Introduction
Colorectal cancer, a malignant tumor of the
digestive system, has gradually increased in the elderly (1). Due to the underlying diseases and
weakened immune function, the level of tolerance is weakened in
elderly patients during surgery, therefore, it requires higher
safety during surgery (2).
Laparoscopy was adopted in clinical practice in 1991 (3). It is the main method for colorectal
cancer surgery due mainly to the small trauma (4). Postoperative cognitive dysfunction
(POCD) often appears in elderly patients undergoing large and
medium-sized surgery under general anesthesia, with symptoms such
as confusion, disorientation, and memory impairment (5). Due to the long anesthesia duration and
the serious trauma caused by radical resection of colorectal
cancer, the risk of POCD in elderly patients is greatly increased
(6). Moreover, some data have shown
that the mechanism of postoperative cognitive dysfunction is
clearly related to the inflammatory response of the body, and it is
more common in cardiothoracic surgery, abdominal surgery and other
major operations (7).
Dexmedetomidine, a novel selective alpha 2
adrenergic receptor agonist, is effective in reducing stress
response and can reduce the use of opioids and section of
pro-inflammatory cytokines, thereby protecting the brain (8). Findings have shown that, the cognitive
function of dexmedetomidine is enhanced after splenectomy in older
rats (9). In addition, the high
dosages of dexmedetomidine have the potential to prevent POCD
(10).
POCD is a common complication of postoperative
anesthesia in the elderly, and the factors affecting its onset are
still unclear. The present study aimed to provide a reference for
the clinical study of dexmedetomidine anesthesia for cognitive
function dysfunction and its influencing factors in elderly
colorectal cancer patients.
Materials and methods
General information
One hundred and forty patients with radical
colorectal cancer under general anesthesia were enrolled in Guizhou
Provincial People's Hospital (Guiyang, China), from March 2012 to
June 2015, including 80 patients in the dexmedetomidine group, with
51 males and 29 females, aged 73.76±14.54 years, weight 56.76±10.12
kg, with the disease duration of 0.71±0.27 years, and 60 cases in
the saline group, including 40 males and 20 females, with an
average age of 74.09±13.87 years, weight between 57.87±9.98 kg, and
the disease duration was 0.68±0.18 years.
Inclusion criteria were: patients whose preoperative
or intraoperative pathology were confirmed as colorectal cancer;
patients who actively received and cooperated with the treatment;
patients with complete data; patients without serious immune system
diseases; patients whose ASA was in grade II–III (aged 60–85
years), with normal cognitive function (MMSE score >27
points).
Exclusion criteria were: Patients with central
nervous system conditions and mental illness, taking sedatives,
antidepressants, high blood pressure, diabetes, coronary heart
disease, cerebral infarction and liver and kidney dysfunction and
other prognostic diseases; patients undergoing radiotherapy and
chemotherapy before surgery.
The study was approved by the Ethics Committee of
Guizhou Provincial People's Hospital and the experimental content
of the patients was described in detail. The patients agreed and
signed a complete informed consent form.
Anesthesia method
All patients who underwent general anesthesia were
applied with an endotracheal intubation procedure and pre-operative
medication was avoided. Detection of vital signs such as heart rate
(HR), electrocardiogram (ECG), non-invasive blood pressure (NIBP),
pulse oxygen saturation (SpO2) and end-tidal carbon
dioxide (PetCO2) were performed on patients during
operation. In addition, Aspect-1000 were connected to monitor the
bispectral index (BIS), then the peripheral venous access was
established. Intravenous injection of 0.04 mg/kg midazolam (Jiangsu
Enhua Pharmaceutical Group Co., Ltd., Jiangsu, China, batch number
080101), 4 µg/kg of fentanyl (Yichang Renfu Pharmaceutical Co.,
Ltd., Yichang, China, National Pharmaceutical Standard H42022076),
0.5–1.5 mg/kg of propofol (Xi'an Libang Pharmaceutical Co., Ltd.,
Xi'an, China, National Pharmaceutical Standard H20040300) and 0.15
mg/kg cis-atracurium (Jiangsu Hengrui Pharmaceutical Co., Ltd.,
Jiangsu, China, National Pharmaceutical Standard H20060869).
Intravenous infusion of remifentanil 0.04–0.4 µg/(kg·min) and
propofol 1.5–2.5 mg/(kg·h) were continuously applied in order to
maintain the effectiveness of anesthesia during the operation, also
intravenous injection of cis-atracurium were intermittent. The
effectiveness of anesthesia was adjusted during the procedure and
the BIS was maintained between 40 and 50; the breathing parameters
were adjusted and the PetCO2 was maintained at 35–45
mmHg. In the study group, 200 µg of dexmedetomidine (batch number:
H20110085, Jiangsu Hengrui Pharmaceutical Co., Ltd.) was diluted to
50 ml (prepared concentration of 4 µg/ml) using physiological
saline. The general anesthesia-induced tracheal intubation was
started, and 1 µg/kg dexmedetomidine hydrochloride was
intravenously pumped in 15 min, and then the pump was maintained at
0.2–0.7 µg/(kg·h). In addition, the infusion rate was adjusted
according to changes in the patient's heart rate and blood
pressure. Dexmedetomidine was discontinued 30 min before the end of
the procedure. In the control group, the same amount of normal
saline was injected in the intravenous pump at the corresponding
time.
Serum collection
Peripheral blood (2 ml) was collected on the 1st day
before and 1st and 3rd day after surgery during fasting period,
placed in an anticoagulation tube and sent to the laboratory. After
coagulation for 60 min (20–25°C), it was centrifuged at 2,600 × g
for 10 min at 4°C. The supernatant was collected at −80°C to be
tested, avoiding repeated freezing-thawing.
Determination of S-100β protein (S-100β) and
interleukin-6 (IL-6) in serum by enzyme-linked immunosorbent assay
(ELISA). S-100β, IL-6 ELISA kit was purchased from Mo Shake
Biological Co., Ltd., using the BS-1101 ELISA analyzer (Beyotime,
Shanghai, China) for detection. 50 µl of the standard was added to
the wells that were coated with the enzyme label, then 40 µl of the
sample dilution was added to the wells of the samples, and 10 µl of
the sample to be tested was added (sample dilution ratio was 5
times). During the operation process, touching the wall of the well
was avoided, the well was gently shaken, the reaction well was
sealed with film, and then incubated in a water bath or incubator
at 37°C for 30 min. The sealing film was carefully uncovered, the
liquid was discarded, and the film was dried with absorbent paper,
and each well was filled with the washing solution. After standing
for 30 sec, this step was repeated five times and then left to dry.
In addition to the blank wells (the blank control wells were
identical to the above steps, but without the enzyme-labeled
reagents and samples), 50 µl of the enzyme-labeled reagent was
added to each well, and the mixture was incubated at 37°C for 30
min and then washed. Substrate A and B (50 µl of each) was added to
each well, and the color was developed at 37°C for 15 min in the
dark. Stop solution (50 µl) was added to each well, and the wells
were zeroed with a blank well, and the absorbance (OD value) of
each well was measured at a wavelength of 450 nm in 25 min. Then
the content of S-100β and IL-6 in the serum was calculated.
Observation indices
The mini mental state examination (MMSE) was
performed 1 day before surgery, and repeated 1 day and 3 days after
surgery. The score was divided into 30 points, of which 28 to 30
points indicate normal cognition, 24–27 are classified as mild
cognitive dysfunction, 19–23 as moderate cognitive dysfunction, and
0–18 as severe cognitive dysfunction (11). The incidence of POCD was compared
between the two groups. The changes of S-100β and IL-6 levels
before and after surgery were observed. The factors that
contributed to the occurrence of POCD were analysed.
Statistical analysis
Statistical analysis of experimental data was
performed using SPSS 19.0 software system (IBM Corp., Armonk, NY,
USA), [n (%)] was used to represent the count data, the chi-square
test was used for comparison between the groups. The measurement
data were expressed as mean ± SD. The t-test was used to compare
two groups, and the analysis of variance was used for comparison
between multiple groups. The main relevant factors were analyzed by
logistic regression The difference was statistically significant at
P<0.05..
Results
Comparison of general information
There was no significant difference between the
experiment group and the control group in terms of sex, age,
weight, height, duration of illness, smoking status and alcoholism
(P>0.05). The surgical procedure of the two groups were
compared, and there was no significant difference in the operation
time between the experiment and control groups (P>0.05). The
anesthesia time and intraoperative blood loss in the experiment
group were significantly lower than those in the control group
(P<0.05) (Table I).
 | Table I.Comparison of clinical data and
surgery conditions (mean ± SD)/[n (%)]. |
Table I.
Comparison of clinical data and
surgery conditions (mean ± SD)/[n (%)].
| Characteristics | Experiment group
(n=80) | Control group
(n=60) | χ2/t
value | P-value |
|---|
| Sex |
|
| 0.128 | 0.720 |
| Male | 51 (63.8) | 40 (66.7) |
|
|
|
Female | 29 (36.2) | 20 (33.3) |
|
|
| Age (years) |
73.76±14.54 |
74.09±13.87 | 0.136 | 0.892 |
| Weigh (kg) |
56.76±10.12 | 57.87±9.98 | 0.646 | 0.519 |
| Height (cm) | 167.65±12.76 | 168.09±11.98 | 0.207 | 0.836 |
| Disease duration
(years) |
0.71±0.27 |
0.68±0.18 | 0.745 | 0.458 |
| Smoking status |
|
| 0.088 | 0.766 |
|
Smoking | 34 (42.5) | 24 (40.0) |
|
|
|
Non-smoking | 46 (57.5) | 36 (60.0) |
|
|
| Alcoholism |
|
| 0.625 | 0.429 |
|
Alcoholic | 44 (55.0) | 37 (61.7) |
|
|
|
Non-alcoholic | 36 (45.0) | 23 (38.3) |
|
|
| Operation time
(min) | 182.67±24.76 | 180.98±23.79 | 0.406 | 0.685 |
| Anesthesia time
(h) |
188.27±54.65a | 211.12±79.98 | 2.007 | 0.047a |
| Intraoperative
blood loss (ml) |
367.09±151.12a | 429.76±217.98 | 2.008 | 0.047a |
MMSE scores between two groups at
different times
There was no significant difference in MMSE score
between the experiment group and the control group before surgery
(P>0.05). The MMSE scores of the two groups on the 1st and 3rd
day after surgery were lower than those before surgery (P<0.05).
The MMSE scores of the control group on the 1st day and 3rd day
after surgery were significantly lower than those of the experiment
group (P<0.05) (Table II).
 | Table II.Comparison of MMSE scores between the
two groups at different times. |
Table II.
Comparison of MMSE scores between the
two groups at different times.
| Group | 1 day before
surgery | 1 day after
surgery | 3 days after
surgery |
|---|
| Experiment
group | 28.93±1.25 |
26.76±1.67a |
28.11±2.01a |
| Control group | 28.89±1.22 |
24.15±1.98a,b |
26.09±1.78a,b |
| t value | 0.189 | 8.448 | 6.176 |
| P-value | 0.850 | <0.001 | <0.001 |
Comparison of POCD status between the
two groups of patients
There were 7 (8.75%) cases of POCD in the experiment
group on the 1st day after surgery, and 13 (21.67%) cases of POCD
in the control group, there was no POCD in the experiment group 3
days after surgery, and 8 (13.33%) cases in the control group, and
there was a significant difference between the two groups
(P<0.05) (Table III).
 | Table III.Comparison of POCD status between the
two groups. |
Table III.
Comparison of POCD status between the
two groups.
| Group | 1 day after
surgery | 3 days after
surgery |
|---|
| Experiment group
(n=80) | 7 (8.75%) | 0 (0.00%) |
| Control group
(n=60) | 13 (21.67%) | 8 (13.33%) |
| χ2
value | 4.672 | 11.31 |
| P-value | 0.031 | 0.0008 |
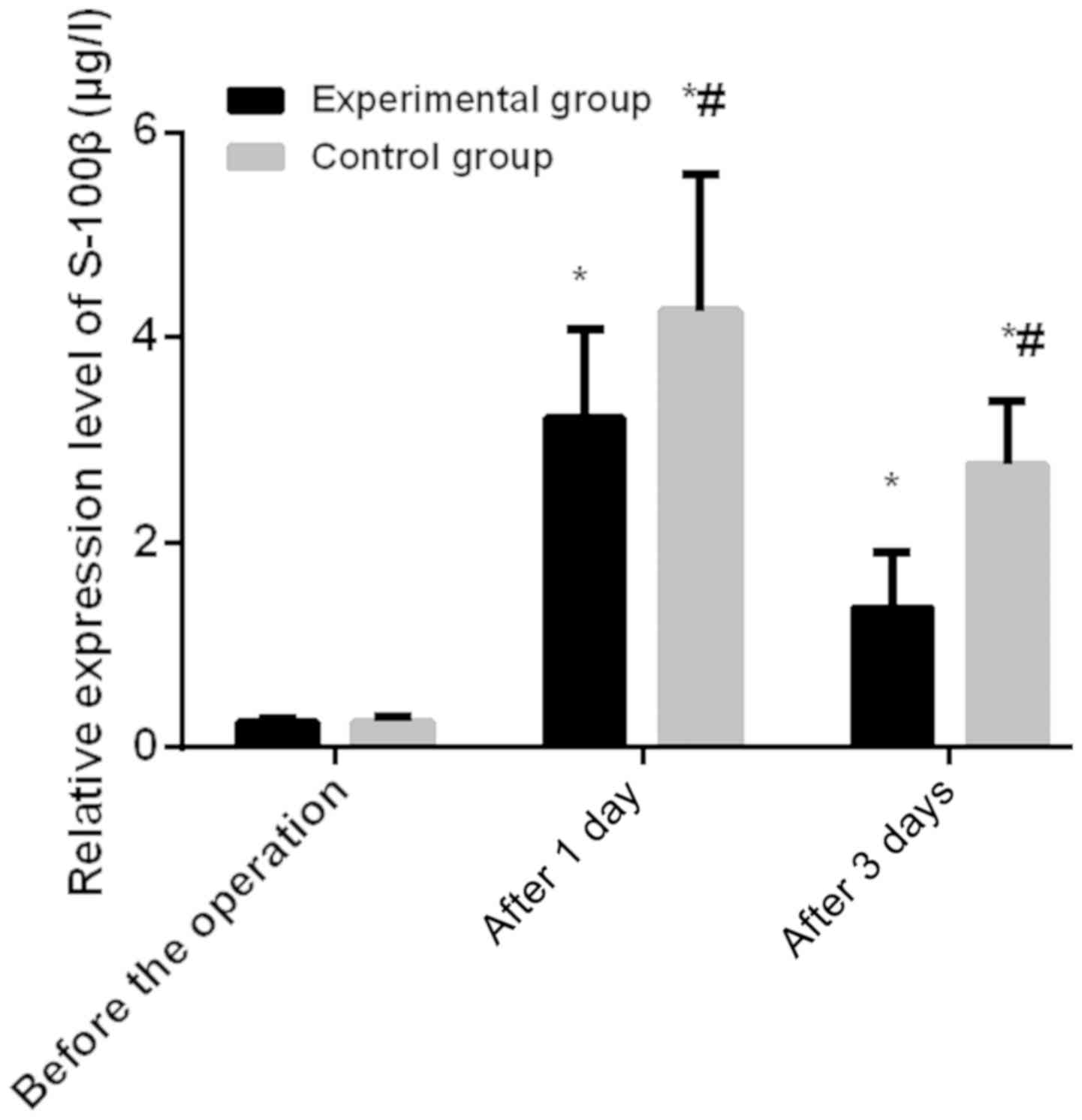
Comparison of serum IL-6 and S-100β
levels in the two groups
There was no significant difference in serum IL-6
and S-100β levels between the two groups before surgery
(P>0.05). The levels of serum IL-6 and S-100β in the two groups
were increased compared with those 1 day and 3 days before surgery,
and the difference was statistically significant (P<0.05). The
levels of serum IL-6 and S-100β in the control group on the 1st and
3rd day after surgery were significantly higher than those in the
experiment group (P<0.05) (Figs.
1 and 2).
Logistic regression analysis of
POCD
The clinical data of all subjects were analysed 1
day after surgery, the clinical data of patients with POCD and
non-POCD patients 1 day after surgery were analyzed by univariate
analysis, the age, duration of anesthesia, intraoperative blood
loss, IL-6 and S-100β expression were the influencing factors of
POCD. Subsequently, multivariate Cox regression analysis of
different indicators showed that age ≥70 years, anesthesia duration
≥3 h, intraoperative blood loss ≥350 ml, the high expressions of
IL-6 and S-100β were important factors related to the occurrence of
POCD (P<0.05) (Tables
IV–VI).
 | Table IV.Comparison of general data of
patients with POCD and non-POCD after 5 h of surgery. |
Table IV.
Comparison of general data of
patients with POCD and non-POCD after 5 h of surgery.
|
Characteristics | POCD group
(n=20) | Non-POCD group
(n=120) | χ2
value | P-value |
|---|
| Sex |
|
| 1.026 | 0.311 |
|
Male | 15 (75.0) | 76 (63.3) |
|
|
|
Female | 5
(25.0) | 44 (36.7) |
|
|
| Age |
|
| 23.51 | <0.001 |
|
<70 | 4
(20.0) | 90 (75.0) |
|
|
|
≥70 | 16 (80.0) | 30 (25.0) |
|
|
| Smoking status |
|
| 0.020 | 0.889 |
|
Smoking | 8
(40.0) | 50 (41.7) |
|
|
|
Non-smoking | 12 (60.0) | 70 (58.3) |
|
|
| Alcoholism |
|
| 0.488 | 0.485 |
|
Alcoholic | 13 (65.0) | 68 (56.7) |
|
|
|
Non-alcoholic | 7
(35.0) | 52 (43.3) |
|
|
| Anesthesia
duration |
|
| 25.16 | <0.001 |
| ≥3
h | 18 (90.0) | 37 (30.8) |
|
|
| <3
h | 2
(10.0) | 83 (69.2) |
|
|
| Intraoperative
blood loss |
|
| 19.65 | <0.001 |
| ≥350
ml | 15 (75.0) | 30 (25.0) |
|
|
| <350
ml | 5
(25.0) | 90 (75.0) |
|
|
| IL-6 |
|
| 22.55 | <0.001 |
| Highly
expressed | 16 (80.0) | 31 (25.8) |
|
|
| Lowly
expressed | 4
(20.0) | 89 (74.2) |
|
|
| S-100β |
|
| 43.14 | <0.001 |
| Highly
expressed | 18 (90.0) | 22 (18.3) |
|
|
| Lowly
expressed | 2
(10.0) | 98 (81.7) |
|
|
 | Table VI.Multi-factor Cox analysis. |
Table VI.
Multi-factor Cox analysis.
|
| β values | P-values | χ2
values | OR values | 95% CI |
|---|
| Constant | −5.546 | 0.002 | 9.891 | 0.004 |
|
| Age | −0.651 | 0.047 | 2.054 | 0.521 | 0.214–1.271 |
| Anesthesia
duration | 1.159 | 0.010 | 6.673 | 3.188 | 1.323–7.685 |
| Intraoperative
blood loss | 1.378 | 0.002 | 9.506 | 3.968 | 1.652–9.529 |
| IL-6 | 0.927 | 0.042 | 4.127 | 2.527 | 1.033–6.180 |
| S-100β | 1.042 | 0.030 | 4.732 | 2.835 | 1.109–7.249 |
Discussion
Colorectal cancer is a common malignant tumor. With
the continuous improvement of living standards, environmental
pollution, and changing lifestyles as well as eating habits, the
incidence and mortality of colorectal cancer have been on the
increase. In 2015, there were 376,000 new cases of colorectal
cancer, which caused 191,000 deaths (12). The incidence of colorectal cancer is
related to dietary structure, chronic inflammation of the
intestine, heredity, colorectal adenoma and other factors (13,14).
Patients with colorectal cancer are often treated with radical
surgery. Laparoscopic surgery is less traumatic than the
traditional surgery, and has a better recovery after surgery
(15). However, findings have shown
that after surgery, clinical complications of POCD such as
learning, memory, and perception appeared after surgery (16). The postoperative POCD in elderly
patients is also closely related to inflammatory reaction, and has
a certain relationship with the patient's preoperative history,
surgical stimulation, age, anesthesia and other factors (17). Colorectal cancer is seriously
affected by the anesthesia and the use of anesthetic drugs during
the surgical treatment, resulting in the occurrence of inflammatory
reactions, massive release of inflammatory mediators, and cognitive
dysfunction in patients after surgery (18,19).
Dexmedetomidine, an imidazole derivative and a
dextrorotatory isomer of medetomidine, is a novel adrenal α2
receptor agonist with high selectivity. It can activate the G
protein on the α2 adrenergic receptor in the central nervous
system, and the release of norepinephrine is inhibited, which
affects the sympathetic nervous system and exerts its sedative,
anti-anxiety and analgesic effects (20,21). It
can activate the cholinergic anti-inflammatory pathway and
downregulate inflammatory factors to exert anti-inflammatory
effects (22). Moreover,
dexmedetomidine is widely used in clinical anesthesia, which can
stabilize the patient's hemodynamics, reduce the incidence of
adverse reactions as well as the use of sedative anesthetics.
Moreover, it has a certain inhibitory effect on the stress response
and secretion and release of inflammatory factors, and there is a
certain protective effect on the brain and myocardium of patients,
which significantly improves the occurrence of POCD (23).
As a polypeptide, cytokines function by regulating
the physiological functions of the body (24). S-100β is a specific indicator for
judging brain damage, which is mainly present in the central
nervous system of the body (25).
The binding of IL-6 to membrane receptors on the surface of tumor
cells enables inducible proliferation of tumor cells, which in turn
inhibits apoptosis of cells and causes postoperative damage
(26).
The surgery of the two groups were compared, there
was no significant difference in the surgery duration between the
experiment group and the control group (P>0.05). The anesthesia
time and intraoperative blood loss in the experiment group were
significantly less than those in the control group (P<0.05). van
Harten et al (27) found that
the incidence of postoperative POCD in surgical patients has a
certain relationship with surgical diseases and anesthetic drugs.
This study showed that compared with the preoperative MMSE scores,
the scores of MMSE after surgery for elderly colorectal cancer were
significantly lower, and the decrease of MMSE score after
dexmedetomidine was significantly reduced. The incidence of POCD on
the 1st day and 3rd day after surgery was significantly lower in
the experiment group than in the control group (P<0.05). This is
consistent with the study by Chan et al (28). Intravenous injection of
dexmedetomidine after anesthesia induction resulted in a
significant reduction in postoperative mental confusion and POCD
incidence. Findings have shown that inflammatory response as an
independent factor often leading to the occurrence of POCD
(29,30), while S-100β protein is a good
indicator of brain damage (31).
The high level of IL-6 reflects the strong surgical
stress response (26). The results
showed that there was no significant difference in serum IL-6 and
S-100β levels between the two groups before surgery (P>0.05).
The levels of serum IL-6 and S-100β in the two groups were
increased on the 1st and 3rd day after surgery, and the difference
was statistically significant (P<0.05). The levels of serum IL-6
and S-100β in the control group on the 1st and 3rd day after
surgery were significant higher than those in the experiment group
(P<0.05). There are many reasons for cognitive dysfunction in
patients after surgery, and the pathogenesis is still unclear. Age,
preoperative underlying disease, type of surgery, duration of
anesthesia, postoperative infection, respiratory complications,
intraoperative anesthesia, and sedation of the patients may be
associated with postoperative cognitive dysfunction (32). Ramlawi et al found that the
severity and duration of the inflammatory response are related to
POCD (33). In this study,
multivariate Cox regression analysis found that in elderly people
aged >70 years, anesthesia duration of more than 3 h,
intraoperative blood loss over 350 ml, high expression of IL-6 and
S-100β are important factors in the occurrence of POCD (P<0.05).
This is consistent with other studies whereby the cognitive
dysfunction is associated with advanced age, low level of
education, high blood pressure comorbidities and long duration of
anesthesia (34).
Many studies on the effects of dexmedetomidine on
cognitive function have no definitive conclusions as the subjects
were different, the dosages, timing, and methods used for
dexmedetomidine were different. Further research on larger number
of samples, and the mechanism of dexmedetomidine need to be carried
out.
In summary, dexmedetomidine can significantly
improve postoperative cognitive dysfunction in elderly patients
with colorectal cancer. The occurrence of cognitive dysfunction is
affected by the age, duration of anesthesia, intraoperative blood
loss and high expression of IL-6 and S-100β.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JZ wrote the manuscript. JZ, GL and FZ were
responsible for ELISA. HF, DZ and SL analyzed and interpreted the
patients' data. BC and HX helped with statistical analysis. All the
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Guizhou Provincial People's Hospital (Guiyang, China). Patients who
participated in this research had complete clinical data. Signed
informed consents were obtained from the patients or the
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Vincent MD, Breadner D, Cripps MC, Jonker
DJ, Klimo P, Biagi JJ, Lam W, O'Connell A, Whiston F, Stitt L, et
al: Phase I/II trial of dose-reduced capecitabine in elderly
patients with advanced colorectal cancer. Curr Oncol. 24:e261–e268.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Finlayson E, Zhao S and Varma MG: Outcomes
after rectal cancer surgery in elderly nursing home residents. Dis
Colon Rectum. 55:1229–1235. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kennedy RH, Francis EA, Wharton R, Blazeby
JM, Quirke P, West NP and Dutton SJ: Multicenter randomized
controlled trial of conventional versus laparoscopic surgery for
colorectal cancer within an enhanced recovery programme: EnROL. J
Clin Oncol. 32:1804–1811. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shen F, Cai WS, Li JL, Feng Z, Liu QC,
Xiao HQ, Cao J and Xu B: Synergism from the combination of
ulinastatin and curcumin offers greater inhibition against
colorectal cancer liver metastases via modulating matrix
metalloproteinase-9 and E-cadherin expression. Onco Targets Ther.
7:305–314. 2014.PubMed/NCBI
|
|
5
|
Feinkohl I, Winterer G, Spies CD and
Pischon T: Cognitive reserve and the risk of postoperative
cognitive dysfunction. Dtsch Arztebl Int. 114:110–117.
2017.PubMed/NCBI
|
|
6
|
Visovatti MA, Reuter-Lorenz PA, Chang AE,
Northouse L and Cimprich B: Assessment of cognitive impairment and
complaints in individuals with colorectal cancer. Oncol Nurs Forum.
43:169–178. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Louzon P, Jennings H, Ali M and Kraisinger
M: Impact of pharmacist management of pain, agitation, and delirium
in the intensive care unit through participation in
multidisciplinary bundle rounds. Am J Health Syst Pharm.
74:253–262. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tasdogan M, Memis D, Sut N and Yuksel M:
Results of a pilot study on the effects of propofol and
dexmedetomidine on inflammatory responses and intraabdominal
pressure in severe sepsis. J Clin Anesth. 21:394–400. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Xiong B, Shi Q and Fang H: Dexmedetomidine
alleviates postoperative cognitive dysfunction by inhibiting neuron
excitation in aged rats. Am J Transl Res. 8:70–80. 2016.PubMed/NCBI
|
|
10
|
Fu C, Dai X, Yang Y, Lin M, Cai Y and Cai
S: Dexmedetomidine attenuates lipopolysaccharide-induced acute lung
injury by inhibiting oxidative stress, mitochondrial dysfunction
and apoptosis in rats. Mol Med Rep. 15:131–138. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dufouil C, Clayton D, Brayne C, Chi LY,
Dening TR, Paykel ES, O'Connor DW, Ahmed A, McGee MA and Huppert
FA: Population norms for the MMSE in the very old: Estimates based
on longitudinal data. Mini-Mental State Examination. Neurology.
55:1609–1613. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Allemani C, Rachet B, Weir HK, Richardson
LC, Lepage C, Faivre J, Gatta G, Capocaccia R, Sant M, Baili P, et
al: Colorectal cancer survival in the USA and Europe: A CONCORD
high-resolution study. BMJ Open. 3:e0030552013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Citronberg J, Bostick R, Ahearn T, Turgeon
DK, Ruffin MT, Djuric Z, Sen A, Brenner DE and Zick SM: Effects of
ginger supplementation on cell-cycle biomarkers in the
normal-appearing colonic mucosa of patients at increased risk for
colorectal cancer: Results from a pilot, randomized, and controlled
trial. Cancer Prev Res (Phila). 6:271–281. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Galsky MD, Stensland KD, Moshier E,
Sfakianos JP, McBride RB, Tsao CK, Casey M, Boffetta P, Oh WK,
Mazumdar M, et al: Effectiveness of adjuvant chemotherapy for
locally advanced bladder cancer. J Clin Oncol. 34:825–832. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Güçlü CY, Ünver S, Aydınlı B, Kazancı D,
Dilber E and Özgök A: The effect of sevoflurane vs. TIVA on
cerebral oxygen saturation during cardiopulmonary bypass -
randomized trial. Adv Clin Exp Med. 23:919–924. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
de Tournay-Jetté E, Dupuis G, Bherer L,
Deschamps A, Cartier R and Denault A: The relationship between
cerebral oxygen saturation changes and postoperative cognitive
dysfunction in elderly patients after coronary artery bypass graft
surgery. J Cardiothorac Vasc Anesth. 25:95–104. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gruppo AIR: Consensus document: a model of
integrated management of patients with psycomotor agitation. Riv
Psichiatr. 51:238–250. 2016.(In Italian). PubMed/NCBI
|
|
19
|
Zhang J, Zhang J, Yu P, Chen M, Peng Q,
Wang Z and Dong N: Remote ischaemic preconditioning and sevoflurane
postconditioning synergistically protect rats from myocardial
injury induced by ischemia and reperfusion partly via inhibition
TLR4/MyD88/NF-κB signaling pathway. Cell Physiol Biochem. 41:22–32.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ohtani N, Kida K, Shoji K, Yasui Y and
Masaki E: Recovery profiles from dexmedetomidine as a general
anesthetic adjuvant in patients undergoing lower abdominal surgery.
Anesth Analg. 107:1871–1874. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yildiz M, Tavlan A, Tuncer S, Reisli R,
Yosunkaya A and Otelcioglu S: Effect of dexmedetomidine on
haemodynamic responses to laryngoscopy and intubation:
Perioperative haemodynamics and anaesthetic requirements. Drugs R
D. 7:43–52. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Pavlov VA and Tracey KJ: The cholinergic
anti-inflammatory pathway. Brain Behav Immun. 19:493–499. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Teegarden BM and Prough DS: Delirium:
Getting back on track. Crit Care Med. 44:1265–1266. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li QY, Xu HY and Yang HJ: Effect of
proinflammatory factors TNF-α, IL-1β, IL-6 on neuropathic pain.
Zhongguo Zhong Yao Za Zhi. 42:3709–3712. 2017.(In Chinese).
PubMed/NCBI
|
|
25
|
Yang B, Qian F, Li W, Li Y and Han Y:
Effects of general anesthesia with or without epidural block on
tumor metastasis and mechanisms. Oncol Lett. 15:4662–4668.
2018.PubMed/NCBI
|
|
26
|
Liu F, Zhang J, Zeng XQ, Zhao YQ and Zuo
YX: Application of general anesthesia combined with epidural
anesthesia/analgesia in rehabilitation after gastric cancer
resection. Zhonghua Yi Xue Za Zhi. 97:1089–1092. 2017.(In Chinese).
PubMed/NCBI
|
|
27
|
van Harten AE, Scheeren TW and Absalom AR:
A review of postoperative cognitive dysfunction and
neuroinflammation associated with cardiac surgery and anaesthesia.
Anaesthesia. 67:280–293. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chan MT, Cheng BC, Lee TM and Gin T; CODA
Trial Group, : BIS-guided anesthesia decreases postoperative
delirium and cognitive decline. J Neurosurg Anesthesiol. 25:33–42.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Barrientos RM, Hein AM, Frank MG, Watkins
LR and Maier SF: Intracisternal interleukin-1 receptor antagonist
prevents postoperative cognitive decline and neuroinflammatory
response in aged rats. J Neurosci. 32:14641–14648. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wu C, Wang R, Li X and Chen J:
Preoperative serum microRNA-155 expression independently predicts
postoperative cognitive dysfunction after laparoscopic surgery for
colon cancer. Med Sci Monit. 22:4503–4508. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang XT, Lv M and Guo HY: Effects of
epidural block combined with general anesthesia on antitumor
characteristics of T helper cells in hepatocellular carcinoma
patients. J Biol Regul Homeost Agents. 30:67–77. 2016.PubMed/NCBI
|
|
32
|
Hanning CD: Postoperative cognitive
dysfunction. Br J Anaesth. 95:82–87. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ramlawi B, Rudolph JL, Mieno S, Feng J,
Boodhwani M, Khabbaz K, Levkoff SE, Marcantonio ER, Bianchi C and
Sellke FW: C-Reactive protein and inflammatory response associated
to neurocognitive decline following cardiac surgery. Surgery.
140:221–226. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Fu M and Li D: General anesthesia combined
with epidural anesthesia on the postoperative cognitive functions
in pregnant women with dystocia. Exp Ther Med. 16:1149–1152.
2018.PubMed/NCBI
|