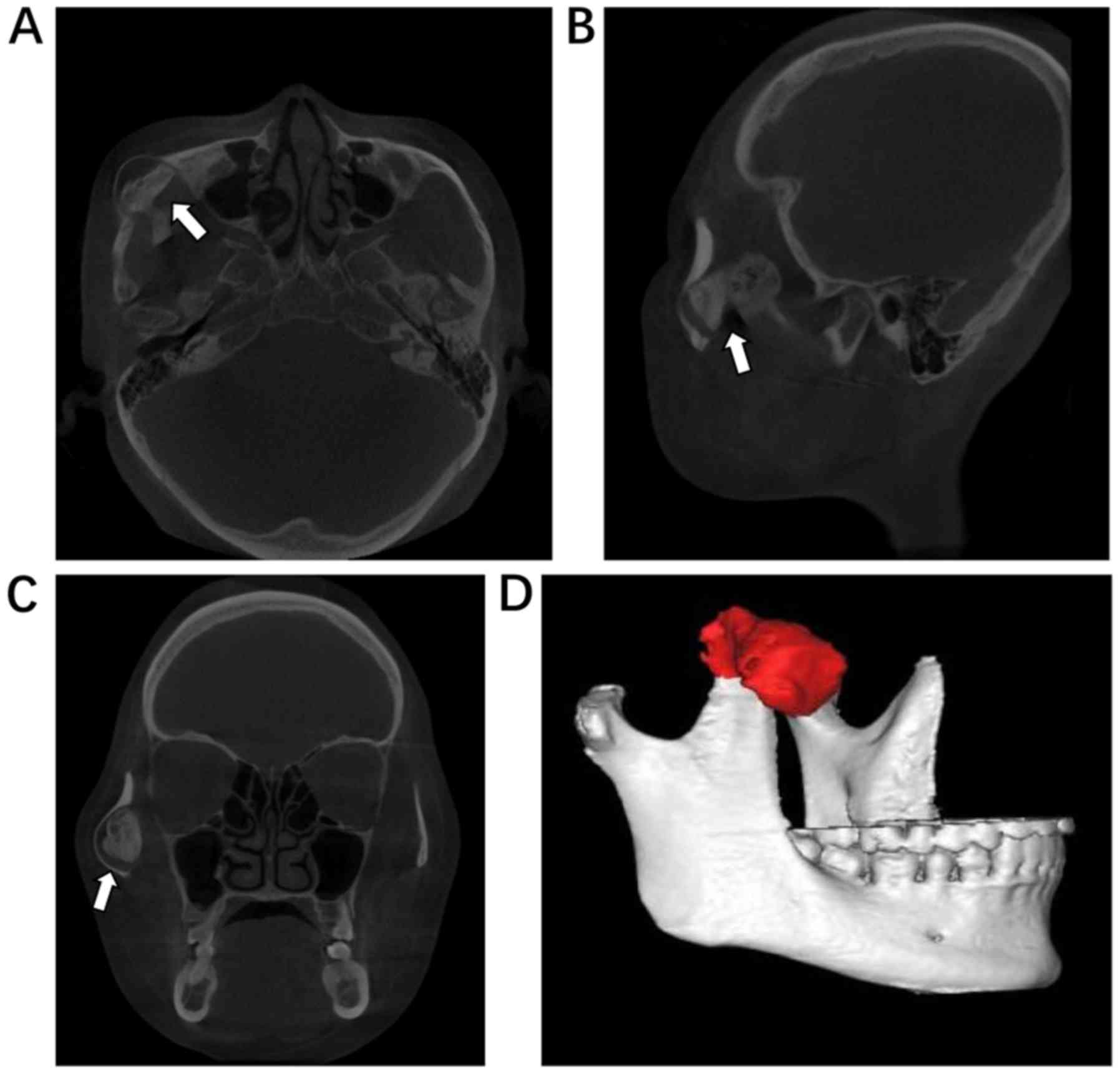
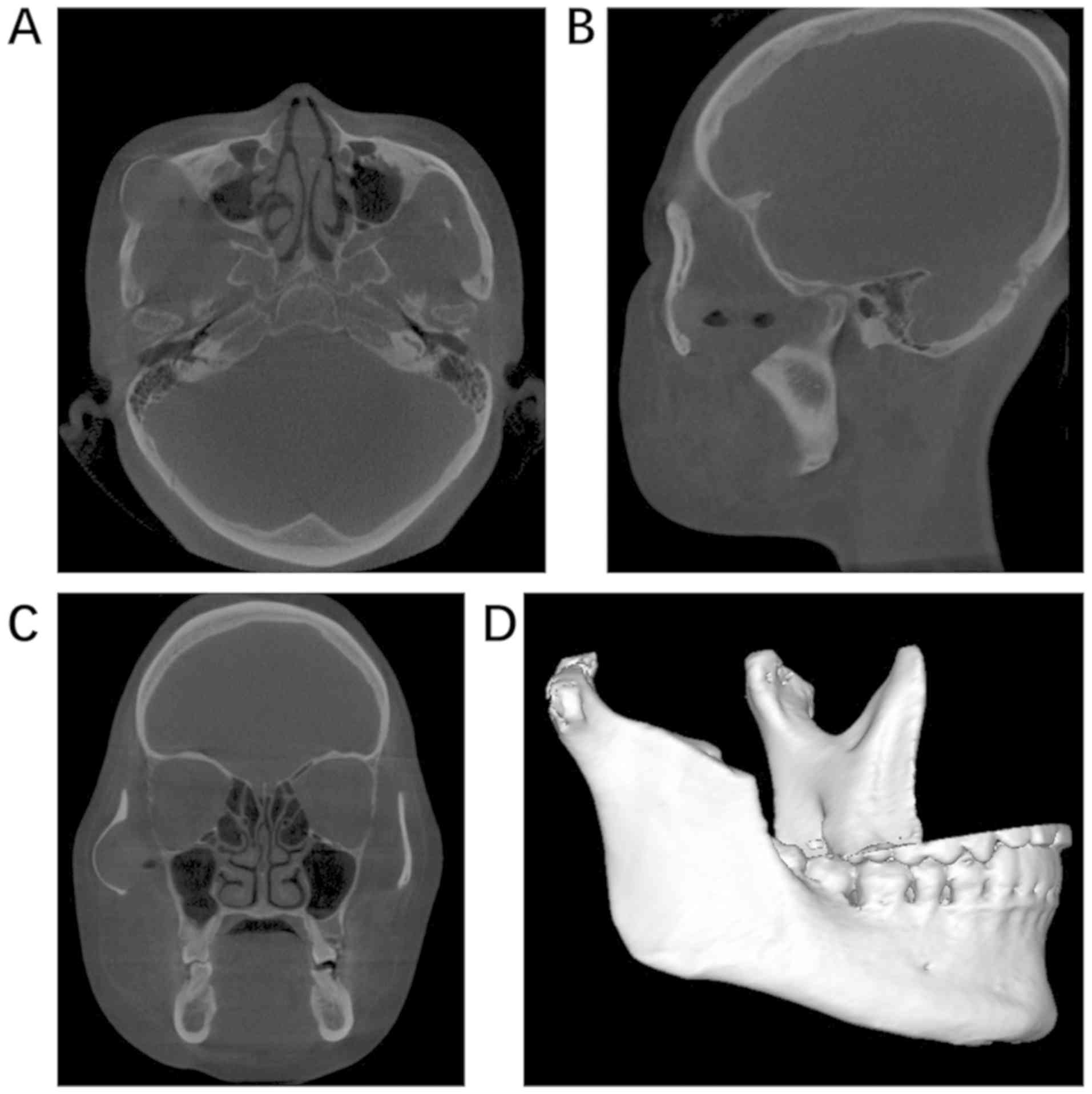
A panoramic radiograph showed an enlarged right
coronoid process (Fig. 1). Cone-beam
computed tomography (CBCT) revealed a mushroom-shaped outgrowth
from the lateral aspect of the coronoid process to the inner
surface of the zygomatic arch, with outward expansion, forming a
pseudojoint (Fig. 2). A diagnosis of
OC of the right coronoid process was made according to the clinical
and radiographic features. The patient was then scheduled for right
coronoidectomy, performed through an intraoral approach as
previously described (5,14).
Considering that the patient suffered from a serious
limitation of mouth opening, all procedures were conducted under
general anesthesia via naso-tracheal intubation. The patient was
taken to the operating room and, after naso-tracheal intubation,
was prepped and draped for transoral incisions. An incision was
made along the anterior border of the ramus to the tip of the
coronoid process. The mucoperiosteal flaps were raised superiorly
to the sigmoid notch and lower portion of the coronoid, and by
blunt dissection, the coronoid process and the tumor were
visualized. The tumor and the coronoid process were removed without
difficulty using a fissure bur and a chisel.
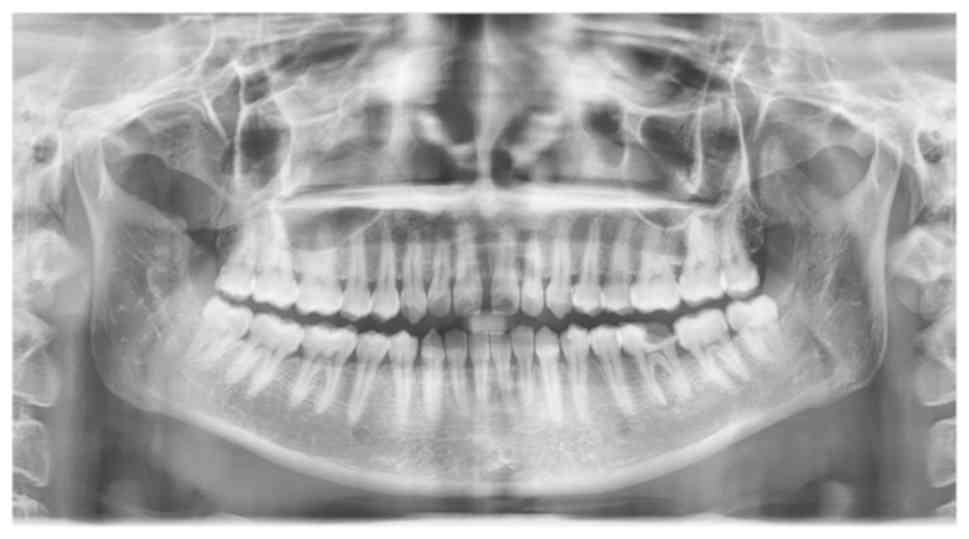
Post-operative panoramic radiograph and CBCT showed
that the tumor and the right coronoid process were totally excised
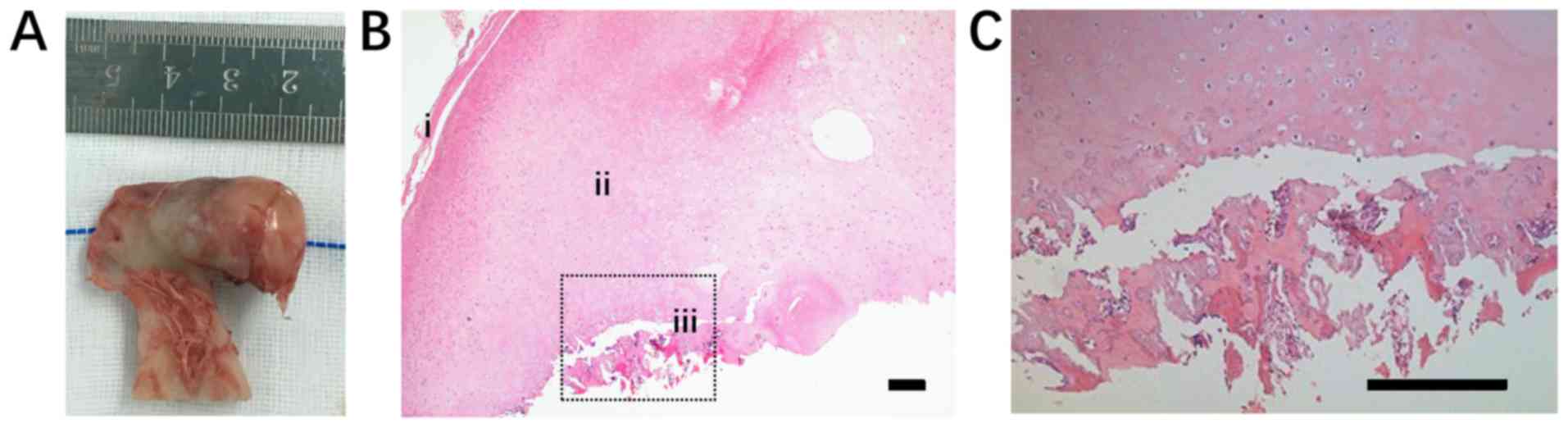
(Figs. 3 and 4). The mass measured ~4×1.5×1.5 cm
(Fig. 5A). Histologically, the tumor
showed the presence of three layers from the surface to the inside:
Fibrous tissue, cartilaginous tissue and cancellous bone (Fig. 5B and C), which confirmed the
diagnosis of OC. Three highly qualified pathologists made the
diagnosis independently. Hematoxylin staining was performed as
follows: The specimen was fixed in 4% paraformaldehyde at 4°C for
24 h and transferred to 19% ethylene diamine tetraacetic acid
(EDTA) solution for decalcification at room temperature for ~2
months. After thoroughly decalcification, the specimen was then
dehydrated as follows: 70% ethanol (60 min), 80% ethanol (40 min),
95% ethanol (30 min), 100% ethanol (25 min) at room temperature,
and embedded in paraffin. Following embedding, the specimen was
sliced sagitally in to 7-µm thick slices. The slices were
deparaffinized in xylene, rehydrated in 100% ethanol, 95% ethanol,
80% ethanol and 70% ethanol for 2 min each, and then stained with
hematoxylin and eosin for 1 min, all at room temperature.
Postoperatively, the patient was able to open their
mouth 36 mm. After a follow-up period of 21 months, there was no
evidence of recurrence and the patient was asymptomatic. The
patient is still being followed up every 6 months, and the
follow-up will be performed over an extended period.
Literature review
The present review was performed using a
computer-assisted search of Medline Industries, Inc. (www.medline.com). The literature published in the
English language on OC of the mandibular coronoid process from
January 1989 to December 2018, concerning clinical characteristics,
histopathological features and treatment, were reviewed. The
criterion for inclusion was any case with a histopathological
description or photomicrograph indicating OC. Cases were excluded
if histopathological characteristics of the lesion were not shown,
even those with a diagnosis of OC.
The review of the literature revealed only 39
reports of OC involving the coronoid process within the last 30
years (5,6,15–48),
plus the present case (Tables I and
II). The median age at onset was
28.7 years (range, 5–57 years), with the largest number of cases
observed in patients 20–30 years old. Men were more commonly
diagnosed (66.7%) than women. Unilateral masses were more
frequently described (32 cases, 82.1%) and a slight tendency for
involvement of the left coronoid process (51.3%) was revealed.
These findings were generally in agreement with previous studies
(6,28).
 | Table I.Clinical characteristics, treatments
and outcomes of cases of coronoid osteochondromas reported in
Medline. |
Table I.
Clinical characteristics, treatments
and outcomes of cases of coronoid osteochondromas reported in
Medline.
| First author/s,
year | Age, years | Sex | Location | Symptoms | Surgical
approach | Follow-up,
months | Recurrence | (Refs.) |
|---|
| Mohan Choontharu
et al, 2018 | 16 | F | Left | A | Intraoral | 6 | None | (48) |
| Mohanty et
al, 2016 | 18 | M | Right | LMO, A | Extraoral | 36 | None | (47) |
| Dandriyal et
al, 2015 | 20 | M | Left | LMO, P | Intraoral | 54 | None | (5) |
| Sawada et
al, 2015 | 14 | M | Left | LMO | Intraoral | 6 | None | (46) |
| Losa-Munoz et
al, 2014 | 42 | M | Right | LMO, A | Intraoral | NA | NA | (45) |
| Fan et al,
2014 | 20 | M | Left | LMO, A | Combined | 20 | None | (44) |
| Stringer et
al, 2013 | 27 | M | Left | LMO, A | Intraoral | NA | None | (43) |
| Aoki et al,
2013 | 18 | M | Right | A, P | Intraoral | 15 | None | (42) |
| Ruiz and Lara,
2012 | 28 | M | Bilateral | LMO | Combined | 36 | None | (41) |
| Ajila et al,
2012 | 28 | M | Left | LMO, A | Intraoral | 12 | None | (40) |
| Coll-Anglada et
al, 2011 | 52 | F | Right | LMO, A | Intraoral | 6 | None | (38) |
| D'Ambrosio et
al, 2011 | 39 | M | Left | LMO | Intraoral | Several years | None | (39) |
| Acosta-Feria et
al, 2011 | 55 | M | Right | LMO, A | Extraoral | 20 | None | (37) |
| Sreeramaneni et
al, 2011 | 45 | F | Left | LMO, A | Combined | 3 | None | (6) |
| Yesildag et
al, 2010 | 16 | M | Right | LMO, A | Extraoral | 14 | None | (36) |
| Zhong et al,
2009 | 39 | F | Bilateral | LMO, A | Intraoral | 9 | None | (35) |
| Etoz et al,
2009 | 43 | F | Right | LMO, A | Intraoral | 6 | None | (33) |
| Thota et al,
2009 | 15 | M | Bilateral | LMO, A | Intraoral | 14 | None | (34) |
| Dede et al,
2007 | 20 | M | Bilateral | LMO, A | Intraoral | NA | NA | (32) |
| Akan and
Mehreliyeva, 2006 | 24 | M | Bilateral | LMO | Intraoral | NA | NA | (30) |
| Villanueva et
al, 2006 | 44 | F | Left | LMO, A | Intraoral | 10 | None | (31) |
| Capote et
al, 2005 | 23 | F | NA | LMO, A, P | Intraoral | 12 | None | (29) |
| Emekli et
al, 2002 | 21 | M | Right | LMO, A, P | Extraoral | NA | NA | (27) |
|
| 26 | F | Right | LMO, A | Intraoral | 6 | None |
|
| Escuder et
al, 2001 | 24 | M | Left | LMO, A | Intraoral | NA | NA | (26) |
|
| 16 | NA | Bilateral | LMO | Intraoral | 12 | None |
|
| Roychoudhury et
al 2002 | 32 | M | Left | LMO, A | Extraoral | 12 | None | (28) |
| Hernandez-Alfaro
et al, 2000 | 22 | M | Left | LMO, A | Extraoral | NA | NA | (25) |
| Chichareon et
al, 1999 | 5 | M | Right | LMO, A | NA | NA | NA | (24) |
| Manganaro,
1998 | 26 | F | Left | LMO, A | Intraoral | Several weeks | None | (23) |
| Chen et al,
1998 | 57 | F | Left | LMO, A | Extraoral | 72 | None | (22) |
| Gross et al,
1997 | 22 | M | Left | LMO, A | NA | NA | NA | (21) |
| Constantinides
et al 1997 | 31 | M | Right | LMO, A | Extraoral | 12 | None | (20) |
| Kermer et
al, 1996 | 40 | M | Left | LMO, A | Extraoral | NA | NA | (19) |
| Çenetoğlu et
al, 1996 | 19 | M | Left | LMO, A | Intraoral | NA | NA | (18) |
| Kerscher et
al, 1993 | 45 | M | Left | LMO | Intraoral | NA | NA | (17) |
| Asanami et
al, 1990 | 17 | M | Left | LMO, A | Combined | NA | NA | (15) |
| Totsuka et
al, 1990 | 37 | F | Left | LMO, A | Intraoral | NA | NA | (16) |
| Present study | 34 | F | Right | LMO, A | Intraoral | 21 | None |
|
 | Table II.Summary of clinical features of
coronoid osteochondromas. |
Table II.
Summary of clinical features of
coronoid osteochondromas.
| Clinical
features | Value |
|---|
| Side, n (%) |
|
|
Left | 20 (51.3) |
|
Right | 12 (30.8) |
|
Bilateral | 6 (15.4) |
| NA | 1 (2.6) |
| Sex, n (%) |
|
|
Male | 26 (66.7) |
|
Female | 12 (30.8) |
| NA | 1 (2.6) |
| Age, years |
|
|
Mean | 28.7 |
|
Range | 5–57 |
| Symptoms, n
(%) |
|
|
Limitation of mouth
opening | 37 (94.9) |
|
Asymmetry | 32 (82.1) |
|
Pain | 4 (10.3) |
As mentioned in several reported cases, the disease
was predominately characterized by a lengthy history (ranging from
3 months to 20 years) of progressive reduction in the ability of
mouth opening (37 cases, 94.9%). Later signs included total trismus
and appreciable swelling in the zygomatic region, visible as facial
asymmetry (32 cases, 82.1%). Pain was not a common symptom (4
cases, 10.3%).
Panoramic radiography usually showed a sessile or
pedunculated bony mass in the affected coronoid process. Water's
view may be useful in identifying coronoid tumors and their
relation to the wall of the maxillary sinus and the zygoma
(25). To visualize the exact shape,
location and density of the tumor, 3-dimensional CT and CBCT were
performed and are considered as the ‘gold standard’ for an accurate
diagnosis (6,36). A pseudojoint formation between the
mass and the protruded zygoma (Fig.
2) was observed in the majority of the cases (38 cases, 97.4%),
a condition that was first described by Oscar Jacob in 1899 and was
hence termed Jacob's disease (49).
From the literature, coronoidectomy was recorded as
the preferred treatment. Data on the surgical approaches were
present in 38 cases, and were used as follows: Extraoral in 24.3%
of cases; intraoral in 64.9% of cases and combined intra- and
extraoral approaches in 10.8% cases, with the intraoral approach
used most often.
Follow-up data were included in 25 of the 39 cases
and showed that the prognosis of coronoid OC was excellent, with no
recurrences or malignant transformations reported.
Discussion
An extensive review of the English literature within
the last 30 years revealed a total of 435 patients with OC in the
craniofacial region. The most frequently affected site was the
mandibular condyle (384 cases, 88.3%), followed by the coronoid
process (8.7%). However, involvement of the posterior maxillary
region (7), maxillary sinus
(8), and the body (9), symphysis (10) and ramus (11) of the mandible were also reported. A
previous review of the literature by Sreeramaneni et al
(6) identified 39 cases of coronoid
OC up until December 2010, after which there were only 12 new cases
reported. Reports with only photographic evidence of OC were not
included in the present review.
The pathogenesis of OC has not yet been elucidated.
Langenskiold (50) hypothesized that
such lesions resulted from cells in the undifferentiated layer that
were displaced from the epiphysis to the metaphyseal area. However,
this may only explain the emergence of lesions in the condylar
region. Another theory hypothesized that there were accumulations
of embryonic cells at the points of tendon attachments, and that
the continuous strain on tendons may stimulate the cartilaginous
potential of the embryonic cells (51). The most widely accepted theory was
hypothesized by Lichtenstein (13),
who suggested that pluripotential cells in the periosteum have the
potential to form chondroblasts or osteoblasts and result in
OC.
OCs can occur independently or as part of an
autosomal dominant disorder known as hereditary multiple OC (HMO)
syndrome (41). In the literature,
of the patients with HMO syndrome, only 2 had lesions in the
craniofacial region (41,52). The discrimination of these two types
is important, as sarcomatous changes are rare in solitary OCs
(1–2%), but do occur in 5–25% of HMO cases (53,54).
Due to the rarity of its occurrence and insidious
onset, OC arising from the coronoid process is often overlooked. A
coronoid OC should be suspected when patients present with a
progressively worsening ability to open their mouth and facial
deformity. Due to the limitation in the ability to open the mouth,
it is important to differentiate this disease from TMJ disorders or
masticatory muscle tendon-aponeurosis hyperplasia (55), the latter of which is more rarely
observed clinically.
CT is considered as the gold standard for diagnosing
OC and provides accurate details regarding the location of the
tumor, its density and its relation to adjacent structures
(30,36), all of which are valuable when
planning the course of treatment. However, CT exposes patients to
high doses of radiation, and thus, its use should comply with
appropriate guidelines. For younger patients, or those with small
morphological alternations that can be clearly discerned by image
examinations with less radiation exposure, the unnecessary use of
CT should be prevented. Recently, CBCT, being an ideal substitute
for CT for the diagnosis of abnormalities in the craniofacial
region, has been extensively applied, owing to its lower radiation
dosage. Furthermore, submentovertex projection of the zygomatic
arch permits a clear visual of the coronoid tumor and the zygomatic
arch, which may be more economical and less time consuming for an
early diagnosis of tumors in the coronoid process.
Histologically, OC reveals the presence of bony
trabeculae covered by a cartilaginous cap and fibrous tissue
(56). When considering the
differential diagnosis of OC, the possibilities of other lesions,
such as bizarre parosteal osteochondromatous proliferations,
osteoma, hyperplasia, giant cell tumors and chondroma, must also be
considered (5,57). Rarer bony tumors have included
chondroblastoma, osteoblastoma, chondrosarcoma, osteosarcoma and
metastatic tumors (12).
Different from OCs of the long bone, the majority of
which are asymptomatic and do not require any treatment (12), the functional and cosmetic problems
resulting from OCs of the craniofacial bone necessitate their
resection. The definitive treatment of coronoid OC is
coronoidectomy. No reconstruction of the face is needed, which
contrasts with the requirements for condylar OC. Surgical
approaches primarily include intraoral and extraoral approaches, or
a combination of both techniques. The intraoral approach is more
favorable, as it allows direct access to the coronoid process while
eliminating the potential of injuring the facial nerve and scarring
(27). However, problems may occur
when facing patients with severe trismus, which could prevent or
hinder surgical access. Additionally, if the mass is large and in
close proximity to the zygomatic arch, an extraoral approach allows
better access and visualization (5).
In the present case, although the tumor was extremely large and the
patient presented with a serious limitation of mouth opening,
considering the patient's young age and that the coronoid process
was not firmly trapped in the zygomatic arch, an intraoral approach
was successfully performed.
Recurrence and malignant transformations of OC are
extremely rare (5,12). For OCs in the craniofacial region,
only 6 recurrences (12,58–62) and
2 malignant transformations (63)
were reported. All cases with recurrence of malignant change were
associated with OCs in the extracoronoid region and were initially
treated in a conservative way, namely local resection of the tumor.
The excellent prognostic outcome of treating patients with coronoid
OCs may be due to the relatively radical surgical procedure in
which the tumor, as well as the coronoid process, are removed.
These findings suggest that a complete resection of the tumor
should be ensured to prevent recurrence or malignant change.
In conclusion, a diagnosis of coronoid OC should be
taken into consideration when facing patients with a limited
ability to open their mouth, especially in patients with no other
symptoms. CT or CBCT scans may serve an important role in an
accurate diagnosis. Timely treatment can prevent possible
complications such as facial swelling and asymmetry. Coronoidectomy
is the ideal treatment. The prognosis of the disease is excellent,
as no recurrence or malignant changes were reported.
Acknowledgements
Not applicable.
Funding
The present study was funded by The Science and
Technology Planning Project of Guangzhou, China (grant no.
2015100110268).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
QT and XL conceived and designed the study. XL and
PSL collected the data. XL and PSL wrote the manuscript. TL
critically revised the article, reanalyzed the data, solved
problems with the 3D reconstruction and edited the figures.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent for publication was
provided by the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dahlin DC and Unni KK: Bone tumors:
General aspects and data on 8,542 cases. Thomas. 1985.
|
|
2
|
Zhang J, Wang H, Li X, Li W, Wu H, Miao J
and Yuan X: Osteochondromas of the mandibular condyle: Variance in
radiographic appearance on panoramic radiographs. Dentomaxillofac
Radiol. 37:154–160. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mirra JM, Picci P and Gold RH: Bone
tumors. Clinical, radiologic, and patholo-gic correlation.
Investigat Radiol. 26:6371991.
|
|
4
|
Arora P, Deora SS, Kiran S and Bargale SD:
Osteochondroma of condyle: Case discussion and review of treatment
modalities. BMJ Case Rep. 2014(pii): bcr20132007592014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dandriyal R, Giri KY, Pant S, Alam S and
Joshi A: Giant osteochondroma of the coronoid process. J Maxillofac
Oral Surg. 14 (Suppl 1):S412–S416. 2015. View Article : Google Scholar
|
|
6
|
Sreeramaneni SK, Chakravarthi PS, Krishna
Prasad L, Raja Satish P and Beeram RK: Jacob's disease: Report of a
rare case and literature review. Int J Oral Maxillofac Surg.
40:753–757. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Brady FA, Sapp JP and Christensen RE:
Extracondylar osteochondromas of the jaws. Oral Surg Oral Med Oral
Pathol. 46:658–668. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Traub DJ, Marco WP, Eisenberg E and
Barrows G: Osteochondroma of the maxillary sinus: Report of a case.
J Oral Maxillofac Surg. 48:752–755. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Miyawaki T, Kobayashi M, Takeishi M,
Uchida M and Kurihara K: Osteochondroma of the mandibular body.
Plast Reconstr Surg. 105:1426–1428. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tanaka E, Iida S, Tsuji H, Kogo M and
Morita M: Solitary osteochondroma of the mandibular symphysis. Int
J Oral Maxillofac Surg. 33:625–626. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Anupam M, Shukla GK, Mishra SC, Bhatia N,
Srivastava AN and Mishra N: Unusual solitary osteochondroma of the
mandibular ramus. J Laryngol Otol. 116:65–66. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Vezeau PJ, Fridrich KL and Vincent SD:
Osteochondroma of the mandibular condyle: Literature review and
report of two atypical cases. J Oral Maxillofac Surg. 53:954–963.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lichtenstein L: Bone tumors. Mosby.
1952.
|
|
14
|
Park SH, An JH, Han JJ, Jung S, Park HJ,
Oh HK and Kook MS: Surgical excision of osteochondroma on
mandibular condyle via preauricular approach with zygomatic arch
osteotomy. Maxillofac Plast Reconstr Surg. 39:322017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Asanami S, Kasazaki Y and Uchida I: Large
exostosis of the mandibular coronoid process. Report of a case.
Oral Surg Oral Med Oral Pathol. 69:559–562. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Totsuka Y, Fukuda H, Iizuka T, Shindoh M
and Amemiya A: Osteochondroma of the coronoid process of the
mandible. Report of a case showing histological evidence of
neoplasia. J Craniomaxillofac Surg. 18:27–32. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kerscher A, Piette E, Tideman H and Wu PC:
Osteochondroma of the coronoid process of the mandible. Report of a
case and review of the literature. Oral Surg Oral Med Oral Pathol.
75:559–564. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Çenetoğlu S, Yavuzert R, Oygür T, Akyol G
and Baran NK: Osteochondroma of the coronoid process of the
mandible. Eur J Plast Surg. 19:333–334. 1996. View Article : Google Scholar
|
|
19
|
Kermer C, Rasse M, Undt G and Lang S:
Cartilaginous exostoses of the mandible. Int J Oral Maxillofac
Surg. 25:373–375. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Constantinides M, Lagmay V and Miller P:
Coronoid osteochondroma of the mandible: Transzygomatic access and
autogenous bony reconstruction. Otolaryngol Head Neck Surg.
117:S86–S91. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gross M, Gavish A, Calderon S and Gazit E:
The coronoid process as a cause of mandibular hypomobility-case
reports. J Oral Rehabil. 24:776–781. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chen PK, Chang SC, Huang F, Chen YR, Yeow
VK and Williams WG: Transzygomatic coronoidectomy through an
extended coronal incision for treatment of trismus due to an
osteochondroma of the coronoid process of the mandible. Ann Plast
Surg. 41:425–429. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Manganaro AM: Osteochondroma of the
coronoid process. Gen Dent. 46:92–94. 1998.PubMed/NCBI
|
|
24
|
Chichareon V, Arpornmaeklong P and
Donsakul N: Fibrodysplasia ossificans progressiva and associated
osteochondroma of the coronoid process in a child. Plast Reconstr
Surg. 103:1238–1243. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hernandez-Alfaro F, Escuder O and Marco V:
Joint formation between an osteochondroma of the coronoid process
and the zygomatic arch (Jacob disease): Report of case and review
of literature. J Oral Maxillofac Surg. 58:227–232. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Escuder i de la Torre O, Vert Klok E, Mari
i Roig A, Mommaerts MY and Pericot i Ayats J: Jacob's disease:
Report of two cases and review of the literature. J
Craniomaxillofac Surg. 29:372–376. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Emekli U, Aslan A, Onel D, Cizmeci O and
Demiryont M: Osteochondroma of the coronoid process (Jacob's
disease). J Oral Maxillofac Surg. 60:1354–1356. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Roychoudhury A, Gupta YK, Parkash H and
Karak AK: Jacob disease: Report of a case and review of the
literature. J Oral Maxillofac Surg. 60:699–703. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Capote A, Rodriguez FJ, Blasco A and Munoz
MF: Jacob's disease associated with temporomandibular joint
dysfunction: A case report. Med Oral Patol Oral Cir Bucal.
10:210–214. 2005.(In English, Spanish). PubMed/NCBI
|
|
30
|
Akan H and Mehreliyeva N: The value of
three-dimensional computed tomography in diagnosis and management
of Jacob's disease. Dentomaxillofac Radiol. 35:55–59. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Villanueva J, González A, Cornejo M, Núñez
C and Encina S: Osteochondroma of the coronoid process. Med Oral
Patol Oral Cir Bucal. 11:E289–E291. 2006.PubMed/NCBI
|
|
32
|
Dede U, Tuzuner AM and Kisnisci RS:
Osteochondroma of coronoid process: Jacob's disease. Int J Oral
Maxillofac Surg. 36:11012007. View Article : Google Scholar
|
|
33
|
Etöz OA, Alkan A and Yikilmaz A:
Osteochondroma of the mandibular coronoid process: A rare cause of
limited mouth opening. Br J Oral Maxillofac Surg. 47:409–411. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Thota G, Cillo JE Jr, Krajekian J and
Dattilo DJ: Bilateral pseudojoints of the coronoid process (Jacob
disease): Report of a case and review of the literature. J Oral
Maxillofac Surg. 67:2521–2524. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zhong SC, Xu ZJ, Zhang ZG, Zheng YH, Li TX
and Su K: Bilateral coronoid hyperplasia (Jacob disease on right
and elongation on left): Report of a case and literature review.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 107:e64–e67.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yesildag A, Yariktas M, Doner F, Aydin G,
Munduz M and Topal U: Osteochondroma of the coronoid process and
joint formation with zygomatic arch (jacob disease): Report of a
case. Eur J Dent. 4:91–94. 2010.PubMed/NCBI
|
|
37
|
Acosta-Feria M, Villar-Puchades R,
Haro-Luna JJ, Ramos-Medina B and Garcia-Solano E: Limitation of
mouth opening caused by osteochondroma of the coronoid process.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 112:e64–e68.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Coll-Anglada M, Acero-Sanz J, Vila-Masana
I, Navarro-Cuéllar C, Ochandiano-Caycoia S, López de-Atalaya J and
Navarro-Vila C: Jacob's disease secondary to coronoid process
osteochondroma. A case report. Med Oral Patol Oral Cir Bucal.
16:e708–e710. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
D'Ambrosio N, Kellman RM and Karimi S:
Osteochondroma of the coronoid process (Jacob's disease): An
unusual cause of restricted jaw motion. Am J Otolaryngol. 32:52–54.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ajila V, Hegde S, Gopakumar R and Babu GS:
Imaging and histopathological features of Jacob's disease: A case
study. Head Neck Pathol. 6:51–53. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Ruiz LP and Lara JC: Craniomaxillofacial
features in hereditary multiple exostosis. J Craniofac Surg.
23:e336–e338. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Aoki N, Okamura K, Niino D, Iwamoto O and
Kusukawa J: Osteochondroma of the right coronoid process (Jacob
disease): A case report. Cranio. 31:66–69. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Stringer DE, Chatelain KB and Tandon R:
Surgical treatment of Jacob's disease: A case report involving an
osteochondroma of the coronoid process. Case Rep Surg.
2013:2537402013.PubMed/NCBI
|
|
44
|
Fan H, Lv X, Shi J, Hu J and Luo E:
One-stage treatment to osteochondroma of the coronoid process and
secondary facial asymmetry with coronoidectomy and reduction
malarplasty: A case report and literature review. J Oral Maxillofac
Surg. 72:1870.e1–1870.e13. 2014. View Article : Google Scholar
|
|
45
|
Losa-Muñoz PM, Burgueño-García M,
González-Martín-Moro J and Sánchez-Burgos R: Osteochondroma of
coronoid process: A rare etiology of Jacob disease.
Craniomaxillofac Trauma Reconstr. 7:306–309. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Sawada K, Schulze D, Matsumoto K, Hirai S,
Hashimoto K and Honda K: Osteochondroma of the coronoid process of
the mandible. J Oral Sci. 57:389–392. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Mohanty S, Gupta H, Dabas J and Kumar P:
Osteochondroma of maxillofacial region: Tumor arising from two
different developmental bones. J Oral Maxillofac Pathol.
20:3292016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Mohan Choontharu M, Buch SA, Babu GS,
Castelino RL, Rao S and Rao K: A rare clinical presentation of an
osteochondroma of coronoid process of mandible. J Dent (Shiraz).
19:325–330. 2018.PubMed/NCBI
|
|
49
|
Jacob O: Une cause rare de constriction
permanente des machoires. Bull Et Mem De La Societe Anatomique De
Paris. 1:917–919. 1899.
|
|
50
|
Langenskiöld A: The development of
multiple cartilagenous exostosis. Acta Orthod Scandinav.
38:259–266. 1967. View Article : Google Scholar
|
|
51
|
Geshickter CF: Tumors of Bone (edition 3).
Philadelphia; PA, Saunders: 1963
|
|
52
|
Navaneetham A, Rao KA, Kumaran S and
Baweja HH: A unique case of multiple osteochondroma: Mandibular
symphysis and femur. Ann Maxillofac Surg. 2:182–184. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Bovee JV, Sakkers RJ, Geirnaerdt MJ,
Taminiau AH and Hogendoorn PC: Intermediate grade osteosarcoma and
chondrosarcoma arising in an osteochondroma. A case report of a
patient with hereditary multiple exostoses. J Clin Pathol.
55:226–229. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Staals EL, Bacchini P, Mercuri M and
Bertoni F: Dedifferentiated chondrosarcomas arising in preexisting
osteochondromas. J Bone Joint Surg Am. 89:987–993. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Yoda T, Sato T, Abe T, Sakamoto I, Tomaru
Y, Omura K, Hatano N, Takato T and Ishii Y: Long-term results of
surgical therapy for masticatory muscle tendon-aponeurosis
hyperplasia accompanied by limited mouth opening. Int J Oral
Maxillofac Surg. 38:1143–1147. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Kung'u A: Tumours of bone and cartilage.
East Afr Med J. 55:572–578. 1978.PubMed/NCBI
|
|
57
|
Kamble V, Rawat J, Kulkarni A, Pajnigara N
and Dhok A: Osteochondroma of bilateral mandibular condyle with
review of literature. J Clin Diagn Res. 10:TD01–TD02.
2016.PubMed/NCBI
|
|
58
|
Wolford LM, Mehra P and Franco P: Use of
conservative condylectomy for treatment of osteochondroma of the
mandibular condyle. J Oral Maxillofac Surg. 60:262–268. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Peroz I, Scholman HJ and Hell B:
Osteochondroma of the mandibular condyle: A case report. Int J Oral
Maxillofac Surg. 31:455–456. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Kwon YE, Choi KS, An CH, Choi SY, Lee JS
and An SY: Recurrent osteochondroma of the mandibular condyle: A
case report. Imaging Sci Dent. 47:57–62. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Wolford LM, Movahed R, Dhameja A and Allen
WR: Low condylectomy and orthognathic surgery to treat mandibular
condylar osteochondroma: A retrospective review of 37 cases. J Oral
Maxillofac Surg. 72:1704–1728. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Ealla KK, Reddy SV, Gadipelly S and Charan
C: Osteochondroma of the palate: An interesting and an unusual case
presentation. J Oral Maxillofac Pathol. 18:303–307. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Xu B, Shi H, Wang S, Wang P and Yu Q:
Secondary chondrosarcoma in the mandibular condyle. Dentomaxillofac
Radiol. 40:320–323. 2011. View Article : Google Scholar : PubMed/NCBI
|