Introduction
Thoracic esophageal cancer (EC) has a high mortality
rate and can be difficult to treat (1). The incidence of EC has increased
rapidly compared with that of other cancer types and the symptoms
often present at a late stage of disease, resulting in a 17% 5-year
survival rate for all stages combined (1).
Esophageal resection is currently the only curative
treatment for EC; however, this surgical procedure is associated
with considerable mortality risk and associated complications
(2). Other treatment options include
chemoradiotherapy, which is the standard approach for treating
local advanced EC (3,4), aiming to achieve optimal tumor control
while improving quality of life. Radiotherapy (RT) is also used to
treat EC, with the aim of effectively covering the target volume
while minimizing irradiation of the surrounding normal tissue. Even
with curative RT, long-term survival rates remain poor due to a
high frequency of lymph node metastasis and regional recurrence
(5,6). Muijs et al (7) demonstrated that the overall survival
rate of patients with EC was considerably low due to the presence
of microscopic tumors outside of the clinical target volume, even
after conformal radiation therapy (CRT). Furthermore, Ji et
al (8) reported that 3D-CRT may
deliver considerable doses of incidental radiation to elective
regions in thoracic EC, which has a substantial impact on the
control of micro-metastases.
In recent years, the clinical application of
technology has increased with the development of new hardware and
software designed to treat cancer. For example, VMAT is a novel
radioactive technique that has been demonstrated to generate
dosimetrically equivalent plans with intensity modulated radiation
therapy (IMRT) (9–11). Using VMAT, RT technology has dynamic
parameters, including variations in dose rate, gantry position,
gantry rotation speed and leaf motion speed. The ability to alter
these parameters generates superior results in target conformity
and in sparing organs at risk (OARs). Despite this, low-dose
irradiation of tissues surrounding the target volume is unavoidable
when using advanced RT technology. The purpose of the present study
was to determine whether advanced RT technology generates
incidental irradiation doses for lymph nodes and to compare three
RT techniques (VMAT, IMRT and 3D-CRT) with respect to the treatment
of patients with thoracic EC.
Materials and methods
Patient selection, ethical approval
and computed tomography (CT) simulation
A total of 15 patients between the ages of 46 and 81
years (mean age, 66.5 years) with early-stage EC [Tumor
(T)1-3 Node (N)0 Metastasis (M)0],
who were previously treated with VMAT at the Hangzhou Cancer
Hospital (Hangzhou, China), were recruited between October 2016 and
July 2017. Each patient was retrospectively re-planned for IMRT and
3D-CRT techniques on the Pinnacle treatment planning system (TPS,
ADAC Pinnacle V9.1, Philips Medical System, USA) with a 6 MV photon
beam from Elekta Axesse equipped with a Millennium MLC with 160
leaves. The present study was approved by the Medical Ethics
Committee of Hangzhou Cancer Hospital (Hangzhou, China) and written
informed consent was obtained from all patients. Patient
characteristics are summarized in Table
I.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Patient | Age, years | Sex | Location | TNM stage | Length, cm | PTV, cc |
|---|
| 1 | 60 | M | Ut |
T2N0M0 | 3 | 279.6 |
| 2 | 68 | M | Ut |
T2N0M0 | 5 | 417.4 |
| 3 | 60 | M | Ut |
T3N0M0 | 10 | 568.6 |
| 4 | 63 | F | Ut |
T2N0M0 | 5 | 195.4 |
| 5 | 57 | M | Ut |
T3N0M0 | 6 | 362.8 |
| 6 | 81 | M | Mt |
T2N0M0 | 13.3 | 446.3 |
| 7 | 56 | M | Mt |
T3N0M0 | 8 | 589.8 |
| 8 | 71 | M | Mt |
T2N0M0 | 10 | 474.0 |
| 9 | 79 | F | Mt |
T2N0M0 | 5 | 273.5 |
| 10 | 76 | M | Mt |
T3N0M0 | 7 | 348.2 |
| 11 | 78 | F | Lt |
T2N0M0 | 3 | 377.8 |
| 12 | 70 | M | Lt |
T2N0M0 | 7 | 380.5 |
| 13 | 46 | M | Lt |
T3N0M0 | 6 | 276.7 |
| 14 | 54 | M | Lt |
T2N0M0 | 7 | 213.1 |
| 15 | 81 | M | Lt |
T2N0M0 | 4.2 | 241.8 |
A CT simulator was used to determine target volume.
Patients were placed in the supine position with arms extended
above the head and the CT images were obtained at 3-mm slices.
Target volume was visualized on the CT images and using an
endoscopic extension. The gross tumor volume and clinical target
volume were contoured by the radiation oncologist according to the
International Commission On Radiation Units and Measurements report
62 (12) and a margin was placed to
form a planning target volume (PVT). The prescription dose was 2.0
Gy × 30 fractions, for a total dose of 60 Gy.
Principles of lymph nodal station
(LNS) delineation
LNS were delineated and termed according to the
Japan Esophageal Society Guidelines (1314), presented in Table II. Delineation focused on thoracic
lymph nodes NO. 105-112. The LNSs were grouped into upper-thorax,
middle-thorax and lower-thorax categories. The delineation of
NO.105-112 was performed using a mediastinal CT window (400 HU
width, at +40 HU level) to identify the segmental bronchi for
limits of visibility (15). All LNSs
were contoured by the same radiation oncologist. On completion of
LNS delineation, an experienced pathologist and radiation
oncologist each verified the LNS contours on the CT images.
 | Table II.Classification of lymph nodal station
in Japan Esophageal Society Guidelines. |
Table II.
Classification of lymph nodal station
in Japan Esophageal Society Guidelines.
| Region | Numbering | Japan Esophageal
Society |
|---|
| Upper-thorax | 105 | Upper thoracic
paraesophageal nodes |
|
| 106tb-R | Right
tracheobronchial lymph nodes |
|
| 106pre | Pretracheal lymph
nodes |
|
| 106tb-L | Left
tracheobronchial lymph nodes |
|
| 106recL | Left recurrent
nerve lymph nodes |
|
| 106recR | Right recurrent
nerve lymph nodes |
| Middle-thorax | 107 | Subcarinal lymph
nodes |
|
| 108 | Middle thoracic
paraesophageal lymph nodes |
|
| 109R | Right main bronchus
lymph nodes |
|
| 109L | Left main bronchus
lymph nodes |
| Lower-thorax | 110 | Lower thoracic
paraesophageal lymph nodes |
|
| 111 | Supradiaphragmatic
lymph nodes |
|
| 112 | Posterior
mediastinal lymph nodes |
|
| 112ao | Thoracic paraaortic
lymph nodes |
|
| 112pul | Pulmonary ligament
lymph nodes |
Treatment plan
VMAT technology aims to improve target area coverage
and spare normal tissues (16). The
advantage of VMAT is shorter treatment times compared with
conventional IMRT technology. Patients were treated with a single
full arc with clockwise rotation of the gantry with start and stop
angles of 182 and 178. The maximum dosage was 600 MU/min and the
maximum gantry rotation velocity was 3 deg/min. Dose distribution
optimization was performed inversely using dose-volume objectives
with instantaneous dose rates, MLC leaf positions and gantry
rotational speeds (17,18).
A 5-coplanar field arrangement was used for the IMRT
plans. The PVT conformity was defined using a right-posterior
oblique field with gantry angle 210, an anterior oblique field with
gantry angle 0 and a left-posterior oblique field with gantry angle
150 to minimize exposure of the lung. The other two beams included
the right-anterior oblique field at gantry angle 315 and
left-anterior oblique field at gantry angle 45 This was used to
compensate for the dose gradients of the target volume due to
anterior and posterior fields. A direct machine parameter
optimization algorithm was applied to optimize the treatment plans.
The minimum field size and monitor unit (MU) of the subfield were
restricted to 2 cm2 and 5 MU.
3D-CRT with 4-field beam arrangements were generated
using the Pinnacle treatment planning system. Treatment plans for a
tumor located in the lower-thorax had an
anteroposterior-posteroanterior, and two right and left lateral
field beam arrangement. Two parallel-opposed oblique fields and
anteroposterior-posteroanterior were always used in the treatment
plans for upper- and middle-thoracic EC to avoid exposure of the
spinal cord. Typical oblique angles were 150º and
210º from the posterior side.
Plan evaluation
Three types of plan were transferred to TPS for
analysis. The cumulative dose volume histograms were generated for
evaluation and comparison. For each target volume, D2%
and D98% (dose corresponding to 2% and 98% of the target
volume), V95%, and V110% (volume of the
target receiving 95% and 110% of the prescription dose), conformal
index (CI), and homogeneity index (HI) were tabulated and reviewed.
The following were selected for evaluation: The mean dose
(Dmean) and the percentage of the lung that received 5
Gy (V5), 20 Gy (V20) and 30 Gy
(V30), the mean dose (Dmean) and the
percentage of the heart that received 20 and 30 Gy (V20
and V30, respectively), and the maximum dose
(Dmax) to the spine. The percentage volume that received
>40 Gy (V40) for each nodal region was calculated and
the equivalent uniform dose (EUD) was also calculated for each
contoured nodal region. The CI, HI and EUD are described below.
CI and HI were defined to describe the quality of
the target as follows: CI=(VT.ref/VT) ×
(TT.ref × Vref), where VT
represents the target volume, VT.ref represents the
target volume wrapped by the reference isodose curve face, and
Vref represents the total volume wrapped by the
reference isodose curve face. A higher CI value, ranging from 0 to
1, represents better conformity.
HI=(D2%-D98%)/Dmean. Where
D2% represents the dose corresponding to 2% of the
target volume, as shown in DVH, and can be deemed the maximum dose;
D98% represents the dose corresponding to 98% of the
target volume, and can be deemed the minimum dose. EUD is the
absorbed dose that is biologically equivalent to the non-homogenous
dose, when given homogenously, and was calculated using the
following formula:
EUD=(1N∑iDia)1a
Where N is the number of voxels in the structure of
interest, Di is the dose in the ith voxel and
a is the tumor-specific parameter for cold spots of interest
in the tumor target volume, reflected by the value of EUD when the
value is <1.
Statistical analysis
The results between the three plans were analyzed
using one-way analysis of variance and Tukey's test was used to
further determine differences in pairwise comparisons. Multiple
parameter regression analysis was conducted to assess the
incidental nodal irradiation (INI). All statistical analyses were
performed using SPSS v.19.0 software (IBM Corp., Armonk, NY, USA).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Comparison of PTV and OAR sparing for
all plans
The target coverage and OAR sparing are summarized
in Table III. The 5F-IMRT plan was
superior in target coverage, as indicated by the
PTV_V95% (P=0.003); 3D-CRT was inferior in terms of
target coverage, as indicated by V95% (P=0.003) and
V110% (P=0.012). The VMAT plan was superior in terms of
CI (P=0.005); all plans demonstrated no significant statistical
difference in HI (P=0.120). V20 and V30 were
reduced by 10.7–22.6% (P=0.002) and 12.8–21% (P=0.026),
respectively, for normal lung tissue using the VMAT plan. 5F-IMRT
was superior regarding the Dmax for the spinal cord
(P=0.037).
 | Table III.Comparison of PTV and organs at risk
sparing for all plans. |
Table III.
Comparison of PTV and organs at risk
sparing for all plans.
| Variable | VMATa |
5F-IMRTa | 3D-CRTa | P-value |
|---|
|
PTV_V95% | 97.3±1.2 | 99.2±1.3 | 95.1±1.5 | 0.003 |
|
PTV_V110% | 1.6±1.1 | 2.4±1.7 | 3.3±1.4 | 0.012 |
|
PTV_D2 | 62.4±0.6 | 62.7±0.3 | 64.2±1.6 | 0.061 |
|
PTV_D98 | 57.6±1.5 | 58.4±0.8 | 55.3±1.4 | 0.074 |
| PTV_HI | 0.1±0.01 | 0.15±0.02 | 0.22±0.05 | 0.120 |
| PTV_CI | 0.85±0.08 | 0.70±0.07 | 0.63±0.03 | 0.005 |
|
Lung_V5 | 48.5±3.2 | 43.4±2.1 | 47.3±5.4 | 0.065 |
|
Lung_V20 | 22.6±3.7 | 25.3±2.8 | 29.2±3.6 | 0.002 |
|
Lung_V30 | 14.3±2.2 | 16.4±1.7 | 18.1±2.6 | 0.026 |
|
Lung_Dmean(Gy) | 10.3±1.2 | 11.2±2.5 | 11.8±1.4 | 0.074 |
|
Heart_V20 | 23.5±2.6 | 22.7±1.3 | 24.6±2.8 | 0.056 |
|
Heart_Dmean(Gy) | 15.7±5.3 | 16.4±6.2 | 17.3±7.5 | 0.077 |
| Spinal
Cord_Dmax(Gy) | 43.5±1.8 | 40.3±2.5 | 44.2±1.4 | 0.037 |
INI dose 60 Gy prescription for
thoracic EC treatment
Tables IV–VI compare the three treatment plans based
on the dosimetric parameters of INI in thoracic EC, the EUD, DVHs
and P-values for each of the thoracic lymph nodes. In the three
plans, the mean EUD was >40 Gy in the majority of the
upper-thoracic lymph nodal regions, except for 106pre and 106tb-L
levels of the VMAT plans. 3D-CRT demonstrated the highest EUD for
106pre (P=0.014) and 106tb-L (P=0.030). V40 of 106pre in
3D-CRT was the highest compared with VMAT and 5F-IMRT (P=0.023).
For middle-thoracic EC, the mean EUD of all lymph nodal regions was
>40 Gy in the VMAT and 5F-IMRT plans, and 108 and 110 levels in
the 3D-CRT plan demonstrated poor results. The VMAT plan exhibited
the greatest EUD and a V40 value of 107 (P=0.004 and
0.006); and 5F-IMRT demonstrated superior values of 108 and 110 in
EUD and V40 (P=0.017, 0.008; P=0.025, 0.036,
respectively). There was a significant difference between the three
treatment plans in 112ao, 112pul-R and 112pul-L levels for lower
thoracic EC. The VMAT plan exhibited the highest values of EUD and
V40 in these lymph nodal stations (P=0.001, 0.001;
P=0.002, 0.004; P=0.015, 0.008, respectively). Comparisons of INI
doses for the three different treatment plans for each
statistically significant lymph node station are further
illustrated in Figs. 1–3. Fig. 1
illustrates that the 3D-CRT plan resulted in higher EUD values for
INI. Fig. 2 shows that the 5F-IMRT
and VMAT plans resulted in relatively higher EUD values compared
with the 3D-CRT plan in INI. Fig. 3
highlights the VMAT plan exhibited higher EUD values compared with
the 5F-IMRT and 3D-CRT plans in INI. A boxplot graph demonstrates
the level of dispersion within the lymph nodal dataset and the EUD
values of INI for the three different treatment plans.
 | Table IV.Incidental nodal irradiation dose for
upper-thoracic EC. |
Table IV.
Incidental nodal irradiation dose for
upper-thoracic EC.
|
| 105 | 106tb-R | 106pre | 106tb-L | 106recR | 106recL |
|---|
|
|
|
|
|
|
|
|
|---|
| Variable | EUD, Gy | V40,
% | EUD, Gy | V40,
% | EUD, Gy | V40,
% | EUD, Gy | V40,
% | EUD, Gy | V40,
% | EUD, Gy | V40,
% |
|---|
| VMAT | 58.8±0.6 | 100±0 | 57.6±0.1 | 97±1 | 35.7±1.4 | 45±14 | 38.6±2.5 | 52±23 | 45.8±1.2 | 53±24 | 52.4±1.6 | 80±31 |
| 5F-IMRT | 60.2±0.3 | 100±0 | 58.8±0.6 | 100±0 | 44.8±0.8 | 65±21 | 43.4±1.3 | 54±15 | 47.3±0.9 | 54±17 | 50.3±2.4 | 78±24 |
| 3D-CRT | 62.5±0.2 | 100±0 | 60.2±0.4 | 100±0 | 50.3±1.2 | 80±18 | 47.5±2.1 | 57±8.0 | 45.2±1.8 | 53±13 | 53.2±1.5 | 81±26 |
| P-value | 0.230 | 1.000 | 0.350 | 0.870 | 0.0140 | 0.0230 | 0.030 | 0.062 | 0.140 | 0.630 | 0.380 | 0.270 |
 | Table VI.Incidental nodal irradiation dose for
lower-thoracic EC. |
Table VI.
Incidental nodal irradiation dose for
lower-thoracic EC.
|
| 110 | 112ao | 112pul-R | 112pul-L |
|---|
|
|
|
|
|
|
|---|
| Variable | EUD, Gy | V40,
% | EUD, Gy | V40,
% | EUD, Gy | V40,
% | EUD, Gy | V40,
% |
|---|
| VMAT | 54.3±0.8 | 86±13 | 60.6±0.5 | 97±11 | 50.3±0.4 | 72±23 | 46.9±0.5 | 62±16 |
| 5F-IMRT | 53.8±0.4 | 84±14 | 52.8±0.9 | 88±23 | 42.3±0.3 | 58±14 | 37.2±0.3 | 38±21 |
| 3D-CRT | 53.4±0.3 | 83±27 | 44.2±1.0 | 65±17 | 35.3±0.2 | 40±20 | 30.5±0.7 | 33±12 |
| P-value | 0.640 | 0.870 | 0.001 | 0.001 | 0.002 | 0.004 | 0.015 | 0.008 |
Discussion
VMAT, IMRT and 3D-CRT are important RT approaches
for the treatment of thoracic EC in both definitive and
neo-adjuvant settings. The dose distribution and dosimetric
parameters of the three treatment plans were acceptable according
to established clinical criteria. The VMAT plan generated the
greatest CI in three technical studies, and decreased the
percentage exposure of the normal lung tissue to 20 and 30 Gy
radiation. The use of 5F-IMRT resulted in the best V95%
and the smallest percentage of 5 Gy and 20 Gy dose incidental
irradiation of the lung and heart, respectively. Finally, of the
three plans, 5F-IMRT also demonstrated the lowest Dmax
in the spinal cord.
Fenkell et al (19) suggested that IMRT plans provide
improved target volume coverage and conformity compared with 3D-CRT
plans, with decreased irradiation of normal structures in cervical
EC. Yin et al (20) reported
that the rapid-arc approach achieved similar coverage to f-IMRT,
and effectively spared OARs in cervical EC. This is similar to the
findings of Benthuysen et al (21), which revealed that VMAT plans had OAR
sparing and PTV coverage similar to that of IMRT in distal EC. The
present study suggests that VMAT may be equivalent to IMRT, and
even slightly more effective than 3D-CRT from a dosimetric
perspective, which is consistent with the literature.
Numerous studies have reported that the poor
long-term survival of patients with EC is associated with a high
incidence of lymph node metastasis and local recurrence of thoracic
EC (22–24). Therefore, the predominant clinical
recommendation is elective nodal irradiation for patients with EC
(25–27). Zhao et al (28) suggested that incidental radiation
doses to lymph nodes were considerable for early stage
non-small-cell lung cancer (NSCLC) without intentional elective
nodal irradiation and that these doses were likely to reach a level
that may achieve a modest clinical benefit. This may account for
the lower incidence of regional failure. Kepka et al
(29) performed a study with 220
patients with NSCLC, which suggested that incidental nodal
irradiation was able to eradicate some subclinical metastases in
regional lymph nodes. The present study demonstrated that RT
technologies generate considerable incidental irradiation doses to
lymph nodal stations in thoracic EC. The mean EUD of all thoracic
lymph nodes NO. 105-112 irradiated using 3D-CRT, 5F-IMRT or VMAT
was >40 Gy.
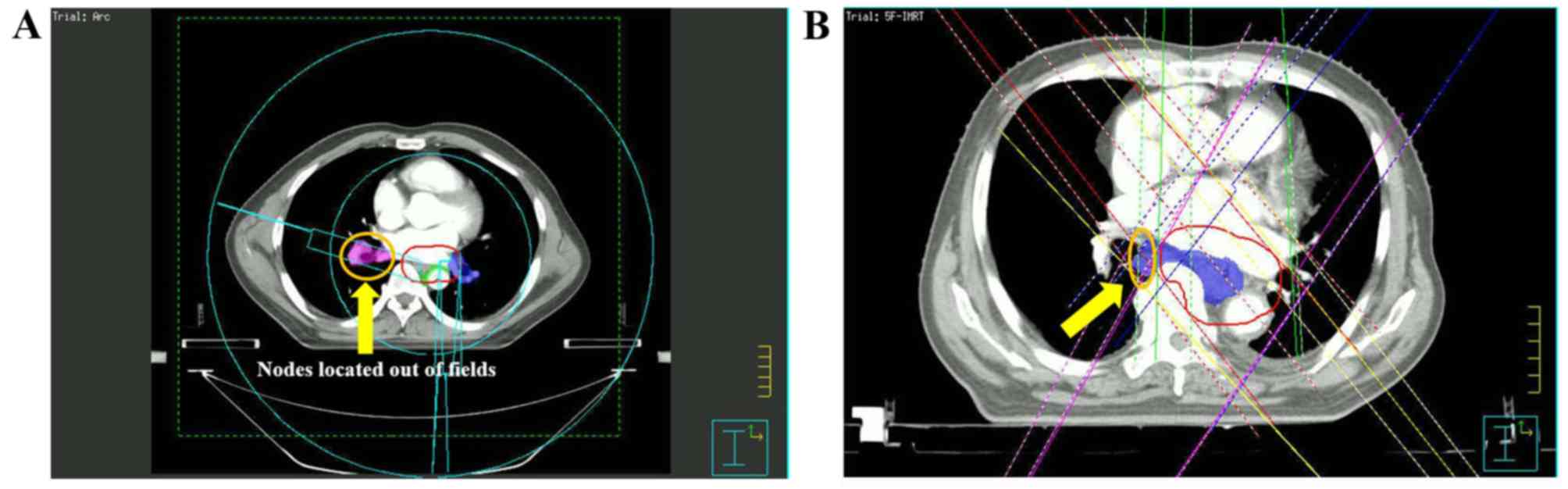
In upper-thoracic EC, the 3D-CRT plan resulted in
higher EUD values in incidental irradiation doses for 106Pre and
106tb-L, compared with 5F-IMRT and VMAT (Fig. 1). In middle- and lower-thoracic EC,
the majority of the lymph nodes are out of the field of irradiation
and using conventional conformal beams does not obtain the desired
incidental irradiation dose (Figs. 2
and 3). This may be explained by the
fact that IMRT and VMAT use multiple segments and therefore, doses
delivered to lymph nodes are lower compared with those delivered by
3D-CRT due to the steeper dose fall-off achieved with IMRT or VMAT.
Due to the location of NO 105 and 106 they are in the field of
radiation, therefore the modulated method of 3D-CRT has an
advantage for incidental irradiation dose in upper-thoracic EC
(Fig. 4). The 5F-IMRT and VMAT plans
demonstrated almost equal mean EUD values in middle-thoracic EC,
and the VMAT plan resulted in greater incidental nodal irradiation
in lower-thorax EC.
The incidental nodal irradiation dose is associated
with treatment technique, beam arrangement, number of beams and
esophageal tumor length, volume and location. Using different
treatment units may influence its contribution to incidental nodal
irradiation (Fig. 5). Reports also
demonstrate that the larger the area of thoracic EC, the higher the
risk of lymph node metastasis (30,31). In
the present study, the length of tumors was 3.00–13.3 cm and lymph
nodes received relatively high incidental irradiation doses.
Further studies are required to determine if controlling metastasis
or recurrence in nodal regions is influenced by the effect of
incidental irradiation in the treatment of thoracic EC.
The present study was a retrospective analysis of
patients with T1-3N0M0 stage
thoracic EC receiving treatment at the Hangzhou Cancer Hospital.
All of the dosimetric metrics for target volume, OARs and
incidental nodal irradiation were collected from DVHs. The true
dose distribution for patients during irradiation may be different
from simulation on TPS, due to organ motion, scattering and leaking
of radiation from leaf pairs. IMRT and VMAT should be performed
with caution in the course of treatment, particularly for
out-of-field lymph nodes. The incidental nodal radiation generated
by IMRT or VMAT warrants further investigation and discussion.
In summary, the present study demonstrated that VMAT
was comparable to 5F-IMRT in regards to the dosimetric
characteristics of planning. Further, incidental nodal irradiation
doses to thoracic nodal levels NO 105–112 are considerable for
thoracic EC, which may have an impact on the control of metastasis
and recurrence in nodal regions.
Acknowledgements
Not applicable.
Funding
This present study was supported by the Medical
Technology Planning Program of Zhejiang Province (grant no.
2018KY596) and the Medical Technology Planning Program of Zhejiang
Province (grant no. 2019KY507).
Availability of data and materials
The data sets used and/or analyzed during the
present study are available from the corresponding author on
reasonable request.
Authors' contributions
NZ, SXW and JHW contributed to the conception of
this study and performed preliminary experimentation. NZ and MG
were responsible for enrolling patients in the study, performing
clinical diagnoses and collecting clinical data. All authors
participated in the statistical analysis, contributed to the
interpretation of the results and manuscript writing. All authors
reviewed the data and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Medical Ethics
Committee of Hangzhou Cancer Hospital (Hangzhou, China) and written
informed consent was obtained from all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
American Cancer Society. Esophageal
cancer, . Atlanta, GA: American Cancer Society; 2007
|
|
2
|
Djarv T, Lagergren J, Blazeby JM and
Lagergren P: Long-term health-related quality of life following
surgery for esophageal cancer. Br J Surg. 95:1121–1126. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Minsky BD, Pajak TF, Ginsberg RJ, Pisansky
TM, Martenson J, Komaki R, Okawara G, Rosenthal SA and Kelsen DP:
INT0123 (Radiation Therapy Oncology Group 94-05) phase III trial of
combined-modality therapy for esophageal cancer: High-dose versus
standard-dose radiation therapy. J Clin Oncol. 20:1167–1174. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cooper JS, Guo MD, Herskovic A, Macdonald
JS, Martenson JA Jr, Al-Sarraf M, Byhardt R, Russell AH, Beitler
JJ, Spencer S, et al: Chemoradiotherapy of locally advanced
esophageal cancer: Long-term follow-up of a prospective randomized
trial (RTOG 85-01). Radiation therapy oncology group. JAMA.
281:1623–1627. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Coia LR, Minsky BD, Berkey BA, John MJ,
Haller D, Landry J, Pisansky TM, Willett CG, Hoffman JP, Owen JB
and Hanks GE: Outcome of patients receiving radiation for cancer of
the esophagus: Results of the 1992–1994 patterns of care study. J
Clin Oncol. 18:455–462. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Smith TJ, Ryan LM, Douglass HO Jr, Haller
DG, Dayal Y, Kirkwood J, Tormey DC, Schutt AJ, Hinson J and Sischy
B: Combined chemoradiotherapy vs. radiotherapy alone for early
stage squamous cell carcinoma of the esophagus: A study of the
Eastern Cooperative Oncology Group. Int J Radiat Oncol Biol Phys.
42:269–276. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Muijs C, Smit J, Karrenbeld A, Beukema J,
Mul V, van Dam G, Hospers G, Kluin P, Langendijk J and Plukker J:
Residual tumor after neoadjuvant chemoradiation outside the
radiation therapy target volume: A new prognostic factor for
survival in esophageal cancer. Int J Radiat Oncol Biol Phys.
88:845–852. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ji K, Zhao L, Yang C, Meng M and Wang P:
Three-dimensional conformal radiation for esophageal squamous cell
carcinoma with involved-field irradiation may deliver considerable
doses of incidental nodal irradiation. Radiat Oncol. 7:2002012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cozzi L, Dinshaw KA, Shrivastava SK,
Mahantshetty U, Engineer R, Deshpande DD, Jamema SV, Vanetti E,
Clivio A, Nicolini G and Fogliata A: A treatment planning study
comparing volumetric arc modulation with rapidArc and fixed field
IMRT for cervix uteri radiotherapy. Radiother. Oncol. 89:180–191.
2008.
|
|
10
|
Guckenberger M, Richter A, Krieger T,
Wilbert J, Baier K and Flentje M: Is a single arc sufficient in
volumetric-modulated arc therapy (VMAT) for complex-shaped target
volumes? Radiother. Oncol. 93:259–265. 2009.
|
|
11
|
Shaffer R, Morris WJ, Moiseenko V, Welsh
M, Crumley C, Nakano S, Schmuland M, Pickles T and Otto K:
Volumetric modulated arc therapy and conventional
intensity-modulated radiotherapy for simultaneous maximal
intraprostatic Boost: A planning comparison study. Clin Oncol (R
Coll Radiol). 21:401–407. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
ICRU Report 62, . Prescribing, Recording,
and Reporting Photon Beam Therapy. (Supplement to ICRU Report
50):21:1999.
|
|
13
|
Japanese Society for Esophageal Disease, .
Guide lines for the clinical and pathologic studies for carcinoma
of the esophagus. Jpn J Surg. 1976:79–86. 1976.
|
|
14
|
Japan Esophageal Society, . Japanese
classification of esophageal cancer, 11th Edition: part I.
Esophagus. 6:71–94. 2009. View Article : Google Scholar
|
|
15
|
Harris KM, Adams H, Lloyd DC and Harvey
DJ: The effect on apparent size of simulated pulmonary nodules of
using three standard CT window settings. Clin Radiol. 47:241–244.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Otto K: Volumetric modulated arc therapy:
IMRT in a single gantry arc. Med Phys. 35:310–317. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fogliata A, Yartsev S, Nicolini G, Clivio
A, Vanetti E, Wyttenbach R, Bauman G and Cozzi L: On the
performances of intensity modulated protons, RapidArc, helical
tomotherapy for selected paediatric cases. Radiat Oncol. 4:22009.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fogliata A, Clivio A, Nicolini G, Vanetti
E and Cozzi L: Intensity modulation with photons for benign
intracranial tumours: A planning comparison of volumetric single
arc, helical arc and fixed gantry techniques. Radiother Oncol.
89:254–262. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fenkell L, Kaminsky I, Breen S, Huang S,
Van Prooijen M and Ringash J: Dosimetric comparison of IMRT vs. 3D
conformal radiotherapy in the treatment of cancer of the cervical
esophagus. Radiother. Oncol. 89:287–291. 2009.
|
|
20
|
Yin Y, Chen J, Xing L, Dong X, Liu T, Lu J
and Yu J: Applications of IMAT in cervical esophageal cancer
radiotherapy: A comparison with fixed-field IMRT in dosimetry and
implementation. J Appl Clin Med Phys. 12:48–57. 2011. View Article : Google Scholar
|
|
21
|
Van Benthuysen L, Hales L and Podgorsak
MB: Volumetric modulated arc therapy vs. IMRT for the treatment of
distal esophageal cancer. Med Dosim. 36:404–409. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shimada H, Kitabayashi H, Nabeya Y,
Okazumi S, Matsubara H, Funami Y, Miyazawa Y, Shiratori T, Uno T,
Itoh H and Ochiai T: Treatment response and prognosis of patients
after recurrence of esophageal cancer. Surgery. 133:24–31. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Greenlee RT, Hill-Harmon MB, Murray T and
Thun M: Cancer statistics, 2001. CA Cancer J Clin. 51:15–36. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nakagawa S, Kanda T, Kosugi S, Ohashi M,
Suzuki T and Hatakeyama K: Recurrence pattern of squamous cell
carcinoma of the thoracic esophagus after extended radical
esophagectomy with three-field lymphadenectomy. J Am Coll Surg.
198:205–211. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hsu FM, Lee JM, Huang PM, Lin CC, Hsu CH,
Tsai YC, Lee YC and Chia-Hsien Cheng J: Retrospective analysis of
outcome differences in preoperative concurrent chemoradiation with
or without elective nodal irradiation for esophageal squamous cell
carcinoma. Int J Radiat Oncol Biol Phys. 81:593–599. 2011.
View Article : Google Scholar
|
|
26
|
Zhao KL, Ma JB, Liu G, Wu KL, Shi XH and
Jiang GL: Three-dimensional conformal radiation therapy for
esophageal squamous cell carcinoma: Is elective nodal irradiation
necessary? Int J Radiation Oncology Biol Phys. 76:446–451. 2010.
View Article : Google Scholar
|
|
27
|
Welsh J, Settle SH, Amini A, Xiao L,
Suzuki A, Hayashi Y, Hofstetter W, Komaki R, Liao Z and Ajani JA:
Failure patterns in patients with esophageal cancer treated with
definitive chemoradiation. Cancer. 118:2632–2640. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhao L, Chen L, Ten Haken R, Chetty I,
Chapet O, Hayman JA and Kong FM: Three-dimensional conformal
radiation may deliver considerable dose of incidental nodal
irradiation in patients with early stage node-negative non-small
cell lung cancer when the tumor is large and centrally located.
Radiother Oncol. 82:153–159. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kepka L, Maciejewski B and Withers RH:
Does incidental irradiation with doses below 50 Gy effectively
reduce isolated nodal failures in non-small-cell lung cancer:
Dose-response relationship. Int J Radiat Oncol Biol Phys.
73:1391–1396. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Huang W, Li B, Gong H, Yu J, Sun H, Zhou
T, Zhang Z and Liu X: Pattern of lymph node metastases and its
implication in radiotherapeutic clinical target volume in patients
with thoracic esophageal squamous cell carcinoma: A report of 1077
cases. Radiother Oncol. 95:229–233. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chen J, Liu S, Pan J, Zheng X, Zhu K, Zhu
J, Xiao J and Ying M: The pattern and prevalence of lymphatic
spread in thoracic oesophageal squamous cell carcinoma. Eur J
Cardiothorac Surg. 36:480–486. 2009. View Article : Google Scholar : PubMed/NCBI
|